Abstract
Background: There is growing interest in enabling older adults’ occupational performance. We tested whether 11 weeks of intensive client-centred occupational therapy (ICC-OT) was superior to usual practice in improving the occupational performance of home-dwelling older adults.
Methods: An assessor-masked randomized controlled trial among adults 60 + with chronic health issues, who received or applied for homecare services. Recruitment took place September 2012 to April 2014. All participants received practical and personal assistance and meal delivery as needed. In addition, they were randomized to receive either a maximum 22 sessions of occupation-based ICC-OT (N = 59) or to receive usual practice with a maximum three sessions of occupational therapy (N = 60). The primary outcome was self-rated occupational performance assessed with the Canadian Occupational Performance Measure (COPM).
Results: No important adverse events occurred. ICC-OT was accepted by 46 participants (88%), usual practice by 60 (100%). After 3 months, the ICC-OT-group had improved 1.86 points on COPM performance; the Usual-Practice group had improved 0.61 points. The between-group difference was statistically significant (95% confidence interval 0.50 to 2.02), t-test: p = 0.001.
Conclusions: ICC-OT improved older adults’ occupational performance more effectively than usual practice. This result may benefit older adults and support programmatic changes.
Introduction
In Denmark, as in many other countries, promoting older adults’ ageing in place is a major aim supported by policy makers and service providers, who anticipate dramatic increases in welfare costs due to ongoing demographic changes [Citation1–3]. In addition, there is growing interest in transferring some of the traditional passive services for older adults to rehabilitation, in an attempt to maintain older adults’ functional ability and to enable their occupational performance and wellbeing [Citation1–3]. In Denmark, most older adults live alone or with a spouse; 33% of 65–79 year-olds and 66% of 80+ year-olds live alone [Citation4]. Danish elder care, including rehabilitation, is a universal service; the responsibility lies at the local level in the municipalities, and all older adults have access free of charge, when certain criteria are met [Citation3]. A Danish national report sums up possibilities and challenges regarding older adults’ participation in rehabilitation [Citation5]. The report is informed by a number of evaluations based on interviews with older adults. To be able to reestablish one’s previous level of functioning was a general aim and motivational factor among the participants of the evaluations. The same pertained to a wish to live independently, especially managing one’s personal care alone. The wish to be independent with regard to housekeeping was less strong. Indeed, older adults who felt lonely were generally less interested in becoming independent, as they feared they would be deprived of their homecare assistants [Citation5].
Occupational therapy (OT) is a valued and well-integrated profession within rehabilitation for older adults [Citation6–9]. In the rehabilitation context of Danish municipalities, home-based OT is typically delivered to older adults in one of two ways: (1) As a comprehensive client-centred OT intervention building on the older adults’ own goals and planned and delivered by occupational therapists through the full period of rehabilitation, in some cases as part of a multidisciplinary approach [Citation10,Citation11], or (2) As an element of homecare re-ablement where occupational therapists work as consultants to the homecare personnel [Citation10].
The core of OT is to enable clients’ occupational performance and wellbeing [Citation12,Citation13]. Occupational performance may be improved through occupation-based OT where occupation acts as both means and end. Typically, acquisitional, adaptive and restorative intervention models are used, and the occupations, which the older adults want or need to do, are addressed in a client-centred process [Citation13–16]. Client-centred practice within OT is defined by the Canadian Association of Occupational Therapists as collaborative approaches aimed at enabling occupation with clients [Citation17]. It is stressed that in client-centred practice:
Occupational therapists demonstrate respect for clients, involve clients in decision-making, advocate with and for clients in meeting clients’ needs, and otherwise recognize clients’ experience and knowledge [Citation17].
Client-centred OT is generally valued and practised within Danish OT, and the Canadian Occupational Performance Measure (COPM), which supports this practice, is widely used in Danish municipalities [Citation18]. Client-centredness holds a high priority in Danish OT curricula, informed by Canadian and US conceptual and practice models and outcome measures [Citation13,Citation14,Citation17,Citation19,Citation20]. Gupta and Taff [Citation21] have argued that client-centred practice is best embodied by occupation-focused interventions in the natural environment of everyday living. This supports the provision of OT in and around the client’s home. Challenges in client-centred practice have been identified at the level of the healthcare system [Citation22]. In Denmark, homecare re-ablement for older adults is becoming increasingly wide spread [Citation23]. A client-centred approach to homecare re-ablement is supported by law through the consolidating act on social services, which emphasizes cooperation with the client and building on the client’s individual goals [Citation10]. Nevertheless, at the time the present study was carried out, Danish occupational therapists’ client-centred values and practices were challenged. Local policies in many Danish municipalities downplayed individual goal-setting by limiting the focus of homecare re-ablement to the performance of tasks and activities for which the older adults would otherwise be eligible to receive help. The aim was to save municipal homecare costs. In addition, the amount of OT within homecare re-ablement was in some municipalities limited to a few visits or no OT at all, and the re-ablement was mainly carried out by homecare assistants. This situation is what we refer to as ‘usual practice’ (as opposed to client-centred) in the present study.
Occupational therapists are obliged to work in an evidence-based manner [Citation24]. Yet there is a paucity of quality intervention literature, and client-centred and home-based OT for older adults has not previously been tested in a Danish context. A recent systematic literature review identified only a small number of high-quality studies concerning home-based and occupation-based OT [Citation25]. The studies were predominantly European and North American, and the interventions were with older adults post stroke, with Parkinson’s disease, or with various chronic health issues [Citation25]. While OT was found to effectively improve occupational performance within the domains of self-care, productivity, and client-identified occupations [Citation26–31], small effect sizes were reported in several studies [Citation26,Citation27,Citation31], and there were problems with maintaining the achieved improvements after discharge [Citation27,Citation29]. The amount of OT in the studies ranged from two to nine sessions [Citation25]. However, the authors did not examine the relationship between amount and outcome. Previous studies have shown that a larger amount of OT and physiotherapy could improve clients’ outcomes in inpatient settings, and that the amount of OT was frequently far too small to be effective [Citation32–34]. There is therefore a need to test the effect of in-home interventions that are more intensive than those reported in the above-mentioned literature review. Furthermore, many older adults who receive home-based services are affected by a range of chronic and often concurrent health issues and have very different needs. Accordingly, it is important to examine the effectiveness, over time, of intensive, client-centred occupation- and home-based OT targeting diverse populations.
Objectives and hypotheses
The objective of this study was to compare 11 weeks of occupation-based intensive client-centred OT (ICC-OT) in the homes of older adults to the usual practice in one Danish municipality. One primary hypothesis was formulated:
Primary hypothesis: ICC-OT will be superior to usual practice in improving the participants’ self-rated occupational performance, measured as the change between the assessments at baseline and 3 months post baseline.
