Abstract
Exsanguination remains the leading cause of preventable death among victims of trauma. For adult and pediatric trauma patients in the prehospital phase of care, methods to control hemorrhage and hemostatic resuscitation are described in this joint consensus opinion by the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, and the National Association of EMS Physicians.
Introduction
Exsanguination remains the leading cause of preventable death among victims of trauma with nearly half of these patients dying in the prehospital setting (Citation1). This statement represents a joint consensus opinion on prehospital hemorrhage control and hemostatic resuscitation by the American College of Surgeons Committee on Trauma, the American College of Emergency Physicians, and the National Association of EMS Physicians. It is intended for use by emergency medical services (EMS) clinicians, EMS medical directors, emergency physicians, trauma surgeons, and nurses in their treatment of the acute trauma patient with severe, life-threatening external bleeding. As bystanders are included in the trauma chain of survival and often serve as the first link in the chain, this document also provides guidance for the layperson in managing hemorrhage in the prehospital setting. This document is not intended to be a comprehensive discussion of hemorrhage control and resuscitation in the trauma patient. Rather, it combines the collective expertise of the authors and represented organizations with current published evidence to offer unified guidance on techniques to control hemorrhage and provide hemostatic resuscitation in this patient population. All clinicians should be familiar with American College of Surgeons Stop the Bleed program and ongoing continuing education to reinforce skills is strongly encouraged.
Points of Consensus
Direct pressure remains the first choice of treatment and effectively controls bleeding in most patients
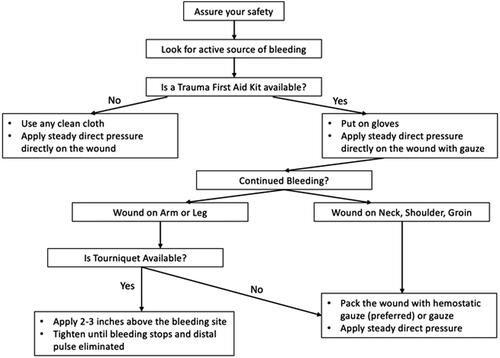
Bleeding Control Algorithm for Life-Threatening External Hemorrhage (Citation2) ()
Identify the source of bleeding and determine if the bleeding is life threatening.
When hemorrhage control with direct pressure alone is not possible or is ineffective, the use of gauze and/or hemostatic-impregnated dressings for wound packing, and the use of tourniquets on extremities to address compressible arterial bleeding, are recommended.
Bleeding from the torso or junctional wounds including the neck, shoulder/axilla, and groin can be controlled by direct pressure, by packing the wound, and/or by placing a junctional tourniquet (axilla or groin only).
Wound packing increases direct pressure on the vessels within the wound (Citation3). To pack a traumatic wound, a clean cloth, gauze, or hemostatic-impregnated dressing is pressed deeply and firmly into the wound. Packing should be added while maintaining direct pressure until the wound is completely filled. Once packed, the wound should be covered with a dressing and significant pressure should be applied by both hands and maintained until initial hemostasis is achieved (Citation3).
Scalp injuries are known to cause severe life-threatening bleeding and can be controlled with direct pressure or rapid wound closure with running nylon suture.
Local Hemostatic-Impregnated Dressings
Tourniquets
There is greater chance of survival for the extremity trauma patient with life-threatening bleeding the earlier a tourniquet is applied (Citation7, Citation8). Among patients who needed a tourniquet in the combat setting mortality was universal when one was not applied (Citation9). Tourniquets should be stored where they can be rapidly accessed and applied.
Extremity tourniquet technique (Citation10)
Apply at minimum 2 to 3 inches proximal to the wound.
Placing a tourniquet as proximal and as tight as possible on the injured extremity (“high and tight” method) should be limited to circumstances where it is impossible or unsafe to determine the exact source of bleeding.
Placement on bare skin is preferred whenever possible. Do not place over the elbow, wrist, knee, or ankle joints.
Ensure that all slack is removed before tightening the windlass to avoid bunching and twisting.
Tighten the tourniquet until bleeding stops and the distal pulse is eliminated.
Note the time the tourniquet was applied and record this time, so the information is readily available. Preferably the time should be recorded on the patient or tourniquet.
Do not loosen the tourniquet once applied.
To maintain effectiveness of hemorrhage control, re-assess the wound and tourniquet following any patient movement (e.g., ground to stretcher, stretcher to ambulance) and during transport to ensure continued adequate hemostasis.
If hemostasis is not obtained, add a second tourniquet 2–3 inches above the tourniquet in place. Do not remove the original tourniquet.
Reassess prior tourniquet application
Tourniquets placed by non-clinicians need to be further evaluated by trained medical professionals.
