ABSTRACT
Childhood trauma (CT) is associated with unhealthy lifestyle in adulthood. However, an in-depth exploration of how CT relates to multiple unhealthy lifestyle behaviors remains inconclusive. This study included 2968 adults from the Netherlands Study of Depression and Anxiety. We examined associations between retrospectively reported CT, its severity, and types with seven unhealthy lifestyle behaviors and a cumulative lifestyle index. Results showed that CT was positively associated with smoking, illicit drug use, social inactivity, sleep deprivation, and excessive weight gain (β = .040–.98, pFDR < .05); negatively associated with alcohol use (β = -.042, pFDR = .033), and most strongly associated with cumulative lifestyle index (β = .141, pFDR < .001). Severe CT history (multiple types or frequencies of trauma) showed the strongest effects. The largest effects with the cumulative lifestyle index were found for physical abuse (β = .159, pFDR < .001), while other CT subtypes (emotional neglect/abuse, sexual abuse) showed similar effects (β = .127–.157, pFDR < .001). Associations were partially explained by the presence of depressive/anxiety disorders, lower education, and higher numbers of chronic diseases. Individuals with CT, especially severe forms, show diverse and accumulated unhealthy lifestyle behaviors in adulthood and, thus, may benefit from lifestyle-based interventions.
Adverse childhood experiences (ACEs) are a critical area of study that examines the lasting impacts of traumatic events during childhood. These traumatic events involve a wide range of adverse experiences, including but not limited to physical abuse, emotional abuse, sexual abuse, and emotional neglect (Felitti et al., Citation1998; Hughes et al., Citation2017). It was found that exposure to ACEs was associated with various negative health outcomes in adulthood, such as chronic diseases, mental health disorders, and health-risk behaviors (Ford et al., Citation2011; Kalmakis & Chandler, Citation2015). For example, childhood trauma (CT), including abuse or neglect, is strongly related to developing depressive and anxiety disorders in adulthood (Hovens et al., Citation2010; J. G. F. M. Hovens et al., Citation2017). One of the possible mechanisms underlying this relation is CT negatively impacting individuals’ lifestyle behaviors, such as patterns of physical activity, weight management, sleep duration, and substance use (smoking, drug, or alcohol use; Kendall-Tackett, Citation2002; Monnat & Chandler, Citation2015; Springer et al., Citation2003). Although these behaviors may act as short-term coping mechanisms for CT, subsequent depression or anxiety may occur as a result of more sedentary behaviors (Boschloo et al., Citation2014; Isaac et al., Citation2009), excessive weight gain (Baldofski et al., Citation2019; Gibson-Smith et al., Citation2016; Jorm et al., Citation2003), short or long sleep duration (van Mill et al., Citation2013; Zhai et al., Citation2015), and substance abuse (Swendsen & Merikangas, Citation2000).
The evidence on how CT increases the risk for affective disorders through unhealthy lifestyle behaviors is still limited, because a thorough and in-depth assessments of the association between CT and adults’ unhealthy lifestyle behaviors is still lacking (Monnat & Chandler, Citation2015; Roche et al., Citation2019). Most studies have primarily focused on substance use and weight management in the context of CT and found a dose-response effect between CT severity and adults’ unhealthy lifestyle (Anda et al., Citation2006; Dube et al., Citation2002; Petruccelli et al., Citation2019; Williamson et al., Citation2002). For instance, evidence has shown modest to strong associations between CT and adults’ smoking behavior, drug abuse, and alcohol abuse (Hughes et al., Citation2017; Kendall-Tackett, Citation2002). In addition, numerous studies have found that individuals with CT often experience disturbed sleep, such as shorter sleep duration than average (Schonning et al., Citation2022; Sullivan et al., Citation2019). Nevertheless, limited evidence is available on CT and other unhealthy lifestyle behaviors, such as physical or social inactivity, even though social dysconnectivity is strongly related to depression onset (Santini et al., Citation2020).
Moreover, while different aspects of an unhealthy lifestyle often coexists in the individual, no study has previously focused on a cumulative unhealthy lifestyle index, which could be a useful marker for individuals’ morbidity and mortality (Grummitt et al., Citation2021). Furthermore, current knowledge of the associations between different subtypes of CT and unhealthy lifestyle behaviors is quite inconsistent. For example, there was research suggesting that physical abuse, rather than emotional neglect or emotional abuse, was slightly more strongly related to drug use (Norman et al., Citation2012). However, other research found that among all CT types, emotional abuse and neglect were more strongly related to various categories of substance dependence, especially, alcohol abuse and smoking (Strathearn et al., Citation2020). Finally, individuals with CT are more often characterized by lower socio-economic status (SES) and higher rates of somatic and/or mental disorders, which in turn are linked to the engagement in unhealthy lifestyle behaviors (Min et al., Citation2013; Romano et al., Citation2015). Therefore, it is important to adjust for these covariates, as they could partially explain the relationship between CT and unhealthy lifestyle.
The aim of this study is to better understand the associations between CT and unhealthy lifestyle by comprehensively examining how CT, its severity, and types were associated with seven unhealthy lifestyle behaviors (smoking, illicit drug use, alcohol use, social inactivity, sleep deprivation, physical inactivity, and excessive weight gain) and a cumulative unhealthy lifestyle index. Data were used from a large adult cohort (n = 2981), with demographic (age, gender), SES, and health-related (chronic/somatic diseases, depressive and/or anxiety disorders) covariates adjusted. It was hypothesized that CT would be associated with multiple unhealthy lifestyle behaviors, with the strongest association between severe CT and the cumulative lifestyle index. No specific hypothesis was made regarding CT types because of the limited and inconsistent evidence.
Method
Sample and study design
Baseline data collected between 2004 and 2007 were analyzed from the Netherlands Study of Depression and Anxiety (NESDA): an ongoing longitudinal cohort study that initially recruited 2,981 participants (female = 66.4%), aged 18–65 years old (M = 41.9, SD = 13.0) (Penninx et al., Citation2008). Within this sample, there were 2,968 participants with an available CT assessment and at least one available unhealthy lifestyle behavior variable. This sample consisted of 2,318 (78.1%) participants with remitted or current depressive and/or anxiety disorders diagnosed by Composite Interview Diagnostic Instrument (CIDI) – lifetime version 2.1 (Robins et al., Citation1988), based on the Diagnostic and Statistical Manual-fourth edition (DSM-IV; APA, Citation2000), and 650 (21.9%) healthy controls (people without a lifetime disorder). DSM-IV diagnoses focused on dysthymia, major depressive disorder (MDD), general anxiety disorder (GAD), panic disorder, social phobia, and agoraphobia.
