?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.Abstract
Background
Time management skills are essential to maintain occupations in everyday life. People with neurodevelopmental or mental disorders often experience persistent difficulties with managing time and organizing daily life, consequently, there is a need to establish interventions with sustainable results.
Aim
The aim was to perform a one-year post-intervention follow-up after the intervention Let’s Get Organized (LGO-S) for people with neurodevelopmental or mental disorders.
Methods
The study is a one-year follow-up of a single group pre-test–post-test design. Thirty-eight persons with difficulties in time management due to neurodevelopmental or mental disorders participated. Instruments to collect data were Assessment of Time Management Skills; Weekly Calendar Planning Activity and the Satisfaction with Daily Occupations instrument. Wilcoxons’s signed-rank test was used to compare data over time.
Results
There were no significant differences in the participants’ outcomes between post-intervention and one-year follow-up in time management skills and regulation of emotions, satisfaction with daily occupations, and global satisfaction. A significant improvement could be seen in the subscale organization and planning at the one-year follow-up compared to post-intervention.
Conclusions
Improvements in time management skills, organization, and planning, regulation of emotions, and satisfaction with daily occupations after the LGO-S can be maintained in the long term.
Introduction
In today’s modern society, time management skills are essential to maintain occupations in everyday life [Citation1,Citation2]. People with impaired executive functioning often experience difficulties in managing time and organizing daily life [Citation3,Citation4]. These difficulties commonly persist over the lifespan and involve challenges in balancing life at home and work [Citation4–6]. Since time management and organization skills have a central role in daily life, treating people with these impairments is a public health issue [Citation7]. To give efficient support to people with ineffective time management skills, there is a need to establish interventions with sustainable results. An occupational therapy group intervention that has been evaluated and has shown promising results is the Swedish version of Let’s Get Organized (LGO-S) [Citation8]; however, the long-term results of the LGO-S are yet to be explored.
Impaired executive functioning is common in people with neurodevelopmental disorders, such as attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), or mental disorders, such as affective disorders. Both daily time management, which refers to managing one’s time and adapting to time demands [Citation9], and organization and planning skills are dependent on executive functions that guide complex goal-directed behaviours [Citation10]. People with ADHD or ASD, for example, rate their time management skills significantly lower than people without cognitive impairment [Citation11]. Emotion dysregulation is a core symptom in adults with ADHD [Citation12,Citation13] and has been considered as a contributor to inefficient time management among persons with neurodevelopmental disorders [Citation14]. The severity of ADHD symptoms correlates with emotion dysregulation, leading to emotional lability that impairs daily life for many [Citation13]. Improvement in ADHD symptoms has also been shown to improve emotion dysregulation [Citation12] and thus improved executive functioning, i.e. time management skills, which may have an effect on emotion regulation. Despite the different aetiologies of these diagnoses, the impaired executive functions result in similar consequences, e.g. ineffective daily time management and organization and planning skills. These deficits often cause problems and distress in areas, such as allocating the right amount of time to activities, sequencing activities, prioritizing and finishing tasks, being organized at work and in social life, and managing routines and daily activities at home [Citation5,Citation15,Citation16]. These difficulties often persist for years – even becoming lifelong struggles for some – and common consequences are the risk of an impoverished lifestyle of affected job performance [Citation4,Citation5,Citation16,Citation17].
Various interventions are offered to improve time management- and organization and planning skills, one of which is metacognitive therapy, aimed at training these skills [Citation18,Citation19], but it has not yet been evaluated in the long term. Occupational therapy interventions to improve daily time management often involve the use of cognitive strategies to support individuals in learning or performance as well as cognitive assistive technology [Citation20,Citation21]. Providing cognitive assistive devices in combination with structured training has been shown to support time management, planning, and organization [Citation21–24]. However, to our knowledge, no studies are exploring the long-term results of interventions to improve time management skills.
