Abstract
Background
The support needs of people with neurodevelopmental disorders are not sufficiently met during the initial years of adulthood.
Aim
To evaluate feasibility and preliminary effects of a novel programme designed to empower young adults with autism spectrum disorder (ASD) and/or attention deficit hyperactivity disorder (ADHD) to make progress within significant life domains (i.e. work, education, finance, housing/household management, health, leisure/participation in society, and relationships/social network).
Material and Method
TRANSITION is a 24-week programme that combines group-based workshops with personalised support based on goal attainment scaling. The study enrolled 26 young adults (50% females; age 17–24 years) in the normative intellectual range, diagnosed with ASD (n = 8), ADHD (n = 4), or both (n = 14). The intervention was delivered by the regular staff of publicly funded psychiatric services in Stockholm, Sweden.
Results
The programme was possible to implement with minor deviations from the manual. Participants and staff generally viewed the intervention positively, but also provided feedback to guide further improvement. There was a high degree of attendance throughout, with 21 participants (81%) completing the programme. All completers exceeded their predefined goal expectations within at least one domain.
Conclusions
The TRANSITION-programme is a promising concept that deserves further evaluation.
Introduction
The transition from adolescence to adulthood is a crucial time of change in most people’s lives, bringing dramatic transformation of virtually every major life domain. The phase of life coined emerging adulthood (approximately ages 18–25) is characterised by opportunities to explore roles and relationships [Citation1], but also increased demands on independence and associated risks such as unemployment, truncated education, dependence on parents, loneliness, onset of mental health conditions, and sedentary lifestyles [Citation2–4].
Adjustment to the environmental demands of adulthood can be particularly hard for people with neurodevelopmental disorders (NDDs), as evidenced by adverse long-term outcomes related to education, employment, relationships, and health [Citation5–11]. Autism spectrum disorder (ASD) and attention deficit hyperactivity disorder (ADHD) are associated with a range of altered cognitive functions that are crucial during these transformative years, including social cognition, self-regulation, central coherence, attention, self-control, planning, and mental flexibility [Citation12–14]. People with these conditions often tend to experience major impairments in adaptive functioning [Citation15,Citation16], and can have difficulties achieving age appropriate functioning [Citation7,Citation17]. As a consequence of poorly coordinated services, young adults with NDDs often are denied the treatment and support they need [Citation18–20]. This group of young people also tend to participate less than their peers in activities (e.g. physical activities, job, and chores) that contribute to adult competencies [Citation21,Citation22]. This mix of functional impairments, insufficient support, and lack of structured activities leaves the individual at risk of inactivity and social isolation.
In order to better understand the needs and aspirations of young adults with NDDs, it is essential to turn to the body of qualitative research focussing on the perspectives of the youths themselves and their caregivers. This body of research highlights the significance of the physical and social environment, the need for a gradual transition to a diverse support, and the importance of comprehensive and integrated services [Citation23]. Some additional themes have been identified in recent studies: to be understood, to understand the world, and to succeed [Citation24]; uncertainty about the future, and a lack of guidance [Citation25]; balancing security and autonomy, holistic support needs, and work as a source of engagement and empowerment [Citation26]. Further, a study on different viewpoints on how students with autism can best navigate university emphasised the importance of individualised and contextual support [Citation27]. Overall, the literature underscores the importance of adequate support, knowledge, and skills to gradually increase one’s independence. A lion’s share of the responsibility for this currently rests with the caregivers, leading to an excessive caregiver burden [Citation28–30]. This can also lead to unequal opportunities, if there are differences in how effectively caregivers can advocate for their children [Citation20,Citation31]. Thus, the extent to which better support for young adults can alleviate the caregiver burden needs to be better understood [Citation32].
To address the diversity of unmet needs, we envision a future with a wide range of evidence-based options. The overall literature on transition in youth with disabilities offers some general guidance. Central themes include a less divided care structure; collaboration among stakeholders; peer involvement; the value of opportunities and experiences; and the importance of information, education, and research [Citation33]. Life skills interventions have shown positive results in secondary-aged youths with disabilities [Citation34], while post-secondary transition programmes seem to have the potential to improve outcome in the educational domain [Citation35]. Favourable outcome of mentorship programmes in the transition to post-secondary education and employment have been linked to structured programmes, group-based or mixed formats, and a relatively long duration [Citation36].
The diversity of transition-related interventions specifically developed for people with NDDs is currently starting to increase. Some comprehensive transition programmes preparing school-aged adolescents for adulthood have recently been developed [Citation37,Citation38], and there are a few programmes with a specific focus on vocational needs [Citation39]. Preliminary support is also appearing for some programmes tailored specifically for the early years of adulthood. A novel skills training programme addressing challenges faced by young adults with ASD has shown preliminary positive effects [Citation40], as has a group-delivered transition service for adults with ASD [Citation41]. Similarly, a programme teaching parents to advocate for adult disability services seems to have the potential to empower parents [Citation42]. Some internet-delivered support programmes for adolescent and young adults with ASD and/or ADHD have also been developed [Citation43,Citation44]. On a more general note, there is also some evidence suggesting that cognitive behavioural therapy (CBT) and related methods can have positive effects for adults with ASD or ADHD [Citation45–48].