Participants were recruited from the community, primary care, and specialized mental healthcare. Individuals who were not fluent in Dutch or had a primary clinical diagnosis of other psychiatric disorders (i.e. psychotic disorder, obsessive-compulsive disorder, post-traumatic stress disorder, bipolar disorder, or severe addiction disorder) that could largely affect the course trajectory of depression and anxiety were excluded. NESDA was approved centrally by the Ethical Review Board of the VU University Medical Centre. All participants provided written informed consent. A detailed description of the sample and procedure of NESDA was described previously (Penninx et al., Citation2008).
Measures
Childhood trauma
CT was measured retrospectively by trained assessors using a 10-minute semi-structured Childhood Trauma Interview (CTI), which was used in the Netherlands Mental Health Survey and Incidence Study (NEMESIS; Graaf et al., Citation2002). Participants were asked whether they had experienced stressful life events and/or any abuse before the age of 16. Four traumatic childhood events were measured: emotional neglect, emotional abuse, physical abuse, and sexual abuse. Each type of CT was assessed on a frequency scale from 0 to 2, with “0” representing “not at all,” “1” representing “once/sometimes” and “2” representing “regularly/often/very often.” The sum score of the four types of CT, which indicated the number of domains and the frequency of the abuse/neglect, was computed by the CT index that ranged from 0 to 8 (Hovens et al., Citation2010). Individuals who had a sum score of 1–3 were defined as having experienced mild CT, and a sum score of 4–8 were defined as having experienced severe CT. The CT index has been found to detect a dose-response association between CT and psychopathology (Hovens et al., Citation2010; Wiersma et al., Citation2009). The CTI shows good reliability and validity, indicated by a Cronbach’s α above 0.90 in the study by Fink et al. (Citation1995).
Unhealthy lifestyle behaviors
Smoking
Smoking was assessed as a self-reported current number of cigarettes smoked per day (range 0–125) and blood-measured cotinine concentration (ng/ml; nicotine markers, range 0–2166; Penninx et al., Citation2008). In the current study, a significant correlation (r = .48, p < .01) was found between the number of cigarettes smoked and cotinine levels. Therefore, a cumulative smoking behavior score was also used as the average score of the two standardized variables.
Illicit drug use
Participants were asked to report whether they used different types of illicit drugs in the last month (yes or no). Both the soft drugs (cannabis) and hard drugs (ecstasy, speed, cocaine, heroin, or Lysergic acid diethylamide (LSD)) were queried (Bos et al., Citation2015; Boschloo et al., Citation2011). In the current study, the number of self-reported drugs used ranged from 0 to 4.
Alcohol use
Two items were used to measure self-reported alcohol consumption on a five-point Likert scale. Item one measured the average frequency of drinking in the last year, ranging from 1 = “never” to 5 = “four or more times per week.” Item two measured the typical quantity of drinks consumed per day, including 1 = “1 or 2,” 2 = “2 or 3,” 3 = “5 or 6,” 4 = “7, 8, or 9,” and 5 = “10 or more” (Bos et al., Citation2015). A drink is defined as a single small (8 ounces; 1/2 pint!) glass of beer, a single shot/measure of liquor/spirits, or a single glass of wine. Alcohol use was calculated and indexed by the self-reported numbers of drinks per week (range 0–65.82) in the last year. To examine how different levels of alcohol use associate with CT, we defined low drinks as “no drinks per week,” regular drinks as “1 to 4 drinks per week,” and heavy drinks as “more than 4 drinks per week.”
Social inactivity
The visiting frequency of five types of social activities was measured, including: (1) cultural events (theater, cinema, or museum); (2) trips to nature or amusement parks; (3) visiting a bar, restaurant, or dancing; (4) attending an activity or meeting of a club or association; and (5) sports activities outside the home. The frequency of attending social activities was reported on a six-point Likert scale, including 1 = “almost never,” 2 = “a couple of times a year,” 3 = “every month,” 4 = “a couple of times a month,” 5 = “every week,” and 6 = “a couple of times a week” (de Wit et al., Citation2015). To investigate unhealthy lifestyle, we used a reversed total score of the frequency of the five activities (range 5–30) with higher numbers indicating less social activities frequency.
Sleep deprivation
Self-reported average sleep hours per night in the last four weeks were used as a measure of sleep deprivation, with higher numbers indicating fewer sleeping hours: 1 = “10 or more hours,” 2 = “9 hours,” 3 = “8 hours,” 4 = “7 hours,” 5 = “6 hours” to 6 = “5 hours or fewer.” The continuous sleep deprivation score was used for the main analyses. To further examine how sleep hours per night relate to CT, participants with 10 or more hours were considered to have a long sleep, 7 to 9 hours were considered to have a regular sleep, and 6 or less hours were considered to have a short sleep (Penninx et al., Citation2008).
Physical inactivity
Seven-item self-reported short-format International Physical Activity Questionnaire (IPAQ-SF) was used to measure how many minutes an individual spent on (1) walking, (2) moderate activity (e.g. leisure cycling), and (3) vigorous activities (e.g. aerobic exercise) in the last seven days (Lee et al., Citation2011). The overall energy expenditure was the summation of the duration (minutes) and frequency (days/week) of the three types of activities computed by Metabolic Equivalent (METs)-minutes per week (METs-minutes/week (Ainsworth et al., Citation1993).; IPAQ has good reliability (Spearman’s rho clustered around 0.8) and validity (median rho of about 0.30; Craig et al., Citation2003; Hagstromer et al., Citation2006; Lee et al., Citation2011). In this study, we used the reversed total score with higher numbers indicating lower engagement in activities.
Excessive weight gain
Excessive weight gain was indexed by BMI (range 14.7–55.83), hip circumference (cm, range 69–175), and waist circumference (cm, range 60–165). BMI was computed as weight (kg) divided by height (m2) of the participants, measured by trained assessors (Penninx et al., Citation2008). Individuals with a BMI ranging between 25.0 and 29.9 were considered overweight, and a BMI ≥ 30 was considered excessive weight gain. In the current study, high and significant correlations (r = .78–.85, p < .01) were found between body mass index (BMI), hip circumference (cm), and waist circumference (cm). Therefore, a cumulative score of excessive weight gain was additionally used as the average score of the three standardized variables.
Cumulative unhealthy lifestyle index
For the unhealthy behaviors significantly and positively linked to CT, a cumulative score was created. These behaviors included smoking, illicit drug use, social inactivity, sleep deprivation, and excessive weight gain. Z-scores were used to standardize values across different lifestyle behaviors. The cumulative index was calculated as the average score of the total standardized lifestyle behaviors and standardized again. The cumulative outcomes were only estimated for participants who completed the measurements of each included lifestyle behavior (n = 2476, 83.4%).
