Abstract
Background
Although housing accessibility is associated with important health outcomes in other populations, few studies have addressed this in a Parkinson’s disease population.
Aim
To determine the most severe environmental barriers in terms of housing accessibility problems and how these evolved over 3 years among people with Parkinson’s disease.
Material and Methods
138 participants were included (men = 67%; mean age = 68 years). The most severe environmental barrier were identified by the Housing Enabler instrument and ranked in descending order. The paired t-test was used to analyse changes in accessibility problems over time.
Results
The top 10 barriers remained largely unchanged over 3 years, but with notable changes in order and magnitude. ‘No grab bar in hygiene area’ and ‘Stairs only route’ were top-ranked in generating accessibility problems at baseline but decreased significantly (p = 0.041; p = 0.002) at follow-up. ‘Difficulties to reach refuse bin’ was top-ranked at follow-up, with a significant increase (p < 0.001) of related accessibility problems.
Conclusions and Significance
The new knowledge about how accessibility problems evolve over time could be used by occupational therapists to recommend more effective housing adaptations taking the progressive nature of Parkinson’s disease into account. On societal level, the results could be used to address accessibility problems systematically.
Introduction
For people with Parkinson’s disease, daily activities can be affected as early as at the first diagnosis [Citation1]. The disease is associated with characteristic motor symptoms (e.g. bradykinesia, tremor, rigidity, postural instability) as well as non-motor symptoms (e.g. depression, cognitive impairments, sleep disturbance) and the symptoms become more serious over time [Citation2]. In the general population, most people remain living in ordinary housing regardless of health decline and disability [Citation3]. However, while people with Parkinson’s disease have a strong desire to age-in-place [Citation4], they move to residential care at a younger age than others [Citation5].
Accessible housing supports independence and is associated with positive health outcomes in the general older population [Citation6–7]. To support ageing-in-place for populations with specific profiles of functional limitations, more knowledge is warranted regarding environmental barriers and the manifestation of accessibility problems for populations facing challenges in their housing situation. Moreover, several review articles have highlighted that few studies have addressed housing accessibility, physical environmental barriers and housing design features among people with Parkinson’s disease [Citation8–10]. Consequently, as Parkinson’s disease is one of the most common chronical, progressive neurological diseases [Citation11] and people with this disease are common in occupational therapy practice, more research is warranted to shed light on the housing situation for this vulnerable segment of the population. Not the least as people with Parkinson’s disease commonly have functional limitation such as gait and balance problems that progress over time, including dependence of mobility devices [Citation12].
Conceptual and theoretical underpinnings
The International Classification of Functioning and Disability (ICF) [Citation13] classifies Parkinson’s disease as a health condition that affects body functions and structures, activities and participation. Furthermore, houses are regarded as environmental factors, which may act as barriers or facilitators. Based on the ICF, the World Report on Disability [Citation14] stated that the physical environment affects disability. Moreover, accessible design in built environments, including housing, are addressed as examples of facilitators that could enable activity and participation. In the Ecological Theory of Ageing (ETA) [Citation15], the person and environment relationship has been described in terms of person-environment (P-E) fit. That is, the degree to which a balance between the person with his/her functional capacity (P) and the demands of the environment (E) is achieved. The P-E fit has been described as one aspect of accessibility [Citation16]. Turning to occupational therapy, numerous theories stress the transactional relationship between the person, the environment and occupation [Citation17]. The Person Environment Occupational Model (PEO) includes all three components and describes their transaction as the main outcome, in terms of occupational performance. The PEO assumes that a closer overlap or fit of the three components generates a more harmonious transaction, implying a more optimal occupational performance. Referring to the ETA, the PEO highlights the P-E relation as an interdependent transaction between the person and the environment [Citation17]. In occupational therapy, there is a general focus on the ‘doing’ as represented by occupational performance [Citation17,Citation18], sometimes with insufficient attention to the role of the underlying components. In addition, and of specific relevance for the present study, to enable occupation not only on the client level occupational therapists should make use of their specific competence on PEO transactions to promote health on the societal level as well [Citation17]. Such approaches are still underdeveloped in current occupational therapy practice and research.
Illustrating the P-E fit, the combination of a progressively declining functional capacity and the prevalence of physical environmental barriers in the housing environment generates accessibility problems [Citation19–20], which is likely to occur for people with Parkinson’s disease given the nature of the disease. Operationalizing accessibility in line with the notion of the P-E fit, the E component is defined as objectively observed physical barriers, based on legislation and national standards for housing design [Citation16]. Furthermore, the E component is juxtaposed with the functional capacity of the individual (the P component), in this case Parkinson’s disease symptoms. In order to promote accessible housing, it is important that occupational therapy practice and research examine and understand key environmental barriers for different sub-groups of the population. Such knowledge is necessary to nurture efficient individual interventions and societal actions, not the least as housing accessibility problems seem to be associated with decreased life satisfaction for older people in general [Citation20].