LGO is a manual-based occupational therapy group intervention developed in the United States, which has been translated and adapted into the Swedish cultural context (LGO-S) [Citation8,Citation25]. The goal of LGO-S is to train and develop effective time management- and organizational skills in daily life; it has been adapted for persons with neurodevelopmental or mental disorders. The intervention includes 10 weekly sessions with a focus on daily time management. Another six optional sessions can be added and have a focus on organization and planning. An initial evaluation of the first ten sessions of LGO-S was carried out in an earlier pre-test–post-test study in Sweden showing that the participants had improved their time management skills and rated higher satisfaction with their daily occupations after the intervention [Citation8]. The result was maintained three months after the intervention and the findings were confirmed and illustrated in a qualitative study where the participants described emotional changes after the intervention, e.g. a positive impact on their sense of control, stress, and self-esteem [Citation26]. The sustainability of intervention results in the long term is crucial for the person with difficulties, and also an important factor to consider when implementing interventions in real-world contexts [Citation27,Citation28]. Sustainable interventions are likewise central from an economic perspective in a health care system with limited resources. Thus, there is a need to explore whether LGO-S provides sustainable results over time. Therefore, the aim was to study the one-year post-intervention follow-up on time management after the intervention Let’s Get Organized for people with neurodevelopmental or mental disorders.
Materials and methods
The study is a one-year follow-up of a single group pre-test–post-test design [Citation8]. Ethical approval was granted by the Regional Ethical Review Board in Uppsala, Sweden (2015/015).
Participants
All of the participants in the earlier study by Holmefur et al. [Citation8] were asked to participate in this follow-up. The original sample was recruited at five psychiatric and habilitation outpatient services in Sweden by nine occupational therapists working at these services and was based on the following inclusion criteria: (1) neurodevelopmental disorder, such as ASD or ADHD without intellectual disability, or being under assessment for the neurodevelopmental disorder, or confirmed diagnosis of a mental disorder, and (2) self-reported difficulties in time management skills to an extent that negatively affected functioning in daily life. The recruitment procedure was further described in Holmefur et al. [Citation8]. An additional inclusion criterion for the present study was the availability of pre- and post-intervention measures in the earlier study. Both this and the earlier study were registered at ClinicalTrials.gov (NCT03659279).
The LGO-S intervention
The intervention which was performed in the earlier study [Citation8] included the first ten sessions of LGO-S, with a focus on daily time management. Approximately 6–12 participants were included in each group, which met once a week during 10 weeks at the service where the participants were enrolled. Each LGO-S session lasts for 1.5 h and is prepared with a theme and exercises described in a manual [Citation25]. The themes focus on managing time and the consequences of impaired daily time management on everyday activities, circadian rhythm, and energy levels during the day. The sessions include structured training in the use of a calendar (electronic or paper) and building cognitive and emotional strategies in daily time management throughout the intervention. Every session starts with a reflection upon mood to connect emotional regulations with the ability to learn. The intervention uses trial and error learning strategies from cognitive rehabilitation [Citation29,Citation30] with the aim of encouraging the participants to share strategies in the group, neutralize the anxiety of making mistakes and try new strategies to support self-efficacy [Citation31]. The LGO-S was led by trained group leaders who were occupational therapists who had attended a two-day course on the key components of and theories behind LGO-S, on leading the sessions, and on collecting data.
Instruments
Three instruments were used to collect data about time management, executive functioning, and satisfaction with daily occupations. Self-reported time management skills were measured using the Swedish version of the Assessment of Time Management Skills questionnaire, (ATMS-S). ATMS-S is validated in Swedish and includes three subscales measuring the following constructs: time management skills (11 items), organization and planning (11 items), and regulation of emotions (5 items) [Citation32]. There are four response alternatives, and each item is scored 1 (never) to 4 (always). The ATMS-S scores for each subscale were transformed to the Rasch-based ATMS units at an interval level range of 0–100 which were used to analyze and report subscale results. Higher scores mean better time management skills [Citation32]. The ATMS-S displays moderate to excellent test-retest reliability overall (ICC = 0.79–0.90 in subscales) [Citation33].