Covariates
All analyses included basic demographic covariates (i.e. age in years and gender). To explore the role of SES and health-related covariates in the association between CT and lifestyle behaviors, we additionally included years of education, number of chronic diseases (range 0–8), and psychiatric status (current/remitted depression and/or anxiety vs. healthy control) in the analyses. Chronic diseases were assessed by a face-to-face interview about the presence and treatment for 20 somatic diseases, including asthma, chronic bronchitis or pulmonary emphysema, heart diseases or infarct, diabetes, stroke or CVA, arthritis or arthrosis, rheumatic complaints tumor or malignant tumor and metastasis, high blood pressure, stomach or intestinal ulcer, intestinal disorders, liver disease or liver-cirrhosis, epilepsy, chronic fatigue syndrome, allergies, thyroid gland disease injury (within the past year), head injury (lifetime), and other chronic disease. Psychiatric status was assessed by the CIDI – lifetime version 2.1. (Robins et al., Citation1988) assessing the current (past six months) and remitted (lifetime, but not past six months) depression and anxiety disorders according to the DSM-IV (American Psychiatric Association, Citation2000).
Data analyses
Descriptive analyses were used to examine sample characteristics to present means (M) with standard deviations (SD), numbers (N) with percentages (%), or medians with interquartile ranges (IQR; for skewed outcome variables). Non-normally distributed outcome variables (number of cigarettes smoked, cotinine concentration, illicit drug use, alcohol use, physical inactivity) were log-transformed (ln; Feng et al., Citation2014). All outcome variables were further standardized (Z-scores).
Spearman’s correlation examined the intercorrelations between CT and multiple lifestyle behaviors. Outcome variables that were non-significantly or negatively correlated to CT were dropped for further cumulative lifestyle index calculation, since they were not considered unhealthy lifestyle behaviors in the current sample. Multiple linear regression analyses examined whether CT was significantly associated with adults’ unhealthy lifestyle behaviors. The central determinant was CT which was coded as (1) continuous total severity score (CT index, range 0–8), (2) dichotomous severity of CT (mild CT versus no CT, severe CT versus no CT), (3) dichotomous subtyped score (emotional neglect versus no CT, emotional abuse versus no CT, physical abuse versus no CT, and sexual abuse versus no CT). To consider the comorbidity between CT subtypes, each CT type was analyzed in a separate model. The outcome was multiple lifestyle behaviors (separate seven outcomes and a cumulative outcome). Separate regression analyses were conducted for each outcome variable. Two models were created to avoid overadjustment and determine the role of SES and health-related covariates: Model 1 adjusted for basic demographic variables (age, gender), and Model 2 additionally adjusted for SES and health-related variables (see covariates section).
Since the majority of missing data in the current sample was below 5%, we used the complete-case analysis as the main analysis (Jakobsen et al., Citation2017). To ensure that missing data did not bias our results, we additionally conducted a sensitivity analysis using multiple imputations for missing lifestyle data. This process was repeated to create 20 imputed datasets (von Hippel, Citation2020), and the results were based on pooled analyses. To examine whether CT shows similar effects on lifestyle behaviors in patient and non-patient samples, additional multiple regression analyses were conducted separately in individuals with current depressive and/or anxiety disorders (n = 1693, 57.0%) and individuals without current disorders (n = 1275, 47.3%). Moreover, we formally checked if main associations in Model 2 could be moderated by psychiatric status using CT × current and CT × remitted depressive and/or anxiety disorder interaction terms on cumulative lifestyle behaviors.
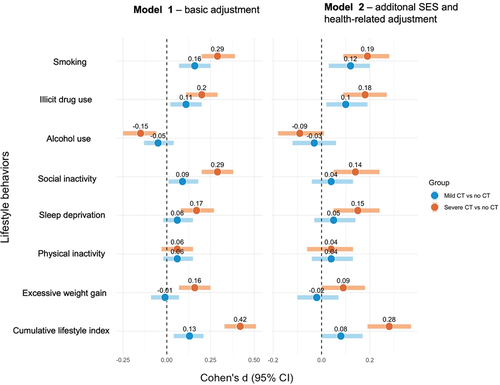
All the analyses used a statistical significance level of 95% (p < .05). Due to a large number of conducted analyses and data not missing completely at random, we performed the Benjamini-Hochberg procedure to control for the false discovery rate (FDR) – the proportion of significant results that are false positives (8 tests per model; pFDR < .05; Benjamini & Hochberg, Citation1995; Jafari & Ansari-Pour, Citation2019). The Benjamini-Hochberg method was selected because it is less stringent than the family-wise error rate, and, thus, is more powerful. To better visualize the effects of CT severity (mild and severe CT versus no CT) on unhealthy lifestyle behaviors, a forest plot that converted standardized regression coefficient (beta, β) to Cohen’s d (95% confidence intervals, CI) was calculated. Data were interpreted using IBM SPSS 27 and RStudio 1.2.5042.
Results
Sample characteristics
Sample characteristics are presented in . The sample consisted of 2968 participants (female = 66.4%), with a mean age of 41.83 years (SD = 13.07). About half of the sample had experienced at least one type of CT (48.5%, n = 1440), and within this sample, 21.6% (n = 641) had severe CT, and 26.9% (n = 799) had mild CT. The mean CT index was 1.61 (SD = 2.12), with the following mean scores in the four domains: emotional neglect at 0.72 (SD = 0.93), emotional abuse at 0.45 (SD = 0.81), physical abuse at 0.21 (SD = 0.55), and sexual abuse at 0.23 (SD = 0.51). Among the participants with CT, 88.7% (n = 1277) had current or remitted depressive and/or anxiety disorder, and the mean number of chronic diseases was 1.05 (SD = 1.17).
Table 1. Sample characteristics (nmax = 2968).
A total of 2348 (79.1%) participants completed data on all unhealthy lifestyle behaviors, with missing data on numbers of cigarettes smoked (n = 80, 2.7%), cotinine concentration (n = 53, 1.8%), illicit drug use (n = 34, 1.1%), alcohol use (n = 41, 1.4%), social inactivity (n = 59, 2.0%), sleep deprivation (n = 356, 12.0%), physical inactivity (n = 193, 6.5%), body mass index (BMI, n = 2, 0.1%), hip circumference (n = 6, 0.2%), and waist circumference (n = 5, 0.2%). Compared to participants who had lifestyle missing data (n = 620), participants with all lifestyle variables (n = 2348) were similar in age and years of education (p > .5), but were more often female (χ2 = 5.79, p < .05), had a lower prevalence of current and remitted depressive and/or anxiety disorders (χ2 = 13.86, p < .05), and a lower CT index score (t (1) = 3.46, p < .05). Little’s Missing Test indicated that the data were not missing completely at random (χ2 = 67.58, df = 6, p < .05).