Begin by determining if a tourniquet is needed (Citation11). If the clinician feels that the tourniquet is needed, follow local guidelines. If it appears a tourniquet was not or is no longer indicated, see the tourniquet conversion instructions that follow.
Ensure hemostasis.
Determine if a distal pulse is present.
Improvised tourniquet
Improvised tourniquets are not recommended in the prehospital setting due to ineffectiveness and should be converted to a commercial grade tourniquet as soon as possible (Citation12). If an improvised tourniquet must be used (Citation13), great care must be taken to ensure that the benefits outweigh the risks. Immediately when a commercial grade tourniquet is available, it should be placed proximal to the wound and the improvised tourniquet removed.
Tourniquet conversion
Tourniquet conversion is the deliberate process exchanging a tourniquet for a pressure dressing or hemostatic agent – this applies to both commercial and improvised tourniquets. Tourniquet conversion must only to be performed by trained medical professionals.
When is the best time to attempt conversion of a tourniquet?
Recommendation: Assuming that the commercial or improvised tourniquet has been applied for a correct indication, a candidate for conversion is one who meets all the following recommendations:
Anticipated transport time to a place where surgical support is immediately available is > 2 hours (Citation14)
Patient is not in shock (shock defined by SBP <90 mmHg if age 10–64, SBP < 110 mmHg age if age 65 and up).
The wound can be monitored for rebleeding during the entire Patient transport.
Absence of complete or near complete amputation.
Tourniquet has been applied for less than 6 hours (Citation15–17)
How do you convert a tourniquet?
Recommendation (Citation15):
Place a new tourniquet, – referred to as “Tourniquet Plus 1”, 2 to 4 inches proximal to the wound and keep it loose. If the original commercial or improvised tourniquet is in this same area, place the new loose Tourniquet Plus 1 proximal to the original tourniquet.
Apply a pressure dressing to the wound. A hemostatic-impregnated dressing may be utilized if available.
Loosen/release the windlass rod on the original commercial or improvised tourniquet.
Monitor the wound for bleeding.
If no bleeding occurs, successful conversion to bleeding control without a tourniquet has been accomplished. If bleeding recurs despite the pressure dressing, tighten Tourniquet Plus 1. Resolving arterial spasm causing delayed bleeding during tourniquet conversion is a possible cause of re-bleeding so careful monitoring of the wound once the tourniquet off is required.
If bleeding continues despite tightening Tourniquet Plus 1, tighten the original tourniquet (if commercial), and replace any improvised tourniquet with a commercial tourniquet.
Continue to reassess any tightened tourniquet(s) for effectiveness.
Tourniquet Pitfalls to Avoid (Citation15, Citation18)
Delaying or avoiding a tourniquet for life threatening extremity bleeding.
Applying a tourniquet to control bleeding when other methods such as direct pressure and wound packing would suffice.
Applying a tourniquet over a joint. Application over the peroneal nerve (knee or ankle) or ulnar nerve (elbow) may result in nerve damage or paralysis.
Applying a tourniquet over clothing. Fully expose the involved limb(s), removing clothing from the limb(s), and do not cover a tourniquet with bandages or any other material.
Applying a tourniquet too close to the wound. Tourniquets placed near/over the wound can increase risk for additional tissue damage.
Applying a tourniquet loosely. This may decrease bleeding but if the distal pulse remains, ongoing arterial flow with obstruction to venous return can result in an increase in venous bleeding. The consequences may include avoidable pain due to venous congestion and compartment syndrome. If pulses are present and there is no hemorrhage, it is likely the tourniquet is not controlling true arterial hemorrhage.
Delaying or avoiding a second tourniquet when arterial bleeding continues.
Loosening a tourniquet periodically. This is different than loosening a tourniquet as part of a tourniquet conversion as outlined previously.
Failing to reassess a tourniquet that may have loosened during transport.
Removing a tourniquet during in a patient in shock and/or ongoing, uncontrolled bleeding.
Allowing patient pain to interfere with proper bleeding control.
Junctional tourniquet (Citation19, Citation20)
Junctional regions are where extremities join the torso, such as the shoulder/axilla or the groin, and are too proximal for extremity tourniquet application.
Junctional tourniquets are external compression devices that occlude blood flow from the aorta, axillary artery, or iliac artery to prevent hemorrhage (Citation21)
Junctional tourniquet options include (Citation21):
A belt that uses a windlass to tighten and stabilize its position on the axilla, abdomen, or groin. Once in place, a pneumatic bladder is inflated to provide targeted compression by occluding the axillary artery (recommended application time < 4 hours), the aorta (recommended application time < 1 hour), or the iliac artery (recommended application time < 4 hours).
A vise-like compression clamp that can be secured to the axilla or groin and tightened with a hand crank to occlude the underlying vasculature (recommended application time < 4 hours).