Secondary hypotheses were formulated, building on our expectations that the ICC-OT would outperform usual practice on three counts: participants’ would be more satisfied with the occupational performance (Secondary hypothesis 1); the observed quality of occupational performance would be higher (motor abilities and process abilities, Secondary hypothesis 2 and 3); and health-related quality of life would be increased (physical components and mental components, Secondary hypothesis 4 and 5), measured as the changes in these variables between the assessments at baseline and 3 months post baseline.
Finally, we expected that the improvements on each of the six above-mentioned outcomes would be maintained 6 months later, i.e. compared with baseline, the ICC-OT group would fare better than the Usual-Practice group (Secondary hypothesis 6 to 11). ( refers to the numbered hypotheses).
Methods
A randomized controlled parallel group superiority trial was performed with an allocation ratio of 1:1 to ICC-OT or usual practice, and assessor-masked assessments at baseline, and at 3 and at 6 months, post-baseline.
Setting and standard services
The study took place in The Municipality of Randers (Randers Kommune), a Danish municipality of 97,500 inhabitants, of which 25% were 60+ years old [Citation35]. Personal care, practical help, meal delivery, OT, homecare re-ablement, physiotherapy, assistive devices and minor home modifications were the responsibility of a municipal homecare office. The services were offered free of charge to home-dwelling older adults with functional limitations when specified requirements were met [Citation10]. Participants in both study groups were eligible for these standard services. The only differences in services pertained to OT and homecare re-ablement.
presents details concerning the rehabilitative services received in the trial period. Within the first 3 months, more participants in the ICC-OT group than in the Usual-Practice group received assistive devices and minor home modifications (24 vs. nine), chi-square test: p = 0.002.
Table 1. Details concerning the received rehabilitative services in the trial period.
Participants
Included in the study were older men and women aged 60+. They experienced occupational performance problems and were therefore applying for, or already receiving, homecare services. They lived in private homes or in sheltered housing and were able to communicate in Danish. Excluded were older adults with physician-ascertained alcohol or drug abuse, tetraplegia, dementia, severe mental illness or severe intellectual disability. Also excluded were older adults who had severe pain and/or rapidly progressive diseases such as cancer or motor neuron disease. These criteria assured that participants in the study were similar to those who would usually be considered for rehabilitation. Further exclusion criteria were: having a rehabilitation plan from a hospital, previous participation in homecare re-ablement, or living with a participant of the present study.
Enrolment and randomization
A homecare officer at a central municipal office invited older adults to participate in the study when the older adults applied for homecare for the first time or were about to have their needs reevaluated. Initial information was given by means of a standardized telephone-protocol. Research occupational therapists visited the older adults, checked eligibility criteria and gave oral and written information. Willing participants gave written informed consent and went through the baseline assessments. Finally, a homecare officer assigned the participants to the ICC-OT or usual practice arm of the study. The officer followed a computerized randomization procedure generated by a data management team. Block randomization produced balanced study arms. The block sizes and the random allocation sequence were concealed until all participants were assigned to their groups. Recruitment took place from 1 September 2012 to 30 April 2014. The last follow-up was performed 31 October 2014.
Intensive client-centred occupational therapy (ICC-OT)
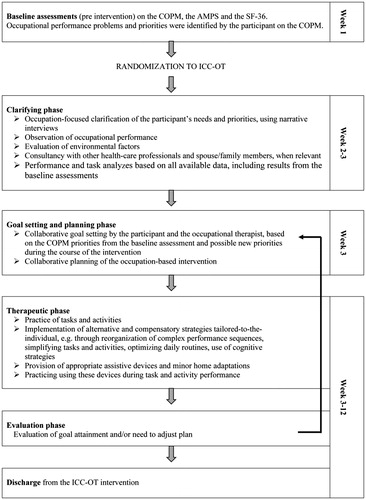
depicts the characteristics of the ICC-OT intervention performed by the research occupational therapist. The ICC-OT took place in and around the participants’ homes and in other environments of the local community, as appropriate given the participants’ performance issues and goals. One research occupational therapist was assigned to each participant. Key points in the ICC-OT that reflected the client-centred approach [Citation13,Citation19] included respecting the older adults’ individual life styles; seeking, respecting and addressing their priorities and choices concerning the focus of the OT intervention; working collaboratively on goal-setting and during the intervention; and assessing the older adult’s performance with an individualized client-centred outcomes measure before and after the intervention. It was possible to change the original goals and to work on new/additional goals if such should evolve during the process.
The protocol (see ) specified up to 11 weeks of ICC-OT (Week 2 to 12) with two sessions per week and a maximum of 22 sessions. The aim of the ICC-OT was to improve occupational performance. Occupations, named and prioritized on the COPM [Citation20] by the participants at the baseline assessment, were targeted. Goal-setting took place Week 3; the goals addressed improving occupational performance within the self-care, productivity and leisure domains. The therapeutic phase (Week 3 to 12) to a large degree involved practising the necessary tasks and activities to achieve the goals. The ICC-OT was tailored to the individual and built on acquisitional, adaptive and restorative models [Citation14]. During the 11 weeks of ICC-OT, no other OT was available to the participants in this group. In Week 13, the participants went through the 3-month assessment. They then received usual practice for the last 3 months of their participation in the study, until the 6-month assessment.
presents details concerning received ICC-OT in the trial period. At group level, the occupations worked on during the ICC-OT were fairly evenly distributed on self-care (32%), productivity (39%) and leisure (29%). The most frequent occupations worked on were, for self-care: dressing, bathing, grocery shopping and functional mobility; for productivity: cleaning, cooking and laundry; and for leisure: hobbies, walks and visiting friends. The occupation-based approach was reflected by the choice of intervention models. Aquisitional models were used 55% of the time, adaptive models 41% of the time and restorative models 4% of the time. One adverse event was reported: a participant cut himself with a knife during a kitchen activity.
Usual practice
Participants in the Usual-Practice group received no input from the research occupational therapists. From Week 2, it was possible (though not mandatory) for the participants to be referred to homecare re-ablement. This was a part of the usual practice of the municipality and was initiated when the homecare officers considered that the participants had potential for improvement in tasks or activities for which they would otherwise require help. Homecare re-ablement took place in the home and lasted up to 3 weeks. It could include three visits by a municipal occupational therapist but was mainly performed by homecare assistants. The tasks and activities that could be worked on were restricted to the areas of self-care and household management. It was not a specific, client-centred approach, and the participants could not choose freely what to work on. The participants performed the tasks and activities, and the assistants gave advice and help when needed, e.g. on how to simplify a task or use an assistive device. The homecare re-ablement staff had no access to the results of the baseline assessments. Thirteen weeks (3 months) after baseline, the participants went through the 3-month assessment and continued receiving usual practice for the last 3 months of their participation in the study, until the 6-month assessment.
presents details concerning received usual practice in the trial period. No documentation was available concerning the exact tasks and activities addressed when participants of the Usual-Practice group had OT.