Correlations between CT and multiple unhealthy lifestyle behaviors are shown in . Overall, different lifestyle behaviors were weakly but significant associated (ρ = −.24 to .20, p < .01). CT significantly correlated with all lifestyle behaviors, except for physical inactivity (ρ = −.03, p > .05), and negatively correlated with alcohol use (ρ = −.08, p < .01). Therefore, a cumulative lifestyle index was created, including five unhealthy lifestyle behaviors that were significantly and positively related to CT. The strongest correlation was found between CT and cumulative lifestyle index (ρ = .18, p < .01).
Table 2. Spearman correlations (ρ) between multiple standardized lifestyle behaviors and childhood trauma index (nmax = 2968).
Associations between CT and lifestyle behaviors
CT Index and unhealthy lifestyle behaviors
When controlling for basic covariates in Model 1, CT index was significantly and positively associated with smoking (β = .141, pFDR < .001; R2 = .033), illicit drug use (β = .105, pFDR < .001; R2 = .049), social inactivity (β = .135, pFDR < .001; R2 = .027), sleep deprivation (β = .088, pFDR < .001; R2 = .074), and excessive weight gain (β = .068, pFDR < .001; R2 = .108); negatively associated with alcohol use (β = −.071, pFDR < .001; R2 = .070); and the association was only absent for physical inactivity (β = .021, pFDR > .05; R2 = .002; ). The strongest association was seen with cumulative lifestyle index (β = .200, pFDR < .001; R2 = .124). After additionally controlling for SES and health-related covariates in Model 2, the effects of CT index were partially reduced on multiple lifestyle behaviors. For instance, the effect for cumulative lifestyle index was reduced (β drop = 29.5%) by the presence of depressive and/or anxiety disorders (β drop = 19.7%), lower SES (β drop = 13.0%), and higher rates of chronic diseases (β drop = 8.1%). Sensitivity analysis, in which multiple imputation was used to account for missing lifestyle data, revealed comparable results of the association between CT index and unhealthy lifestyle (see ).
Table 3. Multiple regression results on standardized childhood trauma score (nmax = 2968).
In addition, we explored the impact of CT on multiple lifestyle behaviors in patient with and without current depressive and/or anxiety disorders.Footnote1 We also tried to explain the negative association between alcohol use and CT by looking at how different levels of alcohol use (i.e. no drinks, regular drinks, and heavy drinks) were associated with CT index. Results showed that heavy drinks (>4 drinks per week) were significantly and negatively associated with CT (β = −.217, p < .05), whereas low drinks (no drinks per week) were not (β = .211, p = .054), when controlling for gender and age. However, the significant association with heavy drinking (β = −.160, p = .057) further disappeared when controlled for SES and health-related covariates. We also conducted regression analyses for sleep duration, as previous findings showed that both short and long sleep are risk factors for psychopathology (van Mill et al., Citation2013; Zhai et al., Citation2015). When controlling for age and gender, short sleep (versus regular sleep) was significantly associated with CT in our sample (β = .610, p < .001). No significant association was found for long sleep (β = .389, p =.058).
Mild and severe CT asssociations with unhealthy lifestyle behaviors
Regression results of mild and severe CT associations with lifestyle behaviors are presented in . To better visualize the effects, the forest plot of between-group effect sizes (Cohen’s d) with 95% CI is presented in . Mild CT was positively associated with smoking (d = 0.16, 95% CI [0.08, 0.25]), illicit drug use (d = 0.11, 95% CI [0.02, 0.19]), social inactivity (d = 0.09, 95% CI [0.01, 0.18]), and cumulative lifestyle index (d = 0.13, 95% CI [0.04, 0.21]) in Model 1. These significance levels only disappeared for social inactivity (d = 0.04, 95% CI [- 0.04, 0.13]) in Model 2. Severe CT was additionally associated with sleep deprivation (d = 0.17, 95% CI [0.08, 0.27]) and excessive weight gain (d = 0.16, 95% CI [0.07, 0.25]); negatively associated with alcohol use (d = −0.15, 95% CI [- 0.25, − 0.06]), and the significance level disappeared for alcohol use (d = −0.09, 95% CI [- 0.10, 0.01]) in Model 2. Overall, participants with severe CT reported more unhealthy lifestyle behaviors, with the strongest difference in cumulative lifestyle index (dmild = 0.08, 95% CI [0.01, 0.18]; dsevere = 0.28, 95% CI [0.18, 0.36]), compared to participants with mild CT.
Figure 1. Forest plot of the effect sizes (Cohen’s d) of mild and severe CT on multiple lifestyle behaviors.
CT types and unhealthy lifestyle behaviors
Among the CT types (), physical abuse showed the strongest association with cumulative lifestyle index (β = .159, pFDR < .001; R2 = .110 in Model 1; β = .116, pFDR < .001; R2 = .213 in Model 2). However, effects were rather comparable with emotional abuse (β = .157, pFDR < .001; R2 = .109 in Model 1; β = .104, pFDR < .001; R2 = .213 in Model 2), sexual abuse (β = .132, pFDR < .00; R2 = .102 in Model 1; β = .096, pFDR = .008; R2 = .211 in Model 2), and emotional neglect (β = .127, pFDR < .001; R2 = .101 in Model 1; β = .085, pFDR < .001; R2 = .209 in Model 2).
Table 4. Multiple regression results on standardized lifestyle behaviors associated with CT types (nmax = 2968).
Discussion
The current study confirmed a dose-response relationship between CT and diverse unhealthy lifestyle behaviors in adulthood (Anda et al., Citation2006; Dube et al., Citation2002; Petruccelli et al., Citation2019; Williamson et al., Citation2002). Some of the findings are consistent with previous studies, showing that CT has a modest impact on weight management (Danese & Tan, Citation2014; Hughes et al., Citation2017; Lang et al., Citation2020), high impact on smoking and illicit drug use (Hughes et al., Citation2017; Ramiro et al., Citation2010), negative impact on sleep duration (Schonning et al., Citation2022; Sullivan et al., Citation2019), and non-significant impact on physical inactivity (Chartier et al., Citation2009; Rodgers et al., Citation2004). Our novel finding was the positive association between CT and social inactivity, and more importantly, the strongest CT associations with the cumulative lifestyle index. These largest effects can be explained by the allostatic load theory, which indicates the overall wear and tear of the body as a result of chronic exposure to stress (McEwen, Citation2005). While the stress systems are adaptative and can help the body response to acute stressors, chronic or repeated activation can lead to negative health outcomes. In this study, adults with CT could accumulate chronic stress over time, which might lead to overall negative patterns of their lifestyle behaviors and increase vulnerability to physical or mental health diseases (Guidi et al., Citation2021). Evidence also showed that early abuse and neglect predict allostatic load even 30 years later (Widom et al., Citation2015).
