ABSTRACT
Objective
Paramedics work in a complex, unpredictable environment, subject to many external stressors including critically unwell patients, dangerous driving conditions, and prolonged shift work. Paramedic fatigue from these and other occupational demands is well documented. Ambulance services attempt to safeguard paramedics from fatigue using internal policies or procedures – a type of Fatigue Risk Management Systems (FRMSs). This study reviews ambulance service fatigue frameworks to understand the current situation in fatigue management in paramedicine, and to identify fatigue monitoring tools, strategies, and other components of these frameworks that are designed to protect personnel.
Methods
This study involved a qualitative document thematic content analysis. All eleven statutory ambulance services across Australia, New Zealand, and Papua New Guinea, represented by the Council of Ambulance Authorities, were contacted and invited to participate. Fatigue frameworks were collated and entered into NVivo where data extraction occurred through three a priori areas (fatigue, fatigue mitigation tools & fatigue management).
Results
Nine of the eleven ambulance services provided fatigue documentation, with one declining to participate, and one did not respond to invitations. Through thematic analysis and abstraction, seven themes were identified: fatigue definition, consequences of fatigue, sources of fatigue, signs and symptoms of fatigue, fatigue-related incidents, fatigue monitoring tools, and fatigue mitigation. There was also poor alignment between provided frameworks and established FRMSs components.
Conclusion
Our findings provide an initial insight into existing ambulance service fatigue frameworks across Australia, New Zealand, and Papua New Guinea. The many inconsistencies in frameworks between ambulance services highlight an opportunity to develop a more consistent, collaborative approach that follows evidence based FRMSs guidelines.
Disclaimer
As a service to authors and researchers we are providing this version of an accepted manuscript (AM). Copyediting, typesetting, and review of the resulting proofs will be undertaken on this manuscript before final publication of the Version of Record (VoR). During production and pre-press, errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal relate to these versions also.INTRODUCTION
Paramedics work tirelessly across a plethora of settings to deliver evidence-based medical care to those in need 24 hours a day, 7 days a week. The irregular, often urgent, and unpredictable nature of ambulance work (i.e., incidents attended, workload, shift length) has the potential to have a negative impact on wellbeing (1). Wellbeing includes the consideration of one’s emotional, social, physical, mental, and spiritual health (2). Fatigue is a key determinant in wellbeing and is highly prevalent in paramedics (3, 4). Indeed, Kearney et al. (5) found fatigue diminished one’s ability to focus while driving in an emergency response scenario and fatigue was identified as being a possible contributor to fatal and non-fatal transport-related injuries. This evidence highlights the need to challenge current practice, to better understand fatigue management strategies for paramedics and enhance their health and safety, and that of their patients.
Fatigue is a multifactorial phenomenon that has no single accepted definition; however, it is commonly differentiated between acute and chronic fatigue (6). The International Civil Aviation Organization (ICAO) (7, p.1), often renowned for excellence in fatigue research, defines fatigue as ‘a physiological state of reduced mental or physical performance capability resulting from sleep loss or extended wakefulness, circadian phase, or workload that can impair a crew member’s alertness and ability to safety operate … or perform safety-related duties’. Fatigue can occur from manual tasking, shift work, sleep disorders, or operating a vehicle (8). In the paramedicine context, clinicians are at a heightened risk of fatigue due to many of the aforementioned factors being prevalent in their work, with significant consequences to ones’ driving abilities, alertness, cognition, memory, and clinical reasoning (9).
Fatigue Risk Management Systems (FRMSs) are an approach used in many workplaces to identify and manage fatigue-related risks (10). The framework fundamentally identifies levels of risk, as opposed to compliance with legislation (i.e., a paramedic’s roster may meet maximum work and rest rules, however fatigue may still prevail). Corresponding risk-based control measures (e.g., naps, mandatory stand down periods etc.) can then be implemented to match the likelihood of fatigue as determined by assessments, monitoring tools, and/or sleep history (10). The overall approach to FRMSs is well established and many components within FRMSs are shown to reduce fatigue and enhance safety within the workplace (10), yet the selection and implementation of these components may vary widely from one organization to the next.
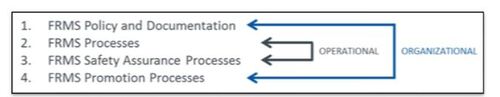
The International Civil Aviation Organization (ICAO) has conducted extensive research into FRMSs and has developed an independent program to assist in the safeguarding of the aviation industry (11). This program explains how to construct and test the effectiveness of FRMSs and as such, represents a benchmark in light of limited literature from other industries. The ICAO FRMSs consists of four components: FRMS Policy and Documentation, FRMS Processes, FRMS Safety Assurance Processes, and FRMS Promotion Processes (11) (see Figure 1). The four components are sub-divided into two streams (11). The organizational stream includes FRMS Policy and Documentation which refers to the organizational arrangements that support operational activities (i.e., responsibility of implementation, FRMSs objectives, and training/ schedules and review opportunities) and FRMS Safety Assurance Processes monitor and evaluate the holistic functionality of the FRMSs (i.e., monitors for acceptable level of fatigue and monitors changes in operational dynamics) (11). Whereas the operational stream includes FRMS Processes which refer to the day-to-day functionality in the operational environment (i.e., monitoring and evaluation of fatigue levels, risk/ hazard assessment, and mitigation opportunities) and FRMS Promotion Processes refers to the communication to and training of operational personnel (11).