Here, we report on the development and feasibility of the TRANSITION-programme, which represents a novel approach to supporting young adults with ASD and/or ADHD. The overarching aim is to promote a low-risk transition period and increase the likelihood of positive long-term social, economic, and health-related outcomes. The intervention attempts to achieve this through two distinct pathways. The first is to increase the participant’s knowledge within key life domains, and thereby their ability to navigate more effectively in society. The second is to utilise goal setting and other basic behavioural change techniques to initiate concrete change within these domains. The present study aimed to investigate the feasibility of the TRANSITION concept, with focus on the following two aspects:
Implementation and acceptability. Can TRANSITION be used as planned in real-world clinical practice? Is the intervention acceptable to participants and staff? How can the intervention be improved? Is the intervention safe?
A preliminary evaluation of efficacy. Does the intervention seem to have intended effects?
Method
Study design
This was an open feasibility study without control group. The study was performed by the Centre of Neurodevelopmental Disorders at Karolinska Institutet (KIND)/Stockholm County Council (SLL), Sweden, in collaboration with two units within the publicly funded psychiatric services in Stockholm (the Child and Adolescent Psychiatric unit at KIND, and the ADHD unit of the Northern Stockholm Psychiatric Services). The data collection was carried out at these two units from October 2015 to August 2017. The study was approved by the Regional Ethics Committee of Stockholm (2015/1432-31).
The intervention
TRANSITION combines a set of group-based workshops pertaining to seven preselected life domains (work, education, finance, household management/housing, health, leisure/participation in society, and relationships/social network) with a mentorship programme in which each participant has regular contact with a mentor and works towards individualised goals. The intervention lasts for a total of 24 weeks. TRANSITION is not intended as an alternative to other interventions, but should rather be viewed as a complementary service.
Development
The development of TRANSITION started in 2015 and involved several key decisions outlined below.
Scope
Given that major life domains are closely intertwined, a holistic approach was chosen [Citation26]. A wide number of life domains from the vast literature on quality of life (QoL), functioning, and support needs were considered. The number of domains were ultimately narrowed down to seven: Work, education, and independent living are arguably the most salient transition points in this phase of life; finance and health were included due to the risk of adverse long-term outcome in these domains; social networks and leisure/participation in society were selected to promote inclusion and QoL. Choices regarding specific content and structure were guided by extensive literature studies, focus groups, dialogues with interest organisations, and communication with relevant organisations and institutions on a municipality, county and national level. One focus group with four parents and three focus groups with a total of seven young adults with ASD and/or ADHD (aged 16–25; lived with parents, alone, or with partner; students, self-employed, employed, or unemployed), were conducted from May to June 2015. Participants were recruited through schools, clinics, and interest organisations. Each focus group meeting lasted approximately 60–90 min.
Target population
Key transition periods in life are important opportunities for behavioural change [Citation49,Citation50]. Preparations before the individual enters adulthood are important, but the individual will most likely also need support once the new skills are to be applied in real life situations (i.e. in young adulthood) [Citation51]. Here we focussed on young adulthood, since few support programmes are available for this crucial life period. We specifically addressed the initial phase of the transition to adulthood (ages 17–24), but acknowledge that transition services could be beneficial also for people in their late 20 s. To ensure that the specific content would be relevant for all participants, the eligible population was further limited to people with ASD and/or ADHD in the normative intellectual range. These two conditions are relatively common and frequently co-occur [Citation52]. While the support needs have been found to differ somewhat between young adults with ASD and ADHD [Citation53], both conditions are linked to major functional impairment [Citation15,Citation16] and adverse long-term outcomes [Citation5–11]. The general concept evaluated here might ultimately prove useful in a more inclusive population (e.g. young adults with intellectual disability, other NDDs, or impairing mental health conditions), albeit after appropriate adaptation of the content.
Mechanism of change
TRANSITION was designed to empower young adults with knowledge, but also to initiate concrete change by means of well-established behavioural change techniques [Citation49]. Goal setting in the form of goal attainment scaling (GAS) was given a central role in TRANSITION. This is a method for producing individualised, criterion-referenced measures of clinically relevant change, which emphasises participant engagement in defining personally meaningful goals [Citation54,Citation55]. From a theoretical perspective, TRANSITION was also informed by behavioural activation [Citation56], psychoeducation, case management [Citation57], and acceptance and commitment therapy (ACT) [Citation58].
Mode of delivery
TRANSITION was explicitly developed as a natural extension to other group-based interventions, such as social skills training and psychoeducation. Given the focus on gradual independence, we did not include caregivers directly. Contact with peers in a similar situation, on the other hand, might have the potential to facilitate observational learning and promote extended social networks. The theoretical part of the intervention, which focussed mainly on acquisition of knowledge, was therefore held as group-based workshops. The structure of this part was inspired by previously developed group interventions such as KONTAKT [Citation59] and PEGASUS [Citation60]. A similar format was recently also shown to be feasible and appreciated in a similar occupation-focussed lifestyle intervention for mental health service users in Sweden [Citation61]. A guest lecturer with a diagnosis of ASD and/or ADHD, who had recently navigated the transition-related challenges, was invited to share experiences. A second, more practically oriented part of the intervention consisted of individual contact with a mentor, which was deemed to be the best option to enable a clear focus on the participant’s own values and goals. To keep the workload on a sustainable level and decrease the risk of drop-out, it was specified that the majority of the contact with the mentor was to be held via telephone, mail, or text messages.
Sustainability
Due to the multidisciplinary nature of support provision, TRANSITION was designed to be applicable in a range of service settings, including mental health services and social services. The idea was to design a programme based on a few basic components with a straight-forward structure that could be delivered by regular staff with diverse training. The manual and work material should be user-friendly, accessible, and easy to adapt/revise. We viewed the length of the intervention as a trade-off between the optimal effect, available resources, and demands on the participant’s time and effort [Citation62]. To be effective, we reasoned that the duration should enable the participants to pursue and attain meaningful goals in the course of the intervention.