Interestingly, we did not find a previously reported positive association between CT and alcohol use (Danese & Tan, Citation2014; Hughes et al., Citation2017; Lang et al., Citation2020), and instead observed a negative association when looking into CT and the number of drinks per week. This finding was not explained by any of the included covariates and may likely stem from the selection bias of NESDA sample that primarily targets affective disorders instead of alcohol dependence (Penninx et al., Citation2008). This inconsistency with earlier findings may also be due to a difference in alcohol use measurement: we examined the number of drinks per week in the last year instead of the alcohol dependence used in previous studies (Lang et al., Citation2020). However, it is important to note that when looking into CT and categorical alcohol use, the negative association between CT and heavy drinks (>4 per week) disappeared after adjusting for SES and health-related covariates. This was mostly driven by the presence of chronic diseases in individuals with CT, as individuals with chronic diseases usually do not drink excessively (Newsom et al., Citation2012).
The association between CT and the cumulative unhealthy lifestyle index was partly explained by the presence of depressive and/or anxiety disorders, lower years of education, and a higher number of chronic diseases. From this, it may be assumed that the environmental context of those exposed to CT is of utmost importance, since CT and low SES frequently co-occur in youth (Assari, Citation2020). This increases the risk of an unhealthy lifestyle behavior during the lifespan, which may subsequently contribute to the somatic and mental health burdens, or the other way around (Boschloo et al., Citation2014; Hamilton et al., Citation2018; Swendsen & Merikangas, Citation2000).
When further looking into CT types, physical abuse showed somewhat stronger effects on unhealthy lifestyle behaviors. However, no considerable differences between CT types were observed. These findings align with the previous meta-analysis, showing that adults with childhood physical abuse had a somewhat higher risk of illicit drug use, but other CT types (emotional abuse and neglect) also showed a significant risk (Norman et al., Citation2012). As noted in previous literature, the current results suggest significant impacts of all forms of CT on health (Norman et al., Citation2012). It is also essential to mention that any type of CT rarely stands alone and often co-occurs with different childhood traumatic events (Hartley, Citation2002). More importantly, the co-currency of CT types addresses the importance of CT severity, as evidence has shown a negative dose-response association between the numbers of CT and adult health (Agorastos et al., Citation2014). Our current study also showed that individuals with severe CT had the strongest associations with multiple unhealthy lifestyle behaviors, particularly the cumulative lifestyle index.
Strengths and limitations
The current study has three central points of contribution to the existing literature. First, the study focused on multiple unhealthy lifestyle behaviors and calculated a cumulative unhealthy lifestyle index. This cumulative lifestyle index indicated the total incidence and extent of individuals’ engagement with multiple unhealthy lifestyle behaviors, which provided a clearer view of how CT impacted various aspects of adults’ unhealthy lifestyle. It is also a good index for individuals’ morbidity and mortality since unhealthy lifestyle behaviors can contribute to adverse health outcomes (Grummitt et al., Citation2021). Second, this study explored an in-depth association between different severity and types of CT and unhealthy lifestyle behaviors, which have meaningful implications for practitioners treating clients with CT. Practitioners should be aware of an increased risk of engagement in multiple unhealthy lifestyle behaviors among patients with CT, especially severe CT, as it could interfere with the effectiveness of an ongoing treatment. Hence, providing supplementary lifestyle-based interventions could be beneficial. It is also important to consider prevention of health-risk behaviors in individuals with CT to mitigate the development of mental and somatic disorders later in life. Last, this study controlled for potentially confounding and explanatory factors in one large-scale cohort with adequate statistical power to determine associations between CT and multiple unhealthy lifestyle behaviors. By creating a two-step model adjusted for covariates, we reduced the risks of overadjustment and revealed how SES and health-related variables explained the CT and lifestyles association. Compared to meta-analyses and systematic reviews that synthesized results from multiple individual studies, this study also had the advantage of avoiding methodological heterogeneity (Thompson, Citation1994).
Some limitations of the current study are noteworthy. The first limitation is retrospectively-reported CT, which is prone to a higher risk of recall bias (Coughlin, Citation1990). This issue is particularly pronounced due to the broad age range of participants, spanning from 18 to 65 years old. Nevertheless, the CTI was found to have good reliability and validity (Fink et al., Citation1995), and previous NESDA studies also showed moderate to high correlations between CTI and Childhood Trauma Questionnaire (CTQ; assessed four years after the baseline), indicating high consistency of retrospective CT reports (Kuzminskaite et al., Citation2020; Spinhoven et al., Citation2014). Second, this study is cross-sectional, which restricts the assessment of the causal relationship between CT and lifestyle behaviors. Longitudinal research that follows children cohorts over time may better explain the causal role of early adversity on individuals’ lifestyle behaviors and explore the developmental course of CT on lifestyle behaviors. Third, although our study is the first to focus on a cumulative lifestyle index, the selection of outcome variables was limited. It was also limited in utilizing the previous version of DSM, as this study collected data from 2004 to 2007 when the diagnostic manual in use was the DSM-IV. There was a lack of additional (objective) measures for each single lifestyle behaviors except for smoking and excessive weight gain. Further studies that measure additional psychological or biological levels (e.g. brain activity, stress-system dysfunction, actigraphy-based sleep or physical activity) of participants’ lifestyle behaviors alongside self-report measures are needed.
Conclusion
Within NESDA, a unique large scale cohort study, individuals with CT indicated a higher frequency of experiencing smoking, illicit drug use, social inactivity, sleep deprivation, and excessive weight gain; however, they seemed to engage less often in alcohol use. A clear dose-response relationship was found between CT and unhealthy lifestyle behaviors, with the highest effects seen for the cumulative lifestyle index. Physical abuse showed somewhat stronger effects, but its effects were rather comparable to other CT types. The effects of CT on unhealthy lifestyle behaviors were reduced in multivariate analyses by the presence of current and/or remitted mental disorders, lower years of education, and higher numbers of chronic diseases. This suggests that that lifestyle-based interventions may be effective for reducing the burden of somatic and psychiatric diseases among individuals with CT.
Ethics
This study was approved by the Ethical Review Board of the VU University Medical Centre.
Supplemental Material
Download MS Word (87.3 KB)Disclosure statement
No potential conflict of interest was reported by the authors.
Supplementary material
Supplemental data for this article can be accessed online at https://doi.org/10.1080/10926771.2024.2307380
Additional information
Funding
Notes
1 When looking into the sample with and without current depressive and anxiety disorders (Table S3, Table S4), the effects of CT differed for multiple lifestyle behaviors, but were rather similar for cumulative lifestyle index (n = 1363, β = .143, pFDR < .001; n = 1113, β = .134, pFDR < .001). Following that, no significant CT x current disorder (β = .020, p = .721) or CT x remitted disorder (β = .003 p = .941) interactions were observed for cumulative lifestyle index, suggesting no moderation effects of psychiatric status on the associations between CT and lifestyle behaviors.