A belt that can be placed around the pelvis with two mechanical pressure pads or an inflatable bladder that occludes the iliac or femoral artery. (recommended application time < 4 hours)
Junctional tourniquets are approved by the Food and Drug Administration (FDA) and Department of Defense. Currently, there is inadequate clinical experience and data in civilian trauma to routinely recommend these.
Blood Products (when available)
Prehospital blood product resuscitation has demonstrated greater than predicted survival with a 37% reduction in 30-day mortality among severely injured civilian patients (Citation22–26).
Among military patients, prehospital transfusion within minutes of injury was associated with significantly reduced 24-hour and 30-day mortality (Citation16)
Damage control resuscitation includes permissive hypotension (allowing for lower than physiologic levels as long as mental status is maintained) if defined in local protocols in non-brain-injured patients (Citation27, Citation28) minimizing crystalloid volume, and adhering to the balanced transfusion of packed red blood cells (PRBCs), plasma, and platelets, to decrease the risk of trauma-induced coagulopathy and endothelial injury. Whole blood may be used as well.
Recommendation: Patients with signs of hemorrhagic shock should receive prehospital blood products whenever available (Citation24–26, Citation29).
Establish a prehospital transfusion protocol utilizing a multi-specialty collaborative approach including, both field and hospital clinicians (Citation30).
Whole blood is preferred over PRBC. If only component blood products (PRBC, plasma) are available, transfuse in a 1:1 ratio.
Supply and Storage
Ensure an adequate supply is readily available.
Ensure any vehicle carrying these products is equipped to maintain appropriate storage conditions.
Consider reallocation of older blood products to high-use areas to avoid expiry waste.
Blood transfusion should ideally be performed utilizing a blood warmer to achieve a delivery temperature of 38 °C/100 °F but no higher than 42 °C/108 °F (Citation28)
Indications for administration
Blood products should be strongly considered when a patient has a penetrating truncal mechanism (Citation31), external signs of hemorrhage, a positive abdominal Focused Assessment with Sonography for Trauma when available with vital signs suggestive of hemorrhagic shock (systolic blood pressure < 90 mmHg, heart rate > 120 beats per minute, or another quantitative measure such as the shock index) (Citation32–35). Systems that wish to integrate prehospital administration of blood and blood products into their practice should work with all appropriate stakeholders to ensure successful delivery
Tracking
Protocols should be in place for tracking all units transfused as well as managing and reporting transfusion-related complications
Prehospital Transfusion of Women of Childbearing Age
Given that most of the blood products available in the field are Rh positive, this can pose a risk of isoimmunization where the mother’s red blood cells are incompatible with the baby’s red blood cells resulting in hemolysis or destruction of the baby’s red blood cells if the patient is early in a pregnancy and EMS is unaware.
However, despite this risk, most systems have decided that the benefits of prehospital transfusion outweigh the risks in this scenario, but there must be a plan for coordination with the trauma centers to ensure that the patient gets Rho(D) immune globulin (RhoGAM) if indicated (Citation35).
While blood products in the field are helpful, the resources utilized can be challenging and logistically not possible for many EMS organizations. Currently, blood product transfusion by civilian EMS for hemorrhagic shock is not the widespread.
If both PRBC and plasma are available, patients should receive both, starting with plasma, in a 1:1 ratio, to result in the greatest potential reduction in mortality (Citation36–41).
Resuscitation induced hypocalcemia (Citation42)
Prehospital blood product transfusion in civilian trauma is associated with hypocalcemia, which in turn predicts decreased survival and the need for massive transfusion.
1 g (10 mL) of calcium gluconate should be given for every 1 to 2 units of blood products transfused in the prehospital setting.
While currently only FDA approved for military use, freeze-dried plasma may also mitigate the costs and storage challenges of traditional cold-stored blood products (Citation43, Citation44).
The use of prothrombin complex concentrate in the prehospital setting is not recommended unless it is administered as goal directed reversal of anticoagulants (Citation45).
Prehospital tranexamic acid (TXA) administration (1–2 grams IV in 100 mL normal saline or lactated Ringers over 10 minutes by IV infusion) should be considered within 3 hours of injury (Citation46–49). The evidence on TXA is evolving.
Hypothermia is a marker for poor prognosis after hemorrhage; thus, maintaining normothermia is recommended (Citation50).
Resuscitative Endovascular Balloon Occlusion of the Aorta (REBOA)
REBOA is a percutaneous procedure for life-threatening abdominal and/or pelvic hemorrhage that temporarily occludes the aorta utilizing an endovascular balloon (Citation51).
There is insufficient data to support recommendation of REBOA to be used in the prehospital setting (Citation52).