To measure executive functioning in the activity of time planning, the Swedish version of Weekly Calendar Planning Activity (WCPA-SE) was used. The WCPA-SE measures a person’s ability to solve cognitive planning tasks involving organization, planning, and the person’s use of strategies [Citation34,Citation35]. The test includes 17 appointments on a list to be organized on a blank calendar sheet. The test is timed, and there are also five rules to be followed. The WCPA-SE results used in his study include the total time to complete the task, the number of correctly entered appointments, the number of rules followed, and the number of strategies used. The number of strategies includes both observed and self-reported strategies, the latter reported in a short interview after the assessment. Another variable in the WCPA-SE results is the efficiency score, which is the ability to perform the test in a short time with high accuracy of correct appointments [Citation36]. Efficiency score was calculated for participants who entered at least seven accurate appointments [Citation36]. Previous studies of WCPA indicate proper psychometric characteristics of discriminant validity [Citation37] and interrater reliability (ICC = 0.99) [Citation38]. Test-retest of WCPA-SE shows sufficient reliability, in particular between test occasions 2 and 3 (ICC = 0.65–0.91) [Citation39].
Satisfaction with daily occupations was measured with the Satisfaction with Daily Occupations instrument (SDO-13) [Citation40]. The SDO-13 is a structured interview including 13 items about work/studies, leisure, home maintenance, and self-care occupations. The person answers whether the activity was performed during the last two months (yes or no) and indicates the level of satisfaction with each activity using a satisfaction scale from 1 (extremely dissatisfied) to 7 (extremely satisfied). As a separate measure, the person also rates his/her global satisfaction with daily occupations from 1 (best possible satisfaction) to 5 (least possible satisfaction). SDO-13 has been shown to have satisfactory internal consistency reliability among persons with mental illness [Citation40] and among clients in primary care [Citation41], as well as good test-retest reliability for persons with mental disorders with rs = 0.84 for the Satisfaction score and rs = 0.92 for Activity level [Citation42].
A study-specific questionnaire was used before the intervention to collect demographic data including age, sex, family status, living arrangements, along with information on education and work.
Data collection
Data for this study were collected 12 months after the completed LGO-S. The participants did not attend any intervention including time management during the period after intervention and until the 12-month follow-up.
Analysis
Collected data were compared to data from the earlier study [Citation8]. In this study, the data from the pre- and post-intervention were re-analyzed for the specific sample that took part in the 12-month follow-up.
The demographics of the participants were reported with descriptive statistics. To explore whether there were any differences in demographic data between the participants who participated at the 12-month follow-up and those who only participated in the earlier study (called non-participants), t-test (for age) or the Pearson chi-square test were used. ATMS-S results for participants and non-participants were compared using the Mann-Whitney U test.
The sample size was small and the Shapiro-Wilks test of normality showed that data were not normally distributed in all instruments and therefore non-parametric statistics were used to analyze the data. The Wilcoxon signed-rank test was used to compare the pre- and post-intervention, and 12-month follow-up data. IBM SPSS Statistics (Version 26.0. Armonk, NY: IBM Corp) was used to perform the statistical analyses. The level of significance was set at <0.05.
Results
In the 12-month follow-up, 38 of the 55 participants in the earlier study [Citation8] were assessed. Accordingly, 17 individuals did not participate in the 12-month follow-up. When comparing the participants to the non-participants, no significant differences were observed in terms of age, sex, or having children. Significantly fewer of the non-participants compared to the participants were employed (p = 0.036). There was no significant difference in time management skills or satisfaction with daily occupations between the participants and the non-participants either before or after the intervention, or in improvement from before to after intervention.
The mean age of the participants in the 12-month follow-up was 36 years, and most of them were women (n = 26). Nearly half of the participants stated that they were currently employed or studying (47%) and 16 of them had children (). The participants had on average attended 8.4 of the ten intervention sessions included (median = 9, range = 5–10). The majority of the participants had ADHD or ASD (n = 26), often in combination with a mental disorder, such as affective disorder or anxiety. Four participants had mental disorders solely and six were under investigation for a neurodevelopmental disorder.
Table 1. Demographic and diagnostic information of the participants.
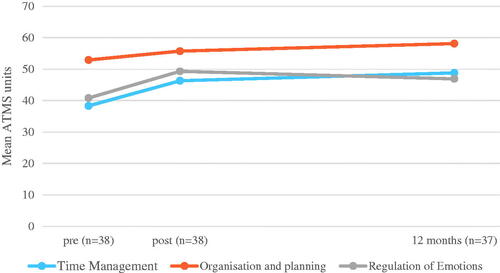
The participants maintained their results both in time management skills and in the regulation of emotions 12 months after the intervention. These aspects improved significantly from pre- to post-intervention ( and ). Further, a significant improvement in organization and planning was found 12 months after the intervention (p = 0.009) compared to post-intervention.