Occupational therapy context
Occupational therapy improves self-perceived performance in meaningful activities for people with Parkinson’s disease [Citation21] and is often delivered through multi-faceted interventions [Citation21–23]. Due to the progressive nature of the disease [Citation11], occupational therapy interventions are often needed over many years. Environmental barriers in the home setting are commonly addressed in rehabilitation, but the effect is often difficult to discern as multiple interventions are delivered simultaneously in complex interventions. The limited Parkinson’s disease research of that kind typically addresses usability, that is, subjective experiences of the environment often in relation to performing an activity, rather than objective housing accessibility problems [Citation8,Citation23,Citation24]. While this is in line with client-centred occupational therapy [Citation24] as well as the legislation governing housing adaptation grants in Sweden [Citation25], knowledge about the most common environmental barriers and their contribution to housing accessibility is insufficient. For example without systematic assessment of the occurrence of environmental barriers, occupational therapists do not have sufficient information to plan foresighted sustainable housing adaptations. Occupational therapy research and practice have the potential to contribute with knowledge on the aggregated level, which goes beyond what could be gained with solely the subjective perspectives of individual clients.
Turning to the societal level, about 50,000–60,000 housing adaptations are approved each year at the cost of almost SEK 1 billion in Sweden [Citation26]. Knowledge about environmental barriers and their contribution to accessibility problems has the potential to inform developments towards housing provision that meet the needs of people living and ageing with progressive diseases such as Parkinson’s disease. The PEO model stresses the need for occupational therapists to address the societal level [Citation17], and research targeting the ageing population has shown that knowledge about specific P-E interactions produces new information regarding housing accessibility on an aggregated level [Citation19,Citation27]. Relating this to Parkinson’s disease, recent studies have found a substantial knowledge gap regarding housing matters and housing design among people with Parkinson’s disease [Citation9–10].
Housing accessibility for people with Parkinson's disease
Research on housing accessibility and environmental barriers represents an uncommon approach when it comes to Parkinson’s disease [Citation28–31]. As it is a progressive disease with functional decline over time [Citation2], the P component exercises a considerable impact on the generation of accessibility problems over time, thus changing the P-E fit for people living and ageing with Parkinson’s disease [Citation31]. A study that exemplified the relevance of Parkinson’s disease research to adopt a societal perspective regarding housing matters shows that people with self-reported Parkinson’s disease have significantly more accessibility problems than matched controls even though the number of environmental barriers did not differ [Citation29]. Increased knowledge about P-E fit dynamics is imperative to develop efficient compensatory strategies, not the least regarding the E component, especially in the later stages of the disease [Citation29]. Two cross-sectional studies [Citation28,Citation31] investigated how environmental barriers contributed to housing accessibility among people with Parkinson’s disease. The first explorative study included 20 people with self-rated Parkinson’s disease and identified three top environmental barriers [Citation28]; ‘Wall-mounted cupboards and shelves placed high (kitchen)’, ‘No/too few seating places (exterior surrounding)’ and ‘No grab bars at shower/bath and/or toilet (hygiene area)’. The second study included people with a confirmed Parkinson’s disease diagnose (n = 253) [Citation31] and confirmed two of the environmental barriers found in the first study but added ‘Stairs only route (entrance)’ to the top three [Citation31]. However, when comparing the top 10 rank lists of environmental barriers from these previous studies, only four barriers were the same [Citation28,Citation31]. Thus, there is a need for further research to delve deeper into possible explanations for these differences and examine the environmental barriers that contribute most to accessibility problems over time for people with Parkinson’s disease.
The overall purpose of this study was to contribute with knowledge useful for individual housings adaptations, as well as a societal perspective on housing accessibility. The specific aim was to determine the most severe environmental barriers in terms of housing accessibility problems and how these evolved over a 3-year period among people with Parkinson’s disease who live in ordinary housing. The following research questions guided the analyses:
Which were the top 10 environmental barriers generating the most accessibility problems at baseline and at the 3-year follow-up?
Did the ranking order of the top 10 environmental barriers change over the 3 years studied? If yes, how did it change?
Did the magnitude of barrier-specific accessibility problems change for the top 10 environmental barriers over the 3 years studied? If yes, how and to what extent?