Pelvic circumferential compression devices (PCCDs)
These devices are most likely to benefit a patient with an open book pelvic fracture. Recognizing the diagnostic limitations in the field, it is often not possible to differentiate a stable from an unstable fracture pattern in the prehospital setting (Citation53–56). There is no clinical evidence that pelvic compression worsens displacement of certain fracture patterns, particularly lateral compression fractures or causes injuries to internal structures through fracture fragment motion. Suspected pelvic fractures should be treated with circumferential pelvic compression (Citation57–59).
Pelvis examination by compression of the iliac crests toward the midline (NOT distraction) should be assessed in the secondary survey. If any instability or crepitus is felt, the patient should be placed in a circumferential wrap centered over the greater trochanters (Citation60). Prehospital PCCD is recommended in suspected pelvic fracture based on a mechanism of severe blunt force trauma or one of the following: pain on exam, hypotension, a compromised exam by altered mental status or distracting injury, or blast/high energy injury with lower extremity amputation.
Prolonged use or overtightening of PCCD may cause pressure ulceration (Citation58).
Pediatric Considerations
Pediatric circulating blood volume is approximately 80 mL/kg. A child may lose up to 45% of circulating blood volume before exhibiting hypotension (Citation59). Therefore, hypotension is a late sign of shock. Hypotension in children is determined by age and systolic blood pressure (SBP < 70 mmHg + (age in years x 2) for age 0–9; SBP < 90 mmHg age 10 and up) (Citation61). Direct pressure at or immediately proximal to the site of injury should always be the initial technique for hemorrhage control (Citation62).
If direct pressure fails to control exsanguinating hemorrhage, a tourniquet should be applied (Citation62).
Except children less than 2 years old, the same tourniquet used for adults can be used for children. The tourniquet should be placed 2–3 inches proximal to the bleeding site with enough proximal pressure to impede arterial blood flow (Citation62). There are published studies in children 2–7 years and 6–16 years where adult tourniquets were successfully used, although three windlass turns were often needed. If the tourniquet fails to provide occlusion, direct pressure should be used (Citation63–65).
Junctional tourniquets may work on teenagers and larger children but there is limited information in the current literature to give guidance.
If commercial tourniquets are too large, apply direct pressure on the wound. For large, deep wounds, pack the wound. Hemostatic-impregnated dressings should be applied with at least 3 minutes of direct pressure (Citation6).
Tourniquets should frequently be reevaluated after placement for appropriate positioning and adequate control of bleeding (Citation62).
The principles of tourniquet conversion are identical for children and adults.
Mass Casualty Situations
The above guidance is not designed to be used in mass casualty situations
In all situations where the number of patients outweigh the available resources, hemorrhage control and treatment should be done as quickly as possible and focused on the most-acute patients using triage principles.
Summary
Consensus-based guidance on prehospital hemorrhage control and hemostatic resuscitation is described
Where variations and differences of opinion are present, local protocols should be developed and followed
Update local protocols based on a performance improvement process.
Ongoing continuing education to reinforce initial training skills is strongly encouraged
Disclosure Statement
No authors have declared any conflict of interest related to this work.
Notes
This consensus document is being published simultaneously in Annals of Emergency Medicine.
References
- Tompeck AJ, Gajdhar AUR, Dowling M, Johnson SB, Barie PS, Winchell RJ, King D, Scalea TM, Britt LD, Narayan M, et al. A comprehensive review of topical hemostatic agents: the good, the bad, and the novel. J Trauma Acute Care Surg. 2020;88(1):e1–e21. doi:10.1097/TA.0000000000002508.
- Bulger EM, Snyder D, Schoelles K, Gotschall C, Dawson D, Lang E, Sanddal ND, Butler FK, Fallat M, Taillac P, et al. An evidence-based prehospital guideline for external hemorrhage control: American College of Surgeons Committee on Trauma. Prehosp Emerg Care. 2014;18(2):163–73. doi:10.3109/10903127.2014.896962.
- Picard C. Hemorrhage control, a fundamental skill: a review of direct pressure, dressings, wound packing and bandages for life saving. Can J Emerg Nurs. 2017;40(2):2626–8.
- Bennett BL, Littlejohn LF, Kheirabadi BS, Butler FK, Kotwal RS, Dubick MA, Bailey HH. Management of external hemorrhage in tactical combat casualty care: Chitosan-based hemostatic gauze dressings –TCCC Guidelines – Change 13-05. J Spec Oper Med. 2014;14(3):40–57. doi:10.55460/03VO-8FLO.
- Peng HT. Hemostatic agents for prehospital hemorrhage control: a narrative review. Mil Med Res. 2020;7(1):13. doi:10.1186/s40779-020-00241-z.
- Littlejohn L, Bennett BL, Drew B. Application of current hemorrhage control techniques for backcountry care: part two, hemostatic dressings and other adjuncts. Wilderness Environ Med. 2015;26(2):246–254. doi:10.1016/j.wem.2014.08.018.
