Abstract
Background
It is important to understand how healthy lifestyle habits can be developed as they are essential in cardiovascular disease (CVD) prevention. There is limited knowledge regarding whether, and how, engaging occupations (things that people do and occupy themselves with) can promote and help sustain healthy lifestyle habits for persons at risk for CVDs, including stroke.
Aim
The aim was to develop knowledge of how engaging in occupations can contribute to changes in lifestyle habits among persons at risk for stroke.
Methods
Six adults presenting with stroke risk factors were interviewed on several occasions after participating in an occupation-focused stroke prevention programme. Grounded theory was utilised, and constant comparative methods guided the analysis.
Findings
Changing lifestyle habits was perceived as a complex process, much like weaving a fabric with many parallel and interlacing threads. Literacy of both health and occupations and participation in engaging occupations were important facilitators for promoting healthy lifestyle habits, yet engagement in health-promoting occupations was described as conditioned behaviour.
Conclusions
CVD prevention programmes can benefit from incorporating engaging occupations to promote healthy lifestyle habits and literacy of health and occupations. However, contextual factors conditioning health and occupations should be considered when developing and implementing sustainable interventions.
Background
People’s occupations and lifestyle habits play an essential role in both the development and prevention of cardiovascular diseases (CVDs) including stroke [Citation1]. Occupations, which term refers to all the things people do or occupy themselves with, play an important role in fulfilling basic human needs to develop and experience wellbeing and to adapt to environmental conditions and change [Citation2]. Yet as a means of illness prevention or health promotion, occupations often appear to be disregarded. There is moreover a knowledge gap in how to promote and sustain healthy lifestyle habits and health-promoting occupations, with no ‘one path that fits all’. Several barriers to healthy lifestyle habits have been reported in persons with risk for CVDs or with established CVDs [Citation3,Citation4]. A recent qualitative study reports that older at-risk adults are often aware of risk factors for CVDs and dementia but are unsure about how to put prevention into practice and manage their risks [Citation5]. Putting prevention into practice by promoting engagement in health-promoting occupations and healthy lifestyle habits is, however, of great importance to prevent and manage many of our major public health diseases, including conditions such as stroke and transient ischaemic attack (TIA) [Citation1].
An important aspect of promoting healthy lifestyle habits is enabling individuals and populations to become more active and involved in occupations that fulfil their needs rather than being ‘add-on’ requirements [Citation2]. For example, exercise training and diet regimes could be add-on requirements aimed to fulfil health goals, but may not be ‘engaging occupations’ for the individual. Engaging occupations, described in previous literature as a special type of occupational experience, may hold promise to this end as they are experienced as highly meaningful, are infused with positive meaning and involve an intense sense of participation [Citation6,Citation7]. Engaging occupations are, moreover, often integrated in people’s everyday life (e.g. work, leisure activities or activities with the family or in the community) and are often carried out regularly [Citation8], making them the opposite of an add-on activity. Engaging occupations are further characterised as a just-right challenge, an optimal match between a person’s skills and their demands in a given context [Citation9], requiring more involvement and commitment than occupations that merely interest the individual [Citation10]. All of the above qualities are recognised as important in behaviour modification.
The use of engaging occupations in CVD prevention programmes is rarely reported and its contribution in promoting healthy lifestyle habits is missing in research. The aim of this study was to explore the impact of participating in engaging occupations in individuals at risk for CVDs by drawing on their experiences after participating in an occupation-focussed stroke prevention programme titled ‘Make my day’, described in depth elsewhere [Citation11]. The occupation-focussed prevention programme under study is based on the assumption that people’s health and wellbeing, as well as literacy of health and occupations, can be influenced by using engaging occupations and applying a holistic and multidisciplinary approach, and thus enabling their doing, being, becoming and belonging according to their natural health needs [Citation2]. Occupation, which is central to the programme, is used both as a goal and a means; for setting personalised lifestyle habit goals, and is measured as an outcome of the programme.
In previous programmes aimed to promote the habit of engagement in health-promoting and meaningful occupations, positive results were found for participation, functioning and wellbeing of well elderly persons [Citation12–15]. Similar programmes offered to persons with diabetes, persons at risk for CVD and persons with an already established CVD have resulted in positive changes in clinical outcome [Citation16,Citation17]. To the best of our knowledge, research focussing on interventions using engaging occupations in the context of targeting multiple modifiable risk factors for CVDs, such as poor dietary and alcohol habits, tobacco use, sedentary behaviour, physical inactivity, obesity, high blood pressure [Citation18] and psychosocial stress [Citation19], is, however, scarce. This topic is nevertheless important because risk factors are embedded in habits and everyday occupations, which is one of the reasons why it is so challenging to make a change. Risk factors are rarely isolated. Evidence supports the role of multiple healthy lifestyle habits in the prevention and management of CVDs [Citation20–22] and suggests that meaningful and purposeful everyday occupations combined with moderate physical exercise and a healthy diet are strongly related to wellbeing and longevity [Citation23,Citation24].
For prevention/health promotion strategies to operationalise the goals of health interventions (e.g. healthy lifestyle habits and positive health outcomes) to be more effective, there is, however, a need for an in-depth exploration of the knowledge underpinning health interventions [Citation25]. A better understanding of how engaging occupations promote healthy lifestyle habits, and the role they play in this process, may contribute to knowledge, and can potentially improve health interventions provided by multidisciplinary teams including occupational therapy professionals.