If there was a change in the magnitude of accessibility problems for the top 10 environmental barriers over 3 years, was the change related to the E component of the P-E fit?
Materials and methods
This study was based on baseline (T1) and 3-year follow-up (T2) data from the longitudinal cohort study ‘Home and Health in People Ageing with Parkinson’s Disease’ (HHPD). The baseline data collection was conducted in 2013 and the 3-year follow-up in 2016. Details regarding the project design, data collection and procedures have been described in a study protocol [Citation32].
Procedure
Two research administrators carried out the data collection at T1, and two other administrators and a PhD student collected the data at T2. All administrators underwent project-specific training. On both occasions, the data were collected through a self-administrated postal survey and at a subsequent home visit about 10 days later (including interview-administrated questions, observations and clinical assessments) for each participant.
Participants and recruitment
Participants were recruited from three hospitals in Skåne County, Sweden. At T1, 653 potential participants met the inclusion criterion of diagnosis of Parkinson’s disease for at least one year (ICD 10-code G20.9). Applying the exclusion criteria, 216 people were excluded. The remaining potential participants (n = 437) were invited to participate. However, 22 were not possible to reach, two had their Parkinson’s disease diagnosis changed, 157 declined and one person showed extensive missing data, resulting in N = 255 for the T1 sample. As they all completed the T1 assessment and agreed to be contacted again, the participants of the final baseline sample (N = 255) were eligible for the follow-up. At T2, 22 participants had deceased, three had moved and one was outside the follow-up window (3 years ±3 months). Accordingly, 229 people were invited to participate. Among those, eight were unreachable, four had a revised diagnosis, 51 declined and one showed extensive missing data.
For this specific study, people who had moved between the two data collection occasions (n = 18) and those who lived in residential care facilities (n = 9) were excluded. Accordingly, our study sample consisted of 138 participants. At T1, their mean (SD) age was 68.3 years old (8.6) and 33% were women. Mean (SD) Parkinson’s disease duration for this group was 8.9 years (5.7), for details see .
Table 1. Participant characteristics at baseline (T1) and the 3-year follow-up (T2), N = 138.
All participants gave their written informed consent, and the principles of the Helsinki Declaration were followed. The HHPD project was approved by the Regional Ethical Review Board in Lund (Nos. 2012/558 and 2015/611).
The Housing Enabler instrument: environmental barriers and housing accessibility problems
The scientifically established instrument Housing Enabler (HE) was used [Citation33–34] to assess environmental barriers and to quantify housing accessibility problems. HE has been used in cross-national research on home and health of the ageing population [Citation35] and has demonstrated sufficient reliability and validity for use in ordinary housing [Citation33]. The instrument is based on the concept of P-E fit [Citation15] and is administered in three steps. Step 1- the person (P) component is assessed through interviews and observations of functional limitations (12 items) and dependence on mobility devices (two items), all items are dichotomously assessed (present or not). In cases where functional limitations vary over time the rating should reflect the ‘worst-case-scenario’ [Citation33]. Step 2- the environmental (E) component consists of 161 physical environmental barriers in the house, categorized into the three housing sections indoors (n = 87), entrances (n = 46), and immediate exterior surroundings (n = 28). The E component is dichotomously assessed (present or not) at a home visit, based on national guidelines and standards for housing design. Step 3 generates the quantification of case-specific accessibility problems. This is achieved by using a scoring matrix, which juxtaposes the functional limitations with the environmental barriers identified in Steps 1 and 2, respectively. In each intersection between P and E where barriers are assessed as present, there are pre-defined severity ratings (0–4; higher = greater problem), that can be summed up to a total accessibility problem score (HE score). However, in this study we only calculated magnitude of accessibility problems generated by each environmental barrier. If there are no functional limitations or mobility devices the scores are always 0.
Descriptive data
Descriptive information (T1 and T2) included the variables gender, age, Parkinson’s disease duration, living alone or with a partner, see . The Hoehn and Yahr scale (HY, range I-V, higher = worse) was used to describe disease severity in ‘on-state’ [Citation36]. Severity of motor symptoms was assessed with Part III of the Unified Parkinson’s Disease Rating Scale (UPRDS III, possible scores 0–108; higher = more motor symptoms) [Citation37]. Global cognitive function was assessed by the Montreal Cognitive Assessment (MoCA, possible scores 0–30, higher = better cognitive function) [Citation38]. The Parkinson’s Disease Activities of Daily Living Scale (PADLS) was used to describe difficulties and dependence in ADL (possible scores 1–5; higher = more problems) [Citation39]. Mobility aids indoors were addressed with the variables any mobility device, cane/crutches, rollators, manual wheelchair or powered wheelchair. Housing was described by the variables: residential location (rural/semi-urban/urban), type of housing (apartment/housing/other), tenure of housing (privately owned/rental), housing adaptations (yes/no) and number of years lived in the same dwelling.