To date, there is no comparative analysis of ambulance fatigue frameworks in the Australasian region. This study aims to report on the current situation of fatigue frameworks in ambulance services and identify fatigue monitoring tools, strategies, and other fatigue components that are being used by ambulance services. It will also provide a high-level comparison of each service’s fatigue frameworks to an established FRMSs components.
METHODS
Setting
All Australasian (Australia, New Zealand & Papua New Guinea) statutory ambulance services (n = 11) were invited to participate in this study due to their affiliation with the Council of Ambulance Authorities (CAA) – the representative body for ambulance services in this region (12). Within the Australasian setting, ambulance as well as most other emergency services operate from separate state- and territory-based organizations, (i.e., paramedics are employed by state- or territory-based ambulance organizations, and are required to hold a tertiary level qualification) (13-14).
Australasian ambulance services employ over 28,000 personnel (15, 16), responding to over 4.2 million requests for service annually via road ambulance, aeromedical services and telehealth (17). EMS clinicians typically work condensed hours involving rotating shifts that last anywhere between 10-14 hours (18), and at times, these shifts can be extended due to reasonable compulsory overtime (18, 19).
Qualitative design
The study applied a deductive, descriptive, conceptual design with a document analysis approach (20) to investigate similarities and differences among fatigue policies, fatigue procedures, and fatigue management frameworks among participating ambulance services. Document analysis uses data extraction and review processes from varying ‘documents’ to expand current knowledge in the study area, in line with the study aims (21). A positivist lens was used for its objectivity and so quantifiable data could be reported as per the study aims. This study is reported as per the Standards for Reporting Qualitative Research (SRQR) (22).
Dalglish et al. (20) propose a 4-step methodology to document analysis, using the READ approach. Step one in this approach involves collecting and collating the appropriate materials required for the document analysis (20). Typically, this can be a complex process that includes sourcing, filtering and deciding on inclusion/exclusion criteria of documents (i.e., official documents, grey literature, media and scholarly work). In the current study, participating ambulance services were requested to provide all documentation, such as policies, procedures, frameworks (including tools/tests), and work instructions, relating to fatigue risk management of paramedics within their service at the time of data collection. Therefore, much of the collecting and collating in this study was pre-determined by the documents provided by the ambulance services, which are referred to as ‘frameworks’ from hereon. The inclusion criteria for frameworks were: ‘documentation from an Australasian ambulance service’ and currently ‘in use’ in the service. Data collection occurred between September and November 2022.
Step two in the READ approach includes the extraction of data (20). In the current study, this step involved uploading the frameworks to NVivo for content data extraction. Data was extracted from each framework using open coding based on the following three a priori areas: fatigue, fatigue mitigation tools, and fatigue management. Data extraction for one ambulance service framework was initially performed independently by two researchers (MF and AL). Both researchers established a collaborative codebook after discussing similarities and differences between their evaluations. One researcher (MF) then proceeded with data extraction of the remaining ambulance service frameworks and met with the other researcher (AL) to review data extracted.
Step three of the READ approach is the analysis phase (20). Analysis involves the review and thematic grouping of codes through the abstraction process. Abstraction is a qualitative research method whereby subject elements are grouped, as per their classification, into a higher level/ theme (23). The more times abstraction occurs on a data set, the further the ‘distance’ or ‘truthfulness’ from the original data is – thus reducing rigor. In this instance, abstraction occurred once. Conceptual extracted data was analyzed within the themes and reported upon in frequencies (quantitative) within this paper.
Step four of the READ approach is the distillation of the findings (20) whereby a reflection occurs on the analytic process. The distillation process allows researchers to take a ‘big picture’ approach to the results of the study and ensure they have been rigorous, measurable, repeatable, and saturated, where possible.
Member checking
Prior to publication, each of the participating ambulance services were provided an opportunity to review the findings to ensure the frameworks provided were interpreted accurately by the research team. To protect the intellectual property and anonymity of ambulance services participating in this study, none of the ambulance services are specifically named throughout the manuscript, and where possible, data is reported in aggregate format. These conditions were agreed upon with the ambulance services prior to data collection.
Ethics
Consultation with the Human Research Ethics Committee at the institution where this work was completed, deemed that ethics approval was not required for the current study as no individual information was gathered.