Outcome measurements and their application in the study
Occupational performance and health-related quality of life were measured at baseline, at the 3-month assessment and at the 6-month assessment. No changes to trial outcomes were made after the trial commenced.
The primary outcome was self-rated occupational performance (Primary hypothesis); this was assessed by the Danish version of the Canadian Occupational Performance Measure (COPM) [Citation20], which is a semi-structured, interview-based outcome measure designed to identify and prioritize occupational performance issues and assess change [Citation20]. The COPM was chosen to match the client-centred focus of the ICC-OT intervention. It helps clients to formulate and evaluate their most important occupations and performance issues and thus supports individual goal-setting and interventions towards client-chosen goals [Citation36]. The COPM has been validated in many populations, including a population of Danish older adults in home settings [Citation18,Citation37]. The primary hypothesis addressed the change from baseline to 3 months. Change from baseline to 6 months was addressed in Secondary hypothesis 6. The participants of the present study prioritized and chose up to five occupational performance problems, and they scored their ability to perform each of these occupations using the numerical, 10-point rating scale of the COPM. A summary score (mean value of all five performance ratings) was computed, and this COPM performance score, ranging from 1 to 10, was used for analysis. At the 3-month and the 6-month assessments, the participants rescored the same occupations without being shown their earlier scores. If fewer problems were rescored than scored at baseline, the summary score was computed with the actual number of rescored occupations, as suggested in the COPM manual. A minimal clinically important difference (MCID) of 2 points for both COPM scores has been suggested for all populations [Citation37], yet an MCID of 1.4 points has been suggested for the COPM performance score based on a study in a group of adults with various health problems [Citation38].
The secondary outcomes were self-rated performance satisfaction, observer-rated performance quality, and health-related quality of life.
Self-rated performance satisfaction (Secondary hypothesis 1 and 7) was assessed on the satisfaction scale of the COPM after the identification of problems and scoring of performance. Again, the COPM numerical scale from 1 to 10 was used [Citation20]. The COPM satisfaction score, ranging from 1 to 10, was scored and rescored in a similar fashion to the performance score, as explained above.
Performance quality (Secondary hypothesis 2, 3, 8, and 9) was assessed on the motor and process scales of the observation-based and standardized Assessment of Motor and Process Skills (AMPS) [Citation39,Citation40]. This assessment has been validated in many populations, including older adults, and in home settings [Citation39,Citation41–43]. The AMPS measures the degree to which a person’s task performance is free of increased clumsiness or physical effort, decreased efficiency, safety risk, and/or need for assistance. The participants in the present study were observed during the performance of two chosen personal or domestic activities. The raw item scores were converted into one linear ADL motor ability measure (AMPS motor score, Secondary hypothesis 2 and 8), and into one linear ADL process ability measure (AMPS process score, Secondary hypothesis 3 and 9) [Citation44]. The many-facet Rasch model of the AMPS allows for missing scores when calculating the ability measures [Citation44]. The scales range from −3 to 4 logits [Citation39,Citation40]. An MCID of 0.3 points has been recommended [Citation39] Assessors must be trained and calibrated to use the AMPS test. To ensure validity in the present study, a post-hoc analysis of the AMPS assessments was performed at Center for Innovative OT Solutions [Citation45]. Two hundred sixty-three assessments (97% of all the performed assessments) were deemed free of rater scoring error and included in the statistical analyses. Nine assessments (3%) were excluded. In accordance with the AMPS manual, the assessors also reported up to three diagnoses per participant found to substantially affect his or her occupational performance [Citation39,Citation40].
Health-related quality of life (Secondary hypothesis 4, 5, 10 and 11) was assessed using the Danish version of the standardized 36-item short-form health survey (SF-36), Version 1.1 [Citation46,Citation47]. The SF-36 has been validated in many populations, including a population of older Danish adults, and in home settings [Citation46–50]. The questionnaire was used in an interview setting [Citation50]. The software computed eight subscales and two summary measures. For the present study, the General Health subscale (SF-36 GH), the physical component summary (PCS, Secondary hypothesis 4 and 10) and the mental component summary (MCS, Secondary hypothesis 5 and 11) were calculated and transformed to scales ranging from 0 to 100. The software imputed missing values if conditions applied [Citation51]. MCIDs of 3 to 5 points have been suggested in the literature [Citation52].
Participant information concerning received help, health issues, and sociodemographic data were collected using the central municipal administrative registers and by asking the participants themselves. A standardized form was created for this purpose.
Occupational therapists
In all, six registered occupational therapists were involved in the assessments and the ICC-OT intervention: two full-time research occupational therapists and four part-time assessors. All were educated in Denmark and had worked eight to 23 years with rehabilitation of Danish older adults. All were experienced users of the COPM and the AMPS. They participated in two 5-hour workshops before the study started, followed up by regular workshops and team meetings. This was done to further improve their intervention and assessment skills, to explain the trial procedures, and to improve adherence to the protocol. Definitions, perceptions and practices related to client-centred practice [Citation13,Citation19] were often discussed. This was done because it has been found in rehabilitation settings, that although occupational therapists described their own practice as being client-centred, their clients had experienced only little or no active involvement in goal setting and no awareness of a ‘client-centred approach’ [Citation53]. In addition, the first author, also an experienced occupational therapist, was available for questions and discussions throughout the study period. An expert on the AMPS organized three workshops with the occupational therapists and was available for questions throughout the study period.
The two research occupational therapists performed the baseline assessments and delivered the ICC-OT. They filled out a standard client record after each session of ICC-OT to record date, duration, and brief details about the tasks and activities worked on, whether acquisitional, adaptive or restorative approaches were used, and which assistive devices were introduced. They also recorded any harms or unintended effects. They did not interact with any occupational therapists who served the Usual-Practice group. The four assessors were assigned by convenience to perform the 3-month and the 6-month assessments. None of the assessors had delivered homecare re-ablement to the older adults that they assessed.
Masking
The study was assessor-masked (single blind). The baseline assessments were carried out before randomization. The assessors who undertook the 3- and 6-month assessments were not informed about the participants’ allocation status or their results from previous assessments. The participants could not be masked at the 3- and 6-month assessments but were urged not to discuss their allocation status with their assessors, and they were not shown the results of their previous assessments.