- Scerbo MH, Mumm JP, Gates K, Love JD, Wade CE, Holcomb JB, Cotton BA. Safety and appropriateness of tourniquets in 105 civilians. Prehosp Emerg Care. 2016;20(6):712–722. doi:10.1080/10903127.2016.1182606.
- Scerbo MH, Holcomb JB, Taub E, Gates K, Love JD, Wade CE, Cotton BA. The trauma center is too late: major limb trauma without a pre-hospital tourniquet has increased death from hemorrhagic shock. J Trauma Acute Care Surg. 2017;83(6):1165–1172. doi:10.1097/TA.0000000000001666.
- Kragh JF, Walters TJ, Baer DG, Fox CJ, Wade CE, Salinas J, Holcomb JB. Survival with emergency tourniquet use to stop bleeding in major limb trauma. Ann Surg. 2009;249(1):1–7. doi:10.1097/SLA.0b013e31818842ba.
- Shackelford SA, Butler FK, Kragh JF, Stevens RA, Seery JM, Parsons DL, Montgomery HR, Kotwal RS, Mabry RL, Bailey JA. Optimizing the use of limb tourniquets in tactical combat casualty care: TCCC guidelines change 14-02. J Spec Oper Med. 2015;15(1):17–31. doi:10.55460/TDTK-RIN8.
- Bedri H, Ayoub H, Engelbart JM, Lilienthal M, Galet C, Skeete DA. Tourniquet application for bleeding control in rural trauma system: outcomes and implications for prehospital providers. Prehosp Emerg Care. 2022;26(2):246–54. doi:10.1080/10903127.2020.1868635.
- Stewart SK, Duchesne JC, Khan MA. Improvised tourniquets. J Trauma Acute Care Surg. 2015;78(1):178–183. (doi:10.1097/TA.0000000000000485.
- Drew B, Bennet BL, Littlejohn L. Application of current hemorrhage control techniques for backcountry care: part one, tourniquets and hemorrhage control adjuncts. Wilderness Environ Med. 2015;26(2):236–245. doi:10.1016/j.wem.2014.08.016.
- Levy MJ, Pasley J, Remick KN, Eastman AL, Margolis AM, Tang N, Goolsby CA. Removal of the prehospital tourniquet in the emergency department. J Emerg Med. 2021;60(1):98–102. doi:10.1016/j.jemermed.2020.10.018.
- Drew B, Bird D, Matteucci M, Keenan S. Tourniquet conversion: a recommended approach in the prolonged field care setting. J Spec Oper Med. 2015;15(3):81–85. doi:10.55460/IJ9C-6AIF.
- Shackelford SA, Del Junco DJ, Powell-Dunford N, Mazuchowski EL, Howard JT, Kotwal RS, Gurney J, Butler FK, Gross K, Stockinger ZT. Association of prehospital blood product transfusion during medical evacuation of combat casualties in Afghanistan with acute and 30 day survival. JAMA. 2017;318(16):1581–1591. doi:10.1001/jama.2017.15097.
- Tactical Combat Casualty Care Guidelines (TCCC) for Medical Personnel. August 1, 2019. https://jts.amedd.army.mil/assets/docs/cpgs/Tactical_Combat_Casualty_Care_Guidelines_01_Aug_2019.pdf. (Accessed February 20, 2023)
- Pons PT. Stop the Bleed: 8 pitfalls to avoid in hemorrhage control. https://www.trauma-news.com/2017/09/stop-bleed-8-pitfalls-avoid-hemorrhage-control/ (Accessed February 20, 2023).
- Smith S, White J, Wanis KN, Beckett A, McAlister VC, Hilsden R. The effectiveness of junctional tourniquets: a systematic review and meta-analysis. J Trauma Acute Care Surg. 2019;86(3):532–9. doi:10.1097/TA.0000000000002159.
- Van Oostendorp SE, Tan EC, Geeraedts LMG. Prehospital control of life-threatening truncal and junctional haemorrhage is the ultimate challenge in optimizing trauma care; a review of treatment options and their applicability in the civilian trauma setting. Scand J Trauma Resusc Emerg Med. 2016;24(1):110. doi:10.1186/s13049-016-0301-9.
- Smith IM, James RH, Dretzke J, Midwinter MJ. Prehospital blood product resuscitation for trauma: a systematic review. Shock. 2016;46(1):3– 16. doi:10.1097/SHK.0000000000000569.
- Brown JB, Cohen MJ, Minei JP, Maier RV, West MA, Billiar TR, Peitzman AB, Moore EE, Cuschieri J, Sperry JL. Pretrauma center red blood cell transfusion is associated with reduced mortality and coagulopathy in severely injured patients with blunt trauma. Ann Surg. 2015;261(5):997–1005. doi:10.1097/SLA.0000000000000674.
