Abstract
Background
An intervention that contains several interacting components can be defined as a complex intervention. This intervention was developed in accordance with the Medical Research Council (MRC) guidance for complex interventions.
Aim
To describe the development, theoretical framework, and content of a client-centred activities in daily living intervention (CADL) for people with stroke.
Material and methods
Different steps were used; identifying the evidence base, identifying/developing theory and the modelling process and outcomes in the development of the CADL. The remodelling of the process and content of the intervention that emerged are defined.
Results
Findings from a series of qualitative studies of people with stroke demonstrated the need to develop an ADL intervention based on the clients’ lived experiences. The theoretical framework is based on empirical research, theories about human occupation and client-centredness. The CADL is applying an occupational and phenomenological perspective in order to enable agency in daily activities and participation in everyday life among persons with stroke.
Conclusions and significance
The article can be used as an example of how to present the development and theoretical framework of a new complex intervention in occupational therapy.
Introduction
The objective of this paper was to describe the development, theoretical framework and content of the client-centred activities in daily living intervention (CADL) for people with stroke in line with Medical Research Council (MRC) guidance for developing complex interventions (See ) [Citation1]. The effects of the CADL have been evaluated in a randomized controlled trial (RCT) (ClinicalTrials.gov NCT01417585) and the CONSORT Statement [Citation2] has been used to report the trial. The findings from the RCT were presented in both qualitative [Citation3,Citation4] and quantitative studies [Citation5–9]. However, the development, rationale and content of the intervention have been requested but have not yet been presented in detail. This article can also be used as an example of how to present the development and theoretical framework of a new complex intervention in occupational therapy.
Findings from a series of qualitative research studies aiming to better understand the lived experience of daily activities in everyday life after stroke [Citation10–16] was the main evidence base for the development of the CADL. The findings from these studies will be presented in further detail under the heading “The process of change” in this manuscript. An occupational and phenomenological perspective was applied using the client’s lived experiences as the point of departure for the client-centred intervention. The CADL is aiming to enable agency in daily activities [Citation17] and participation in everyday life [Citation18] among persons with stroke. According to Aarts and colleagues [Citation19], independence in ADL is associated with a person’s sense of agency in daily life, i.e. the feeling that a person is responsible for their own actions and their outcomes. Agency, from an occupational perspective, could be seen as a prerequisite to participation in daily activities and participation in everyday life. Enacting agency is a complex phenomenon that entails a person making things happen in everyday life through negotiating different aspects of various situations that may arise as part of continuous, changing transactional situations [Citation17]. Townsend and Laundry pointed out that the recognition of persons as active agents is important in interventions that aim to enable participation in everyday occupations [Citation20].
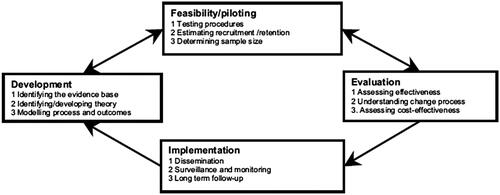
When an intervention depends on the interaction of multiple components, it can be described as a complex intervention. The CADL intervention was developed [Citation21,Citation22] by using the different phases of the MRC guidance [Citation1]. This present article has been outlined according to these phases as depicted in , although in practice this was an iterative rather than a linear process. The first step in the development of the CADL was to identify the evidence base. The second step was to identify and develop theory and the third step was the modelling process and outcomes. In the following, the framework of these three steps will be presented. The feasibility/piloting has been presented elsewhere [Citation21,Citation22] but the remodelling of the process and content of the CADL intervention that emerged from these studies will be described.
Development
Identifying the evidence base
Stroke often have consequences in everyday life functioning due to impairments, activity limitations and participation restrictions [Citation23,Citation24]. The sudden changes in people’s life world that are experienced as the subjective, historical, social, concrete and practical world [Citation25] can lead to the fact that you can no longer do the activities that you usually do [Citation26] in everyday life [Citation27,Citation28]. Our previous qualitative studies showed that after a stroke, people no longer experienced their daily activities as being taken-for-granted activities, i.e. activities that are performed automatically and without thinking [Citation14–16,Citation29–31]. Typical tasks such as dressing, eating, house cleaning as well as washing, working, hobbies and socializing with others, could not be performed as previously and a person often became dependent on others to carry out ADL.
Furthermore, people with mild stroke reported that they perceived there were restrictions in their participation in daily activities and social roles [Citation32] and that the change still was evident at six months [Citation33]. Family members were at risk of depression and reported caregiver burnout, social isolation, physical problems and decreased life satisfaction [Citation23,Citation24,Citation34]. Cardol, De Jong and Ward [Citation35] stressed that rehabilitation strategies should increase individual autonomy and participation in daily activities in order to enable persons to make decisions and act as they wish. Thus, there was an incentive to develop this ADL intervention with a view of enabling participation in ADL after stroke and reducing the caregiver’s burden.
The rehabilitation process after stroke is complex, involving many interacting components and multiple professionals. Commonly, the occupational therapists initiate an ADL assessment and training in the early phase of rehabilitation. Despite evidence of the beneficial effects of occupational therapy interventions to improve ADL ability and reduce the risk of deterioration of ADL ability after stroke [Citation23], the rationale and strategies for the interventions have often been vaguely defined and described.