The aim of this study was to develop knowledge by exploring how engaging occupations can contribute to changes in lifestyle habits among persons at risk for stroke, who have previously participated in an occupation-focussed stroke prevention programme called ‘Make my day’ (hereafter referred to as ‘the prevention programme’).
Method
The study is nested in a descriptive multiple case study (in manuscript) that was carried out in 2018–2019 in Region Stockholm, Sweden. Participants were recruited using convenience sampling [Citation26]. Grounded theory [Citation27] was utilised in analysing the interview data. Interviews had a focus on experiences of engaging occupation and lifestyle habit change and were conducted over 12 months with individuals who had participated in the prevention programme, which involved using engaging occupations as a tool for promoting health and healthy activity patterns [Citation11]. This interview study was approved by the Regional Ethical Review Board in Stockholm, Sweden (Ref. No. 2015/834-31 and 2016/2203-32). Positioning of the researchers in data collection and analysis and reflections about ethics have been woven into the methods segment under each relevant heading.
Settings
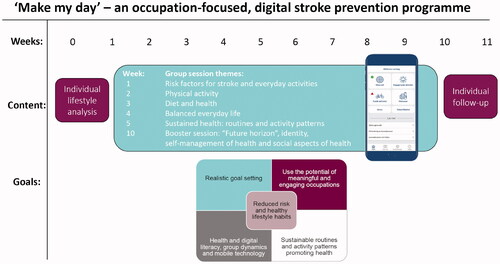
The study and prevention programme were performed in a health care setting in Region Stockholm, Sweden. The prevention programme (see for programme flowchart) [Citation11] consisted of several group sessions focussing on experiencing and learning about stroke risks, various preventative occupations and lifestyle habits. Participants attended sessions together with peers and allied health professionals (e.g. occupational therapist, physiotherapist and dietician). Health-promoting occupations were practised together in the group. The participants in the prevention programme had support from an mHealth application (app) (mobile phone health technology) produced in collaboration with Scientific Med Tech AB (http://www.scientificmed.com). The app was used to share information and exchange feedback and for self-monitoring of health by registering lifestyle habits, participation in engaging occupations and individual lifestyle habit goal achievements.
Participants
Persons at risk for stroke who had experienced and been diagnosed with a TIA were included in the study. A stroke risk screening survey [Citation28] was utilised to select potential participants. Seventeen individuals (four women) were identified by clinicians at two hospitals in Stockholm, and through a TIA register (n = 15). They were contacted by this article’s last author, also the project’s principle investigator (A.-H.P.) and a research assistant. Eight agreed to participate.
Inclusion criteria were: (a) age: 55–75 years; (b) presence of three or more risk factors for stroke (e.g. smoking, physical inactivity, poor diet, diabetes, high blood pressure, atrial fibrillation, high cholesterol, and family history of stroke), scored as high or moderate risk on the Stroke Risk Score Card; (c) access to either a smartphone or a wireless device and (d) motivation for lifestyle change. Exclusion criteria were: (a) lack of motivation to participate and/or make an effort for lifestyle change; (b) ongoing drug abuse and (c) non-Swedish language fluency, since the prevention programme and mHealth app prototype are available in Swedish only so far. One person was excluded because they did not have access to a wireless device. Altogether seven persons were eligible and recruited to the study, but one dropped out before baseline because of perceived lack of time.
Six individuals (four men and two women) participated in the study. The participants were between 59-70 years old. Besides having had a TIA 1–15 months prior to their participation in the prevention program, the participants had between 2 and 5 stroke risk factors scored as high in the Stroke Risk Score Card [Citation28]. One person was included based on scoring high on two risk factors as well as having had a previous TIA, which altogether was considered as a high risk. The participants had 9–15 years of education and a yearly income varying from <19,300 to >58,000 Euro. Three participants were living alone and three with a partner or a child.
The participants can in different ways be seen as vulnerable due to their health risks and lifestyle. The research team had experience and expertise in conducting research that includes people with risks for ill-health and long-term conditions. Participation in the study was based on written and oral informed consent and consent was reconfirmed at each interview. The participants had several opportunities to ask questions regarding their participation and receive support if needed. The names of study persons mentioned here are fictional to protect personal integrity in compliance with data protection regulations.
Data collection
Repeated in depth interviews [Citation27] with participants in the prevention programme were conducted by the first author (E.M.). The first interview was conducted after the prevention programme had ended and interviews two and three over a longer period of time (12 months). The individual interviews were semi-structured, with open-ended questions, and grounded in topics that participants had focussed on intensively during the prevention programme: ‘knowledge about stroke risk and health’, ‘health and lifestyle habits’, ‘engaging occupations’, ‘social aspects of health’, ‘changing lifestyle habits’ and ‘health apps and digital aids’ [Citation11]. During the interviews focus was on the participants’ statements about their experiences, reflected on and restated what the participant had said, to check for accuracy, and followed up on own interpretations that had derived from writing analytic notes (memos), at each follow-up interview. In total, 17 interviews were conducted over 12 months. Five of the participants were interviewed on three occasions, and one participant twice. The person interviewed twice was not able to participate in the last interview because of health issues (unrelated to stroke risk). The first and the last follow-up interview were conducted in person while the second follow-up was performed over the telephone. The interviews lasted between 10 and 68 min and were audio-taped.
In an attempt to position the data collector, E.M. (first author) is a Swedish licenced occupational therapist and lecturer in public health science with previous experience in conducting qualitative research. E.M. did not have a prior relationship with the participants from the prevention programme. Through E.M.’s theoretical foundation in occupational science, E.M. had a preunderstanding of engaging occupation, which was relevant in relation to data collection where experiences of a process of change and engaging occupation were explored.