- Brown JB, Sperry JL, Fombona A, Billiar TR, Peitzman AB, Guyette FX. Pre‐trauma center red blood cell transfusion is associated with improved early outcomes in air medical trauma patients. J Am Coll Surg. 2015;220(5):797–808. doi:10.1016/j.jamcollsurg.2015.01.006.
- Morrison JJ, Oh J, DuBose JJ, O'Reilly DJ, Russell RJ, Blackbourne LH, Midwinter MJ, Rasmussen TE. En-route care capability from point of injury impacts mortality after severe wartime injury. Ann Surg. 2013;257(2):330–4. doi:10.1097/SLA.0b013e31827eefcf.
- Apodaca A, Olson CM, Bailey J, Butler F, Eastridge BJ, Kuncir E. Performance improvement evaluation of forward aeromedical evacuation platforms in Operation Enduring Freedom. J Trauma Acute Care Surg. 2013;75(2 Suppl 2):S157–S163. doi:10.1097/TA.0b013e318299da3e.
- Guyette FX, Sperry JL, Peitzman AB, Billiar TR, Daley BJ, Miller RS, Harbrecht BG, Claridge JA, Putnam T, Duane TM, et al. Prehospital blood product and crystalloid resuscitation in the severely injured patient: a secondary analysis of the prehospital air medical plasma trial. Ann Surg. 2021;273(2):358–364. doi:10.1097/SLA.0000000000003324.
- Spaite DW, Hu C, Bobrow BJ, Chikani V, Sherrill D, Barnhart B, Gaither JB, Denninghoff KR, Viscusi C, Mullins T, et al. Mortality and prehospital blood pressure in major traumatic brain injury: the absence of a hypotension threshold. JAMA Surg. 2017;152(4):360–368. doi:10.1001/jamasurg.2016.4686.
- Spaite DW, Hu C, Bobrow BJ, Chikani V, Barnhart B, Gaither JB, Denninghoff KR, Adelson PD, Keim SM, Viscusi C, et al. Association of out-of-hospital hypotension depth and duration with traumatic brain injury. Ann Emerg Med. 2017;70(4):522–530.e1. doi:10.1016/j.annemergmed.2017.03.027.
- Rehn M, Weaver A, Brohi K, Eshelby S, Green L, Røislien J, Lockey DJ. Effect of prehospital red blood cell transfusion on mortality and time of death in civilian trauma patients. Shock. 2019;51(3):284–8. doi:10.1097/SHK.0000000000001166.
- Zielinski MD, Stubbs JR, Berns KS, Glassberg E, Murdock AD, Shinar E, Sunde GA, Williams S, Yazer MH, Zietlow S, et al. Prehospital blood transfusion programs: capabilities and lessons learned. J Trauma Acute Care Surg. 2017;82(6S Suppl 1):S70–S78. doi:10.1097/TA.0000000000001427.
- Alarhayem AQ, Myers JG, Dent D, Liao L, Muir M, Mueller D, Nicholson S, Cestero R, Johnson MC, Stewart R, et al. Time is the enemy: mortality in trauma patients with hemorrhage from torso injury occurs long before the “golden hour. Am J Surg. 2016;212(6):1101–5. doi:10.1016/j.amjsurg.2016.08.018.
- van Turenhout EC, Bossers SM, Loer SA, Giannakopoulos GF, Schwarte LA, Schober P. Pre-hospital transfusion of red blood cells. Part 1: a scoping review of current practice and transfusion triggers. Transfus Med. 2020;30(2):86–105. doi:10.1111/tme.12667.
- van Turenhout EC, Bossers SM, Loer SA, Giannakopoulos GF, Schwarte LA, Schober P. Pre-hospital transfusion of red blood cells. Part 2: a systematic review of treatment on outcomes. Transfus Med. 2020;30(2):106–133. doi:10.1111/tme.12659.
- Mena-Munoz J, Srivastava U, Martin-Gill C, Suffoletto B, Callaway CW, Guyette FX. Characteristics and outcomes of blood product transfusion during critical care transport. Prehosp Emerg Care. 2016;20(5):586–593. doi:10.3109/10903127.2016.1163447.
- McGinity AC, Zhu CS, Greebon L, Xenakis E, Waltman E, Epley E, Cobb D, Jonas R, Nicholson SE, Eastridge BJ, et al. Prehospital low-titer cold-stored whole blood: philosophy for ubiquitous utilization of O-positive product for emergency use in hemorrhage to injury. J Trauma Acute Care Surg. 2018;84(6S Suppl 1):S115–S119. doi:10.1097/TA.0000000000001905.