Structure and content
During the initial session, the participants meet individually with the mentor to map their current situation and to formulate individualised homework assignments and goals using GAS (see detailed procedure below under Data sources). During the subsequent five weeks, participants take part in weekly workshops including up to 10 participants and two mentors/group leaders. The five sessions cover the seven predefined life domains. After completion of the group intervention, the participants meet individually with the mentor to make a preliminary assessment of goal attainment and update the GAS scales. Thereafter, the participants and their mentor continue to have contact via telephone, SMS, or e-mail, during approximately four months. The mentor is instructed to limit this contact to approximately 30 min/week, but as long as the work progresses as planned there is no minimum level. Face-to-face meetings are allowed if deemed necessary. The mentorship phase ends with a concluding follow-up meeting, which includes a final assessment of goal attainment. Homework is given weekly throughout the intervention. Participants receive a folder that includes materials used each session (e.g. notes and homework assignments). A preliminary manual clarifies implementation practices. For more information regarding structure and contents, see and .
Figure 1. Structure of the TRANSITION programme and measures used in the feasibility study. QOLI: Quality of Life Inventory; GAS: Goal Attainment Scaling.
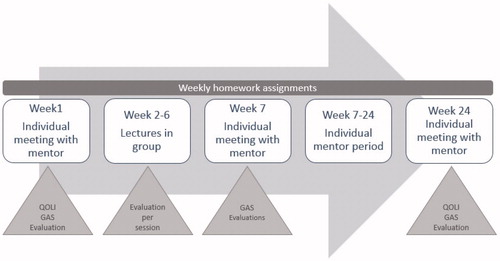
Table 1. Outline of the TRANSITION-programme.
Participants: eligibility and recruitment
Eligible participants were aged 17–24 years in the normative intellectual range with an International Classification of Diseases – 10th Revision [Citation63] diagnosis of ASD (F84.0, F84.1, F84.5, or F84.9) and/or ADHD (F90.0) according to clinical records and recommended regional assessment guidelines [Citation64]. Exclusion criteria were insufficient Swedish proficiency, intellectual disability (IQ < 70), and severe mental disorders that might jeopardise full participation or safety of the participants (e.g. severe depression, suicidality).
The ambition was to recruit participants reflecting the heterogeneity of young adults with ASD and/or ADHD in the normative intellectual range regarding gender, functional impairment, comorbidity, and social adjustment. To increase diversity, participants for three separate TRANSITION-groups were recruited using different strategies for each group. For the first group, we explicitly reached out to young adults who previously participated in similar group-based interventions (e.g. KONTAKT or PEGASUS). The participants in the second group were recruited among patients at the ADHD unit of the Northern Stockholm Psychiatric Services, while the third group were recruited from the client registry of an insurance company (Trygg-Hansa). Potential participants received verbal and written information about the study, and had opportunity to ask follow-up questions. All participants signed a written consent form and were informed that they could terminate their participation at any time. All approached participants consented.
Setting and staff training
The intervention was delivered at two outpatient units within the publicly funded psychiatric service in Stockholm (the Child and Adolescent Psychiatric unit at KIND, and the ADHD unit of the Northern Stockholm Psychiatric Services). Mentors/group leaders were recruited from the regular staff of each unit. A total of six mentors/group leaders (four psychologists, one social worker, and one occupational therapist) were involved. Eligible mentors/group leaders were trained professionals with a basic training in CBT and a general interest in the social/societal issues addressed by the programme, who had prior experience in providing service for people with NDDs. To ensure good treatment fidelity, the mentors/group leaders participated in a one-day introduction before the start of the intervention. Group supervision (2–3 h) by personnel from KIND (three psychologists involved in the development of the intervention) was scheduled approximately once every month in the course of the intervention (somewhat more frequent at the start, and less frequent towards the end). If necessary, additional supervision was provided by phone.
Data sources
Demographic and clinical data
At the pre-inclusion meeting, the mentors collected information regarding the participant’s date of birth, gender, diagnoses, date and department of neuropsychiatric assessment, current medication, and substance use disorders. Information on IQ and psychiatric comorbidity was acquired via medical records. If information on IQ was not available, or if the reported IQ score ranged between 70 and 85, a qualitative assessment of the participant’s suitability for the intervention was made. In addition to the diagnoses retrieved from medical records, suicidal ideation and depression were assessed with the MINI International Neuropsychiatric Interview (module A ‘Major depressive disorder’; module B ‘Suicidality’) if deemed necessary [Citation65]. If there was an ongoing depressive episode, severity was assessed with the Montgomery–Åsberg Depression Rating Scale (MADRS) self-evaluation questionnaire [Citation66].
Implementation and acceptability
Attendance for each session and number of participants completing the intervention was recorded. In addition, each contact between the participant and the mentor was documented, as a measurement of proximal workload. An evaluation questionnaire was completed by the participants after each group session and individual meeting with the mentor. The questionnaire comprised both open-ended questions and Likert-scaled items. The evaluations focussed on the content of the specific session and shared experiences with others. Overall assessments of the group-based part and mentor period were evaluated after completion (week 7 and 24, respectively). Information about the intervention’s acceptability and implementability was actively requested from the mentors and participants throughout the study. Mentors/group leaders were explicitly asked in supervision about deviations from the manual, and material used in the individual and group sessions (PowerPoint presentations, set goals and scales) was systematically collected.