Data management and statistical methods
The sample size was based on an MCID of 2 points on the COPM [Citation37], a standard deviation (SD) of 2.22 [Citation54], an alpha level of 0.05, and a power of 80%. Twenty participants in each group were required. Allowing for a 20% attrition rate [Citation55] and with the wish to perform several secondary analyses, the study aimed at including 120 participants. To ensure a reliable dataset, data were entered twice in Epi-data [Citation56] by two independent researchers. In the case of an incongruence, the original data form was consulted to establish the correct result. Stata 12 was used for the analyses [Citation57]. The significance level was set at 0.05. The analyses were performed by original assigned groups (intention-to-treat) on all available data. At baseline, data were presented per randomized group by mean and SD or number and percentage. The between-group differences in change from baseline to 3 months and from baseline to 6 months on the COPM performance, COPM satisfaction, the AMPS and the SF-36 were presented with 95% confidence intervals (CIs) and tested with t-tests for independent samples. The within-group changes from baseline to 3 months and from baseline to 6 months were presented with SDs and tested with t-tests for paired samples. Exploratory multiple linear regression analyses were used to adjust the primary outcome for possible assessor influence, and to explore possible effect modification concerning age, general health and sex. Chi-square tests and tests for trend were used to analyze categorical and ordinal outcomes. Correlations between two outcomes were explored by Spearman’s rho.
Ethics
Laws and regulations according to the Declaration of Helsinki were followed, and special attention was drawn to consent and confidentiality [Citation58]. Informed consent was given by all participants, and the study was approved by the Danish Data Protection Agency (trial identifier Jnr 2012-52-0049). The Scientific Ethics Committee of Central Denmark Region deemed the study not to fall under the category biomedical research, and further ethical approval was therefore not required (query number 153/2012). The article complies with the CONSORT statement for transparent reporting [Citation59].
Trial registration
The study was registered through Current Controlled Trials, trial identifier ISRCTN93873801 DOI 10.1186/ISRCTN93873801 [Citation60]. No important changes were made to methods after trial commencement.
Results
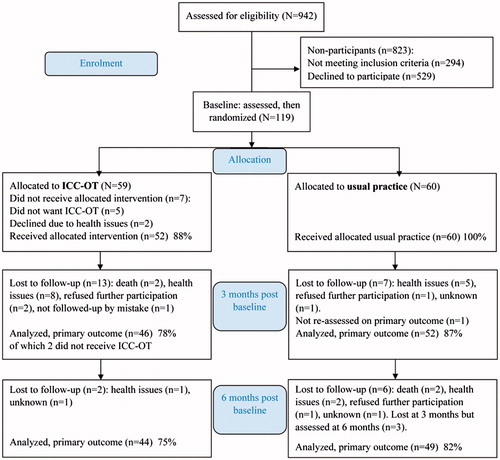
illustrates the participant flow. Of the 942 older adults assessed for eligibility, 119 finally enrolled (take-up rate 18%). The most common reasons given for not participating were directly related to health issues or expressed as an anticipation that participation would be too onerous. Some older adults did not have any problems that they wanted to work on. Non-participants were on average 4.4 years older than participants (95% CI 2.76 to 6.05), t-test: p < 0.001. There was no difference in sex distribution, chi-square test: p = 0.74. The between-group differences in numbers lost to follow-up at 3 months and at 6 months were not statistically significant, chi-square test: p = 0.21 and 0.35, respectively.
presents demographics and baseline measurements for both groups. All experienced some difficulty with their occupational performance at baseline. Participants in the ICC-OT group received 43 minutes (median) of personal care and/or practical help per week, and participants in the Usual-Practice group received 34 minutes (median) per week, Wilcoxon’s rank sum test: p = 0.46. The participants’ SF-36 GH (General Health) score was significantly lower in both groups than the score of 62.55 (SD 22.5) derived from Danish norm data for men and women 75 + years old [Citation47], t-test: p < 0.001. Those who were lost to follow-up at the 3-month assessment had somewhat poorer perceived general health at baseline than those who were reassessed. They did not differ on other demographics and baseline measurements. All participants had at least one health issue, which substantially affected their occupational performance. The 215 health issues reported at baseline were assigned to the following categories [Citation39,Citation40]: ‘orthopaedic/musculoskeletal’ 109 (51%), ‘medical’ 51 (24%), ‘neurologic stroke/nonstroke’ 30 (14%), ‘sensory/falls’ 14 (6%), ‘psychiatric’ nine (4%), ‘impairment of learning’ one (0.5%), and ‘unknown’ one (0.5%).
Table 2. Demographics and baseline measurements for both groups.
Primary hypothesis, change from baseline to the 3-month assessment on COPM performance
shows that the primary hypothesis of the study was confirmed, as the ICC-OT group improved their COPM performance from baseline to the 3-month assessment statistically significantly more than the Usual-Practice group: difference 1.26 points (95% CI 0.50 to 2.02), t-test: p = 0.001.
Table 3. Occupational performance and health related quality of life. Within-group changes and between group differences in change.
An exploratory multiple linear regression analysis adjusting for assessors at baseline and at the 3-month assessments, revealed a slightly smaller difference: 1.12 points (95% CI 0.35 to 1.89), p = 0.005. The between-group difference in means on the COPM performance score at the 3-month assessment was explored, too; the conclusions remained similar to the primary analyses on change-scores. (This explorative analysis was applied to all hypotheses. The results as well as the mean scores on all outcomes at 3 and 6 months are found in Appendix 1).
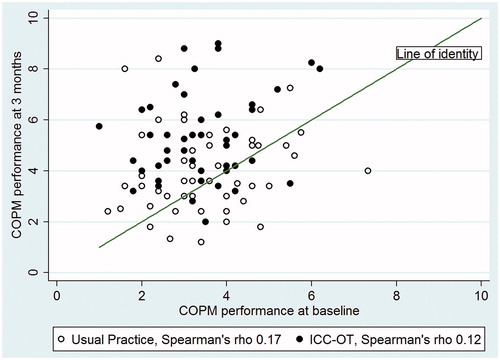
illustrates the main result: The COPM performance scores were, in general, higher at the 3-month assessment than at baseline, and this was mostly due to improvements in the ICC-OT group. Low correlations were found between baseline and 3-month scores: ICC-OT group, Spearman’s rho: 0.12, p = 0.43, Usual-Practice group, Spearman’s rho: 0.17, p = 0.17.
also presents the within-group changes from baseline to 3 months. A closer examination of these changes revealed statistically significant improvements in the mean scores within both groups. Exploratory analyses at participant level concerning an MCID of 2 points on the COPM performance score were carried out. The analyses showed that in the ICC-OT group 22 participants (48%) improved and one (2%) declined, while in the Usual-Practice group eight (15%) improved and four (8%) declined. A similar analysis concerning an MCID of 1.4 points showed that in the ICC-OT group 28 participants (61%) improved and two (4%) declined, while in the Usual-Practice group 18 (35%) improved and seven (13%) declined. Tests for trend confirmed that statistically significantly more participants in the ICC-OT group than in the Usual-Practice group improved their COPM performance by an MCID of 2 points or more, p < 0.001, and by an MCID of 1.4 points or more, p = 0.007.