- Holcomb JB, del Junco DJ, Fox EE, Wade CE, Cohen MJ, Schreiber MA, Alarcon LH, Bai Y, Brasel KJ, Bulger EM, et al. The prospective, observational, multicenter, major trauma transfusion (PROMMTT) study: comparative effectiveness of a time -varying treatment with competing risks. JAMA Surg. 2013;148(2):127–36. doi:10.1001/2013.jamasurg.387.
- Holcomb JB, Donathan DP, Cotton BA, Del Junco DJ, Brown G, Wenckstern T v, Podbielski JM, Camp EA, Hobbs R, Bai Y, et al. Prehospital transfusion of plasma and red blood cells in trauma patients. Prehosp Emerg Care. 2015;19(1):1–‐9. doi:10.3109/10903127.2014.923077.
- Pusateri AE, Moore EE, Moore HB, Le TD, Guyette FX, Chapman MP, Sauaia A, Ghasabyan A, Chandler J, McVaney K, et al. Association of prehospital plasma transfusion with survival in trauma patients with hemorrhagic shock when transport times are longer than 20 minutes: a post hoc analysis of the PAMPer and COMBAT trials. JAMA Surg. 2020;155(2):e195085. doi:10.1001/jamasurg.2019.5085.
- Holcomb JB, Tilley BC, Baraniuk S, Fox EE, Wade CE, Podbielski JM, del Junco DJ, Brasel KJ, Bulger EM, Callcut RA, et al. Transfusion of plasma, platelets, and red blood cells in a 1:1:1 vs a 1:1:2 ratio and mortality in patients with severe trauma: the PROPPR randomized clinical trial. JAMA. 2015;313(5):471–‐82. doi:10.1001/jama.2015.12.
- Sperry JL, Guyette FX, Brown JB, Yazer MH, Triulzi DJ, Early-Young BJ, Adams PW, Daley BJ, Miller RS, Harbrecht BG, et al. Prehospital plasma during air medical transport in trauma patients at risk for hemorrhagic shock. N Engl J Med. 2018;379(4):315–26. doi:10.1056/NEJMoa1802345.
- Brown JB, Guyette FX, Neal MD, Claridge JA, Daley BJ, Harbrecht BG, Miller RS, Phelan HA, Adams PW, Early BJ, et al. Taking the blood bank to the field: the design and rationale of the prehospital air medical plasma (PAMPer) trial. Prehosp Emerg Care. 2015;19(3):343–50. doi:10.3109/10903127.2014.995851.
- Moore HB, Tessmer MT, Moore EE, Sperry JL, Cohen MJ, Chapman MP, Pusateri AE, Guyette FX, Brown JB, Neal MD, et al. Forgot calcium? Admission ionized-calcium in two civilian randomized controlled trials of prehospital plasmas for traumatic hemorrhagic shock. J Trauma Acute Care Surg. 2020;88(5):588–96. doi:10.1097/TA.0000000000002614.
- Shlaifer A, Siman-Tov M, Radomislensky I, Peleg K, Shina A, Baruch EN, Glassberg E, Yitzhak A. Prehospital administration of freeze‐dried plasma, is it the solution for trauma casualties? J Trauma Acute Care Surg. 2017;83(4):675–82. doi:10.1097/TA.0000000000001569.
- Sunde GA, Vikenes B, Strandenes G, Flo K-C, Hervig TA, Kristoffersen EK, Heltne J-K. Freeze dried plasma and fresh red blood cells for civilian prehospital hemorrhagic shock resuscitation. J Trauma Acute Care Surg. 2015;78(6 Suppl 1):S26–S30. doi:10.1097/TA.0000000000000633.
- Peralta MR, Chowdary P. The use of new procoagulants in blunt and penetrating trauma. Curr Opin Anaesthesiol. 2019;32(2):200–5. doi:10.1097/ACO.0000000000000696.
- El-Menyar A, Sathian B, Asim M, Latifi R, Al-Thani H. Efficacy of prehospital administration of tranexamic acid in trauma patients: a meta-analysis of the randomized controlled trials. Am J Emerg Med. 2018;36(6):1079–1087. doi:10.1016/j.ajem.2018.03.033.
- Huebner BR, Dorlac WC, Cribari C. Transexamic acid use in prehospital uncontrolled hemorrhage. Wilderness Environ Med. 2017;28(2S):S50–S60. doi:10.1016/j.wem.2016.12.006.
- Moore EE, Moore HB, Kornblith LZ, Neal MD, Hoffman M, Mutch NJ, Schöchl H, Hunt BJ, Sauaia A. Trauma-induced coagulopathy. Nat Rev Dis Primers. 2021;7(1):30. doi:10.1038/s41572-021-00264-3.
- Guyette FX, Brown JB, Sperry JL. Tranexamic acid during prehospital transport in patients at risk for hemorrhage after injury. JAMA Surg. 2021;156(7):688. doi:10.1001/jamasurg.2021.0262.