Our previous qualitative studies identified that occupational therapists used different therapeutic strategies in their ADL interventions, such as providing structured instructions or feedback on specific client-identified activities and initiating adaptations within a familiar context [Citation12,Citation36,Citation37]. In order to strengthen the client-centred perspective in rehabilitation after stroke, it was necessary to understand the needs, priorities and goals of persons with stroke and their families [Citation38]. Hence, previous research showed that applying strategies and providing a structure for occupational therapy were essential components and should consequently be integral parts of the development of the CADL intervention.
Identifying/developing theory
Identify theory
The next step (see ) in the modelling of the content, process, and outcomes in the development of the CADL intervention was to identify and develop theory. The CADL intervention applied an occupational and phenomenological perspective in which the client’s lived experiences were used as the point of departure. The theoretical framework is presented in the following section.
The occupational perspective
The occupational perspective was based on the Model of Human Occupation (MOHO) [Citation39] as the MOHO seeks to explain how occupation is motivated, patterned and performed. According to Kielhofner [Citation39], many human life activities are taken for granted and are portrayed as activities that give structure and meaning to people’s everyday lives. The CADL was influenced by the MOHO’s emphasis on understanding what people do in their everyday lives. The MOHO was used to explain why problems in daily living could arise after stroke, and how impairments and environmental factors could disrupt occupational performance and participation in everyday life. The MOHO has also integrated a client-centred perspective and the concept of the lived body [Citation40], which is in line with the phenomenological perspective applied to the CADL.
Client-centredness
Another cornerstone of the CADL’s theoretical framework is the concept of client-centredness, which emerged from the Canadian Model of Occupational Performance (CMOP) and was [Citation41] characterized by strong links to practice, particularly to the client’s active participation in the process of occupational therapy. The concepts of person-centred, patient-centred and client-centred care and other similar concepts have been used interchangeably in healthcare research and practice. Client-centredness described by Carl Rogers, specifies that a therapeutic relationship requires an understanding and safe environment in which the person is the expert and the therapist is a tool to support the person in finding their own answers [Citation42]. Adopting a person-centred approach was also in line with the WHO’s goals for community-based rehabilitation. The goals state that people with disabilities and their family members should make their own decisions and take responsibility for changing their lives and improving their communities [Citation43].
A client-centred perspective implies that it is the client with perceived needs and desires who should drive the occupational therapy intervention [Citation44]. This approach supports the use of the client’s unique life-world experiences as the point of departure for goal setting and collaboration with the therapist in the rehabilitation process. Hence, working in a client-centred way in the CADL requires viewing the clients as partners in the rehabilitation process and recognizing their experiences, needs, goals and knowledge [Citation45]. It is also necessary to emphasize autonomy, choice, and partnership – the shared responsibility of the therapist and the client – enablement, contextual congruence, accessibility and respect for diversity [Citation3].
It is fundamental in rehabilitation to create opportunities in practice and experiences in the performance of everyday occupations, based on trust and an informed relationship with the client. It is also essential to involve the person’s significant others and gradually assist the person to gain autonomy in decision-making and action [Citation17]. A systematic review by Kristensen and co-authors [Citation46] concluded that there was support for a client-centred approach after stroke, as persons felt more involved and had a higher survival rate when they had received rehabilitation that focussed on their own goals. In CADL, the interaction between the therapist and the client is based on the client’s experiences and desires in order to support the clients to achieve their goals. This is a guiding principal of the CADL intervention [Citation41].
The concept of Activities of Daily Living (ADL)
During the development of the intervention, the definition of ADL was refined and widened in order to be in accordance with the concepts of occupation [Citation39] and client-centredness [Citation41]. Traditionally, the concept of ADL was divided into two parts, i.e. personal ADL (P-ADL), including personal tasks such as using the toilet, bathing, dressing, eating and grooming, and instrumental ADL (I-ADL) [Citation47], which included more complex tasks such as taking care of the household, financial management, driving a car. The ADL definition used in the CADL intervention includes all activities that a person needs and wants to perform [Citation47].
A phenomenological perspective – the lived experience
In CADL the importance of understanding the client’s experiences of daily activities after stroke is emphasized. The phenomenological concept of life-world and life-world experiences emerged from Husserl [Citation25], who defined the concept of life-world as the individualized life-world that is obvious and concrete and is subjective and taken for granted in our everyday lives without questioning its existence. According to Husserl [Citation25], the life-world is a social world in which people live, communicate with and understand each other, and focuses on the person’s experiences in everyday life. Thus, the understanding and awareness of the life-world might be viewed differently by different persons. Merleau-Ponty [Citation26], building on Husserl’s life-world concept, introduced the “lived body” as something in which the life-world is the lived world to which people have access through their bodies. Moreover, the body itself is the foundation of a person’s life-world and it is through the body that a person perceives the world [Citation26]. He stated that the person is “the body and you cannot separate the life-world from the body”. The body is viewed as being always present in a person’s daily activities and is also the starting point from which people act and understand their life-worlds. The body is not seen as a separate object; instead, the body is lived or experienced in immediate connection with the environment in everyday life. A disability often leads to a changed body and thereby a changed life-world and might result in difficulties understanding the lived experience of disability and loss of activities, which are common after a stroke. Our phenomenological studies (n = 15) have shown that occupational therapists could use their empathetic understanding to enter their clients’ life-worlds and should meet them in their changing life-worlds over time. The findings of research that adopted a phenomenological approach can guide occupational therapists’ understanding of the lived experience of disability [Citation27], which was used as a cornerstone of the theoretical framework in the development of the CADL intervention.
When we identified the theoretical framework in the guidance for complex interventions (see ), the next step was to summarize the development of theory in the research group to be used as a platform in the development and modelling of the intervention.