Data analysis
After all interviews had been conducted, transcribed verbatim and checked for accuracy against the recorded files, they were analysed using a constant comparative method [Citation27]. Initially, the first interview transcript was read and coded line by line independently by both E.M. and the last author (A.-H.P.), after which, codes were compared and combined. The rest of the interview transcripts were thereafter explored, one at the time, by E.M. and descriptions and processes relating to engaging occupations and lifestyle habit changes were coded using ATLAS.ti [Citation29].
A constant moving back and forth between the whole text, interviews and smaller segments generated initial codes and helped to conceptualise preliminary ideas of categories. During the process of comparing parts and the whole of the text, reflective and analytic notes, or memos, were written by E.M. These memos further facilitated developing initial categories, by referring to them when testing the data with analytical questions. Examples of such questions were: How did the participant perceive and experience social aspects of the process of changing lifestyle habits? How did different factors interconnect in the process of changing lifestyle habits? What was hindering participating in engaging occupations and, therefore, what was hindering the progress in the participants health? Based on the memos, and following repeated analytic discussions about the findings and preconceptions among the co-authors, selective coding was conducted. In the analytic discussions, E.M. had a comprehensive understanding and context for the data because she was active throughout the data collection phase, whereas third author E.Å. had clinical experience with the target population with a professional background as a physician. Co-authors (A.H.P., E.A. and S.G.) had experiences in qualitative analysis and research within occupational therapy and occupational science. Codes that E.M. had grouped together, were discussed and compared with earlier interpretations and relationships between groups of codes were established and six sub-categories and three categories were formed.
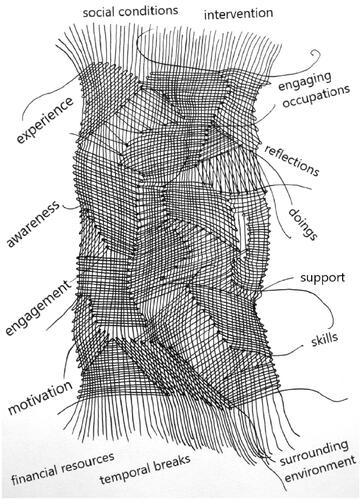
As a final analysis step to synthesise the findings creating the core category, the metaphor of ‘weaving a fabric’ was developed (see for an illustration of the core category). Both a ‘woven fabric’ and the occupation of ‘weaving’ were seen as a metaphor for exploring the data, mirroring the overall process of lifestyle habit change among the participants, with respect to the process of being able to create a larger pattern of habits. Quotes were translated independently from Swedish into English by E.M. and A.-H.P. and translations were compared for consistency with the aim to preserve the meaning in the original quotes.
Findings
The findings from this study show how behaviour change and healthy lifestyle habits can be promoted through participation in engaging occupations. Promoting healthy lifestyle habits and participation in engaging occupations is, however, a complex process imbued with several internal and contextual features. To illustrate this multifaceted, situated and very practical process of shaping and reshaping a pattern of lifestyle habits, the metaphor of weaving can be used to portray the participants’ experiences. This is captured in the study’s core category, ‘Weaving lifestyle habits’. Weaving involves parallel and interlaced threads (warps and wefts) consisting of different materials and shapes.
The threads affected both the process (weaving) of promoting healthy lifestyle habits and the participants’ overall lifestyle (fabric or pattern). Each finding in the woven fabric can be seen as an isolated thread with its own meaning and characteristics, and also as different sub-threads situated in a larger context with the possibility to both facilitate or hinder the process of weaving a healthy lifestyle for these persons. Many threads were intricately connected and dependent on each other and, considered together, had the potential to contribute to sustainability in the participants’ emerging lifestyle habit pattern.
The core category ‘Weaving lifestyle habits’ comprises three main categories and six sub-categories (see for compilation of the categories). Two of the main categories, Awareness of health, occupations and risk factors and Conditioned pathways to health, describe how important literacy of health and occupation, and individual and contextual features and conditions were perceived to be for making changes in lifestyle habits. The last main category, Changing ways of doing through experience, describes occupational experiences as even more central to shaping and sustaining a pattern of healthy lifestyle habits, where specifically experiencing engaging occupations, together with increasing literacy of health and occupations, is a strong facilitator for healthy lifestyle habits.
Table 1. Description of core category ‘Weaving Lifestyle Habits’, and underlying main and sub categories.
Awareness of health, occupations and risk factors
According to the participants, an important part of weaving lifestyle habits was becoming aware of what could affect one’s health and wellbeing, such as what individual risk factors and lifestyle habits looked like. Over time, becoming and continuously being aware of and understanding how different occupations could promote one’s wellbeing became a tool for changing lifestyle habits. However, the participants expressed that habits and engaging occupations were dependent on various social, physical or temporal factors that could both facilitate and hinder their engagement in healthy lifestyle habits.
Increasing awareness of health and how one lives life
The participants described that the prevention programme, with its occupation-focussed design, and self-monitoring through the mHealth app had contributed to their increased awareness of health. This was important in the process of making lifestyle-related changes because it affected health-related decisions. For example, Sam said, ‘Yes, I sort of learned when I came here … how to prevent stroke. What are the risks … So nowadays I think of that. Yes, I sort of avoid certain things.’ Increased awareness of lifestyle habits meant that the participants tried to engage less in for example sedentary habits, which are associated with increased stroke risk. The mHealth app that was offered as part of the intervention, as well as other health apps, contributed to awareness of habits on a day-to-day basis.