Efficacy
Goal attainment in the course of intervention was the primary measure of intended effects. Relevant goals and scales were set in close collaboration between the participant and the mentor during the individual meetings. At the first meeting (week 1), 2–4 relevant life domains were chosen. Previous experience and current situation within the chosen domains were formulated, strengths and difficulties relating to the domains were discussed, and a valued direction within the domain was formulated [Citation58]. Thereafter, preliminary goals, concrete activities and relevant scales were defined. Each scale ranged from the most unfavourable outcome (–2) to the most favourable outcome (+2), with the expected outcome in between (0) and intermediary steps of less and more than expected (–1 and +1, respectively). The GAS should be specific (i.e. precisely defined, preferably in behavioural terms), measurable (i.e. preferably possible to assess objectively), attainable (i.e. not dependent on external factors or resources outside of the participant’s control), realistic (i.e. adapted to the individual’s situation and motivation), and timely (i.e. matching the predefined time frame of the intervention). Participants should be allowed to try out more than one goal, in order to subsequently have the option to focus on the most meaningful ones and abandon others along the way. Drawing from the transtheoretical model of change, we acknowledge that the participant’s readiness for change in a specific domain might vary considerably [Citation67]. Consequently, the goals pursued in TRANSITION might range from exploring possible change, to actually initiating change, or maintaining change that has already been established. At the second individual meeting (week 7), a preliminary assessment of the GAS scores was conducted by the mentor in collaboration with the participant based on information from reviewed homework assignments. This was also an opportunity to revise the goals or set new ones based on the insights gained during the group sessions. At the concluding individual meeting (week 24), the final outcome was assessed by the mentor in collaboration with the participant based on regular contact with mentor and reviewed homework assignments. The procedure for GAS formulation was detailed in the manual and was included in the training course for mentors. Further, the process was regularly discussed in supervision.
The secondary outcome measure was the self-rated Quality of Life Inventory (QOLI)) [Citation68] measured pre- and postintervention. The scale includes 16 life domains. Each domain is scored on two dimensions: importance and satisfaction. For each area of life, a raw score is computed by multiplying the two dimensions. A total score is calculated by summarising the scores of every domain rated as important or extremely important, and dividing the score by the number of included areas. This score can be transformed to a normative T-score. A test-retest coefficient of rtt = 0.73 for an interval of two weeks and an internal consistency reliability (coefficient alpha) for the sum of the weighted satisfaction ratings of rtt = 0.79 have been reported [Citation68].
Safety
All spontaneously reported adverse event in the course of the intervention were recorded. An adverse event was defined as any reported occurrence considered to be unfavourable for the participant. Subsequently, the likelihood that an adverse event was related to the intervention was assessed.
Data analysis
Distributions of baseline characteristics were compared between the three recruited groups using Kruskal-Wallis test by ranks for continuous/discrete data and Fisher’s exact test for dichotomous data. The number of set goals and the attained GAS scores within each domain was summarised descriptively. In addition, the levels reached by the completers in their most and second most favourable domain were summarised across participants. The change in total QOLI scores (T-scores) from pre- to postintervention was analysed in completers. To better understand the heterogeneity of QOLI scores, explorative subgroup analyses were performed post hoc regarding sex (males/females), diagnosis (ADHD, ASD, or both), comorbid mental health condition (yes/no), psychostimulants (yes/no), antidepressants (yes/no), and baseline QoL scores categorised as low/very low (≤42 T-scores) or average (≥43 T-scores) in accordance with the QOLI manual [Citation68]. Due to the small sample size, Wilcoxon signed-rank test was used for all these analyses. The association of change scores on QOLI with IQ and age were analysed using linear regression. The three recruited intervention-groups were collapsed in all analyses of outcome data. IBM SPSS statistics version 24 was used for all analyses.
Feedback on the intervention received verbally or in the written evaluations were grouped thematically by one of the authors, with the aim to identify potential areas for improvement. A second author checked the integrity of the categories, to ensure that no important suggestion was discarded. The participants’ overall evaluations of the group-based part and the mentorship were summarised.
Results
Demographic data
Three open TRANSITION-group (two groups with 10 participants, and one with 6 participants) were included. The 26 participants (50% females) were 17–24 years of age and diagnosed with ASD (n = 8), ADHD (n = 4), or both (n = 14). The Two participants had an additional diagnosis of specific learning disorder. Comorbid mental health conditions and psychotropic medication were relatively common in all groups. The participants’ full-scale IQ had a distribution similar to that of the general population. The age distribution differed significantly between the groups, with one group including only participants below age 20 ().
Table 2. Baseline characteristics of the participants in each of the three TRANSITION groups and the total sample.
Implementation and acceptability
The intervention was possible to implement as specified, with some minor deviations from the manual. First, the mentors expressed that they were pressed for time during the first individual meeting. Second, the material prepared for the group sessions was in some cases found excessive and some aspects had to be omitted. Third, a concluding group session was added after the mentor period in one of the groups. This was done at the request of the participants to provide an opportunity to share experiences. Supplementary Appendix (Table S1) provides an overview of adjustments made at different stages of the programme in each group.
A total of 21 participants (81%) completed the 24-week programme, while 5 dropped out (2 at an early stage and 3 after completion of the group sessions). Four of the participants who dropped out cited lack of motivation or time, while one had relocated. Attendance was relatively high throughout the programme. All enrolled participants except one showed up for the first individual meeting. The group sessions were attended by 21 participants (81%) on average, and all participants except two came to the second individual meeting with the mentor. During the subsequent mentor period, the participants who completed the programme had contact with the mentor to a varying degree (median = 30 times; range = 10–87). The contact mainly consisted of text-messages and phone calls. The communication focussed on continued work towards set goals, but also included bookings and cancellations of meetings. The total number of calls ranged from 0 (a few participants preferred text messages or email) to 23, with a median of 8 calls. The total duration of the calls ranged from 0 to 8 h, with a median of 3 h. The final individual meeting with the mentor was attended by 21 participants.