Developing theory
A qualitative research synthesis (QRS) [Citation48] of the findings from qualitative studies (n = 15) conducted in the research group [Citation10–16,Citation29–31,Citation37,Citation49–52] was performed. Most of these studies were based on interview data on the lived experiences in everyday life after acquired brain injury, mainly stroke [Citation14,Citation29–31,Citation50,Citation52]. These studies applied a phenomenological approach – the Empirical Phenomenological Psychological (EPP) method [Citation53] – although the psychological perspective was replaced by an occupational perspective [Citation10,Citation14–16,Citation29–31,Citation37,Citation50,Citation52] and the phenomenology perspective of Merleau-Ponty [Citation26] was incorporated into the analyses. A few studies also applied a constant comparative Grounded Theory approach [Citation30,Citation31,Citation54,Citation55].
Modelling process and outcome
The findings from the QRS served as a basis for developing and integrating theory in the modelling of the CADL intervention. A number of general characteristics of the process of change, and of how significant experiences from engaging in daily activities appeared to enable change, were identified across the studies included in the QRS. A summary of the synthesis is presented in the following section.
The process of change
Several studies showed the importance of enabling discovery and awareness of disabilities in order to gradually learn how to solve problems in daily activities after stroke. This discovery process [Citation10] appeared to be a prerequisite for finding and using conscious strategies to solve problems [Citation10,Citation11,Citation13–15,Citation29,Citation30,Citation49–51]. Two phenomenological studies [Citation12,Citation37] and a mixed methods study [Citation56] identified the therapeutic strategies used by therapists.
There were some common characteristics across the series of qualitative studies on persons’ lived experience in daily activities after stroke when describing the process of change that persons with stroke experienced during their rehabilitation [Citation14–16,Citation29–31]. The general characteristics of the process of change are presented in a “non-linear” process () and were used in the modelling of CADL. In , the characteristics are also linked to the different components of CADL.
Table 1. General characteristics of the process of change after stroke, and their links to the components of the CADL intervention.
The general characteristics of the process of change showed how significant experiences from doing desired and valued daily activities contributed to change, described as experiences of agency in daily activities and participation in everyday life [Citation17,Citation18]. This was formulated as the general aim of the CADL intervention. The general characteristics of the process of change were used in the modelling of the CADL and these also served to guide the therapists’ understanding of how to enable significant experiences. In the following, the seven general characteristics of the process of change are presented.
1. Discovering the new body and self by doing familiar activities
The persons’ experiences from doing activities that were formerly taken for granted contributed to discovery after stroke. By engaging in familiar activities, the persons learned about their new body and about their abilities by comparing them with their old self. Learning about their new body was easier in activities that had previously been incorporated into the person’s habit-body, i.e. habits and routines had been integrated into the body and were taken for granted in everyday life [Citation26]. Familiar contexts and objects supported the doing and discovery of the new body and self [Citation10,Citation13–18,Citation29–31,Citation50,Citation57].
2. Incorporating new discoveries into familiar activities
Experiences from doing familiar activities were linked to the person’s former experiences and habit-body. Gradually, the person’s “new body” was discovered and incorporated into daily living. Experiences from situations that gave “just the right challenge” contributed to the incorporation of the “new” into daily living [Citation13–16,Citation19,Citation29–31,Citation50,Citation57].
3. Learning how to solve problems by doing valued activities
The most important facilitators in the recovery process were the experiences from doing activities that had purpose and meaning. By performing engaging activities, which the clients were asked to do on their own, they learned how to solve problems. Activities that were linked to their sense of self, identity or social roles, such as working, travelling and being an active member of a union, were important and allowed them to recognize themselves and see a possible future. Experiences of doing activities that they felt a strong desire to do were important facilitators in the recovery process. Engaging in activities that had purpose and meaning also facilitated a series of activities in daily life; and doing activities in inspiring places was regarded as enabling recovery [Citation10,Citation11,Citation14–16,Citation29–31,Citation50,Citation57].
4. Using conscious strategies in frequently performed activities
Frequent experience of trying to solve problems when doing familiar activities on their own was a prerequisite for finding and using conscious strategies to solve problems. Persons with stroke needed to be gradually confronted with the problems by having different types of feedback on their performance in order to understand the problem and how to solve it. The struggle of doing activities was a facilitator, although some situations were too challenging, and no feedback was received.” Just the right challenge” kinds of experiences contributed to discovery and the ability to solve problems in doing [Citation10,Citation11,Citation14,Citation15,Citation30].
By practicing conscious strategies in activities on a daily basis, persons with stroke became more capable of using conscious strategies to solve problems in doing. Finding and using strategies were a prerequisite for incorporating the strategies into their new-old habits in everyday life [Citation10,Citation11,Citation13–15,Citation29,Citation30].
5. Experiencing a sense of belonging by sharing activities with others
Performing activities with others who understood their experiences contributed to experiences of a sense of belonging. At first, other persons enabled a structure and were experienced as guides in managing the new world, or as an extension of the body in daily living [Citation11]. Doing and interacting with significant others and with colleagues and other patients was a prerequisite for recovery. Re-establishing relationships with colleagues at their workplaces was described as very important for recovery among persons of working age [Citation16,Citation17,Citation30,Citation50,Citation58].