It [the app] has been very good … I got aware of what I was doing … it has helped me change my lifestyle habits … I have started running again … I eat more fruits and vegetables. (Mona)
Others described that the mHealth app made them aware of different health risks, and address issues such as physical inactivity, stress and imbalance in their daily life, or alcohol and tobacco consumption. All participants had become especially aware of the importance of dietary habits and the health impact of foods. Eating more vegetables and doing less snacking was a topic that came up in all the interviews. Mona repeatedly said: ‘Without candy – no stroke … that has become a mantra for me, sort of.’ The importance of physical activity was another topic that was discussed in all the interviews. For several participants, awareness and monitoring of the daily step count in the mHealth application stimulated increased engagement in other physical activities.
Becoming and being aware of engaging occupations and health
Becoming and being aware of risk factors and health also entailed literacy regarding engaging occupations. The participants unanimously described that engaging occupations evoked positive feelings, such as ‘it’s fun’, ‘it feels good’, ‘it makes me happy’, ‘they are very important’, ‘they’re an important factor for wellbeing’, ‘you think you shouldn’t be doing anything else’. In addition, engaging occupations seemed to have different characteristics. One participant explained:
It [an engaging occupation] is a physical activity – and not just physical. It is so much more. Engaging occupations could be social occupations, helping others, spending time with family or playing with [your] grandchildren, or they could be leisure activities, such as creative hobbies, photography, or specific work tasks you do on your own. (George)
A common feature of all these occupations was the intense focus the participants experienced while performing the occupations, which was described as health-promoting. John elaborated: ‘…they contribute to health in the sense that they are relaxing. One gets something to focus on, something totally different’. The relaxation provided by engaging occupations helped the participants cope with their otherwise busy lives.
Different aspects, however, affected the participants’ performance and participation in engaging occupations, such as ill health and fluctuating weather conditions when the seasons changed. During periods of ill health or in the winter, some of the participants engaged less in such occupations. Especially occupations such as doing physical exercise, walking or gardening became difficult. Engaging in fewer of such occupations in turn had a negative effect on their wellbeing and possibility to maintain healthy lifestyle habits. As Richard expressed it, ‘Sitting still is the worst thing one can do … during winter I do it anyway, because one does not have that energy … I don’t have anything like – “Oh, this will be fun to do!”’.
Over time the participants became aware that not having occupations that were engaging was a barrier in their process of changing lifestyle habits and it also made it harder for some of the participants to self-manage their stroke risk factors.
Conditioned pathways to health
Understanding pathways and motivators to health was another part in the participants’ process of ‘weaving lifestyle habits’. Internal factors for motivation and for acquiring healthy lifestyle habits were the participants’ vision of healthy ageing, fear of ill health and experience of rewards. Other people’s lifestyle habits and choices, social support, as well as an unstable economic situation and not having access to health-promoting physical environments were external factors impacting the participants’ motivation, lifestyle habits and participation in engaging occupations.
Abstract health visions and tangible rewards
Ageing healthy and being able to engage in occupations in the future with family and friends was described as a strong motivator for incorporating healthy lifestyle habits into one’s daily life. The participants had realised that their TIA had been a warning and it motivated them to make changes. Tina said that she wanted her life to look different in the future: ‘I don’t want to have a stroke … I want a life. I want to become 93 years old’. The fear of not being healthy in the future, and the potential risk of suffering another TIA or of having a stroke sometimes caused the participants stress and worry. However, from this feeling came also motivation to make lifestyle habit changes. Other motivating factors were the fears and wishes of relatives.
At the same time, the vision of future health and ill health was somewhat abstract and it was important to also have more tangible rewards. Feelings of wellbeing and happiness, provided through participation in engaging occupations, were experienced as very rewarding and as a motivator for making lifestyle habit changes. Mona described joy and the sense of meaning she experienced while at the sports arena, jumping up and down, clapping and cheering, while watching her grandchildren do sports. She said: I love watching my grandchildren do sports … when I do something and it feels good in my whole body, the heart turns red and the brain turns red … then it is engaging. (Mona).
The rewarding feeling of happiness Mona experienced through her engaging occupation provided motivation for further engagement in other social and physical occupations. The follow-ups in the prevention programme in themselves were portrayed as engaging and as providing tangible rewards that helped keep the motivation up. George said, ‘Really positive, to have evaluations after the prevention programme. … creates motivation to try to continue training until February’. John described how the regular follow-ups during and after the prevention programme provided feelings of social belonging, which was a concrete form of support and was a source of motivation: ‘So, what I think was supportive, is that this was a regular thing … to come and talk … and have the time to follow up …’. The participants felt a connection to the group who had all participated in the prevention programme. Even though they came from different backgrounds, they believed that they had common traits that had contributed to their ill health. Understanding these traits, for example stress of different kinds affecting lifestyle habits, was helpful in the process of breaking old, non-health-promoting habits. For instance, Sam, had experienced stress due to the stigma of retiring early because of chronic illness. However, he described that, partly because of his participation in the prevention programme, he had developed the courage to see himself as a worker again. By the last interview, Sam had returned to working life, which, he felt, impacted positively on his wellbeing: ‘… that I got this chance to be part of this group. It has meant a lot. Without it … I don’t think I would have changed as much as I did’.