Researcher reflexivity
As a proficient paramedic of 8 years working for an Australasian state-based ambulance service across metropolitan, regional and remote settings, and currently enrolled in a Doctor of Philosophy, the lead researcher has the necessary experience to research fatigue in paramedicine. As a paramedic, he has experienced and applied fatigue frameworks during his practice and holds an in-depth understanding of the barriers and enables to contemporary paramedic fatigue management. Furthermore, he currently serves on an employer-based committee to review and enhance current fatigue policy and procedures. This, when considered with his experience, skills and training as a paramedic, has influenced his perspectives on fatigue mitigation and management, and his drive to better support front-line healthcare professionals.
The supporting research team consists of three academics with backgrounds in occupational therapy (AL), psychology (AW), and human movement (K-AB), all of whom have research interests and experience in fatigue, sleep, research design, stress, shift workers and vulnerable/high-risk population groups. They have extensive research experience in both qualitative and quantitative realms, and each bring different areas of expertise to the current study.
RESULTS
Nine (81.8%) of the 11 services invited submitted documents related to fatigue management. These varied in length (one paragraph to 17 pages) and age (2-12 years since originally adopted and 0-9 years since updated). Although the scope of each framework varied; however, fatigue definitions, fatigue etiology/ signs and symptoms, procedures to escalate concerns, and fatigue monitoring tools (if present) were consistent.
Services provided fatigue documentation in the form of policies, or procedures – or both. In total, there was one informal work instruction (a section from a manager’s email), six policies, and six procedures. Typically, policies included the rules or expectations of paramedics, whereas the procedures provided a set of instructions or processes to follow to be compliant with the policy. Over half (n = 6) of the frameworks were past their annual or bi-annual review date, one did not have a review date, and one exceeded their review date by more than five years. Three services advised that their current frameworks were under review and in the process of being revised at the time of data collection. Finally, two frameworks indicate that their policy is all inclusive as is, whereas others have an evidence-based information section to support their policy and/or assist paramedics when identifying fatigue.
Framework comparison
Overall, the fatigue frameworks of Australasian ambulance services have a poor alignment to the ICAO FRMSs guidelines, which is a benchmark in fatigue management and mitigation. One service did not follow any of the components, while two services followed all components for two themes. Overarchingly, ambulance service frameworks most closely aligned to the ICAO guidelines in the ‘FRMS Policy and Documentation’ component.
Fatigue definition
Fatigue was defined in the frameworks as mental (n = 5), physical (n = 5), and emotional (n = 2) exertion that impairs alertness and affects one’s ability to work safely (n = 5) or normally (n = 3). Fatigue was also described as a subjective and multisensory experience (n = 2) that reduces mental and physical performance (n = 4) or where physical and mental limits are reached/exceeded (n = 3), resulting from sleep loss/inadequate restorative sleep (n = 4), and/or extended periods of wakefulness (n = 3). Two ambulance services indicated that fatigue was a state or feeling of tiredness and exhaustion, while two other services stated fatigue was more than ‘just tired’ or drowsy feelings. Some services (n = 4) mentioned circadian rhythms in their definition of fatigue but did not discuss or elaborate on this further.
Consequences of fatigue
Consequences of fatigue were identified in eight of the frameworks. Decreased reaction time and impaired decision-making ability were the most common consequences of fatigue (n = 4), followed by impaired coordination, inability to assess and respond to risks and hazards, reduced vigilance, and an increase in incidents and injuries (n = 3). Further, poor judgement and memory, concentration difficulties, becoming easily distracted, and less effective interpersonal communication were also mentioned (n = 2). Inability to recall a sequence of events, mood fluctuations, reduced visual perception, short periods of involuntary sleep and impaired fitness for work were the least prevalent consequences of fatigue mentioned in the frameworks (n = 1).
Sources of fatigue
Three frameworks acknowledged sources of fatigue in ambulance personnel and separated them into two categories, work-related and personal factors, as a part of their risk mitigation. In these frameworks, multiple work-related sources of fatigue were highlighted, including shift work, long hours, physically and mentally demanding work, exposure to trauma, workload (both high or low), frequency of breaks, stressful situations, and uncontrolled work environments. Individual or personal factors outlined in these three frameworks included the quantity and quality of rest obtained prior to a work shift, sleep disorders, family commitments, second jobs, study, use of any mind-altering substance (e.g., alcohol, medications, and illicit substances), and frequency and timing of food/drink. Emotional stressors were also listed, although none of the frameworks specifically stated if this should be considered a personal stressor.
Signs and symptoms of fatigue
Ambulance services listed reduced visual perception, slow reaction times (n = 5), microsleeps, yawning, poor hand-eye coordination, and irritability (n = 4) as the mental and physical signs of fatigue. The act of falling asleep or a desire to sleep, impatience, increase in risk taking behavior, and difficulty concentrating (n = 3) were also common signs and symptoms of fatigue that were highlighted in the included frameworks. Additional signs and symptoms only mentioned in one of the frameworks included not reacting to safety-critical alerts or information in an acceptable timeframe, lapses of attention during safety-critical activities or general limited attention span, slowed reflexes, increased lethargy, speech difficulties, head nodding, impaired judgement, difficulty problem solving, amotivation, difficulty keeping eyes open, not feeling refreshed post-sleep, and drowsiness.