6. Experiencing the meaning of doing in a new way
Experiencing and understanding the meaning of using a strategy or a new way of doing was a prerequisite for recovery. Practicing former habits in a new way was a prerequisite for the incorporation of new-old habits and for experiencing the meaning of doing in a new way [Citation10,Citation13–16,Citation29–31,Citation50,Citation57]. For example, by performing familiar activities in familiar contexts, persons with stroke appeared to link their present experience with their former experience, which helped them perform the activities more as a routine and as part of a new habit pattern, which they could perform coherently without consciously thinking about it [Citation14].
7. Experiencing a possible future horizon
Through their experiences of doing, the persons gradually re-valued the meaning of carrying out certain activities in daily life. The experience of the “new meaning” was a prerequisite for making new decisions and setting goals for the future. Often, activities that had previously been important to them changed their meaning. Experiencing the meaning of doing in a new way or carrying out new activities was a prerequisite for doing in a new way and for experiencing a future horizon [Citation14,Citation15,Citation29–31,Citation57]. By gradually discovering their own strengths and weaknesses when performing daily activities, it appeared as if the future horizon became visible to them.
To conclude, the results from the research synthesis of the series of empirical studies provided support for: (1) applying a phenomenological perspective in the CADL intervention by taking the person’s unique life-world experiences as the point of departure, and (2) enabling the individual to have significant experiences of performing present, and for the future desired and valued activities – within a social context. The combination of understanding the client’s unique life-world and enabling a significant experience from doing were identified as the two most important general strategies for the occupational therapists to integrate into the therapeutic process of the CADL in order to enable change.
Feasibility/piloting
Several feasibility studies have been conducted during the process of developing the CADL intervention (see , Feasibility and piloting) in order to test concepts and procedures as well as estimate recruitment and decide on the sample size [Citation21,Citation22]. The modelling of the complex intervention provided important information about the design of both the intervention and the evaluation process. The following section describes the modelling of the process and content of the CADL intervention that emerged from the identified evidence, theory base, and the developed theory (see ) that influenced the components and strategies that developed the model of the intervention.
Testing procedures
A pilot study was an essential step in the development and testing of the Client-Centred Self-Care Intervention (CCSCI), which was the first pilot version of the CADL. The purpose was to study the feasibility of the design and the procedures [Citation21,Citation22]. The results from these pilot studies led to remodelling and revision of the CCSCI.
Remodelling the process and outcomes
During this research process, based on the results of the pilot study [Citation21,Citation22], we found the study design and methods to be appropriate for a full-scale RCT [Citation5], but with the following modifications: (1) to evaluate the intervention at different stages of the post-stroke rehabilitation process in order to also follow the impact of the intervention in relation to spontaneous recovery and other rehabilitation services and, (2) to include other occupational domains in addition to personal and instrumental ADL, such as recreational activities or productivity, which may be of importance for the individual client in a later phase of rehabilitation and, (3) change the name from ‘course’ to ‘workshop’ to give the participating occupational therapists’ adequate expectations from the beginning in order to enable their engagement and active learning. By integrating new knowledge from recent qualitative studies conducted by the HELD research group (Health in Everyday Life among people with neurological Disorders) and others, as well as theory/evidence [Citation39,Citation41,Citation59,Citation60,Citation61], a draft of the new client-centred ADL intervention (CADL) was designed for persons with stroke.
Modelling the process of the client-centred ADL intervention (CADL)
In 2009, the CADL was further developed in five workshops by 44 occupational therapists working in inpatient geriatric rehabilitation, inpatient medical rehabilitation and home-based rehabilitation, with experience (of between 2 and 39 years) of the rehabilitation of stroke patients. The researchers (first, second) led the workshop (n = 5) (five full days spread over one month), which aimed to bridge the gap between praxis and research through dialogue and collaboration, which is consistent with a scholarship of practice framework [Citation39]. The workshop used a collaborative approach, which enabled the active engagement of the participating occupational therapists. By facilitating peer learning, the therapists and the researchers were able to learn from each other. Researchers with extensive experience of rehabilitation were involved in both the workshop and in the implementation of the CADL.
The content of the workshops included lectures by experienced researchers about the concepts and theories behind the intervention, reading and discussion of the articles [Citation12,Citation15,Citation16,Citation21] behind the intervention, as well as working with a case with the objective of understanding how research-based knowledge was integrated into the CADL. During the workshop and the implementation of the CADL in clinical practice, the researchers discussed to establish fewer goals during the rehabilitation process than previously decided (from five goals to three goals) and it was assumed that the steps in CADL were more like components in a non-linear intervention process.
The CADL content
In the following section, the nine components that together build up the CADL intervention process are presented. The nine components focus on occupational therapists’ actions and strategies. Each component is complex and includes multiple strategies. The rationale of each component is also described, as well as how the component (i.e. comprising actions and strategies) relates to the other components and is expected to enable significant experiences and changes in accordance with the process of change identified by the QRS [Citation48] (see ).
The overall aim of the CADL intervention is to enable agency in daily activities and participation in everyday life among persons with stroke. The CADL intervention is conducted in a client-centred context [Citation41] and should be adjusted to the individual’s ability, motivation, perceptions and needs in close collaboration between the client and therapist. The CADL intervention provides a structure for how to discover and solve problems encountered in daily activities after stroke. Two general strategies are combined and used by the occupational therapists across the nine components (i.e. during the entire intervention process) in order to enable change: (1) using the client’s lived experience as a point of departure, and (2) enabling significant experience to be gained from engaging in valued daily activities.