The social support from the group and the group leaders seemed to be both rewarding and helpful. Tina said, ‘They [the participants and leaders], gave me energy to do this … to become a better person’. By reflecting alone and together, the participants also started to create new narratives regarding their future overall lifestyle. The mHealth app, giving results and feedback, seemed to be a useful tool in this process and provided instant rewards for several of the participants. However, some participants were not interested in technical devices and saw the social support and engaging in occupations together as a more central part in the process of weaving lifestyle habits.
Contextual conditions for occupations and lifestyle habits
Even though they realised that engaging occupations themselves can contribute to motivation and wellbeing, the participants expressed that conditions such as an accessible environment, social support and financial resources were necessary for them to perform engaging occupations. Lack of lighting in walking areas or large geographic distances were examples of barriers for participation in physical engaging occupations. John reflected on how staying at the summer cabin, a long distance from the grocery stores, automatically led to a more sedentary time:
I have a country house down in the south of Sweden, but it is mostly my wife who goes there … I’ve realized that when I’m there, from an activity perspective it’s a disaster. Whenever you need to go somewhere, you need to use the car. (John)
Such contextual conditions were acknowledged to cause stress and become barriers for healthy lifestyle habits. George said, ‘… the stress, it has mainly been about my in-laws … it wears out my health … one does not find the time to do things together as one would wish’. Social context played a major role in lifestyle habit formation and maintenance. Physical activity levels and what the participants ate depended a lot on who they were spending time with. John said, ‘When it comes to dietary intake, one is dependent on one’s partner as well’. Other people’s willingness or ability to join in occupations also had an impact on the participants’ physical exercise levels:
Otherwise, I probably wouldn’t have gone and trained as much as I do. We support each other … he [a friend of Richard’s] texts: ‘No training for me today.’ … Then it is pretty easy in the morning to just say, ‘Ah, what the heck [in other words, I won’t go to the training session either]!’ (Richard)
Regardless of the type of contextual factor acting as a barrier for the participants, these factors at times caused stress, which in turn took away the energy and motivation needed to shape the weaving of healthy lifestyle habits.
Changing ways of doing through experience
Discovering and rediscovering occupations and participating in different occupations and activities in the prevention programme and in everyday life was another important part of the process of weaving healthy lifestyle habits. It was important to actively tackle any disruptions to one’s occupations and here, support from others and strong engagement in the occupations was important. These two parts in the lifestyle habit weaving, together with the other threads, contributed to a more solid and sustainable woven fabric over time.
(Re)discover occupations and changing habits through doing
Besides becoming aware, during and after their participation in the prevention programme, of the situatedness of occupations and habits, the participants gradually started to make practical changes in their everyday life. Some became more physically active, changed their diet and learnt how to manage stress better. It seemed to have to do with their experience of engaging in meaningful and engaging occupations. Sam expressed that ‘Often, there is change when something happens. It doesn’t have to be something negative, it can be like this [the prevention programme]: positive’. By participating in occupations together with others, the participants had discovered new ways to promote their health through occupations, or had rediscovered forgotten, health-promoting occupations that they could engage in again. Mona described that the experience of being involved in the prevention programme, participating in occupations and at the same time reflecting about occupations and lifestyle habits had given her more than other forms of health education and support had given her previously:
I was aware of all the unhealthy stuff I was doing. But not as deeply as when I came here [to the prevention programme] … we got to try out different ways to eat diverse foods … Everyone is also different and takes in different things in different ways. This made it real for me… (Mona)
The participants described being inspired by the prevention programme; in this context, they talked about a specific session where they had participated in preparation of healthy snacks. They described that after this they ate healthier and prepared more home-cooked meals and snacks than before. They also did more preparation and meal planning on the weekends to manage healthy eating on weekdays. Sam described a number of things he had changed following the prevention programme:
What has changed because of the prevention programme is probably food, drinks and activities. I also drink very little soda … This has changed because of the prevention programme … I don’t know the last time when I ate smoked sausage. And I used to eat that a lot! Sausage on sandwiches, macaroni and sausage, yes, there always was a lot of sausage!! (Sam)
The participants described keeping vegetables easily accessible and visible at home and at work (e.g. on a kitchen table or counter) and trying not to buy and keep snacks at home, and in this way, to limit temptations: ‘Trying to put a bowl of cherry tomatoes where it’s visible and when it was strawberry season … I replaced those tomatoes …’ (John). After getting to try out different physical occupations in the prevention programme, the participants also incorporated transport walking or biking, rather than driving or taking public transport, more into their habits. They had discovered through experiencing and reflection that it could be quite engaging to look at buildings and one’s surroundings while taking a walk to the store or work, instead of taking the car or bus. Most participants had increased their amount of physical exercise, as well as reducing the number of cigarettes or alcoholic beverages per day. This was much related to their experiences from self-monitoring their habits on the mHealth and other health apps, which both visualised and reminded them of their lifestyle habits and engaging occupations.