Table 2. Results and comparisons in time management, organization and planning, and regulation of emotions.
The participants’ executive functioning as measured by the number of correctly entered appointments with WCPA-SE which had shown significant improvement in the earlier study (p < 0.001) [Citation8] was maintained at the 12-month follow-up. The results of total time and the number of strategies used did not show any significant change either post-intervention or at the 12-month follow-up. The number of rules followed had improved post-intervention but was not sustained at the 12-month follow-up (). The participants performed the WCPA-SE more efficiently after the intervention as the efficiency score improved post-intervention (p = 0.001), but this improvement was not present at the 12-month follow-up ().
Table 3. Results and comparisons of executive functions.
The participants’ satisfaction with their performed occupations, which had increased significantly post-intervention (p = 0.005), was maintained at the 12-month follow-up. Similarly, the statistically significant improvement (p = 0.002) in the global satisfaction with daily occupations from pre-intervention to post-intervention (m = 3.2–2.8) was sustained at the 12-month follow-up (m = 2.6) (lower scores indicate greater satisfaction) (). The number of activities increased after intervention but had dropped at the 12-month follow-up ().
Table 4. Results and comparisons in satisfaction of daily occupations.
Discussion
The results demonstrate that the participants’ improved time management skills after the LGO-S intervention [Citation8] were still present at 12 months, even though they obtained no further time management intervention. The results also show that the participants maintained their improved satisfaction with daily occupations and global satisfaction 12 months after attending the intervention. Thus, this study indicates that the improvements in time management- and organization and planning skills, emotional regulation, and satisfaction with daily occupations gained during the LGO-S intervention were maintained over time.
The results of the current study expand the promising results presented by Holmefur et al. [Citation8] regarding improved time management skills after LGO-S. When data over time are available (), it is possible to see how intervention with LGO-S part 1, focussing mainly on time management and regulation of emotions, coincides with the outcome. The maintained a higher level of time management skills after intervention could have been due to the use of a calendar, which is one of the main aims of the intervention and is emphasized and supported at each session during the 10-week intervention. It should be noted that this significant difference is maintained since self-rated time management skills could be subject to a response shift in the participants whereby they adapt their internal standards when experiencing changes in their health status, which may result in an underestimation of the true improvement [Citation43].
Interestingly, skills in organization and planning, which improved moderately during the intervention, showed even further improvements 12 months after intervention although the participants had no interventions targeting this topic during that period. This improvement could be because participants had integrated a new habit, namely using the calendar in their everyday life, which might have improved organization and planning on an ongoing basis. Additionally, to organize daily life it is necessary to be able to estimate activity duration, an essential part of time management. The result emphasizes how time management and organization and planning are intertwined, and that the improvement might be because when time management skills are maintained at a higher level, it is possible for organization and planning to develop. The results of WCPA-SE also showed that the participants sustained their increased ability to enter appointments in the calendar correctly, which indicates a sustained ability for time planning between post-intervention and the 12-month follow-up. However, they did not manage to do this as fast as post-intervention, which explains the decreased efficiency score at the 12-month follow-up. A possible explanation for the maintained improvement might also be that the participants were able to integrate the cognitive strategies learned into daily life, indicating that the changes remained stable beyond the end of the treatment, something which has been observed in other studies [Citation44]. Using the cognitive strategies effectively while tolerating potential mistakes increases the person’s confidence in approaching a task [Citation20]. In a qualitative study including participants who had undergone the LGO-S, the participants claimed it was hard to maintain routines and use strategies after the intervention, yet their increased confidence made them continue with this struggle [Citation26]. This corresponds with our results, indicating that the participants continued to use the strategies, which is one of the aims of the LGO-S intervention.