The nine components applied to the therapeutic process: From Scholarship to Practice
1) The first meeting with the client
Initially, the occupational therapists need to focus on their first meeting with the client in order to establish a relationship when starting the CADL intervention. The occupational therapists need to understand each client’s unique lived experiences of the new situation after stroke in order to meet the client where they need to be met as a point of departure for the intervention process. The essential strategy is to create an atmosphere of empathy and understanding regarding the client’s lived experiences in order to establish a relationship of trust with the clients and to find a proper way of inspiring the client. Understanding the client’s lived experience is a strategy the occupational therapists use during the entire intervention process to maintain a relationship based on trust. Since experiences a sense of chaos are common at the beginning of the recovery process after stroke, the occupational therapists need to take time to listen to their client’s experiences.
2) Observation in an activity
A combined strategy of collecting information from conversations and observations in actual practical situations is used by the occupational therapist to create a picture and understanding of their client’s situation. Observation of the client is conducted when performing a familiar activity of the client’s choice. The therapist and client need to understand the client’s actual ability to perform activities in order to create a shared understanding of the client´s ability to perform ADLs and need to participate in the CADL intervention. The observation and the client’s experience of doing is important for the next step.
3) Scoring the activity together
The occupational therapist evaluates the ADL performance with their client, either with or without an ADL instrument. The occupational therapist creates a “seeing situation” for their client to enable them to learn to understand their ability, realize the value of the intervention and be able to set the goals together. Scoring the activity together helps both client and therapist to discover any difficulties in performing the activity, but also shows how the client values activities and performance.
4) Formulating goals by using the COPM
Another important component of the CADL is the Canadian Occupational Performance Measure (COPM) [Citation60], an individualized, client-centred measurement designed to be used by occupational therapists to identify changes over time in a client’s perception of their own ability to perform different activities. The measure is designed to detect changes in a client’s self-perception of occupational performance over time. The client needs to understand the expectations and goals of the intervention in order to be ready to collaborate with the therapist in a partnership. A prerequisite for a person to consciously use compensatory strategies and incorporate them in their daily life is to be aware of their problems [Citation10] and to set goals for their rehabilitation [Citation60].
5) Using GOAL-PLAN-DO-CHECK
The occupational therapists’ enablement of the client’s discovery of the new situation [Citation10] is intended to facilitate the learning and problem-solving process. Thus, a global problem-solving strategy [Citation62] is introduced to provide a structure for the therapist and the client to talk through the Goal-Plan-Do-Check strategy in relation to the problems encountered in the performance of the ADL. In component 4, the client identifies goals based on the COPM, and in component 5 the therapist guides them in the discovery and formulation of an intervention plan to meet the goals. The client will then perform the activity according to the plan in order to gain experience of doing and discovering and checking whether the plan has been effective. If the client does not achieve the goal, the therapist and the client modify the plan together.
A key component is that clients are encouraged to discover these new strategies by themselves and are guided by their occupational therapist in this active exploration. The therapist should support the clients in becoming their own problem solvers rather than solving the problems for them. The client needs to practice the problem-solving strategy in different activities and contexts, both with their therapist and on their own (see component 8).
6) Using a diary as a structure for training
A training diary is used during the intervention process to give a structure to the implementation of the problem-solving strategy in everyday life. The client and their occupational therapist plan the CADL intervention and how and when the client should perform the chosen activities, and the client is encouraged to keep a training diary. The diary helps the client resume responsibility for their own goals and training and is also used as a tool to inform others about and document the training related to the goals of the CADL intervention.
7) Reporting and involving others
The occupational therapist supports the client to inform their significant others and other staff members at the rehabilitation clinic about their goals and planned strategies for the CADL intervention. The problem-solving strategy and the use of formulating goals, a plan, and the strategies used for performing the activities and a “self-check” are explained to relatives, home help services and other persons close to the client in order to enable them to support the client in using the strategies in daily activities. The therapeutic relationship with occupational therapists, social interactions with others, and being in a supportive context all appear to be prerequisites for recapturing ADL [Citation15,Citation16].
8) Training to perform and integrate activities
One important component of the CADL intervention is to enable the clients to practice and integrate daily activities by using the global problem-solving strategy as a structure for doing in a new way. The client practices the chosen activities named in the intervention plan using the planned strategies, both on their own and with their occupational therapist. The strategies used by the occupational therapists to enable significant experiences that contribute to change make the competence visible to the client, facilitating the discovery of the new body and doing, and revealing new solutions to problems in activities that have purpose and meaning. For the training to be successful, the therapists need to adjust the training to the needs of the clients. In order to give the clients adequate challenges, the occupational therapists gradually withdraw their support, guidance and presence during the CADL intervention. By repeatedly engaging in different daily activities, the clients integrate new strategies and ways of doing in everyday life after stroke.
9) Evaluation of the goals
During the rehabilitation process, when the goals according to the COPM have been evaluated and achieved, the client and their occupational therapist discuss and evaluate the strategies that have been implemented and then formulate new goals and strategies together. Clients often need help to organize their day and establish new routines and structures in their everyday lives. By integrating concrete structures for doing things, the challenges in performing daily activities can be adjusted to meet the client’s present ability and future goals. Gradually, the client takes over responsibility for implementing the global problem-solving strategy in their everyday life.