Managing habits and disruptions with engagement and support
Weaving lifestyle habits, finally, involved shaping new habits, which were not always easy to mould or uphold. A new habit that had recently become part of everyday life but was not fully established as part of the person’s identity, was more easily disrupted than old habits that were linked to a participant’s identity. For example, a period of illness or vacation, which meant a disruption in the participant’s new habits and occupational pattern, could reintroduce old, unhealthy habits. Resuming health-promoting habits after such disruptions required a deep individual commitment, among other things to engaging anew in health-promoting occupations. Practically practising these occupations repeatedly with social support was another important aspect of resuming engagement in health-promoting habits and occupations after such disruptions. John said that, for him, support from the prevention programme was important to manage these disruptions:
The biggest challenge is to continue with the good habits. It is easy to lose focus and to do what you have always done. Therefore, it is very important and inspiring to have the evaluation at 6 and 12 months. A factor for motivation really. (John)
Long-established lifestyle habits that one had, for example a sedentary time in front of the television or smoking, were described as especially difficult to break or reduce. If a planned health-promoting occupation were not engaging enough, it was easier to, for example, stay on the couch, or continue smoking, according to the participants. It was, however, possible to break a habit and incorporate new occupations into one’s daily life over time, especially if one had support and if the new occupation was thoroughly engaging:
I’ve just started a new occupation. I’ve started dancing square dance. And it is engaging! Because I felt, ‘No, I’m not getting out walking … I have to do something indoors’, and then a girl came to me and said, ‘Um, why don’t you do square dance? Come with me tomorrow’. Because I used to dance before, a lot. So now I dance and I’m totally exhausted! I dance once a week. (Mona)
All participants described that in general they thought that health-promoting occupations, such as transport walking, biking, dancing or meal planning, had become more engaging since they had participated in the prevention programme and experienced and reflected together. These occupations were therefore perceived as easier to maintain, even if disruptions sometimes happened.
Discussion
This study has explored people’s experiences of how engaging occupations can contribute to changing lifestyle habits. The metaphor of weaving was utilised to illustrate the complexity of shaping lifestyle habits imbued with individual and contextual features and conditions. The aim of this metaphor is to show that the ability to change lifestyle habits depends on a combination of factors. In contrast to a woven fabric that has a beginning and an end, the weaving of this fabric can be seen as a continuous process without end. To shape and maintain a healthy lifestyle habit pattern, one needs skills, resources, favourable conditions and engagement, and many of the threads in the weaving process have to be changed or reinforced over time.
A strong facilitator for shaping healthy lifestyle habits was an active pursuit of participating in engaging occupations. The findings from the current study are in line with previous research where engaging occupations were described in terms of characteristics viewed by the participants as important to support healthy lifestyle habits, such as evoking positive feelings, wellbeing and satisfaction, being perceived as highly purposeful, and involving a sense of intense participation [Citation6–8]. Engaging occupations also brought a sense of reward and were described as a motivator for changing lifestyle habits. This type of experience of inherent interest or enjoyment (intrinsic motivation) has, in many behaviour change theories, been emphasised as important for sustainable lifestyle habit change [Citation30]. This finding is therefore a contribution to the field of behavioural and occupational science, expanding our knowledge of how healthy lifestyle habits can be developed and supported with engaging occupations.
In previous research it has been described that engaging occupations are often performed regularly [Citation6] and can promote balance between inner motivation and outer demands [Citation8]. In this study, continuity in performing engaging occupations was described as an important thread in weaving lifestyle habits; however, it was challenged by different contextual conditions, for example seasonal changes. During winter, physical and health-promoting engaging occupations, such as exercising outside, were hard to pursue, a fact which impacted negatively on the participants’ wellbeing, coping abilities, and maintenance of other healthy lifestyle habits.
The participants’ engagement in health promoting and engaging occupations was also dependent on different conditions and resources (e.g. social support, a health-promoting environment, finances, health care, knowledge, motivation). The situational complexity affecting individuals trying to change their unhealthy habits and maintain healthy lifestyle habits has been previously described [Citation3,Citation4]. Contextual features can contribute to shape people’s possibility to participate in engaging occupations [Citation31], and in this study ‘problematic situations’ (situations that stand in the way of habit change or that prevent engagement in occupations) were mainly due to a socio-cultural context, the surrounding environment and disruption. Social relationships, such as those developed during the prevention programme, primarily helped the participants to engage in, for example physical exercise.
Behaviours of friends and family were moreover important in enabling the participants to change and maintain healthy lifestyle habits. For instance, if the participants’ friends and family did not themselves make healthy food choices, the participants found it harder to pursue these behaviours on their own. This situatedness and the complexity of both changing or integrating occupations into everyday life are described in the newly published book by Twinley, Illuminating the Dark Side of Occupation [Citation32]. In congruence with the findings from this study, a participant from a study in Twinley’s book expressed the view held by several others, that even if they made a change in themselves, the occupational change or transition to new habits was not sustainable over time if the social contexts and environment were not changed as well. The specific case was about recovery from addiction, but the argument applies to many other lifestyle habits [Citation32]. It is therefore important to consider the social context and the larger socio-cultural and environmental conditions when developing and implementing health interventions [Citation33].
A dilemma regarding engaging occupations and their contribution to health or healthy lifestyle habits is that many people participate in occupations that are perceived as engaging and rewarding, but that these occupations can paradoxically be considered ‘non-health-promoting’ [Citation32,Citation34,Citation35]. Being sedentary in front of a television screen was described as a habit that the participants in the present study found hard to change. To break their sedentary habits, the participants expressed that they needed an equally purposeful and rewarding replacement occupation; otherwise, the new health-promoting occupation was easily opted out in favour of staying on the couch. This is an example of a situation where health knowledge or awareness of risk factors alone are not enough to practically change lifestyle habits, which also has been described in a qualitative review [Citation36].
Health literacy, that refers to both a person’s health knowledge and awareness and a person’s ability and process to understand and use information to promote, maintain or improve their health [Citation37], has for a long time been considered important for having and sustaining multiple healthy lifestyle habits [Citation38]. In drawing a parallel to health literacy, literacy of health and occupations has been described as a strong facilitator for shaping healthy lifestyle habits in the present study and this was promoted, as in several other occupation focussed programmes [Citation12–17], through occupational self-analysis in tandem with participating in and experiencing occupations. By actively engaging in and experiencing occupations in the prevention programme, and in between sessions, the participants gained literacy in how their occupations interrelate with health. Participants expressed that this made them more engaged in their overall health and even risk-reducing occupations became engaging.