Fatigue-related incidents
In five of the frameworks there was a requirement that paramedics complete a report when fatigue was determined to be a contributing factor to an incident, including their fatigue score, if present (see Fatigue Monitoring Tools). The report is completed via the relevant safety information system at the paramedic’s earliest opportunity. Further, a safety report is also required when paramedics generate a high fatigue score, which is then discussed with the paramedic’s relevant manager at the next possible opportunity. Additionally, four (of the five) ambulance services indicated that a Human Resources (HR) team member reviews all fatigue-related incidents to establish contributing factors and see if any changes to policy or procedure can be implemented to prevent a recurrence.
Fatigue monitoring tools
Five ambulance services described the use of tools to assess fatigue levels in paramedics at varying points throughout a shift, which enables the implementation of fatigue mitigation strategies. Across these five services, three different tools were reported, with some ambulance services using more than one tool. These tools included the Prior Sleep and Wake Model (PSWM), the Fatigue Self-Assessment Tool (FSAT), and a ‘service-specific’ self-assessment of fatigue.
As described in the relevant frameworks, the PSWM is a predictive fatigue model that accounts for sleep obtained in the preceding 48 hours before shift commencement and current time awake (see Supplemental File Appendix 1 for additional information). Three statutory services indicate this tool ‘should’ be used at the commencement of each shift, whereas one statutory service states employees ‘must’ use it. The PSWM provides a total fatigue score between 0 and 16, and based on this score, each service has pre-determined tiers which indicate varying degrees of fatigue risk (see Supplemental File Appendix 1). Each tier results in a variety of escalation measures, up to and including immediate stand-down of the paramedic. One ambulance service was using the PSWM for paramedics that solely undertake on-call duties, whereas three services use the PSWM in their framework to determine fatigue risk for all paramedics, including employees that work rotating rosters and on-call.
The FSAT, is described in the frameworks as a subjective, 1-minute self-assessment tool, completed via pen and paper or a smartphone application. The FSAT assesses fatigue within an operational context at a given point in time. In the two services using this tool, personnel could use the FSAT at any time they were concerned about their fatigue level throughout a shift, which allowed for implementation of appropriate mitigation strategies based on the level of fatigue risk identified. Completion of the FSAT was not, however, compulsory in either of the ambulance services that used the tool as part of their fatigue frameworks. After completion of the FSAT, paramedics are categorized into a predetermined risk tier (see Supplemental File Appendix 2).
Finally, a service-specific self-assessment tool was used, which is a non-validated yes/no questionnaire that assists paramedics in personal decision-making surrounding fatigue risks. The tool was used as a secondary level measure following completion of the PSWM. Specifically, if a paramedic feels the PSWM has insufficiently recorded their fatigue, they are encouraged to self-identify subjective fatigue signs and symptoms via the service-specific self-assessment fatigue tool, which then promotes discussion with the on-shift supervisor.
Fatigue mitigation
Fatigue mitigation strategies were evident across most ambulance service frameworks (n = 8). Half of the services with fatigue mitigation strategies highlighted that fatigue management is a shared responsibility between the employee and employer, and supportive communication between both parties was required for safety. As reported in the relevant frameworks, mitigation strategies can be divided into four distinct categories, which include the planning phase of a shift, immediately pre-shift, during a shift and post-shift.
Ambulance services used preparatory strategies such as roster design and education to prevent or reduce fatigue risks from occurring in paramedics when working shift work. For instance, a bio-mathematical tool and employee feedback could be used for actual or planned rosters to reduce fatigue risks whilst maintaining service delivery. Fatigue training for new paramedics was mandated in two ambulance services. These same two services discussed the use of annual refresher training, one which detailed a minimum of one hour a year, including but not limited to education modules regarding duty of care to self and others in relation to fatigue, the human body clock, personal fatigue indicators, health, diet and exercise, and the effects of drugs and alcohol.
Pre-shift fatigue management strategies, highlighted by other services included undertaking moderate exercise before work, walking around during breaks where possible, promoting healthy sleep habits using dark curtains, a cool bedroom, considering ear plugs, and eating light and healthy food. Finally, some ambulance service fatigue mitigation strategies suggested paramedics should plan domestic duties around shift schedules and inform friends and family of their schedule so that the paramedic can be accommodated within social gatherings.
Fatigue strategies for implementation during a shift were fairly consistent across frameworks and included: reallocation of position (alternating between driver and attending clinician), crew allocation (to a lower/higher workload area) or configuration (e.g., if both paramedics are fatigued on an ambulance, swapping them with a non-fatigued crew) (n = 3), caffeinated beverages or nutritional meal breaks (n = 2), increased supervision/monitoring of alertness (n = 3), a restorative fatigue (sleep) break (n = 3), and conveyance to/from the ambulance station via a paid transportation agent (i.e., taxi) (n = 2). Additionally, one service implements a low acuity workload dispatch (n = 1) to address on duty fatigue, and another employs a strategy where communication staff (dispatch) make regular contact with operational staff working on-road during the following circumstances: a paramedic is undertaking long transport legs, a paramedic is at high fatigue risk, and a paramedic is working between the hours of 0000 and 0600. To ensure appropriate fatigue management and allow paramedics to finish on time, a service outlined how they only dispatch paramedic crews to the three highest acuity job categories within 30 minutes of shift termination, and the two highest acuity job categories in the last 15 minutes of shift termination with immediate back-up requested.