Discussion
An ADL intervention is a standard part of the rehabilitation process after stroke and there is empirical evidence to support the beneficial effects of an ADL intervention [Citation63]. However, the theoretical rationale and strategies for how to apply ADL interventions after stroke were not clearly defined in research conducted before the development of the CADL intervention (i.e. before 2009). We therefore found it important to report on how we developed the theoretical base and modelled the content of the new and complex ADL intervention, before the effectiveness of the intervention was evaluated in an RCT [Citation5–9]. Nevertheless, developing and evaluating a new and complex client-centred intervention has been a long process involving multiple phases. We have learnt that qualitative research can be used as an important framework for modelling the content of an intervention, but it also served to better understand the therapeutic components and underlying rationale of the intervention. This is in line with the MRC guidance of developing complex interventions in health care [Citation1]. By conducting longitudinal qualitative studies on the experiences of clients, significant others and rehabilitation professionals during the rehabilitation and recovery process, researchers and therapists can refine the intervention strategies and implement the new knowledge and understanding in clinical practice.
To our knowledge, this qualitative approach as a framework for complex intervention research has not previously been described in detail, even though the benefit of using qualitative methods to generate knowledge of the implementation of an intervention has been highlighted [Citation63]. Furthermore, according to Upshure and colleagues [Citation64], knowledge derived from qualitative research has the potential to redefine best practice in rehabilitation. By understanding the nature of the lived experience [Citation14] after stroke and how experiences may change [Citation40] in the process of recapturing ADL [Citation15,Citation16], therapists need to integrate this understanding in their clinical work [Citation65–67]. This paper described a systematic and clear process based on current scholarship and grounded in theory that occupational therapists can utilize in practice to enhance participation in meaningful activities for persons with stroke.
However, developing new interventions and testing these interventions in feasibility studies takes time. Since the beginning of the development of the CADL (2009), new research and evaluations have been conducted that contribute to new knowledge and evidence. For example, research has provided findings [Citation68–70] that support the components of the CADL intervention, such as guided goal setting and the use of COPM. Furthermore, the findings from Skidmore and colleagues [Citation68,Citation69] regarding the use of strategy training, in which the therapists, in the same way as in the CADL, guided the participants learning through their own experiences.
Several implications for future scholarship and practice can be drawn from this project. In a review by Wolf and colleagues [Citation71], the findings from the first pilot version of the CADL [Citation21,Citation22] were included and the authors pointed out that it was difficult to draw any conclusions from the studies as they lacked an adequate description of the interventions that were evaluated. Unfortunately, poor descriptions of interventions negatively affect the ability to understand and implement the interventions with future clients. Thus, the intention of this paper was to clearly define and describe the theoretical framework and how the components of the intervention were developed and implemented. This could offer practical guidelines for how to apply CADL. In other publications of CADL, the description of the intervention has been limited due to restrictions in the number of pages of articles in scientific journals.
However, the underlying therapeutic mechanisms of the CADL need to be further investigated by synthesizing the findings from all studies conducted on the CADL. Another important field of future research is to evaluate complex and client-centred rehabilitation interventions after stroke by identifying or developing assessment instruments that are sensitive to detecting changes in complex processes. Finally, we need to investigate whether this model of the CADL and its components could be viewed as a generic process model that could be applied to other groups than people with stroke.
In summary, by conducting a series of both quantitative and qualitative studies in accordance with the MRC guidance [Citation1], it is possible to develop theory-based models for intervention that are likely to be easier to implement if the intervention is based on the experiences of clients and rehabilitation professionals [Citation65,Citation72] and is developed in collaboration with researchers. According to the MRC guidance of best practice, we have developed the CADL intervention systematically as we were using the best available evidence and appropriate theory at the time. We tested the intervention by using a carefully phased approach in which we started with a pilot study and moved on to an RCT study. The results have been as widely disseminated as possible. We also monitored the implementation process and recognized that further research was needed and that CADL modelling will continue in the future.
Disclosure statement
The authors report no conflicts of interest. The authors are solely responsible for the content and writing of the paper.
Additional information
Funding
References
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655.
- Boutron I, Moher D, Altman DG, et al. Extending the CONSORT statement to randomized trials of nonpharmacologic treatment: explanation and elaboration. Ann Intern Med. 2008;148:295–309.
- Ranner M, Guidetti S, von Koch L, et al. Experiences of participating in a client-centred ADL intervention after stroke. Disabil Rehabil. 2019;41:3025–3033.
- Bertilsson A, von Koch L, Tham K, et al. Client-centred ADL intervention after stroke: significant others’ experiences. Scand J Occup Ther. 2015;22:377–386.
- Bertilsson AS, Ranner M, von Koch L, et al. A client-centred ADL intervention: three-month follow-up of a randomized controlled trial. Scand J Occup Ther. 2014;21:377–391.
- Guidetti S, Ranner M, Tham K, et al. A client-centred ADL intervention for persons with stroke: one-year follow-up of a randomized controlled trial. J Rehabil Med. 2015;47:605–611.
- Bertilsson AS, Eriksson G, Ekstam L, et al. A cluster randomized controlled trial of a client-centred, activities of daily living intervention for people with stroke: one year follow-up of caregivers. Clin Rehabil. 2016;30:765–775.
- Gustavsson M, Guidetti S, Eriksson G, et al. Factors affecting outcome in participation one year after stroke: a secondary analysis of a randomized controlled trial. J Rehabil Med. 2019;51:160–166.
- Hedman A, Eriksson G, von Koch L, et al. Five-year follow-up of a cluster-randomized controlled trial of a client-centred activities of daily living intervention for people with stroke. Clin Rehabil. 2019;33:262–276.
- Tham K, Borell L, Gustavsson A. The discovery of disability: a phenomenological study of unilateral neglect. Am J Occup Ther. 2000;54:398–406.
- Tham K, Kielhofner G. Impact of the social environment on occupational experience and performance among persons with unilateral neglect. Am J Occup Ther. 2003;57:403–412.