The evaluation of the group-based part was completed by 24 participants: 18 (75%) rated this part as good or excellent, 4 as acceptable, and 2 as unsatisfactory. The latter two reported that the content was to general and not fully relevant to their current situation. The content of the subsequent mentor period was found fully or partially relevant by 20 of the 21 (95%) completers. Feedback on specific aspects of the programme was provided by both mentors/group leaders and participants, and included thoughts on group constellation and preparation, challenges related to GAS, and the importance of adjusting the content of the group sessions to each specific group. The participants also requested more time for discussion in the groups. Suggestions for improvement are listed in the Supplementary Appendix (Table S2).
Efficacy
The goals selected by the participants were distributed across all domains, with a particularly high number of participants opting for the domains of health and finance (). Typical goals included applying for a job, paying bills independently, going to the gym regularly, organising housework, improving study techniques, and seeing friends/family more frequently (Table S3). A total of 90 goals were set and the final outcomes were distributed relatively even across the scale levels. All the participants who completed the programme reached a level of greater than expected or the most favourable outcome in at least one of their goals (). A substantial proportion (45%) of the selected goals did not result in the expected outcome, which was in line with our expectations that some goals would be abandoned along the way. Goals attained during the programme included sending job applications, finding a structure for studying, starting to prepare meals by on one’s own, keeping a sustainable budget each month, going to the gym regularly, and starting to go out with friends (Table S3).
Figure 2. The goal attainment scale level attained by the completers in their most and second most favourable domain.
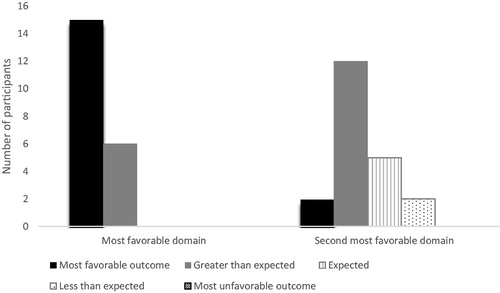
Table 3. Participants’ identified goals within each life domain, and the score level attained.
All the 21 participants who completed the intervention provided pre- and post-measurement for the QOLI. Preintervention, 11 of 21 participants (52%) had low to very low overall QoL (T-score of ≤42) while the rest of the participants were within the average span (T-score between 43 and 58). Postintervention, eight participants (38%) had a low to very low classification and the remainder had average. In the total sample, the change in T-score from preintervention (median: 41; range: 16–58) to postintervention (median: 45; range: 22–54) was not statistically significant (Z = 1.17, p = 0.23). Explorative analyses revealed that there was a significant positive change from preintervention (median: 32; range: 16–41) to postintervention (median: 38; range: 22–54) in those with low to very low overall well-being at baseline (Z = 2.67, p = 0.008), and a non-significant decline from preintervention (median: 50; range: 44–58) to postintervention (median: 47; range: 35–53) in the participants starting out in the average QoL span (Z = –1.60, p = 0.11). No other significant association was found between baseline characteristics and change in QoL.
Safety
A total of five adverse events were reported during the intervention. One of these was related to the intervention (i.e. a participant with a general medical condition feeling worse in related to a set goal), while the remaining four events were considered unrelated (i.e. stress induced by moving to a new apartment, separation from a partner, and hospitalisation due to a side effect of ongoing medication).
Discussion
This study evaluated feasibility, acceptability, and preliminary efficacy and safety of the TRANSITION-programme in young adults with ASD and/or ADHD. The programme was shown to be feasible in clinical practice, with a high degree of attendance throughout. All participants who completed the whole programme exceeded their expectations in at least one life domain. Participants and mentors/group leaders mainly viewed the intervention favourably, but also provided valuable feedback that will guide further improvement.
At this early stage, the key question is whether or not to continue the evaluation of this programme. A clear indication of positive effect in at least one major outcome domain seems like a reasonable precondition. The changes reflected by the GAS is a reassuring in this respect. The results regarding QoL, on the other hand, are less clear-cut. A substantial proportion of the participants reported QoL in the low range, echoing the previous body of research on QoL in young people with NDDs [Citation69]. Participants who started out with low or very low QoL improved significantly, while those with a baseline level in the average range displayed a non-significant decline. This preliminary finding should be interpreted with caution, but it is likely that TRANSITION temporarily disrupts daily life by moving participants out of their comfort zone. This change might hypothetically break a vicious circle of inactivity and loneliness in some, while the stress induced by the change might outweigh the gains in the short-term perspective for others. In the continued evaluation, it will be important to clarify how QoL develops over time depending on baseline levels.