Twelve months after participating in LGO-S, the participants maintained an increased satisfaction with daily activities and, what is more, maintained their improved global satisfaction. Even if the results indicate that participants did not engage in a greater number of activities, they seemed to perform their activities in a way they found more satisfying or chose to participate in other more satisfying activities, which could be reflected in the improved and subsequently maintained satisfaction. Subjective perceptions of occupation are an important outcome for this group as it is closely associated with outcomes, such as quality of life and self-rated health [Citation45]. The abovementioned recent qualitative study, where LGO-S participants were interviewed [Citation26], illustrates that using the calendar and other cognitive and emotional strategies after attending LGO-S had a positive impact on satisfaction with daily life. The participants in that study described a feeling of calm and security when using the calendar and other strategies, and that the control gained reduced negative stress [Citation26]. In addition, our study shows that the participants maintained their improved results in emotional regulations 12 months after the intervention. This result is in line with a recent study among female adults with ADHD, which shows that establishing routines and enhancing time management, for example learning to estimate activity length accurately, was a key component that was considered to improve the participants’ ratings of performance and satisfaction [Citation24]. It is very important for occupational therapy interventions to target this aspect as it has been proved that emotional dysregulation is a distinct symptom in adult ADHD in daily life and a major cause of impairment [Citation12,Citation46]. One such occupational therapy intervention is the LGO addressing time management skills and our study suggests that its’ benefits are also sustainable over time.
Methodological considerations
The high proportion of non-participants (31%) in the long-term follow-up might have affected the result. It could be suspected that only the participants who were satisfied with the LGO intervention chose to participate in the follow-up, which might have boosted the results. As there are no significant differences in time management skills post-intervention between the participants and non-participants at the 12-month follow-up, there is reason to believe that the factors for not participating in the 12-month follow-up study were not primarily related to the intervention, time management skills, or the result of the intervention. Because no systematic factors related to the intervention that could have influenced the participation in the 12-month follow-up study were found, there is a low risk that the results are overrated due to such factors. Of course, it is still possible that the participants in the 12-month follow-up were those who succeeded the best over time due to other possible explanations or unknown factors that might separate the groups. The results show that a larger proportion of the participants at the 12-month follow-up were working, compared to the non-participants, an outcome that is similar to that of another study evaluating intervention with assistive technology [Citation23]. We speculate that this is because a job provides structure and helps the person to maintain daily routines, which are generally easily lost and need to be constantly regained by persons with neurodevelopmental and mental disorders [Citation26]. Having a fixed structure of working hours may make it easier to plan for participation despite the presence of a disorder [Citation47], which could have influenced the ability to participate in the 12-month follow-up. In studies including people with ADHD, ASD, or mental disorders, drop-outs are common and might be due to their time management difficulties or other health issues, which is also shown in another recent long-term follow-up study including people with ADHD where 41% failed to participate at follow-up [Citation48]. Nevertheless, the results need to be interpreted carefully, particularly because of the weak design without a control group and would benefit from confirmation in other studies.
Conclusions
This study has shown that the LGO-S intervention can lead to improved and maintained time management-, organization and planning skills, regulation of emotions, and satisfaction with daily occupations in the long term. The results also indicate that organization and planning develop further during the first year following the intervention. It is yet to be seen whether intervention with LGO-S part 2 will increase organization and planning skills in a similar way. Future research should be conducted to establish the effect of the LGO-S in a randomized trial. The findings of this study are of importance for occupational therapists working in the field to be able to offer valid and sustainable interventions for people with neurodevelopmental or mental disorders.
Acknowledgements
The authors would like to thank all the participants who took part in this study. We also thank the occupational therapists who contributed to the data collection.
Disclosure statement
The authors report no conflict of interest. The authors alone are responsible for the content and writing of the paper.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Thomack B. Time management for today's workplace demands. Workplace Health Saf. 2012;60(5):201–203.
- Claessens BJC, van Eerde W, Rutte CG, et al. A review of the time management literature. Personnel Rev. 2007;36(2):255–276.
- Valko L, Schneider G, Doehnert M, et al. Time processing in children and adults with ADHD. J Neural Transm. 2010;117(10):1213–1228.
- Eklund M, Leufstadius C, Bejerholm U. Time use among people with psychiatric disabilities: implications for practice. Psychiatr Rehabil J. 2009;32(3):177–191.