- Guidetti S, Tham K. Therapeutic strategies used by occupational therapists in self-care training: a qualitative study. Occup Ther Int. 2002;9:257–276.
- Lampinen J, Tham K. Interaction with the physical environment in everyday occupation after stroke: a phenomenological study of visuospatial agnosia. Scand J Occup Ther. 2003;10:147–156.
- Erikson A, Karlsson G, Borell L, et al. The lived experience of memory impairment in daily occupation after acquired brain injury. OTJR: Occup Participat Health. 2007;27:84–94.
- Guidetti S, Asaba E, Tham K. The lived experience of recapturing self-care. Am J Occup Ther. 2007;61:303–310.
- Guidetti S, Asaba E, Tham K. Meaning of context in recapturing self-care after stroke or spinal cord injury. Am J Occup Ther. 2009;63:323–332.
- Bergström A, Eriksson G, Asaba E, et al. Complex negotiations: the lived experience of enacting agency after a stroke. Scand J Occup Ther. 2015;22:43–53.
- Fallahpour M, Jonsson H, Joghataei M, et al. “I am not living my life”: lived experience of participation in everyday occupations after stroke in Tehran. J Rehabil Med. 2013;45:528–534.
- Aarts H, Custers R, Marien H. Priming and authorship ascription: when nonconscious goals turn into conscious experiences of self-agency. J Pers Soc Psychol. 2009;96:967–979.
- Townsend E, Landry J. Interventions in a societal context: enabling participation. In: Christiansen C, Baum C. editors. Occupational therapy, performance, participation, and well-being. Thorofare New Jersey: Slack Inc.; 2005. p. 495–518.
- Guidetti S, Andersson K, Andersson M, et al. Client-centred self-care intervention after stroke: a feasibility study. Scand J Occup Ther. 2010;17:276–285.
- Guidetti S, Ytterberg L. A randomised controlled trial of a client-centred self-care intervention after stroke: a longitudinal pilot study. Disabil Rehabil. 2011;33:494–503.
- Legg L, Drummond A, Leonardi-Bee J, et al. Occupational therapy for patients with problems in personal activities of daily living after stroke: systematic review of randomised trials. BMJ. 2007;335:922.
- Steultjens EMJ, Dekker J, Bouter LM, et al. Occupational therapy for stroke patients: a systematic review. Stroke. 2003;34:676–687.
- Husserl E. The crisis of European sciences and transcendental phenomenology. Evanston (IL): Northwestern University Press; 1970. Original work: Die Krisis der europäischen Wissenschaften und die transzendentale Phänomenologie, Philoshopia; 1936.
- Merleau-Ponty M. Phenomenology of perception. (C. Smith, Trans.) London: Routledge & Kegan Paul Ltd; 2002/1945.
- McKevitt C, Redfern J, Mold F, et al. Qualitative studies of stroke: a systematic review. Stroke. 2004;35:1499–1505.
- Rudman DL, Hebert D, Reid D. Living in a restricted occupational world: the occupational experiences of stroke survivors who are wheelchair users and their caregivers. Can J Occup Ther. 2006;73:141–152.
- Eriksson G, Tham K. The meaning of occupational gaps in everyday life after the first year after stroke. OTJR: Occupat Participat Health. 2010;30:49–58.
- Erikson A, Park M, Tham K. Belonging: a qualitative, longitudinal study of what matters for persons after stroke during the one year of rehabilitation. J Rehabil Med. 2010;42:831–838.
- Erikson A, Park M, Tham K. Place integration through daily activities: one year of rehabilitation after stroke. OTJR: Occupat Participat Health. 2010;20:68–77.
- Rochette A, Desrosiers J, Bravo G, et al. Changes in participation after a mild stroke: quantitative and qualitative perspectives. Top Stroke Rehabil. 2007;14:59–68.
- Kelly-Hayes M, Beiser A, Kase C, et al. The influence of gender and age on disability following ischemic stroke. The Framingham study. J Stroke Cerebrovasc Dis. 2003;12:119–126.
- Eriksson G, Tham K, Fugl-Meyer AR. Couples’ happiness and its relationship to functioning in everyday life after brain injury. Scand J Occup Ther. 2005;12:40–48.
- Cardol M, De Jong BA, Ward CD. On autonomy and participation in rehabilitation. Disabil Rehabil. 2002;24:970–974.
- Gahnström-Strandqvist K, Tham Josephsson S, et al. Actions of competence in occupational therapy practice. Scand J Occup Ther. 2000;7:15–25.
- Wohlin Wottrich A, von Koch L, Tham K. The meaning of rehabilitation in the home environment after acute stroke from the perspective of a multiprofessional team. Phys Ther. 2007;87:778–788.
- Lawrence M, Kinn S. Defining and measuring patient-centred care: an example from a mixed-methods systematic review of the stroke literature. Health Expect. 2012;15:295–326.
- Kielhofner G. Model of human occupation: theory and application. 4th ed. Baltimore (MD): Lippincott Williams & Wilkins, A Wolters Kluwer business; 2008.
- Kielhofner G, Tham K, Baz T, et al. Performance capacity and the lived body. In: Kielhofner G, editor. A model of human occupation. Theory and application. 3rd ed. Baltimore: Lippincott Williams & Wilkins; 2002.
- Townsend EA, Polatajko JH. Enabling occupation II: advancing an occupational therapy vision for health, well-being, and justice through occupation. Ottawa (Ontario): CAOT Publications ACE; 2007.