To prevent fatigue from culminating post-shift, four ambulance services dictate minimum periods of rest between rostered shifts in their frameworks. Specifically, two services require a minimum 10-hour rest period, whereas the other two services require eight hours of rest. Of these, two services also have frameworks which control the maximum number of hours a paramedic can work within a given extended time frame. In one of these frameworks, no more than 70-hours can be worked by paramedics within a seven-day period, while the other states that a maximum of 16-hours can be worked within a 24-hour period, or a maximum of 32 hours overtime within a pay fortnight. Finally, two frameworks state that if an employee is stood down due to fatigue from personal sources, then sick leave will be taken. Conversely, two ambulance services mandate that sick leave is taken whether the fatigue is from a work or non-work source.
DISCUSSION
This study aimed to understand the current fatigue management approaches used by Australasian ambulance services, identify fatigue monitoring tools, and safeguards used by services to protect ambulance personnel. Overall frameworks varied greatly in content and depth, and the approach to fatigue management was not consistent between services. There was also a poor alignment to established FRMSs guidelines.
This paper demonstrates that within Australasian ambulance services there is variation in the definition of fatigue through all frameworks, albeit similar in essence. However, only half the included frameworks supported the mutual responsibility of fatigue management. Literature generally agrees that workplace fatigue results from three intertwined factors; sleep homeostasis, core work processes, and circadian rhythm (8) which are all controllable and uncontrollable factors for the employee, employer, and regulator. As previously mentioned, there is no single agreed upon definition of fatigue within the literature given its significant variation and interpretation among industrial groups, however, fatigue management is consistently supported throughout the literature as a mutually shared (employee and employer) responsibility (24). Ambulance services are turning their research towards paramedic health and psychosocial wellbeing; therefore, an agreed definition of fatigue would be required to guide targeted interventions. This could occur through future consolidation of research.
Previous research has highlighted the various sources of fatigue in paramedics (25, 26), some of which were identified within the ambulance service fatigue frameworks analyzed in this study. Rotating shift work, particularly night work, was the most frequently cited source of fatigue within the frameworks reviewed, in addition to shift extensions, reduced or no access to breaks, extended work hours, environmental constraints (e.g., temperature, vibrations, noise levels) and inadequate staffing. Each of these factors have been shown to contribute to fatigue in paramedics (19, 25), hence their inclusion in FRMSs is warranted. Given rotating shift work, shift extensions, and access to meal breaks were the most cited fatigue risk factors, further research should be completed to better understand the lived experience of paramedics.
Fatigue monitoring is a contemporary approach to FRMSs, assisting employee safety whilst simultaneously optimizing performance and productivity (10, 11, 27, 29). Both objective and subjective fatigue monitoring tools can be implemented, and aim to provide an assessment of fatigue, assisting in the decision-making process of an employee’s fitness-for-duty. In this study, just over half the frameworks reviewed included the use of a fatigue monitoring tool, four of which frameworks used the PSWM. The authors recommend, in conjunction with two recent studies, (28, 29), that each service has a validated tool to help start the assessment of fatigue for both patient and paramedic safety.
Sparrow et al. (30) studied truck drivers over two consecutive duty cycles, comparing PSWM results against the gold standard tool for detecting fatigue, the Psychomotor Vigilance Test (PVT), which assesses vigilant attention through reaction time on an electronic screen (31). Compared to the PVT, the authors found the PSWM demonstrated poor specificity and low sensitivity to differentiate safe from unsafe fatigue levels in truck drivers (30). Furthermore, nurses who worked night shifts and averaged 5.74 hours (1.3 ± hours) of sleep were found to have significantly poorer outcomes on the PVT, compared to day shift working nurses (32). Given one criterion, out of three, in the PSWM is reliant on personnel having >5 hours sleep in the preceding 24 hours for a risk profile to be generated, these studies challenge the appropriateness of this minimum rule.
Although the PSWM is used widely as part of FRMSs in different industries, further research should be directed into the appropriateness of using the PSWM in prehospital settings, and whether there are alternative tools, such as the PVT, Karolinska Sleepiness Scale, Epworth Sleepiness Scale or Stanford Sleepiness Scale (31, 33), which may be more accurate in determining fitness-for-duty based on fatigue. To the authors’ knowledge, no such study exists currently. In addition to the PSWM, two ambulance services used the FSAT, however no research has examined the accuracy of this tool in either paramedics or other health care occupations, thus further research should be directed towards validating this tool for use by ambulance services.