Limitations and future directions
In future evaluations, it will be vital to address some major shortcomings of this initial study. First, this preliminary evaluation of efficacy was limited in scope. The intended effects of TRANSITION reach beyond goal attainment and QoL, embracing aspects such as service utilisation, caregiver burden, meaningful participation, functioning, and health outcomes. In particular, it will be important to use International Classification of Functioning, Disability and Health core sets in further evaluations [Citation15,Citation16]. Further, intermediary measures could potentially shed light on the mechanisms of change. Increased knowledge, in combination with new experiences of attaining meaningful goals, would presumably increase the participants’ beliefs in their ability to succeed when confronted with challenges (i.e. self-efficacy). Self-efficacy is central to several leading theories of behavioural change, and was recently shown to be associated with return to work among unemployed young adults with disabilities [Citation70]. The related construct of self-determination should also be explored further, given the clear parallels between TRANSITION and the self-determined learning model of instruction [Citation71]. Second, threats to internal validity must be addressed in future evaluations. While we feel reasonably confident that much of the observed change was attributable to the intervention, we cannot rule out that the outcome in part was a function of time (e.g. regression to the mean or development). Further, the study lacked an independent outcome rater, session recordings, and fidelity assessments. Third, the sample was relatively small and data was missing for a proportion of the participants on some variables (e.g. IQ). While it is important to stress the preliminary nature of the explorative analyses in particular, we still believe that these analyses will help guide future evaluations. Fourth, generalizability across societies (e.g. service systems that diverge from the Swedish model) and diversity (e.g. socioeconomic status, cultural background, cognitive abilities, and previous exposure to similar interventions) should be investigated further.
These limitations notwithstanding, we conclude that further evaluation is justified. This would ideally commence in a step-wise manner [Citation72]. First, we need more information about how this intervention will fit into the organisation of current service provision. This would include a detailed mapping of current practice, but also more precise estimates of the demand. Second, the manual must be modified based on feedback. In addition, barriers to participation should be identified (e.g. transportation, lack of parental support). Third, the usefulness of the concept in different service settings (e.g. social services) should be explored further. Given the extensive societal costs related to NDDs [Citation73,Citation74], it is also important to conduct cost-effectiveness analyses. Finally, it is important to emphasise that there are limits to what we should expect from TRANSITION and similar interventions. To enable young people with NDDs to live fulfilling lives, it is crucial that major institutions in society adapt to diversity and facilitate a more sustainable person-environment fit.
Online_Appendix_SJOT.docx
Download MS Word (25.1 KB)Acknowledgement
We would like to thank all participants, our colleagues at the ADHD unit of the Northern Stockholm Psychiatric Services, and everybody providing help and support during the development of TRANSITION.
Disclosure statement
Sven Bölte discloses that he has in the last 5 years acted as an author, consultant or lecturer for Shire, Medice, Roche, Eli Lilly, Prima Psychiatry, GLGroup, System Analytic, Kompetento, Expo Medica, and Prophase. He receives royalties for text books and diagnostic tools from Huber/Hogrefe, Kohlhammer and UTB. Tatja Hirvikoski discloses that she receives royalties for manuals and text books from Hogrefe. The other authors declare that they have no conflict of interest.
Additional information
Funding
References
- Arnett JJ. Emerging adulthood. A theory of development from the late teens through the twenties. Am Psychol. 2000;55:469–480.
- Carcillo S, Fernández R, KöNigs S, et al. NEET youth in the aftermath of the crisis: challenges and policies. OECD Social, Employment and Migration Working Papers, No. 164. Paris: OECD Publishing; 2015.
- Nelson MC, Story M, Larson NI, et al. Emerging adulthood and college-aged youth: an overlooked age for weight-related behavior change. Obesity. 2008;16:2205–2211.
- Schulenberg JE, Sameroff AJ, Cicchetti D. The transition to adulthood as a critical juncture in the course of psychopathology and mental health. Dev Psychopathol. 2004;16:799–806.
- Croen LA, Zerbo O, Qian Y, et al. The health status of adults on the autism spectrum. Autism. 2015;19:814–823.
- Hirvikoski T, Mittendorfer-Rutz E, Boman M, et al. Premature mortality in autism spectrum disorder. Br J Psychiatry. 2016;208:232–238.
- Howlin P, Goode S, Hutton J, et al. Adult outcome for children with autism. J Child Psychol and Psychiat. 2004;45:212–229.
- Jonsson U, Alexanderson K, Kjeldgard L, et al. Diagnosis-specific disability pension predicts suicidal behaviour and mortality in young adults: a nationwide prospective cohort study. BMJ Open. 2013;3:e002286.
- Kuriyan AB, Pelham WE, Jr., Molina BS, et al. Young adult educational and vocational outcomes of children diagnosed with ADHD. J Abnorm Child Psychol. 2013;41:27–41.
- Michielsen M, Comijs HC, Aartsen MJ, et al. The relationships between ADHD and social functioning and participation in older adults in a population-based study. J Atten Disord. 2015;19:368–379.
- Taylor JL, Seltzer MM. Employment and post-secondary educational activities for young adults with autism spectrum disorders during the transition to adulthood. J Autism Dev Disord. 2011;41:566–574.
- Hartman CA, Geurts HM, Franke B, et al. Changing ASD-ADHD symptom co-occurrence across the lifespan with adolescence as crucial time window: illustrating the need to go beyond childhood. Neurosci Biobehav Rev. 2016;71:529–541.
- Magiati I, Tay XW, Howlin P. Cognitive, language, social and behavioural outcomes in adults with autism spectrum disorders: a systematic review of longitudinal follow-up studies in adulthood. Clin Psychol Rev. 2014;34:73–86.
- Sonuga-Barke E, Bitsakou P, Thompson M. Beyond the dual pathway model: evidence for the dissociation of timing, inhibitory, and delay-related impairments in attention-deficit/hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2010;49:345–355.
- Bölte S, Mahdi S, Coghill D, et al. Standardised assessment of functioning in ADHD: consensus on the ICF Core Sets for ADHD. Eur Child Adolesc Psychiatry. 2018;27:1261–1281.
- Bölte S, Mahdi S, de Vries PJ, et al. The Gestalt of functioning in autism spectrum disorder: results of the international conference to develop final consensus International Classification of Functioning, Disability and Health core sets. Autism. 2019;23:449–467.