Data analysis
Descriptive statistics were used to report the sample characteristics on the two measurement occasions. To determine the environmental barriers that contributed the most to housing accessibility problems, an average magnitude was computed for each of the 161 barriers at T1 as well as T2. The top 10 environmental barriers were listed for both occasions and sorted in descending order based on the magnitude of accessibility problems to provide a ranking list. Furthermore, delta values were computed and analysed by paired samples t-tests to compare magnitudes of the top 10 barriers found at T1 and T2. Based on the top 10 environmental barriers found at T1 and T2, the housing sections were also examined with regard to magnitude of accessibility problems and displayed visually using a bar graph for each housing section at T1 and T2; paired-samples t-test was used to analyse potential changes.
In order to examine changes over time with regard to frequencies of environmental barriers, McNemar's test was used. If there was a significant change in frequency of the barrier along with a corresponding significant change in magnitude of accessibility problems between T1 and T2, we interpreted the accessibility problems as being related to the environment.
For all tests, the level of statistical significance was set to p < 0.05 and used for interpretation of results. The IBM SPSS Statistics 25 software (IBM Corporation, Armonk, NY, USA) and the HE software (Veten & Skapen HB and Slaug Enabling Development, Lund and Staffanstorp, Sweden) were used for the analyses.
Results
Top 10 environmental barriers and their ranking order at baseline and follow-up
The top three environmental barriers at T1 were: ‘No grab bar at shower/bath and/or toilette’ (hygiene area; average HE score = 7.39), ‘Stairs the only route’ (entrance; average HE score = 6.50) and ‘Wall-mounted cupboards and shelfs placed high’ (kitchen; average HE score = 6.26) (). At T2, the top three environmental barriers were: ‘Refuse bin difficult to reach’ (exterior surrounding; average HE score = 8.24), ‘Wall-mounted cupboards and shelfs placed high’ (kitchen; average HE score = 6.71) and ‘No grab bar at shower/bath and/or toilette’ (hygiene area; average HE score = 5.92). Furthermore, the ranking order of the top 10 barriers generating the most accessibility problems changed from T1 to T2. This change was mainly within the top 10 environmental barriers found at T1, although the barrier ‘Insufficient manoeuvring space around white goods/storage units’ (general indoors), which was not included at T1 was ranked as number five at T2.
Table 2. Top 10 environmental barriers (EB) generating most accessibility problems (HE score) at baseline and the 3-year follow-up, N = 138.
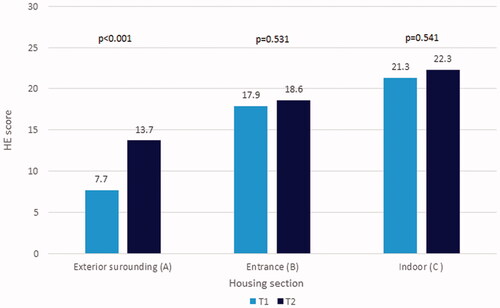
Environmental barriers in the indoor environment (summed HE score T1/T2 = 21.3/22.3) and at entrances (summed HE score T1/T2 = 17.9/18.6) contributed most to accessibility problems at T1 as well as T2 (see ).
Figure 1. Development of magnitude of accessibility problems (HE score) per housing section at the two measure points. The figure is based on summed HE scores from the top 10 environmental barriers that contributed to most housing accessibility problems per housing section, at T1 and T2. The change between T1 and T2 was analysed with paired sample t-test.
Change in magnitude of housing accessibility problems over 3-year period
Examining changes in magnitude of accessibility problems per housing section showed that immediate exterior surrounding was the only section where accessibility problems increased significantly (p < 0.001) over the 3 years (). Analysing the results on the item level, six environmental barriers showed roughly the same change in magnitude of accessibility problems over the 3-year period. Five out of those were statistically significant (see ). Two other environmental barriers had decreased significantly in the generation of accessibility problems at T2, these were ‘No grab bar at shower/bath and/or toilette’ (hygiene area) (Δ =-1.47, p = 0.041) and ‘Stair the only route’ (entrances) (Δ =-1.89, p = 0.002). The same two barriers decreased significantly in frequencies as well (p < 0.001 for both barriers). In contrast, three other environmental barriers generated a statistically significant increase in accessibility problems at T2, namely the barriers ‘Refuse bin difficult to reach’ (exterior surrounding: Δ = 4.09, p < 0.001), ‘Letterbox difficult to reach’ (exterior surrounding: Δ = 1.97, p = 0.001) and ‘Insufficient manoeuvring spaces around white goods/storage units’ (kitchen: Δ = 3.01, p < 0.001). Two out of those increased significantly regarding frequencies of the barrier, that is ‘Insufficient manoeuvring spaces around white goods/storage units’ (kitchen; p < 0.001) and ‘Refuse bin difficult to reach’ (exterior surrounding; p < 0.001). The significant increase in magnitude of accessibility problems for these two barriers were thus interpreted as partly related to greater demands in the environment in terms of environmental barriers (see ).