Ambulance services were found to employ a range of strategies to mitigate fatigue risks in their workforce. In the frameworks reviewed, caffeine, rotating work positions and increased supervision were widely used to assist in maintaining performance and alertness on shift, however, there is varying levels of evidence supporting such strategies (34). For instance, caffeine was found to be one of the most prevalent fatigue management strategies used in shift workers (35). Specifically, older research in defense personnel found >50% of people consumed caffeine to induce wakefulness (36, 37), while Parry et al. (38) found short-term caffeine use to potentially increase cognitive functioning to that of rested levels. Furthermore, a recent recommendation suggested EMS providers should have access to caffeine to help manage fatigue when required (28, 29). Conversely, there is limited research investigating if task rotation (driver vs attendant roles) and increased supervision of workers’ alertness levels influence fatigue in paramedics. While caffeine is supported in the literature as an effective fatigue management strategy to induce wakefulness and cognitive functioning, further research should be directed to the plausibility of task rotation and supervision within the emergency setting.
Strategic napping was also highlighted as a mitigation strategy by ambulance services. Although limited research has investigated the impact of napping in paramedics, it is commonly used in other safety-sensitive occupations, such as aviation, where it is proven to reduce subjective sleepiness, sleep debt, and enhance key job functions for pilots whilst on duty (39). While some of the analyzed frameworks discuss the use of a restorative fatigue break or nap, they are solely described in the purpose of reactive rather than preventative fatigue management in paramedics. A recent review found improved cognitive performance after a mean 41.3-minute (28.3± min) nap early within a night shift when compared with a control group of non-nappers (40). Furthermore, a meta-analysis found paramedics experience decreased fatigue and improved work performance with scheduled naps during a shift (41). Given this evidence supporting the prophylactic effect of napping, ambulance services could consider integrating the use of short napping as a preventative fatigue mitigation strategy in their fatigue framework. This is further supported by Patterson et al. (28) recommendation, supporting napping in EMS shifts, of extended duration (i.e., ≥ 12 hours) and overnight duty.
Education was identified as a preventive fatigue mitigation strategy in two of the reviewed frameworks, and further supported within the literature (28, 29, 42). Barger et al. (42) conducted a systematic review into the effects of fatigue training on safety, sleep, and fatigue in emergency medical service personnel and shift workers, finding education enhanced safety and health outcomes in clinicians. Specifically, fatigue training was found to reduce burnout rates and stress while improving acute fatigue scores, and personal and patient safety (42). In this review, sleep quality was also enhanced in five of the reviewed studies examining the impact of fatigue training (42). While only two of the ambulance services implemented fatigue training as part of their fatigue frameworks, it is possible additional services involved in this study had other sorts of education available to employees that were not captured as part of their formal fatigue frameworks. Notwithstanding this, given the strong evidence supporting the positive impact of fatigue education and training on health and safety, ambulance services should consider wider implementation of this strategy to reduce fatigue.
LIMITATIONS
This comparative analysis was based on fatigue frameworks provided by statutory ambulance services in Australasia. Nine out of the eleven possible services provided fatigue frameworks for this study; thus, our findings may not be generalizable to all ambulance services in this region. Furthermore, some frameworks referred to other organizational documents that were unattainable at the time of the study, which may limit the accuracy and thoroughness of our analysis. Additionally, at the time of data collection, at least three of the frameworks provided were under review, which may further limit the accuracy of the findings should there be any significant changes to these frameworks following the review process. Furthermore, the analysis of the frameworks was by conducted by two researchers (MF and AL), thus some nuances and/or service specific language may not have been interpreted as intended. To help mitigate this limitation, each participating ambulance service had the opportunity to read and comment on the findings prior to publication to ensure a) the level of agreed anonymity was satisfactory, and b) the interpretation of the framework was accurate.
CONCLUSIONS
Paramedic work can be unpredictable in nature and require the performance of high-acuity lifesaving skills that demand high levels of alertness, a rapid reaction to change, and the ability to perform in dangerous and uncontrolled environments. Ambulance services attempt to reduce fatigue and support their staff through fatigue frameworks. There are consistencies in Australasian ambulance services in the use of similar fatigue mitigation strategies and the application of fatigue monitoring tools. However, there are variances in the risk appetite of statutory ambulance services to fatigue risk, management of a fatigued employees, and as expected, fatigue definitions. It is clear further research is required to promote a consistent approach to fatigue management by ambulance services that support paramedic wellbeing, prevent fatigue, and improve clinical outcomes for patients.
ACKNOWLEDGEMENTS: The authors would like to acknowledge the ambulance services who participated in this study, who without, this study would not have been feasible.
DECLARATION OF INTEREST STATEMENT: One author (M.F.) works for the Queensland Ambulance Service, Australia, however all authors declare nil conflicts of interest.
Due to the nature of the research, due to privacy reasons, supporting data is not available.