Active engagement was also expressed to bring about a continuance of performing health-promoting occupations, putting prevention into practice, which recently has been described as challenging in a study of at-risk older adults [Citation5]. Active involvement in occupations has recently been highlighted as an important ingredient in health interventions, which can enable individuals to overcome obstacles for doing [Citation39]. In agreement with Fritz & Cutchin [Citation31], occupational therapists have an opportunity, in for example prevention programmes, to use their knowledge of occupation, and of habit and environmental modifications, to work with lifestyle habit change and increase people’s literacy of occupation, to enable them to take control and adapt to changing contexts and to promote participation in health-promoting and engaging occupations.
Methodological considerations/limitations
This qualitative study systematically explores experiences that can be built on to promote healthy lifestyle habits, which adds to previous quantitative research in the field [Citation20–22]. Conducting several interviews over the space of 12 months with each participant was a strength because it allowed for topics to be iteratively explored in subsequent interviews [Citation27]. The time between interviews provided space for reflection as well as the possibility to follow up for accuracy, which can be seen as positive for credibility [Citation40]. It can also be seen as a strength that the interviewer (E.M.) was not involved in delivering the prevention programme in that this minimised the risk that the participants would disclose only positive views.
A possible criticism of the design is that a positive change in lifestyle habits was expected because the aim was to explore how engaging occupations would contribute to change. However, the findings illustrate how conditioned both engaging occupations and healthy lifestyle habits were experienced to be, showing that the analysis process was open and not directed. Openness to the data was, moreover, enabled through a reflexive process that included writing memos, and discussing preconceptions while analysing the data among all co-authors who had different professional backgrounds (occupational therapists, a physician and a public health educator) and varying experience of the target group and of qualitative research, which can be seen as strengthening the rigour of the analysis and the trustworthiness of the findings.
The study described social, economic and environmental resources and conditions as important in facilitating but also as hindering lifestyle habit change. Therefore, one limitation of the study may be the homogeneity of the sample. Even though the group had a variety of socio-economic background and included both men and women, the sampling procedure and inclusion criteria did not include people from immigrant backgrounds, people who were not motivated to change, or people who did not have access to technical devices. Wider inclusion specifically targeting vulnerable groups is important for future studies to inform health interventions and to contribute to the United Nations (UN) Sustainable Development Goals stated in Agenda 2030, of promoting health and wellbeing for all.
Conclusion
Weaving lifestyle habits was perceived as a continuous and complex process where many parallel, interlacing and interdependent threads affected the participants’ engagement in occupations and lifestyle habit change. Increased literacy of health and occupation and experiencing engaging occupations were key facilitators, as was a supportive social and environmental context, which also included the prevention programme. Health interventions for persons at risk for CVDs or with established CVDs could benefit from using experiential and practical approaches to enhance literacy and participation in health-promoting and engaging occupations. It is, however, important to consider changing as well as hindering contexts in the development and implementation of health interventions, which could impact both the uptake and the maintenance of engaging occupations and healthy lifestyle habits.
Acknowledgements
We are grateful to the participants, for taking part in the prevention programme and interviews, as well as to: Jonas Beckman and Maria Mackaldener, students in the Occupational Therapy Bachelor’s programme, for transcribing the interviews; the health care professionals from Academic Primary Health Care Centre, Region Stockholm who participated in delivering the prevention programme: Reg. Occupational Therapist and research assistant Christina Ericsson, Reg. Physiotherapist Carmen Wärlinge, and consultant and Reg. Dietician Monica Pehrsson; and lastly, Stockholms Sjukhem, for providing suitable facilities and for collaboration in the project.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Goldstein LB, Bushnell CD, Adams RJ, Council on Peripheral Vascular Disease, and Interdisciplinary Council on Quality of Care and Outcomes Research, et al. Guidelines for the primary prevention of stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011;42(2):517–584.
- Wilcock A, Hocking C. An occupational perspective of health. 3rd ed. Thorofare: SLACK incorporated. 2015. p. 86, 421–423.
- Murray J, Craigs CL, Hill KM, et al. A systematic review of patient reported factors associated with uptake and completion of cardiovascular lifestyle behaviour change. BMC Cardiovasc Disord. 2012;12:120.
- Murray J, Fenton G, Honey S, et al. A qualitative synthesis of factors influencing maintenance of lifestyle behaviour change in individuals with high cardiovascular risk. BMC Cardiovasc Disord. 2013;13:48.
- Akenine U, Barbera M, Beishuizen CRL, et al. Attitudes of at risk older adults about prevention of cardiovascular disease and dementia using eHealth: a qualitative study in a European context. BMJ Open. 2020;10:e037050.
- Jonsson H. A new direction in the conceptualization and categorization of occupation. J Occup Sci. 2008;15(1):3–8.
- Jonsson H, Josephsson S, Kielhofner G. Narratives and experience in an occupational transition: a longitudinal study of the retirement process. Am J Occup Ther. 2001;55(4):424–432.
- Jonsson H. The first steps into the third age: the retirement process from a Swedish perspective. Occup Ther Int. 2011;18(1):32–38.
- Csikszenmihaily M. Flow: the psychology of optimal experience. New York: Harper & Row. 1990.