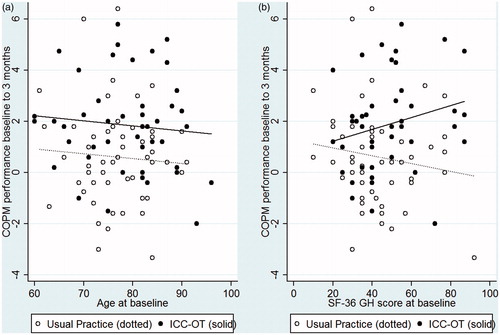
illustrates exploratory analyses conducted concerning age and general health in relation to COPM performance, using multiple linear regression. Age did not modify the between-group differences in change from baseline to 3 months in COPM performance, p = 0.99, and age did not independently influence the change, p = 0.42 (see ). In contrast, general health at baseline tended to modify the between-group differences in change, seen as the different directions of the slopes in . However, the slopes were not statistically significantly different, p = 0.073. The between-group difference in change among participants with an SF-36 GH score from 50 and up was 2.11 points (95% CI 0.92 to 3.31), whereas among participants with an SF-36 GH score below 50 the difference was only 0.59 points (95% CI -0.42 to 1.60). However, the differences in change between participants with higher and lower general health were not statistically significant, p = 0.057.
Figure 4. (a,b) Exploratory analyses of age and health status' influence on change in COPM from baseline to 3 months.
An exploratory regression analysis concerning sex (not illustrated) showed that the between-group difference in change from baseline to 3 months in COPM performance was 1.77 points (95% CI 0.35 to 3.19) in men and 1.04 points (95% CI 0.13 to 1.95) in women. Nevertheless, this difference between men and women was not statistically significant, p = 0.39. Sex did not independently influence the change: the difference in change between men and women was 0.12 points (95% CI −0.71 to 0.96), p = 0.77.
Secondary hypotheses, changes from baseline to 3 months and to 6 months
shows that at 3 months, no between-group differences in change were found concerning any of the secondary hypotheses (Secondary hypothesis 1 to 5). The within-group improvements in COPM satisfaction and on the AMPS motor scale were statistically significant in both groups. Changes from baseline to 6 months in COPM performance (Secondary hypothesis 6), COPM satisfaction (Secondary hypothesis 7) and on the AMPS motor scale (Secondary hypothesis 8) were statistically significantly larger in the ICC-OT group than in the Usual-Practice group.
Discussion
The primary hypothesis regarding the effectiveness of ICC-OT in the home was confirmed: ICC-OT significantly improved the participants’ own perceptions of their occupational performance compared to usual practice. This principal finding is consistent with previous studies of the effect of occupation-based OT in the homes of older adults with stroke, Parkinson’s disease or multiple chronic health issues [Citation26,Citation28–31]. The initial COPM performance score () was close to findings in other European studies among home-dwelling older adults [Citation31,Citation61,Citation62]. The between-group difference in improvement at 3 months on COPM performance of 1.26 points in the present study () was comparable to a between-group difference in improvement of 1.2 points found in a Dutch study of occupation-based OT for older adults with Parkinson’s disease [Citation31]. As older adults often perform activities of daily living near their maximal capabilities [Citation63], it may be hypothesized that even small improvements in occupational performance can be of importance to their everyday life. In the present study, the mean change in COPM performance at 3 months of 1.87 points in the ICC-OT group was close to or exceeding proposed MCIDs of 2 and 1.4 points [Citation37,Citation38], and a statistically significantly higher proportion of participants in the ICC-OT group than in the Usual-Practice group achieved these MCIDs. The importance of the principal findings on COPM performance in the ICC-OT group are also strengthened by concurrent improvements in COPM satisfaction that were close to an MCID of 2 points and by improvements on the AMPS motor scale that exceeded an MCID of 0.3 points [Citation39]. The latter result indicates that there had been an observable change in the participants’ quality of ADL task performance related to motor skills. The robustness of the outcome concerning our primary hypothesis is supported by the fact that the effectiveness pertained to both male and female participants and to participants of all ages (60 to 96 years). Thus, we have reason to believe that the achieved and statistically significant improvements in the ICC-OT group were of clinical and individual importance to a large number of the participants.
The ICC-OT was effective, even in a group where 80% of the participants were already receiving homecare services at the time of inclusion. A Danish economic evaluation of homecare re-ablement from 2016 suggested that this approach was more successful among first-time applicants for homecare than among older adults who had received homecare prior to homecare re-ablement [Citation64]. Therefore, as only 20% of the participants in the present study were first-time applicants, the effect would probably have been greater if more first-time applicants for homecare services had been included.
Six months post baseline, the achieved improvements were still larger in the ICC-OT group than in the Usual-Practice group. The between-group differences in improvement on COPM performance, COPM satisfaction, and the AMPS motor scale were also statistically significant in favor of the ICC-OT group. The positive results on the COPM at 6 months are in line with results of home-based OT for older adults with Parkinson’s disease [Citation31] and indicate that the strategies learned through OT can be successfully implemented in everyday life.
Our exploratory analysis indicated a larger effect of ICC-OT among participants who scored ≥50 on the SF-36 GH score at baseline. These findings should be further investigated, as it would be of help if older adults with a large potential for improvement from ICC-OT could be identified. In addition, our exploratory findings indicate a need to develop interventions for older adults with a smaller potential for improvement. In this subgroup, improved occupational performance may not be the only success criterion; maintenance of occupational performance may be an appropriate aim, too. Further research may show whether embedding periods of ICC-OT within homecare re-ablement programs and implementing a more nuanced definition of the aims could accommodate the rehabilitation needs of older adults at lower levels of general health.
Strengths and limitations
The validity of the results was strengthened by the randomized controlled design, the use of assessments validated for older populations, experienced occupational therapists, blinding of the assessors, and the educational workshops before and during the study. Meanwhile, the study also had some limitations.