DECLARATION OF GENERATIVE AI IN SCIENTIFIC WRITING:
The authors did not use a generative artificial intelligence (AI) tool or service to assist with preparation or editing of this work. The authors take full responsibility for the content of this publication.
Funding Sources: This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Disclosure statement: One author (M.F.) works for the Queensland Ambulance Service, Australia, however all authors declare nil conflicts of interest.
Table 1: Australasian ambulance service comparison to the ICAO FRMS benchmark
SupplementalFile_UPEC-2024-0177.R2.docx
Download MS Word (14.4 KB)REFERENCES
- Meadley B, Caldwell J, Perraton L, Bonham M, Wolkow AP, Smith K, Williams B, Bowles KA. The health and well-being of paramedics – A professional priority. Occ Med. 2020;70:149-151
- Wheeler B, Dippenaar E. Physiological and psychological components of paramedic wellbeing. Int Para Prac. 2020;10
- Khan WAA, Conduit R, Kennedy GA, Jackson ML. The relationship between shift work, sleep, and mental health among paramedics in Australia. Sleep Health. 2020;6:330-337
- Pyper Z, Paterson JL. Fatigue and mental health in Australian rural and regional ambulance personnel. Emer Med Aus. 2016;2:62-66
- Kearney J, Muir C, Smith K. Occupational injury among paramedics: a systematic review. Inj Prev, 2022;28:176-184
- Dawson D, Sprajcer M, Thomas M. How much sleep do you need? A comprehensive review of fatigue related impairments and the capacity to work or drive safely. Acc Anal Prev. 2021;151:1-13
- International Civil Aviation Organization (ICAO). Fatigue Management: Safety, Flight Operations. [accessed 2023 OCT 15] https://www.icao.int/NACC/Documents/eDOCS/FS/FS-Flyer_US-Letter_ANB-Fatigue-Management_2013-08-23.pdf
- Milia LD, Smolensky MH, Costa G, Howarth HD, Ohayon MM, Philip P. Demographic factors, fatigue, and driving accidents: An examination of the published literature. Acc Anal Prev. 2011;43:516-532
- Ramey S, MacQuarrie A, Cochrane A, McCann I, Johnston CW, Batt AM. Drowsy and Dangerous? Fatigue in Paramedics: an overview. Ir J of Para. 2019;4
- Sprajcer M, Thomas MJW, Sargent C, Crowther ME, Boivin DB, Wong IS, Smiley A, Dawson D. How effective are Fatigue Risk Management Systems (FRMS)? A review. Acc Anal Prev. 2022;165
- International Civil Aviation Organization (ICAO). Doc 9966: Manual for the Oversight of Fatigue Management Approaches, (2nd digital ed). [accessed 2023 OCT 10] https://www.icao.int/safety/fatiguemanagement/FRMS%20Tools/Doc%209966.FRMS.2016%20Edition.en.pdf
- Council of Ambulance Authorities (CAA). 2023 CAA Congress Partnering Prospectus. [accessed 2023 SEP 29] https://issuu.com/firstbycaa/docs/2024_congress_prospectus?e=43025687/98291461
- Howes LM, Goodman-Delahunty J. Career decisions by Australian police officers: a cross-section of perspectives on entering, staying in and leaving policing careers. Pol Prac Res. 2018;16:453-468
- Delardes B, Nehme E, Bowles KA, Chakraborty S, Cox S, Smith K. Characteristics and outcomes of patients referred to a general practitioner by Victorian paramedics. Pre Emer Care. 2024
- Kaunihera Manapou Paramedic Council. Paramedic Statistics (2024). [accessed 2024 JUN 15] https://paramediccouncil.org.nz/common/Uploaded%20files/Whakapapa/Website%20-%20Paramedic%20statistics.pdf
- Australian Health Practitioner Regulation Agency [AHPRA]. Paramedicine Board of Australia Registrant Data 2024. [accessed 2024 JUN 15] https://www.paramedicineboard.gov.au/News/Statistics.aspx
- Australian Government: Productivity Commission 2023. Report on Government Services-Ambulance Services. [accessed 2024 JUN 16] https://www.pc.gov.au/ongoing/report-on-government-services/2023/health/ambulance-services
- Patterson PD, Weaver MD, Hostler D, Guyette FX, Callaway CW, Yealy DM. The shift length, fatigue, and safety conundrum in EMS. Pre Emer C. 2012;16:572-576
- Paterson JL, Sofianopoulos S, Williams B. What paramedics think about when they think about fatigue: contributing factors. Emer Med Aus. 2014;26:139-144
- Dalglish SL, Khalid H, McMahon SA. Document analysis in health policy research: the READ approach. H Pol Plan. 2020;35:1424-1431
- Marriott SC, Grov EK, Gonzalez MT. Mental Health signs relevant for an assessment tool suitable for student and novice nurses a document analysis. Iss Men H Nur. 2021;43:638-649