- Stern A, Maeir A. Validating the measurement of executive functions in an occupational context for adults with attention deficit hyperactivity disorder. Am J Occup Ther. 2014;68(6):719–728.
- Franke B, Michelini G, Asherson P, et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. 2018;28(10):1059–1088.
- Chang Z, Ghirardi L, Quinn PD, et al. Risks and benefits of attention-deficit/hyperactivity disorder medication on behavioral and neuropsychiatric outcomes: a qualitative review of pharmacoepidemiology studies using linked prescription databases. Biol Psychiatry. 2019;86(5):335–343.
- Holmefur M, Lidström-Holmqvist K, Roshanay AH, et al. Pilot study of Let's Get Organized: a group intervention for improving time management. Am J Occup Ther. 2019;73(5):7305205020p1–7305205020p10.
- Sköld A, Janeslätt GK. Self-rating of daily time management in children: psychometric properties of the Time-S. Scand J Occup Ther. 2017;24(3):178–186.
- World Health O. International classification of functioning, disability and health (ICF). Geneva: World Health Organization; 2001.
- Hayat Roshanai A, Janeslätt G, White S, et al. Time management skills in relation to general self-efficacy and parental sense of competence in individuals with and without cognitive disabilities. Cogent Psychol. 2019;6(1):1–16.
- Shaw P, Stringaris A, Nigg J, et al. Emotion dysregulation in attention deficit hyperactivity disorder. Am J Psychiatry. 2014;171(3):276–293.
- Beheshti A, Chavanon M-L, Christiansen H. Emotion dysregulation in adults with attention deficit hyperactivity disorder: a meta-analysis. BMC Psychiatry. 2020;20(1):120–120.
- Maedgen JW, Carlson CL. Social functioning and emotional regulation in the attention deficit hyperactivity disorder subtypes. J Clin Child Psychol. 2000;29(1):30–42.
- Brown TE, Flood E, Sarocco P, et al. Persisting psychosocial impairments in adults being treated with medication for attention deficit/hyperactivity disorder. Psychopharmacol Bull. 2017;47(4):8–17.
- Levy A, Perry A. Outcomes in adolescents and adults with autism: a review of the literature. Res Autism Spectr Disord. 2011;5(4):1271–1282.
- Adler DA, McLaughlin TJ, Rogers WH, et al. Job performance deficits due to depression. Am J Psychiatry. 2006;163(9):1569–1576.
- Solanto MV, Marks DJ, Wasserstein J, et al. Efficacy of meta-cognitive therapy for adult ADHD. Am J Psychiatry. 2010;167(8):958–968.
- Lopez PL, Torrente FM, Ciapponi A, et al. Cognitive-behavioural interventions for attention deficit hyperactivity disorder (ADHD) in adults. Cochrane Database Syst Rev. 2018;3(3):CD010840.
- Toglia JP, Rodger SA, Polatajko HJ. Anatomy of cognitive strategies: a therapist's primer for enabling occupational performance. Can J Occup Ther. 2012;79(4):225–236.
- Gillespie A, Best C, O'Neill B. Cognitive function and assistive technology for cognition: a systematic review. J Int Neuropsychol Soc. 2012;18(1):1–19.
- Janeslatt G, Lindstedt H, Adolfsson P. Daily time management and influence of environmental factors on use of electronic planning devices in adults with mental disability. Disabil Rehabil Assist Technol. 2015;10(5):371–377.
- Lindstedt H, Umb-Carlsson Õ. Cognitive assistive technology and professional support in everyday life for adults with ADHD. Disabil Rehabil Assist Technol. 2013;8(5):402–408.
- Gutman SA, Balasubramanian S, Herzog M, et al. Effectiveness of a tailored intervention for women with attention deficit hyperactivity disorder (ADHD) and ADHD symptoms: a randomized controlled study. Am J Occup Ther. 2019;74(1):7401205010p1.
- White SM. Ha Koll – gruppintervention för att hantera tid och organisera aktiviteter (LGO-S). In: Janeslätt G, Donlau M, Lidström Holmqvist K, editors. Svensk översättning, version 2.0. Nacka: Sveriges Arbetsterapeuter; 2019.
- Holmqvist K, Tollén A, Holmefur M. Toward control over time: participant experience of attending the group intervention Let’s Get Organized. Am J Occup Ther. 2020;74(4_Supplement_1):7411515440p1. Forthcoming.