References
- Agorastos, A., Pittman, J. O., Angkaw, A. C., Nievergelt, C. M., Hansen, C. J., Aversa, L. H., Parisi, S. A., Barkauskas, D. A., & Baker, D. G. The Marine Resiliency Study Team. (2014). The cumulative effect of different childhood trauma types on self-reported symptoms of adult male depression and PTSD, substance abuse and health-related quality of life in a large active-duty military cohort. Journal of Psychiatric Research, 58, 46–54. https://doi.org/10.1016/j.jpsychires.2014.07.014
- Ainsworth, B. E., Haskell, W. L., Leon, A. S., Jabobs, D. R., Montoy, H. J., Sallis, J. F., & Paffenbarger, R. S. (1993). Compendium of physical activities: Classification of energy costs of human physical activities. Medicine & Science in Sports & Exercise, 25(1), 71–80. https://doi.org/10.1249/00005768-199301000-00011
- American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders fourth edition text revision (DSM-IV TR). https://doi.org/10.1176/appi.books.9780890423349
- Anda, R. F., Felitti, V. J., Bremner, J. D., Walker, J. D., Whitfield, C., Perry, B. D., Dube, S. R., & Giles, W. H. (2006). The enduring effects of abuse and related adverse experiences in childhood. European Archives of Psychiatry and Clinical Neuroscience, 256(3), 174–186. https://doi.org/10.1007/s00406-005-0624-4
- Assari, S. (2020). Family socioeconomic status and exposure to childhood trauma: Racial differences. Children-Basel, 7(6), 57. https://doi.org/10.3390/children7060057
- Baldofski, S., Mauche, N., Dogan-Sander, E., Bot, M., Brouwer, I. A., Paans, N. P. G., Cabout, M., Gili, M., van Grootheest, G., Hegerl, U., Owens, M., Roca, M., Visser, M., Watkins, E., Penninx, B. W. J. H., & Kohls, E. (2019). Depressive symptom clusters in relation to body weight status: Results from two large European multicenter studies. Frontiers in Psychiatry, 10, 858. https://doi.org/10.3389/fpsyt.2019.00858
- Benjamini, Y., & Hochberg, Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society: Series B (Methodological), 57(1), 289–300. https://doi.org/10.1111/j.2517-6161.1995.tb02031.x
- Bos, H. M. W., Boschloo, L., Schoevers, R. A., & Sandfort, T. G. M. (2015). Depression and anxiety in patients with and without same-sex attraction: Differences in clinical expression, lifestyle factors, and vulnerability indicators. Brain and Behavior, 5(9), e00363–e00363. https://doi.org/10.1002/brb3.363
- Boschloo, L., Reeuwijk, K. G., Schoevers, R. A., & Penninx, B. W. J. H. (2014). The impact of lifestyle factors on the 2-year course of depressive and/or anxiety disorders. Journal of Affective Disorders, 159, 73–79. https://doi.org/10.1016/j.jad.2014.01.019
- Boschloo, L., Vogelzangs, N., Smit, J. H., van den Brink, W., Veltman, D. J., Beekman, A. T. F., & Penninx, B. W. J. H. (2011). Comorbidity and risk indicators for alcohol use disorders among persons with anxiety and/or depressive disorders: Findings from the Netherlands study of depression and anxiety (NESDA). Journal of Affective Disorders, 131(1), 233–242. https://doi.org/10.1016/j.jad.2010.12.014
- Chartier, M. J., Walker, J. R., & Naimark, B. (2009). Health risk behaviors and mental health problems as mediators of the relationship between childhood abuse and adult health. American Journal of Public Health, 99(5), 847–854. https://doi.org/10.2105/AJPH.2007.122408
- Coughlin, S. S. (1990). Recall bias in epidemiologic studies. Journal of Clinical Epidemiology, 43(1), 87–91. https://doi.org/10.1016/0895-4356(90)90060-3
- Craig, C., Marshall, A., Sjostrom, M., Bauman, A., Booth, M., Ainsworth, B., Pratt, M., Ekelund, U., Yngve, A., Sallis, J., & Oja, P. (2003). International physical activity questionnaire: 12-country reliability and validity. Medicine and Science in Sports and Exercise, 35(8), 1381–1395. https://doi.org/10.1249/01.MSS.0000078924.61453
- Danese, A., & Tan, M. (2014). Childhood maltreatment and obesity: Systematic review and meta-analysis. Molecular Psychiatry, 19(5), 544–554. https://doi.org/10.1038/mp.2013.54
- de Wit, L. M., van Straten, A., Lamers, F., Cuijpers, P., & Penninx, B. W. J. H. (2015). Depressive and anxiety disorders: Associated with losing or gaining weight over 2 years? Psychiatry Research, 227(2), 230–237. https://doi.org/10.1016/j.psychres.2015.02.025
- Dube, S. R., Anda, R. F., Felitti, V. J., Edwards, V. J., & Croft, J. B. (2002). Adverse childhood experiences and personal alcohol abuse as an adult. Addictive Behaviors, 27(5), 713–725. https://doi.org/10.1016/S0306-4603(01)00204-0
- Felitti, V. J., Anda, R. F., Nordenberg, D., Williamson, D. F., Spitz, A. M., Edwards, V., & Marks, J. S. (1998). Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults: The adverse childhood experiences (ACE) study. American Journal of Preventive Medicine, 14(4), 245–258. https://doi.org/10.1016/S0749-3797(98)00017-8
- Feng, C., Wang, H., Lu, N., Chen, T., He, H., Lu, Y., & Tu, X. M. (2014). Log-transformation and its implications for data analysis. Shanghai Archives of Psychiatry, 26(2), 105–109. https://doi.org/10.3969/j.issn.1002-0829.2014.02.009
- Fink, L. A., Bernstein, D., Handelsman, L., Foote, J., & Lovejoy, M. (1995). Initial reliability and validity of the childhood trauma interview: A new multidimensional measure of childhood interpersonal trauma. The American Journal of Psychiatry, 152(9), 1329–1335. https://doi.org/10.1176/ajp.152.9.1329