- O’Brien B, Harris I, Beckman T, Reed D, Cook, D. Standards for Reporting Qualitative Research (SRQR): a synthesis of recommendations. Acc Med. 2014;89:1245-1251
- Lindgren BM, Lundman B, Graneheim UH. Abstraction and interpretation during the qualitative content analysis process. Int J Nurs Stud. 2020;108
- Gander P, Hartley L, Powell D, Cabon P, Hitchcock E, Mills A, Popkin S. Fatigue risk management: Organizational factors at the regulatory and industry/ company level. Acc Anal Prev. 2009;43:573-590
- Khan WAA, Jackson ML, Kennedy GA, Conduit R. A field investigation of the relationship between rotating shifts, sleep, mental health and physical activity of Australian Paramedics. Sci Rep. 2021;11:866
- Courtney JA, Francis AJP, Paxton SJ. Caring for the carers: fatigue, sleep, and mental health in Australian paramedic shift workers. Aus J Org Psy. 2021;2: 32-41
- Wolkow AP, Rajaratnam SMW, Anderson C, Howard ME, Mansfield D. Recommendations for current and future countermeasures against sleep disorders and sleep loss to improve road safety in Australia. Int Med J. 2019;49:1181-1184
- Patterson PD, Higgins JS, Van Dongen HPA, Buysse DJ, Thackery RW, Kupas DF, Becker DS, Dean BE, Lindbeck GH, Guyette FX, et al. Evidence-based guidelines for fatigue risk management in emergency medical services. Pre Hosp Care, 2018;22:89-101
- Martin-Gill C, Higgins JS, Van Dongen HPA, Buysse DJ, Thackery RW, Kupas DF, Becker DJ, Dean BE, Lindbeck GH, Guyette FX et al. Proposed performance measures and strategies for implementation of the fatigue risk management guidelines for emergency medical services. Pre Hosp Care, 2018;22:102-9
- Sparrow AR, Riedy S, Van Dongen HP. Fatigue Risk Management by Prior Sleep Wake Model (PSWM): Too easy to be reliable? Sleep, 2017;40
- Ferris M, Bowles KA, Bray M, Bosley E, Rajaratnam SMW, Wolkow AP. The impact of shift work schedules on PVT performance in naturalistic settings: a systematic review. Int Arc Occ & Env. 2021;94:1475-1494
- Ganesan S, Magee M, Stone JE, Mulhall MD, Collins A, Howard ME, Lockley SW, Rajaratnam SMW, Sletten TL. The impact of shift work on sleep, alertness and performance in healthcare workers. Sci Rep. 2019;9:4635.
- Patterson PD, Weaver MD, Fabio A, Teasley EM, Renn ML, Curtis BR, Matthews ME, Kroemer AJ, Xun X, Bizhanova Z et al. Reliability and validity of survey instruments to measure work-related fatigue in the emergency medical services setting: a systematic review. Pre Hosp Care. 2018;22;17-27
- Hartzler BM. Fatigue on the flight deck: The consequences of sleep loss and the benefits of napping. Acc Anal Prev. 2014;62:309-318
- Shriane AE, Ferguson SA, Jay SM, Vincent GE. Sleep hygiene in shift workers: a systematic literature review. S Med Rev. 2019;53
- Greenwood K, Rich W, James J. Sleep hygiene practices and sleep duration in rotating shift workers. Work Stre. 1995;9:2-3
- Brick C, Seely D, Palermo T. Association between sleep hygiene and sleep quality in medical students. Beh Slp Med. 2010;2:113-121
- Parry D, Iqbal S, Harrap I, Oeppen RS, Brennan PA. Caffeine: benefits and drawbacks for technical performance. Brit J of O Max Surg. 2023;61:198-201
- Rangan S, Riedy SM, Bassett R, Klinck ZA, Hagerty P, Schek E, Zhang Y, Hursh SR, Van Dongen HPA. Predictive and proactive fatigue risk management approaches in commercial aviation. J of Bio & Med Rhy. 2020;37:1479-1482
- Dutheil F, Bessonnat B, Pereira B, Baker JS, Moustafa F, Fantini ML, Mermillod M, Neval V. Napping and cognitive performance during night shifts: a systematic review and meta-analysis. Sleep. 2020;43:1-15
- Martin-Gill C, Verger LK, Moore C, Higgins JS, Teasley EM, Weiss PW, Condle JP, Flickinger KL, Coppler PJ, Sequeira DJ, et al. Effects of napping during shift work on sleepiness and performance in emergency medical services personnel and similar shift workers: a systematic review and meta-analysis. Pre Hosp Care. 2018;22:47-57
- Barger LK, Runyon MS, Renn ML, Moore CG, Weiss PM, Condle JP, Flickinger KL, Divecha AA, Coppler PJ, Sequeira DJ, et al. Effect of fatigue training on safety, fatigue, and sleep-in emergency medical services personnel and other shift workers: a systematic review and meta-analysis. Pre Hosp Care. 2018;22:58-68
- Dawson D, McCulloch K. Managing Fatigue: it’s about sleep’, Sleep Med Rev. 2005;9:365-380