The take-up rate of 18% was low. The refusers most often explained their decision with reference to their health. Nevertheless, refusers may have declined the ICC-OT treatment for several additional reasons. First, they may have been opposed to specific details about the ICC-OT. Second, they may have been disinclined to participate in a scientific study per se, either because their involvement implied repeated assessments or because they were uncertain whether they would be assigned to either of the two groups. Such barriers to participating in RCTs have previously been reported [Citation65], and a qualitative pilot study among older adults before the present study could have led to adjustments of the design, the content and the information material [Citation66]. This could possibly have resulted in a better take-up rate. Another reason for refusing participation in the study may be the fact, touched upon in the introduction, that some older adults feared that they would lose their homecare assistants if they should become independent as a result of the ICC-OT [Citation5].
The total loss to follow-up was 21.8% and highest among participants with lower general health. A large loss to follow-up is often seen in studies among older adults and may be difficult to avoid due to fluctuating health in this age group [Citation55]. The difference in loss to follow-up was not statistically significant between the two groups. Nevertheless, many refusers referred to health issues as their reason for not participating, and the difference in change from baseline to 3 months was smaller in the subgroup with low general health. Therefore, one may speculate that if more participants with low general health had participated in the study and completed the 3-month assessment, a smaller general effect may have been detected, suggesting that the participants had an intuitive self-sense as to whether they would benefit.
A large majority of the participants were living alone, the rest with a spouse. In many countries/cultures, it is more common for older adults to live with their family than it is in Denmark. An active buy-in of spouse or family was not emphasized in the ICC-OT; yet they could be included in the therapy if the older adult wished to. Other studies of home-based interventions for older adults have focused more on including primary caregivers [e.g. Citation30,Citation31], and future studies of ICC-OT may explore how the presence of family may influence the participants’ motivation and outcome.
In the Danish welfare state, services such as homecare, home-based OT, assistive devices etc. are free when older adults meet certain criteria [Citation10]. If the participants were required to pay for some of these services themselves, for instance assistive devices, they might have declined them, and consequently, the effect of the ICC-OT might have been smaller.
The participants in the present study were not blinded to their group allocation, since, as pointed out in other randomized controlled trials within rehabilitation, the behaviorally based intervention (the ICC-OT) required their active participation [Citation67]. To diminish the difference in the anticipation of ‘effect’ among the participants, we could have placed more emphasis on the fact that we tested two different approaches instead of stressing that we tested a special program versus usual practice [Citation68].
A warning has been raised that therapist’s and other health workers’ practices can be heavily influenced by discourses of ‘normal ageing’ linked to inevitable declines in physical and cognitive abilities, and with a heavy focus on the promotion of safety [Citation69], which may lead to not entirely client-centred practices. Such issues were discussed with the research occupational therapists throughout the present study. Nevertheless, the therapists’ individual experiences with rehabilitation of older adults and the fact that most participants were already receiving homecare services may have influenced the focus of the ICC-OT. Still, the breadth of activities worked on during ICC-OT, and the fact that many of the tasks and activities worked on could not be addressed through usual practice, suggest that the participants in the ICC-OT group were, indeed, given more free choice of goals than those in the Usual-Practice group, who received homecare re-ablement. This reflects the client-centred practice embedded in the ICC-OT [Citation13,Citation19].
The participants in the Usual-Practice group had also improved on the primary outcome at 3 months, although to a lesser degree than the ICC-OT group. No participants in the Usual-Practice group received ICC-OT, and measures were taken to avoid that the treatment principles of the ICC-OT should inspire occupational therapists working with the Usual-Practice group. Nevertheless, the initial COPM interview was performed with all participants before randomization, and it has been pointed out that this interview may have a therapeutic effect in itself, since it increases awareness and motivation [Citation31,Citation61]. Thus, a change process may also have started in the Usual-Practice group, which may have reduced the difference in outcome between the two groups.
The primary analysis was performed on the change scores between baseline and 3 months, as recommended in the COPM manual [Citation20]. This procedure is expected to create estimates of high precision. However, due to the low correlations between the baseline and 3-month scores in the present study, narrower confidence intervals were found on the between-group differences in 3-month scores than on the differences in change scores. Thus, if low correlations between baseline and 3-month scores on the COPM is a general trend, and if groups to be compared are expected to be similar at baseline, as in RCTs, higher statistical power can be obtained by comparing post intervention scores than change scores.
An issue worth discussing is how to interpret the results of an RCT within OT. The outcome measures COPM and AMPS were chosen to focus on problems relevant to the participants, in line with the client-centred approach of ICC-OT. A caveat concerning the COPM in relation to client-centredness has been expressed by Hammell [Citation70] who points out that the categorisations self-care, productivity and leisure were not derived from clients’ experiences and do not fully reflect clients’ experiences of occupational engagement and a meaningful life. As an answer to this, researchers may consider ways of supplementing the interpretation of attained changes in future studies, e.g. by including a qualitative evaluation to learn more about participants’ own perceptions of how achieved changes may affect their occupational engagement during and after the intervention [Citation66]. In the present RCT, two MCIDs were used to interpret the primary outcome concerning between-group differences in change as well as within-group improvements and individual changes. More research has been called for to examine MCIDs in relation to the COPM [Citation37,Citation38]. In addition, it has been questioned whether it is meaningful to infer the amount of change that is detectable or important to individuals based on a group average [Citation71]. Secondary outcomes were used to supplement the interpretation of the primary result. We did not assess whether the participants were becoming independent of help, as this was not the expressed aim of the ICC-OT. Yet it is a question of interest for municipal decision makers, who allocate scarce healthcare resources. We therefore recommend embedding concurrent economic evaluations in future RCTs addressing the effectiveness of OT in a homecare setting [Citation66]. No follow-up was performed after 6 months, and future studies may explore long-term effectiveness of ICC-OT.
Conclusions
In-home ICC-OT, in which older adults with various chronic health issues intensively practised the activities they valued the most for up to 11 weeks, supplemented by free access to assistive devices and minor home modifications, effectively improved their self-rated occupational performance at 3 months and 6 months post baseline. The participants’ satisfaction with their occupational performance also improved, as well as the observed quality of their occupational performance. The ICC-OT was effective regardless of sex or age, yet participants with the lowest general health improved to a lesser degree. The observation that there was still a benefit 6 months post baseline indicates that the improvements achieved and the strategies learned were successfully implemented in everyday life. The results may be generalized to home-dwelling older men and women aged 60+, who live alone or with a spouse in a Scandinavian homecare context and experience occupational performance problems due to various health issues.
Clinical implications
The results of the present study are an important contribution to the emerging evidence base concerning intensive and client-centred OT for older adults with occupational performance problems. These results should therefore be taken into consideration when planning rehabilitative OT services and homecare re-ablement for home-dwelling older adults.