- Ford, E. S., Anda, R. F., Edwards, V. J., Perry, G. S., Zhao, G., Li, C., & Croft, J. B. (2011). Adverse childhood experiences and smoking status in five states. Preventive Medicine, 53(3), 188–193. https://doi.org/10.1016/j.ypmed.2011.06.015
- Gibson-Smith, D., Bot, M., Paans, N. P. G., Visser, M., Brouwer, I., & Penninx, B. W. J. H. (2016). The role of obesity measures in the development and persistence of major depressive disorder. Journal of Affective Disorders, 198, 222–229. https://doi.org/10.1016/j.jad.2016.03.032
- Graaf, R., Bijl, R., Smit, F., Vollebergh, W. A. M., & Spijker, J. (2002). Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: Findings from the Netherlands Mental Health Survey and incidence study. The American Journal of Psychiatry, 159(4), 620–629. https://doi.org/10.1176/appi.ajp.159.4.620
- Grummitt, L. R., Kreski, N. T., Kim, S. G., Platt, J., Keyes, K. M., & McLaughlin, K. A. (2021). Association of childhood adversity with morbidity and mortality in US adults: A systematic review. JAMA Pediatrics, 175(12), 1269–1278. https://doi.org/10.1001/jamapediatrics.2021.2320
- Guidi, J., Lucente, M., Sonino, N., & Fava, G. A. (2021). Allostatic load and its impact on health: A systematic review. Psychotherapy and Psychosomatics, 90(1), 11–27. https://doi.org/10.1159/000510696
- Hagstromer, M., Oja, P., & Sjostrom, M. (2006). The international physical activity questionnaire (IPAQ): A study of concurrent and construct validity. Public Health Nutrition, 9(6), 755–762. https://doi.org/10.1079/PHN2005898
- Hamilton, J. L., Brindle, R. C., Alloy, L. B., & Liu, R. T. (2018). Childhood trauma and sleep among young adults with a history of depression: A daily diary study. Frontiers in Psychiatry, 9, 673. https://doi.org/10.3389/fpsyt.2018.00673
- Hartley, C. C. (2002). The co-occurrence of child maltreatment and domestic violence: Examining both neglect and child physical abuse. Child Maltreatment, 7(4), 349–358. https://doi.org/10.1177/107755902237264
- Hovens, J. G. F. M., Giltay, E. J., van Hemert, A., & Penninx, B. (2017). [Emotional scars: Impact of childhood trauma on the development of depressive and anxiety disorders later in life]. Tijdschrift Voor Psychiatrie, 59(5), 286–296.
- Hovens, J., Wiersma, J., Giltay, E., Oppen, P., Spinhoven, P., Penninx, B. W., & Zitman, F. (2010). Childhood life events and childhood trauma in adult patients with depressive, anxiety and comorbid disorders vs. controls. Acta Psychiatrica Scandinavica, 122(1), 66–74. https://doi.org/10.1111/j.1600-0447.2009.01491.x
- Hughes, K., Bellis, M. A., Hardcastle, K. A., Sethi, D., Butchart, A., Mikton, C., Jones, L., & Dunne, M. P. (2017). The effect of multiple adverse childhood experiences on health: A systematic review and meta-analysis. The Lancet Public Health, 2(8), e356–e366. https://doi.org/10.1016/S2468-2667(17)30118-4
- Isaac, V., Stewart, R., Artero, S., Ancelin, M.-L., & Ritchie, K. (2009). Social activity and improvement in depressive symptoms in older people: A prospective community cohort study. The American Journal of Geriatric Psychiatry, 17(8), 688–696. https://doi.org/10.1097/JGP.0b013e3181a88441
- Jafari, M., & Ansari-Pour, N. (2019). Why, when and how to adjust your P values? Cell Journal, 20(4), 604–607. https://doi.org/10.22074/cellj.2019.5992
- Jakobsen, J. C., Gluud, C., Wetterslve, J., & Winkel, P. (2017). When and how should multiple imputation be used for handling missing data in randomised clinical trials – a practical guide with flowcharts. BMC Medical Research Methodology, 17(1), 162. https://doi.org/10.1186/s12874-017-0442-1
- Jorm, A. F., Korten, A. E., Christensen, H., Jacomb, P. A., Rodgers, B., & Parslow, R. A. (2003). Association of obesity with anxiety, depression and emotional well-being: A community survey. Australian and New Zealand Journal of Public Health, 27(4), 434–440. https://doi.org/10.1111/j.1467-842X.2003.tb00423.x
- Kalmakis, K. A., & Chandler, G. E. (2015). Health consequences of adverse childhood experiences: A systematic review. Journal of the American Association of Nurse Practitioners, 27(8), 457–465. https://doi.org/10.1002/2327-6924.12215
- Kendall-Tackett, K. (2002). The health effects of childhood abuse: Four pathways by which abuse can influence health. Child Abuse & Neglect, 26(6), 715–729. https://doi.org/10.1016/S0145-2134(02)00343-5
- Kuzminskaite, E., Vinkers, C. H., Elzinga, B. M., Wardenaar, K. J., Giltay, E. J., & Penninx, B. W. J. H. (2020). Childhood trauma and dysregulation of multiple biological stress systems in adulthood: Results from the Netherlands study of depression and anxiety (NESDA). Psychoneuroendocrinology, 121, 104835. https://doi.org/10.1016/j.psyneuen.2020.104835
- Lang, J., Kerr, D., Petri-Romao, P., McKee, T., Smith, H., Wilson, N., Zavrou, M., Shiels, P., Minnis, H., & Salinas-Miranda, A. (2020). The hallmarks of childhood abuse and neglect: A systematic review. PloS ONE, 15(12), e0243639. https://doi.org/10.1371/journal.pone.0243639
- Lee, P. H., Macfarlane, D. J., Lam, T. H., & Stewart, S. M. (2011). Validity of the international physical activity questionnaire short form (IPAQ-SF): A systematic review. International Journal of Behavioral Nutrition and Physical Activity, 8(1), 115. https://doi.org/10.1186/1479-5868-8-115
- McEwen, B. S. (2005). Stressed or stressed out: What is the difference? Journal of Psychiatry & Neuroscience: JPN, 30(5), 315–318.