- Rogers CR. Client-centered therapy: its current practice, implications, and theory. Boston: Houghton Mifflin; 1951.
- World Health Organisation. Community-based rehabilitation guidelines: World Health Organization; 2003 [cited 2020 Mar 27]. Available from: https://www.who.int/publications-detail/community-based-rehabilitation-cbr-guidelines.
- Law M, Baptiste S, Mills J. Client-centred practice: what does it mean and does it make a difference? Can J Occup Ther. 1995;62:250–257.
- Ranner M, von Koch L, Guidetti S, et al. Client-centred ADL intervention after stroke: occupational therapists’ experiences. Scand J Occup Ther. 2016;23:81–90.
- Kristensen HK, Persson Nygren C, Boll M, et al. Evaluation of evidence within occupational therapy in stroke rehabilitation. Scand J Occup Ther. 2011;18:11–25.
- Fisher AG. Uniting practice and theory in occupational framework 1998. Eleonor Clark Slage Lecture. Am J Occup Ther. 1998;52:509–521.
- Major CH, Savin-Baden M. An introduction to qualitative research synthesis: managing the information explosion in social science research. New York (NY): Routledge; 2010.
- Ekstam L, Tham K, Borell L. Couples’ approaches to changes in everyday life during the first year after stroke. Scand J Occup Ther. 2011;18:49–58.
- Johansson U, Tham K. The meaning of work after acquired brain injury. Am J Occup Ther. 2006;60:60–69.
- Patomella A-H, Johansson K, Tham K. Lived experience of driving ability following stroke. Disabil Rehabil. 2009;31:726–733.
- von Koch L, Wottrich AW, Holmqvist LW. Rehabilitation in the home versus the hospital: the importance of context. Disabil Rehabil. 1998;20:367–372.
- Karlsson G. Psychological qualitative research from a phenomenological perspective. Stockholm: Almqvist & Wiksell International; 1993.
- Charmaz K. Constructing grounded theory: a practical guide through qualitative analysis. London: SAGE; 2006.
- Glaser B, Strauss A. The discovery of grounded theory: strategies for qualitative research. Chicago (IL): Aldine Publishing Co; 1967.
- von Koch L, Holmqvist LW, Wottrich AW, et al. Rehabilitation at home after stroke: a descriptive study of an individualized intervention. Clin Rehabil. 2000;14:574–583.
- Erikson A, Karlsson G, Söderström M, et al. A Training apartment with electronic aids to daily living: lived experiences of persons with brain damage. Am J Occup Ther. 2004;58:261–271.
- Fallahpour M, Tham K, Joghataei MT, et al. Perceived participation and autonomy: aspects of functioning and contextual factors predicting participation after stroke. J Rehabil Med. 2011;43:388–397.
- The National Board of Health and Welfare. [Nationella riktlinjer för vård vid stroke] National guidelines for Stroke Care. 2018 [cited 2020 Nov 12]. Available from: https://www.socialstyrelsen.se/regler-och-riktlinjer/nationella-riktlinjer/slutliga-riktlinjer/stroke/.
- Law M, Baptiste S, Mills J. Canadian occupational performance measure. Toronto: CAOT Publications; 1991.
- Legg LA, Lewis SR, Schofield-Robinson OJ, et al. Occupational therapy for adults with problems in activities of daily living after stroke. Cochrane Database Syst Rev. 2017;(7):CD003585.
- Polatajko HJ, Mandich AD, Missiuna C, et al. Cognitive orientation to daily occupational performance (CO-OP): Part III – The protocol in brief. Phys Occup Ther Pediatr. 2001;20:107–123.
- Moore GF, Audrey S, Barker M, et al. Process evaluation of complex interventions: Medical Research Council guidance. BMJ. 2015;350:h1258.
- Upshur RE, VanDenKerkhof EG, Goel V. Meaning and measurement: an inclusive model of evidence in health care. J Eval Clin Pract. 2001;7:91–96.
- Eriksson C, Tham K, Guidetti S. Occupational therapists’ experiences in integrating a new intervention in collaboration with a researcher. Scand J Occup Ther. 2013;20:253–263.
- Eriksson C, Erikson A, Tham K, et al. Occupational therapists experiences of implementing a new complex intervention in collaboration with researchers: a qualitative longitudinal study. Scand J Occup Ther. 2017;24:116–125.
- Eriksson C, Eriksson G, Johansson U, et al. Occupational therapists’ perceptions of implementing a client-centered intervention in close collaboration with researchers: a mixed methods study. Scand J Occup Ther. 2020;27:142–153.
- Skidmore ER, Dawson DR, Whyte EM, et al. Developing complex interventions: lessons learned from a pilot study examining strategy training in acute stroke rehabilitation. Clin Rehabil. 2014;28:378–387.
- Skidmore ER, Dawson DR, Butters MA, et al. Strategy training shows promise for addressing disability in the first 6 months after stroke. Neurorehabil Neural Repair. 2015;29:668–676.
- Polatajko H, McEwen SE, Ryan JD, et al. Pilot randomized controlled trial investigating cognitive strategy use to improve goal performance after stroke. Am J Occup Ther. 2012;66:104–109.
- Wolf TJ, Chuh A, Floyd T, et al. Effectiveness of occupation-based interventions to improve areas of occupation and social participation after stroke: an evidence-based review. Am J Occup Ther. 2015;69:6901180060p1–6901180060p11.
- Whalley H. K. Client-centred practice in occupational therapy: critical reflections. Scand J Occup Ther. 2013; 20:174–181.