Acknowledgements
The occupational therapists Karen Andersen, Anette Bjerring, Dorte Sølund Hansen, Karin Breiner Henriksen, Lene Ifversen, Jytte Jakobsen, Birgitte Krogh Jespersen, Zita Jespersgaard, Louise Møldrup Nielsen, Hanne Pedersen, Helle Søndergaard Thomsen, senior consultant Nils Høgel, and the steering committee from The Municipality of Randers and VIA University College are greatly acknowledged for their participation and support.
Disclosure statement
The authors report no conflicts of interest.
Additional information
Funding
References
- World Health Organization (WHO). World report on ageing and health. Geneva: WHO Press; 2015.
- Christensen K, Doblhammer G, Rau R, et al. Ageing populations: the challenges ahead. Lancet. 2009;374:1196–1208.
- Fersch B. Expectations towards home care re-ablement in Danish municipalities. Int J Soc Social Policy. 2015;35:126–140.
- AEldre Sagen. AEldre i tal 2017. [Older adults in numbers 2017]. Copenhagen: AEldre Sagen; 2017. [in Danish].
- Hansen EB. AEldres Deltagelse i Hverdagsrehabilitering: Muligheder Og Udfordringer [Older adults’ participation in home-care re-ablement – possibilities and challenges]. Copenhagen: KORA; 2015. [in Danish].
- Atwal A, McIntyre A, editors. Occupational therapy and older people. 2nd ed. Chichester: Blackwell Publishing Ltd; 2013.
- Lewis SC. Elder care in occupational therapy. Thorofare (NJ): SLACK Incorporated; 2003.
- Mountain G. Occupational therapy with older people. London: Whurr Publishers Ltd; 2004.
- Law M, McColl MA. Interventions, effects, and outcomes in occupational therapy. Adults and older adults. Thorofare (NJ): SLACK Incorporated; 2010.
- Indenrigsministeriet. 2015a. Bekendtgørelse af lov om social service (serviceloven) [Consolidating act on social services]. LBK nr. 1053 af 08/09/2015. [in Danish].
- Ministeriet for Sundhed og Forebyggelse. 2014a. Bekendtgørelse af sundhedsloven. [Consolidating health act]. LBK nr. 1202 af 14/11/2014. [in Danish].
- World Federation of Occupational Therapists (WFOT). Fundamental beliefs. [Internet]; 2017 [cited 2017 Oct 24]. Available from: http://www.wfot.org/AboutUs/FundamentalBeliefs.aspx
- Townsend EA, Polatajko HJ. Enabling occupation II: advancing an occupational therapy vision for health, well-being, & justice through occupation. 2nd ed. Ottawa (ON): CAOT Publications ACE; 2013.
- Fisher AG. Occupational therapy intervention process model. A model for planning and implementing top-down, client-centered, and occupation-based interventions. Fort Collins (CO): Three Star Press, Inc; 2009.
- Fisher AG. Occupation-centred, occupation-based, occupation-focused: same, same or different? Scand J Occup Ther. 2013;20:162–173.
- Polatajko HJ, Davis JA. Advancing occupation-based practice: interpreting the rhetoric. Can J Occup Ther. 2012;79:259–260.
- Canadian Association of Occupational Therapists. Enabling occupation: an occupational therapy perspective. Ottawa (ON): CAOT Publications ACE; 1997.
- Larsen AE, Carlsson G. Utility of the Canadian Occupational Performance Measure as an admission outcome measure in interdisciplinary community-based geriatric rehabilitation. Scand J Occup Ther. 2012;19:204–213.
- Sumsion T, editor. Client-centred practice in occupational therapy. A guide to implementation. 2nd ed. Edinburgh: Churchill Livingstone Elsevier; 2006.
- Law M, Baptiste S, Carswell A, McColl MA, Polatajko H, Pollock N. Canadian occupational performance measure, Danish version, revised 2007 by Larsen AE. Copenhagen: Danish Association of Occupational Therapists; 2007.
- Gupta J, Taff SD. The illusion of client-centred practice. Scand J Occup Ther. 2015;22:244–251.
- Wilkins S, Pollock N, Rochon S, et al. Implementing client-centred practice: why is it so difficult to do? Can J Occup Ther. 2001;68:70–79.
- Winkel A, Langberg H, Waehrens EE. Reablement in a community setting. Disabil Rehabil. 2014;37:1347–1352.
- World Federation of Occupational Therapists (WFOT). Code of ethics. [Internet]; 2016 [cited 2017 Dec 18]. Available from: http://www.wfot.org/ResourceCentre.aspx
- Nielsen TL, Petersen KS, Nielsen CV, et al. What are the short-term and long-term effects of occupation-focused and occupation-based occupational therapy in the home on older adults’ occupational performance? A systematic review. Scand J Occup Ther. 2017;24:235–248.
- Walker MF, Gladman JRF, Lincoln NB, et al. Occupational therapy for stroke patients not admitted to hospital: a randomised controlled trial. Lancet. 1999;354:278–280.
- Walker MF, Hawkins K, Gladman JRF, et al. Randomised controlled trial of occupational therapy at home: results at 1 year. J Neurol Neurosurg Psychiatry. 2001;70:267.
- Logan PA, Gladman JRF, Avery A, et al. Randomised controlled trial of an occupational therapy intervention to increase outdoor mobility after stroke. Brit Med J. 2004;329:1372–1375. [Erratum in: BMJ 2005;330:137].
- Gitlin LN, Winter L, Dennis MP, et al. A randomized trial of a multicomponent home intervention to reduce functional difficulties in older adults. J Am Geriatr Soc. 2006;54:809–816.
- de Vriendt P, Peersman W, Florus A, et al. Improving health related quality of life and independence in community dwelling frail older adults through a client-centred and activity-oriented program. A pragmatic randomized controlled trial. J Nutr Health Aging. 2016;20:35–40.
- Sturkenboom IHWM Graff MJL, Hendriks JCM, et al. Efficacy of occupational therapy for patients with Parkinson’s disease: a randomised controlled trial. Lancet Neurol. 2014;13:557–566. with online corrected version from 2016 Feb 24.
- Kirk-Sanchez NJ, Roach KE. Relationship between duration of therapy services in a comprehensive rehabilitation program and mobility at discharge in patients with orthopedic problems. Phys Ther. 2001;81:888–895.
- Jull G, Moore AP. What is a suitable dosage of physical therapy treatment? Man Ther. 2002;7: 181–182.
- Kimberley TJ, Samargia S, Moore LG, et al. Comparison of amounts and types of practice during rehabilitation for traumatic brain injury and stroke. JRRD. 2010;47:851–862.
- Randers Kommune. Nøgletal [key statistics]. [Internet]; 2016 [cited 2017 Dec 18]. Available from: https://omkommunen.randers.dk/media/28047/bilag-1-aldersgrupper.pdf [in Danish].