- O'Cathain A, Croot L, Duncan E, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9(8):e029954.
- Craig P, Dieppe P, Macintyre S, et al. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337(7676):979–983.
- White SM, Riley A, Flom P. Assessment of time management skills (ATMS): a practice-based outcome questionnaire. Occup Ther Mental Health. 2013;29(3):215–231.
- White S. Let's Get Organized: an intervention for persons with co-occurring disorders. Psychiatr Serv. 2007;58(5):713–2730.
- Bandura A. Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev. 1977;84(2):191–215.
- Janeslatt GK, Holmqvist KL, White S, et al. Assessment of time management skills: psychometric properties of the Swedish version. Scand J Occup Ther. 2018;25(3):153–161.
- Thorsson M, Holmefur M, Lidström-Holmqvist K. Test-retest reliability of the Swedish version of the Assessment of Time Management Skills (ATMS-S) – in adults with neurodevelopmental disorders (in manuscript).
- Toglia J. Weekly calendar planning activity (WCPA): a performance test of executive function. Bethesda, MD: AOTA Press, The American Occupational Therapy Association Inc.; 2015.
- Toglia J. Veckoplanering i kalender – aktivitetsbaserat test av exekutiva funktioner (WCPA-SE). [Swedish manual: weekly calendar planning activity (WCPA): a performance test of executive function]. Stockholm: Swedish Association of Occupational Therapists; 2017.
- Toglia J, Lahav O, Ari EB, et al. Adult age and cultural differences in performance on the weekly calendar planning activity (WCPA). Am J Occup Ther. 2017;71(5):7105270010p1.
- Toglia J, Berg C. Performance-based measure of executive function: comparison of community and at-risk youth. Am J Occup Ther. 2013;67(5):515–523.
- Weiner NW, Toglia J, Berg C. Weekly calendar planning activity (WCPA): a performance-based assessment of executive function piloted with at-risk adolescents. Am J Occup Ther. 2012;66(6):699–708.
- Holmqvist KL, Holmefur M, Arvidsson P. Test–retest reliability of the Swedish version of the Weekly Calendar Planning Activity – a performance-based test of executive functioning. Disabil Rehabil. 2020;42(18):2647–2652.
- Eklund M, Backstrom M, Eakman AM. Psychometric properties and factor structure of the 13-item satisfaction with daily occupations scale when used with people with mental health problems. Health Qual Life Outcomes. 2014;12(1):191.
- Wästberg BA, Persson EB, Eklund M. The Satisfaction with Daily Occupations (SDO-13) Scale: psychometric properties among clients in primary care in Sweden. Occup Ther Health Care. 2016;30(1):29–41.
- Eklund M, Gunnarsson AB. Satisfaction with daily occupations: construct validity and test–retest reliability of a screening tool for people with mental health disorders. Aust Occup Ther J. 2007;54(1):59–65.
- Schwartz CE, Bode R, Repucci N, et al. The clinical significance of adaptation to changing health: a meta-analysis of response shift. Qual Life Res. 2006;15(9):1533–1550.
- López-Pinar C, Martínez-Sanchís S, Carbonell-Vayá E, et al. Long-term efficacy of psychosocial treatments for adults with attention-deficit/hyperactivity disorder: a meta-analytic review. Front Psychol. 2018;9: 1-16..
- Eklund M, Leufstadius C. Relationships between occupational factors and health and well-being in individuals with persistent mental illness living in the community. Can J Occup Ther. 2007;74(4):303–313.
- Hirsch O, Chavanon M, Riechmann E, et al. Emotional dysregulation is a primary symptom in adult attention-deficit/hyperactivity disorder (ADHD). J Affect Disord. 2018;232:41–47.
- Liljeholm U, Bejerholm U. Work identity development in young adults with mental health problems. Scand J Occup Ther. 2020;27(6):431–440.
- Lam AP, Matthies S, Graf E, et al. Long-term effects of multimodal treatment on adult attention-deficit/hyperactivity disorder symptoms: follow-up analysis of the COMPAS trial. JAMA Netw Open. 2019;2(5):e194980.