- Willoughby MT. Developmental course of ADHD symptomatology during the transition from childhood to adolescence: a review with recommendations. J Child Psychol and Psychiat. 2003;44:88–106.
- Eklund H, Cadman T, Findon J, et al. Clinical service use as people with Attention Deficit Hyperactivity Disorder transition into adolescence and adulthood: a prospective longitudinal study. BMC Health Serv Res. 2016;16:248.
- Swift KD, Sayal K, Hollis C. ADHD and transitions to adult mental health services: a scoping review. Child Care Health Dev. 2014;40:775–786.
- Taylor JL, Henninger NA. Frequency and correlates of service access among youth with autism transitioning to adulthood. J Autism Dev Disord. 2015;45:179–191.
- Ratcliff K, Hong I, Hilton C. Leisure participation patterns for school age youth with autism spectrum disorders: findings from the 2016 National Survey of Children’s Health. J Autism Dev Disord. 2018;48:3783.
- Shimoni M, Engel-Yeger B, Tirosh E. Participation in leisure activities among boys with attention deficit hyperactivity disorder. Res Dev Disabil. 2010;31:1234–1239.
- Anderson KA, Sosnowy C, Kuo AA, et al. Transition of individuals with autism to adulthood: a review of qualitative studies. Pediatrics. 2018;141:S318–s327.
- Thompson C, Bölte S, Falkmer T, et al. To be understood: transitioning to adult life for people with Autism Spectrum Disorder. PLoS One. 2018;13:e0194758.
- Chen J, Cohn ES, Orsmond GI. Parents’ future visions for their autistic transition-age youth: hopes and expectations. Autism. 2019;23:1363–1372.
- Sosnowy C, Silverman C, Shattuck P. Parents’ and young adults’ perspectives on transition outcomes for young adults with autism. Autism. 2018;22:29–39.
- Thompson C, Bölte S, Falkmer T, et al. Viewpoints on how students with autism can best navigate university. Scand J Occup Ther. 2019;26:294–305.
- Cadman T, Eklund H, Howley D, et al. Caregiver burden as people with autism spectrum disorder and attention-deficit/hyperactivity disorder transition into adolescence and adulthood in the United Kingdom. J Am Acad Child Adolesc Psychiatry. 2012;51:879–888.
- Grootscholten IAC, van Wijngaarden B, Kan CC. High functioning autism spectrum disorders in adults: consequences for primary caregivers compared to schizophrenia and depression. J Autism Dev Disord. 2018;48:1920–1931.
- van Steijn DJ, Oerlemans AM, van Aken MA, et al. The reciprocal relationship of ASD, ADHD, depressive symptoms and stress in parents of children with ASD and/or ADHD. J Autism Dev Disord. 2014;44:1064–1076.
- Eilenberg JS, Paff M, Harrison AJ, et al. Disparities based on race, ethnicity, and socioeconomic status over the transition to adulthood among adolescents and young adults on the autism spectrum: a systematic review. Curr Psychiatry Rep. 2019;21:32.
- Söderqvist H, Kajsa E, Ahlström BH, et al. The caregivers’ perspectives of burden before and after an internet-based intervention of young persons with ADHD or autism spectrum disorder. Scand J Occup Ther. 2017;24:383–392.
- Nguyen T, Stewart D, Gorter JW. Looking back to move forward: reflections and lessons learned about transitions to adulthood for youth with disabilities. Child Care Health Dev. 2018;44:83–88.
- Alwell M, Cobb B. Functional life skills curricular interventions for youth with disabilities: a systematic review. CDTEI. 2009;32:82–93.
- Lindsay S, Lamptey DL, Cagliostro E, et al. A systematic review of post-secondary transition interventions for youth with disabilities. Disabil Rehabil. 2019;41:2492–2505.
- Lindsay S, R. Hartman L, Fellin M. A systematic review of mentorship programs to facilitate transition to post-secondary education and employment for youth and young adults with disabilities. Disabil Rehabil. 2016;38:1329–1349.
- DaWalt LS, Greenberg JS, Mailick MR. Transitioning together: a multi-family group psychoeducation program for adolescents with ASD and their parents. J Autism Dev Disord. 2018;48:251–263.
- Hatfield M, Falkmer M, Falkmer T, et al. Evaluation of the effectiveness of an online transition planning program for adolescents on the autism spectrum: trial protocol. Child Adolesc Psychiatry Ment Health. 2016;10:48.
- Taylor JL, McPheeters ML, Sathe NA, et al. A systematic review of vocational interventions for young adults with autism spectrum disorders. Pediatrics. 2012;130:531–538.
- Oswald TM, Winder-Patel B, Ruder S, et al. A Pilot Randomized Controlled Trial of the ACCESS Program: a group intervention to improve social, adaptive functioning, stress coping, and self-determination outcomes in young adults with autism spectrum disorder. J Autism Dev Disord. 2018;48:1742–1760.
- Nadig A, Flanagan T, White K, et al. Results of a RCT on a transition support program for adults with ASD: effects on self-determination and quality of life. Autism Res. 2018;11:1712–1728. Epub 2018 Nov 19.
- Taylor JL, Hodapp RM, Burke MM, et al. Training parents of youth with autism spectrum disorder to advocate for adult disability services: results from a pilot randomized controlled trial. J Autism Dev Disord. 2017;47:846–857.
- Wentz E, Nyden A, Krevers B. Development of an internet-based support and coaching model for adolescents and young adults with ADHD and autism spectrum disorders: a pilot study. Eur Child Adolesc Psychiatry. 2012;21:611–622.