- Morris K, Cox DL. Developing a descriptive framework for ‘occupational engagement. J Occup Sci. 2017;24(2):152–164.
- Patomella A-H, Guidetti S, Mälstam E, et al. Primary prevention of stroke: randomised controlled pilot trial protocol on engaging everyday activities promoting health. BMJ Open. 2019;9(11):e031986.
- Clark F, Azen SP, Zemke R, et al. Occupational therapy for independent-living older adults. A randomized controlled trial. Jama. 1997;278(16):1321–1326.
- Barnes M, Bigari K, Culler T, et al. Healthy lifestyles through an adaptive living program: a pilot study. Occup Ther Int. 2008;15(4):269–283.
- Clark F, Jackson J, Carlson M, et al. Effectiveness of a lifestyle intervention in promoting the well-being of independently living older people: results of the Well Elderly 2 Randomised Controlled Trial. J Epidemiol Community Health. 2012;66(9):782–790.
- Levasseur M, Filiatrault J, Lariviere N, et al. Influence of Lifestyle Redesign® on health, social participation, leisure, and mobility of older French-Canadians. Am J Occup Ther. 2019;73(5):7305205030p1.
- Sw Ng S, Chan DY, Chan MK, et al. Long-term efficacy of occupational lifestyle redesign programme for stroke. Hong Kong J Occup Ther. 2013;23:46–53.
- Pyatak E, King M, Vigen CLP, et al. Addressing diabetes in primary care: hybrid effectiveness–implementation study of Lifestyle Redesign® occupational therapy. Am J Occup Ther. 2019;73(5):7305185020p1.
- O'Donnell MJ, Xavier D, Liu L, INTERSTROKE investigators, et al. Risk factors for ischaemic and intracerebral haemorrhagic stroke in 22 countries (the INTERSTROKE study): a case-control study. Lancet. 2010;376(9735):112–123.
- Booth J, Connelly L, Lawrence M, et al. Evidence of perceived psychosocial stress as a risk factor for stroke in adults: a meta-analysis. BMC Neurol. 2015;15(1):233.
- Towfighi A, Markovic D, Ovbiagele B. Impact of a healthy lifestyle on all-cause and cardiovascular mortality after stroke in the USA. J Neurol Neurosurg Psychiatry. 2012;83(2):146–151.
- Sisti LG, Dajko M, Campanella P, et al. The effect of multifactorial lifestyle interventions on cardiovascular risk factors: a systematic review and meta-analysis of trials conducted in the general population and high risk groups. Prev Med. 2018;109:82–97.
- Larsson SC, Åkesson A, Wolk A. Primary prevention of stroke by a healthy lifestyle in a high-risk group. Neurology. 2015;84(22):2224–2228.
- Poulain M, Herm A, Pes G. The blue zones: areas of exceptional longevity around the world. Populationyearbook. 2014;11:87–108.
- Steptoe A, Deaton A, Stone AA. Psychological wellbeing, health and ageing. Lancet. 2015;385(9968):640–648.
- Davis R, Campbell R, Hildon Z, et al. Theories of behaviour and behaviour change across the social and behavioural sciences: a scoping review. Health Psychol Rev. 2015;9(3):323–344.
- DePoy Gitlin Introduction to research: understanding and applying multiple strategies. 4th ed. St. Louis: Elsevier/Mosby; 2011.
- Charmaz K. Constructing grounded theory. 2nd ed. London, Thousand Oaks (CA): SAGE Publication Ltd.; 2014.
- Association NS. Stroke Risk Score Card 2018. Available from: https://www.stroke.org/stroke-risk-scorecard-2018/.
- ATLAS.ti. 2015. Scientific Software Development GmbH. Atlas.ti for Windows V8. 7.5.15 ed. Berlin: Germany.
- Michie S, Campell R, Brown J, et al. ABC of Behavior Change. 2nd ed. 2014. Great Britain: Silverback Publishing.
- Fritz H, Cutchin MP. The transactional perspective on occupation: a way to transcend the individual in health promotion interventions and research. J Occup Sci. 2017;24(4):446–457.
- Twinley R. Illuminating the dark side of occupation. international perspectives from occupational therapy and occupational science. 1st ed. Oxon: Routledge; 2021.
- O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954.
- Twinley R. The dark side of occupation: a concept for consideration. Aust Occup Ther J. 2013;60(4):301–303.
- Asaba E, Bergström A, Patomella A-H, et al. Engaging occupations among persons at risk for stroke: a health paradox. Scan J Occup Ther. 2020. DOI:https://doi.org/10.1080/11038128.2020.1829036.
- Ravenhill G, Gkanasouli L, Lawrence M. Experiences of transient ischemic attack diagnosis and secondary prevention: a qualitative review. Brit J Neurosci Nurs. 2019;15:14–25.
- Kickbusch I, Pelikan JM, Apfel F, et al. Health literacy: the solid facts. Copenhagen: World Health Organization (WHO); 2013.
- Aaby A, Friis K, Christensen B, et al. Health literacy is associated with health behaviour and self-reported health: a large population-based study in individuals with cardiovascular disease . Eur J Prev Cardiol. 2017;24(17):1880–1888.
- Larsson EA. Threshold occupational science concepts for lifestyle change: ‘doing’ wellness in a course for US college students. J Occup Sci. 2020;27:274–287.
- Grinyer T. The value of interview on multiple occasions or longitudinally. The SAGE Handbook of Interview Research: The Complexity of the Craft; 2012.