- Bennett BL, Giesbrect G, Zafren K, Christensen R, Littlejohn LF, Drew B, Cap AP, Miles EA, Butler FK, Holcomb JB, et al. Management of hypothermia in tactical combat casualty care: TCCC guideline proposed change 20-01 (June 2020). J Spec Oper Med. 2020;20(3):21. doi:10.55460/QQ9R-RR8A.
- Lendrum R, Perkins Z, Chana M, Marsden M, Davenport R, Grier G, Sadek S, Davies G. Pre-hospital resuscitative endovascular balloon occlusion of the aorta (REBOA) for exsanguinating pelvic hemorrhage. Resuscitation. 2019;135:6–13. doi:10.1016/j.resuscitation.2018.12.018.
- Butler FK, Holcomb JB, Shackelford SA, Barbabella S, Bailey JA, Baker JB, Cap AP, Conklin CC, Cunningham CW, Davis MS, et al. Advanced resuscitative care in tactical combat casualty care: TCCC guidelines. J Spec Oper Med. 2018;18(4):37–55. doi:10.55460/YJB8-ZC0Y.
- Schweigkofler U, Wohlrath B, Trentzsch H, Horas K, Hoffmann R, Wincheringer D. Is there any benefit in the pre-hospital application of pelvic binders in patients with suspected pelvic injuries? Eur J Trauma Emerg Surg. 2021;47(2):493–8. doi:10.1007/s00068-019-01239-6.
- Cross AM, Davis C, Penn-Barwell J, Taylor DM, De Mello WF, Matthews JJ. The incidence of pelvic fractures with traumatic lower limb amputation in modern warfare due to improvised explosive devices. J R Nav Med Serv. 2014;100(2):152–156. doi:10.1136/jrnms-100-152.
- Coccolini F, Stahel PF, Montori G, Biffl W, Horer TM, Catena F, Kluger Y, Moore EE, Peitzman AB, Ivatury R, et al. Pelvic trauma: WSES classification and guidelines. World J Emerg Surg. 2017;12:5. doi:10.1186/s13017-017-0117-6.
- Shackelford SA, Hammesfahr R, Morissette DM, Montgomery HR, Kerr W, Broussard M, Bennett BL, Dorlac WC, Bree S, Butler FK, et al. The Use of Pelvic Binders in Tactical Combat Casualty Care. J Spec Oper Med. 2017;17(1):135–147. doi:10.55460/1WLZ-MKW4.
- Fu C-Y, Wu Y-T, Liao C-H, Kang S-C, Wang S-Y, Hsu Y-P, Lin B-C, Yuan K-C, Kuo I-M, Ouyang C-H, et al. Pelvic circumferential compression devices benefit patients with pelvic fractures who need transfers. Am J Emerg Med. 2013;31(10):1432–1436. doi:10.1016/j.ajem.2013.06.044.
- Advanced Trauma Life Support. Student Course Manual (10th Edition). Chicago (IL): American College of Surgeons. 2018.
- Pediatric Advanced Life Support. Dallas (TX): American Heart Association. 2020.
- Pierrie SN, Seymour RB, Wally MK, Studnek J, Infinger A, Hsu JR. Pilot randomized trial of pre-hospital advanced therapies for the control of hemorrhage (PATCH) using pelvic binders. Am J Emerg Med. 2021;42:43–48. doi:10.1016/j.ajem.2020.12.082.
- Cunningham A, Auerbach M, Cicero M, Jafri M. Tourniquet usage in prehospital care and resuscitation of pediatric trauma patients—Pediatric Trauma Society position statement. J Trauma Acute Care Surg. 2018;85(4):665–667. doi:10.1097/TA.0000000000001839.
- Bobko JP, Lai TT, Smith R, Shapiro G, Baldridge T, Callaway DW. Tactical emergency casualty care? Pediatric appendix: novel guidelines for the care of the pediatric casualty in the high-threat, prehospital environment. J Spec Oper Med. 2013;13(4):94–107. doi:10.55460/EF77-LDYW.
- Harcke HT, Lawrence LL, Gripp EW, Kecskemethy HH, Kruse RW, Murphy SG. Adult tourniquet for use in school-age emergencies. Pediatrics. 2019;143(6):e20183447. doi:10.1542/peds.2018-3447.
- Kelly JR, Levy MJ, Reyes J, Anders J. Effectiveness of the combat application tourniquet for arterial occlusion in young children. J Trauma Acute Care Surg. 2020;88(5):644–647. doi:10.1097/TA.0000000000002594.
- Charlton NP, Goolsby CA, Zideman DA, Maconochie IK, Morley PT, Singletary EM. Appropriate tourniquet types in the pediatric population: a systematic review. Cureus. 2021;13(4):e14474. doi:10.7759/cureus.14474.