- Min, M. O., Minnes, S., Kim, H., & Singer, L. T. (2013). Pathways linking childhood maltreatment and adult physical health. Child Abuse & Neglect, 37(6), 361–373. https://doi.org/10.1016/j.chiabu.2012.09.008
- Monnat, S. M., & Chandler, R. F. (2015). Long term physical health consequences of adverse childhood experiences. The Sociological Quarterly, 56(4), 723–752. https://doi.org/10.1111/tsq.12107
- Newsom, J. T., Huguet, N., McCarthy, M. J., Ramage-Morin, P., Kaplan, M. S., Bernier, J., McFarland, B. H., & Oderkirk, J. (2012). Health behavior change following chronic illness in middle and later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67(3), 279–288. https://doi.org/10.1093/geronb/gbr103
- Norman, R. E., Byambaa, M., De, R., Butchart, A., Scott, J., Vos, T., & Tomlinson, M. (2012). The long-term health consequences of child physical abuse, emotional abuse, and neglect: A systematic review and meta-analysis. PloS Medicine, 9(11), e1001349–e1001349. https://doi.org/10.1371/journal.pmed.1001349
- Penninx, B. W. J. H., Beekman, A. T. F., Smit, J. H., Zitman, F. G., Nolen, W. A., Spinhoven, P., Cuijpers, P., De Jong, P. J., Van Marwijk, H. W. J., Assendelft, W. J. J., Van Der Meer, K., Verhaak, P., Wensing, M., De Graaf, R., Hoogendijk, W. J., Ormel, J., Van Dyck, R., & Consortium, N. R. (2008). The Netherlands study of depression and anxiety (NESDA): Rationale, objectives and methods. International Journal of Methods in Psychiatric Research, 17(3), 121–140. https://doi.org/10.1002/mpr.256
- Petruccelli, K., Davis, J., & Berman, T. (2019). Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse & Neglect, 97, 104127. https://doi.org/10.1016/j.chiabu.2019.104127
- Ramiro, L. S., Madrid, B. J., & Brown, D. W. (2010). Adverse childhood experiences (ACE) and health-risk behaviors among adults in a developing country setting. Child Abuse & Neglect, 34(11), 842–855. https://doi.org/10.1016/j.chiabu.2010.02.012
- Robins, L. N., Wing, J., Wittchen, H. U., Helzer, J. E., Babor, T. F., Burke, J., Farme, A., Jablenski, A., Pickens, R., Regier, D. A., Sartorius, N., & Towle, L. H. (1988). The composite international diagnostic interview. An epidemiologic instrument suitable for use in conjunction with different diagnostic systems and in different cultures. Archives of General Psychiatry, 45(12), 1069–1077. https://doi.org/10.1001/archpsyc.1988.01800360017003
- Roche, A. I., Kroska, E. B., Miller, M. L., Kroska, S. K., & O’Hara, M. W. (2019). Childhood trauma and problem behavior: Examining the mediating roles of experiential avoidance and mindfulness processes. Journal of American College Health, 67(1), 17–26. https://doi.org/10.1080/07448481.2018.1455689
- Rodgers, C., Lang, A., Laffaye, C., Satz, L., Dresselhaus, T., & Stein, M. (2004). The impact of individual forms of childhood maltreatment on health behavior. Child Abuse & Neglect, 28(5), 575–586. https://doi.org/10.1016/j.chiabu.2004.01.002
- Romano, E., Babchishin, L., Marquis, R., & Fréchette, S. (2015). Childhood maltreatment and educational outcomes. Trauma, Violence & Abuse, 16(4), 418–437. https://doi.org/10.1177/1524838014537908
- Santini, Z. I., Jose, P. E., York Cornwell, E., Koyanagi, A., Nielsen, L., Hinrichsen, C., Meilstrup, C., Madsen, K. R., & Koushede, V. (2020). Social disconnectedness, perceived isolation, and symptoms of depression and anxiety among older Americans (NSHAP): A longitudinal mediation analysis. The Lancet: Public Health, 5(1), e62–e70. https://doi.org/10.1016/s2468-2667(19)30230-0
- Schonning, V., Sivertsen, B., Hysing, M., Dovran, A., & Askeland, K. G. (2022). Childhood maltreatment and sleep in children and adolescents: A systematic review and meta-analysis. Sleep Medicine Reviews, 63, 101617. https://doi.org/10.1016/j.smrv.2022.101617
- Spinhoven, P., Penninx, B. W. J. H., Hickendorff, M., van Hemert, A. M., Bernstein, D. P., & Elzinga, B. M. (2014). Childhood trauma questionnaire: Factor structure, measurement invariance, and validity across emotional disorders. Psychological Assessment, 26(3), 717–729. https://doi.org/10.1037/pas0000002
- Springer, K. W., Sheridan, J., Kuo, D., & Carnes, M. (2003). The long-term health outcomes of childhood abuse. An overview and a call to action. Journal of General Internal Medicine, 18(10), 864–870. https://doi.org/10.1046/j.1525-1497.2003.20918.x
- Strathearn, L., Giannotti, M., Mills, R., Kisely, S., Najman, J., & Abajobir, A. (2020). Long-term cognitive, psychological, and health outcomes associated with child abuse and neglect. Pediatrics, 146(4), e20200438. https://doi.org/10.1542/peds.2020-0438
- Sullivan, K., Rochani, H., Huang, L. T., Donley, D. K., & Zhang, J. (2019). Adverse childhood experiences affect sleep duration for up to 50 years later. Sleep, 42(7), zsz087. PMID: 31281929. https://doi.org/10.1093/sleep/zsz087
- Swendsen, J. D., & Merikangas, K. R. (2000). The comorbidity of depression and substance use disorders. Clinical Psychology Review, 20(2), 173–189. https://doi.org/10.1016/S0272-7358(99)00026-4
- Thompson, S. G. (1994). Systematic review: Why sources of heterogeneity in meta-analysis should be investigated. BMJ, 309(6965), 1351–1355. https://doi.org/10.1136/bmj.309.6965.1351
- van Mill, J. G., Vogelzangs, N., van Someren, E. J. W., Hoogendijk, W. J. G., & Penninx, B. W. J. H. (2013). Sleep duration, but not insomnia, predicts the 2-year course of depressive and anxiety disorders. The Journal of Clinical Psychiatry, 75(2), 119–126. https://doi.org/10.4088/JCP.12m08047
- von Hippel, P. T. (2020). How many imputations do you need? A two-stage calculation using a quadratic rule. Sociological Methods & Research, 49(3), 699–718. https://doi.org/10.1177/0049124117747303
- Widom, C. S., Horan, J., & Brzustowicz, L. (2015). Childhood maltreatment predicts allostatic load in adulthood. Child Abuse & Neglect, 47, 59–69. https://doi.org/10.1016/j.chiabu.2015.01.016
- Wiersma, J., Hovens, J., Oppen, P., Giltay, E., Schaik, D., Beekman, A., & Penninx, B. W. J. H. (2009). The importance of childhood trauma and childhood life events for chronicity of depression in adults. The Journal of Clinical Psychiatry, 70(7), 983–989. https://doi.org/10.4088/JCP.08m04521
- Williamson, D. F., Thompson, T. J., Anda, R. F., Dietz, W. H., & Felitti, V. (2002). Body weight and obesity in adults and self-reported abuse in childhood. International Journal of Obesity and Related Metabolic Disorders, 26(8), 1075–1082. https://doi.org/10.1038/sj.ijo.0802038
- Zhai, L., Zhang, H., & Zhang, D. (2015). Sleep duration and depression among adults: A meta‐analysis of prospective studies. Depression and Anxiety, 32(9), 664–670. https://doi.org/10.1002/da.22386