- Pollock N. Client centred assessment. Am J Occup Ther. 1993;47:298–301.
- McColl MA, Carswell A, Law M, Pollock N, Baptiste S, Polatajko H. Research on the Canadian occupational performance measure: an annotated resource. Ottawa (ON): CAOT Publications ACE; 2006.
- Eyssen ICJM, Steultjens MPM, Oud TAM, et al. Responsiveness of the Canadian occupational performance measure. J Rehabil Res Dev. 2011;48:517–528.
- Fisher AG, Jones KB. Assessment of motor and process skills: volume 1-development, standardization, and administration manual. 7th revised ed. Fort Collins (Co): Three Star Press, Inc.; 2012.
- Fisher AG, Jones KB. Assessment of motor and process skills: volume 2-user manual. 8th ed. Fort Collins (Co); Three Star Press, Inc; 2014.
- Fisher AG. The assessment of IADL motor skills: an application of many-faceted Rasch analysis. Am J Occup Ther. 1993;47:319–329.
- Doble SE, Fisk JD, Lewis N, et al. Test-retest reliability of the Assessment of Motor and Process Skills (AMPS) in elderly adults. Occup Ther J Res. 1999;19:203–215.
- Park S, Fisher AG, Velozo CA. Using the assessment of motor and process skills to compare occupational performance between clinic and home settings. Am J Occup Ther. 1994;48:697–709.
- OTAP. Occupational Therapy Assessment Package (Version 3.04) [Computer software]. Fort Collins (CO): Three Star Press; 2016 [Internet]. [cited 2017 Dec 18]. Available from http://www.innovativeotsolutions.com
- Center for Innovative OT Solutions. [Internet]; 2017 [cited 2017 Dec 18]. Available from: http://www.innovativeotsolutions.com
- Ware JE, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483.
- Bjørner JB, Damsgaard MT, Watt T, Bech P, Rasmussen NK, Kristensen TS, Modvig J, Thunedborg K. Dansk Manual Til SF-36. Et Spørgeskema Om Helbredsstatus [Danish Manual for the SF-36]. Copenhagen: LIF; 1997. [in Danish].
- Bjorner JB, Thunedborg K, Kristensen TS, et al. The Danish SF-36 health survey: translation and preliminary validity studies. J Clin Epidemiol. 1998;51:991–999.
- Ware JE. SF-36® Health Survey © 1988; 2002. MOT, Health Assessment Lab, QualityMetric Incorporated (IQOLA SF-36 Danish Version 1.1).
- Lyons RA, Perry HM, Littlepage BNC. Evidence for the validity of the Short-form 36 questionnaire (SF-36) in an Elderly Population. Age Ageing. 1994;23:182–184.
- QualityMetric Health Outcomes™ Scoring Software 4.0 [Computer software]. QualityMetric Incorporated 24 Albion Road, Bldg 400. Lincoln, R.I. 02865, USA 2017 [Internet] [cited 2017 Dec 18]. Available from: https://campaign.optum.com/content/optum/en/optum-outcomes/what-we-do/health-surveys.html
- Samsa G, Edelman D, Rothman ML, et al. Determining clinically important differences in health status measures: a general approach with illustration to the Health Utilities Index Mark II. Pharmacoeconomics. 1999;15:141–155.
- Maitra K, Erway F. Perception of client-centered practice in occupational therapists and their clients. Am J Occup Ther. 2006;60:298–310.
- Dekkers M, Søballe K. Activities and impairments in the early stage of rehabilitation after Colles' fracture. Disabil Rehabil. 2004;26:662–668.
- Gardette V, Coley N, Toulza I, et al. Attrition in geriatric research: how important is it and how should it be dealt with? J Nutr Health Aging. 2007;11:265–271.
- Lauritsen JM, Bruus M. EpiData version 3.1. A comprehensive tool for validated entry and documentation of data. Odense (Denmark): The EpiData Association, 2003–2005.
- StataCorp. Stata statistical software: release 12. College Station (TX): StataCorp LP; 2011.
- World Medical Association. World Medical Association Declaration of Helsinki. Ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194.
- Moher D, Schulz KF, Altman DG. The CONSORT statement: revised recommendations for improving the quality of reports of parallel group randomized trials. BMC Med Res Methodol. 2001;1:2.
- Current Controlled Trials. [Internet]; 2017 [cited 2017 Dec 18]. Available from: https://s3-us-west-2.amazonaws.com/webcitation/6fc2d850dde348335d1ab0b668 28190d475a6967
- Langeland E, Førland O, Aas E, Birkeland A, Folkestad B, Kjeken I, Jacobsen FF, Tuntland H. Modeller for Hverdagsrehabilitering – En Følgeevaluering i Norske Kommuner [Models for Everyday Rehabilitation – an Evaluation in Norwegian Municipalities]. Bergen: Senter for Omsorgsforsknings Rapportserie nr 6; 2016. [in Norwegian].
- Tuntland H, Aaslund MK, Espehaug B, et al. Reablement in community-dwelling older adults: a randomised controlled trial. BMC Geriatr. 2015;15:145.
- Hortobágyi T, Mizele C, Beam S, et al. Old adults perform activities of daily living near their maximal capabilities. J Gerontol A Biol Sci Med Sci. 2003;58A:453–460.
- Kjellberg J, Ibsen R. Rehabiliterende Hjemmepleje Efter Roskilde-Modellen [Rehabilitating home-care following the Roskilde Model]. Copenhagen: Det Nationale Institut for Kommuners og Regioners Analyse og Forskning; 2016. [in Danish].
- Ross S, Grant A, Counsell C, et al. Barriers to participation in randomised controlled trials: a systematic review. J Clin Epidemiol. 1999;52: 1143–1156.
- Richards DA, Hallberg IR, editor. Complex interventions in health. Oxon (OX): Routledge; 2015.
- Polgar S, Thomas SA. Introduction to research in the health sciences. 6th ed. London: Elsevier Health Sciences; 2013.
- Boutron I, Guittet L, Estella C, et al. Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS Med. 2007;2:e61–0370-80.
- Njelesani J, Teachman G, Durocher E, et al. Thinking critically about client-centred practice and occupational possibilities across the life-span. Scand J Occup Ther. 2015;22:252–259.
- Hammell KRW. Client-centred practice in occupational therapy: critical reflections. Scand J Occup Ther. 2013;20:174–181.
- Hays RD, Woolley JM. The concept of clinically meaningful difference in health-related quality-of-life research. How meaningful is it? Pharmacoeconomics. 2000;18:419–423.
Appendix 1. Occupational performance and health related quality of life.
Mean scores and between group differences at 3 and 6 months