- Backman A, Mellblom A, Norman-Claesson E, et al. Internet-delivered psychoeducation for older adolescents and young adults with autism spectrum disorder (SCOPE): an open feasibility study. Res Autism Spectr Disord. 2018;54:51–64.
- Bishop-Fitzpatrick L, Minshew NJ, Eack SM. A systematic review of psychosocial interventions for adults with autism spectrum disorders. J Autism Dev Disord. 2013;43:687–694.
- Hesselmark E, Plenty S, Bejerot S. Group cognitive behavioural therapy and group recreational activity for adults with autism spectrum disorders: a preliminary randomized controlled trial. Autism. 2014;18:672–683.
- Lopez PL, Torrente FM, Ciapponi A, et al. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2018;3:Cd010840.
- Spain D, Blainey SH. Group social skills interventions for adults with high-functioning autism spectrum disorders: a systematic review. Autism. 2015;19:874–886.
- National Institute for Health and Care Excellene (NICE). Behaviour change: general approaches; 2007 [cited 2019 Jun 30]. Available from: www.nice.org.uk/guidance/ph6.
- National Institute for Health and Care Excellene (NICE). Behaviour change: individual approaches; 2014 [cited 2019 Jun 30]. Available from: www.nice.org.uk/guidance/ph49.
- Burke MM, Waitz-Kudla SN, Rabideau C, et al. Pulling back the curtain: issues in conducting an intervention study with transition-aged youth with autism spectrum disorder and their families. Autism. 2019;23:514–523.
- Antshel KM, Zhang-James Y, Faraone SV. The comorbidity of ADHD and autism spectrum disorder. Expert Rev Neurother. 2013;13:1117–1128.
- Elias R, White SW. Autism goes to college: Understanding the needs of a student population on the rise. J Autism Dev Disord. 2018;48:732–746.
- Kiresuk TJ, Smith A, Cardillo JE. Goal attainment scaling: applications, theory, and measurement. London: Psychology Press; 2014.
- Ruble L, McGrew JH, Toland MD. Goal attainment scaling as an outcome measure in randomized controlled trials of psychosocial interventions in autism. J Autism Dev Disord. 2012;42:1974–1983.
- Martell CR, Addis ME, Jacobson NS. Depression in context: strategies for guided action. New York: W. W. Norton; 2001.
- Dieterich M, Irving CB, Bergman H, et al. Intensive case management for severe mental illness. Cochrane Database Syst Rev. 2017;1:Cd007906.
- Hayes SC, Strosahl KD, Wilson KG. Acceptance and commitment therapy: an experimental approach to behavior change. London: Guilford Press; 1999.
- Choque Olsson N, Flygare O, Coco C, et al. Social skills training for children and adolescents with autism spectrum disorder: a randomized controlled trial. J Am Acad Child Adolesc Psychiatry. 2017;56:585–592.
- Hirvikoski T, Lindstrom T, Carlsson J, et al. Psychoeducational groups for adults with ADHD and their significant others (PEGASUS): a pragmatic multicenter and randomized controlled trial. Eur Psychiatry. 2017;44:141–152.
- Lund K, Hultqvist J, Bejerholm U, et al. Group leader and participant perceptions of Balancing Everyday Life, a group-based lifestyle intervention for mental health service users. Scand J Occup Ther. 2019. DOI:10.1080/11038128.2018.1551419.
- Jonsson U, Olsson NC, Coco C, et al. Long-term social skills group training for children and adolescents with autism spectrum disorder: a randomized controlled trial. Eur Child Adolesc Psychiatry. 2019;28:189–201.
- World Health Organization (WHO). International classification of diseases, 10th Revision (ICD-10). Geneva: WHO; 1992.
- Axén M, Brar A, Huslid H, et al. Regionalt vårdprogram: ADHD, lindrig utvecklingsstörning och autismspektrumtillstånd hos barn, ungdomar och vuxna [Regional Clinical Guidelines: ADHD, Intellectual Disability, and Autism Spectrum Disorder in Children, Adolescents, and Adults]. 2010 [cited 2019 Jun 30]. Available from: http://www1.psykiatristod.se/Global/vardprogram_fulltext/RV_ADHD_Utvecklingsstorning_Autism_2010.pdf.
- Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International Neuropsychiatric Interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry. 1998;59:22–33.
- Montgomery SA, Åsberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–389.
- Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997;12:38–48.
- Frisch M. Quality of life inventory: manual and treatment guide. New York: Bloomingdale PsychCorp; 1994.
- Jonsson U, Alaie I, Lofgren Wilteus A, et al. Annual research review: quality of life and childhood mental and behavioural disorders – a critical review of the research. J Child Psychol Psychiatr. 2017;58:439–469.
- Andersen A, Larsson K, Pingel R, et al. The relationship between self-efficacy and transition to work or studies in young adults with disabilities. Scand J Public Health. 2018;46:272–278.
- Shogren KA, Raley SK, Burke KM, et al. The self-determined learning model of instruction teacher’s guide. Lawrence, KS: Kansas University Center on Developmental Disabilities; 2019.
- Rounsaville BJ, Carroll KM, Onken LS. A stage model of behavioral therapies research: getting started and moving on from stage I. Clin Psychol. 2006;8:133–142.
- Bernfort L, Nordfeldt S, Persson J. ADHD from a socio-economic perspective. Acta Paediatr. 2008;97:239–245.
- Buescher AV, Cidav Z, Knapp M, et al. Costs of autism spectrum disorders in the United Kingdom and the United States. JAMA Pediatr. 2014;168:721–728.