Discussion
The main findings of this study are that environmental barriers in the dwellings of people with Parkinson’s disease in Sweden seem to remain largely the same over a 3-year period (see ), however, with notable changes regarding their order and generation of accessibility problems. Furthermore, the magnitude of the environmental barriers situated indoors and at entrances contributed most to accessibility problems at both T1 and T2, although exterior surroundings is the only section where the accessibility problems increased significantly over the 3 years. Examining the top 10 environmental barriers, barriers in hygiene areas and at entrances were in top at T1, but decreased significantly and were ranked lower at T2. An environmental barrier in the exterior surroundings regarding waste management rose to top of the list at T2, with a significant increase in accessibility problems over 3 years. This new knowledge of how environmental barriers evolve over time for people with Parkinson’s disease is potentially useful to develop efficient housing and rehabilitation interventions for this specific population, on the individual, as well as the societal level.
Implications for occupational therapy practice
Our study is the first that addresses environmental barriers and accessibility problems among people with Parkinson’s disease with a follow-up design and the findings are in line with a previous cross-sectional study based on the same project [Citation31]. That is, nine of the top 10 barriers in the present study are the same as in Slaug et al. [Citation31], but the ranking order and magnitude of accessibility problems differ. Both studies indicate that the top 10 barriers generating most accessibility problem for this population are roughly the same. However, this needs to be further evaluated in other samples and not the least in other national contexts as the results of the current study could be a reflection of Swedish housing specifics.
Furthermore, the fact that the order of barriers and the magnitude of accessibility problems generated changed over time is in line with the notion of P-E fit [Citation15], thus indicating that there is a dynamic relationship between the person and environment, which changes over time. This is also in agreement with theories and practice models in occupational therapy, such as the PEO model that highlights the person-environment transaction [Citation17]. Importantly, the PEO model also includes the occupation component in the transaction, addressing occupational performance as the main outcome [Citation17]. In comparison, the main outcome of P-E fit is adaptive behaviour, representing a broader concept [Citation15]. Adaptive behaviour includes, for example, activities of daily living (ADL) [Citation15], which is part of occupational performance in PEO [Citation17]. Accordingly, both theories resonate with underpinnings of occupational therapy. However, focussing on how environmental barriers generate accessibility problems for people with Parkinson’s disease, in this study we did not address occupation, but rather examined the underlying aspects of the P and E components. Such basic knowledge is useful to identify intervention targets on the component level but should be complemented with data regarding how people themselves perceived the PEO transaction, thus adding the occupational aspect for people with Parkinson’s disease.
The finding that two barriers generated less accessibility problems after 3 years (‘No grab bar at shower/bath and/or toilette’, hygiene area; ‘Stairs the only route’, entrance) deserves a comment. Both decreased significantly in frequency as well as in magnitude of accessibility problems. The decrease indicates that these two barriers had been modified during the 3-year period, for example, due to individual housing adaptations reducing accessibility problems. Possible housing adaptations that could remove these environmental barriers are installation of grab bars in showers/toilettes and installation of ramps, representing some of the most common housing adaptations in Sweden [Citation26]. In the light of changes during a rather brief period of time, occupational therapists using housing adaptations to support occupational performance for people with Parkinson’s disease should take the progressive nature and the characteristic symptoms of the disease into account [Citation2]. As earlier research has shown that repeated housing adaptations cost both time and money [Citation40], a more proactive approach may be favourable for this population. For example, our results indicate that some environmental barriers generate a greater magnitude of problems after three years, which suggests that routine follow-ups of housing adaptations should be included in occupational therapy interventions, to maintain P-E fit in the long-term. Hence, it is important to inform and guide people with Parkinson’s disease and their family members to find individualised housing adaptation solutions to support active ageing during the course of the progressive disease.
A barrier that usually can be modified without far-reaching adaptations is ‘Insufficient manoeuvring space in relation to movable furnishing’ (indoors), which showed a significant decrease in frequency at T2. This implies that reorganization within the dwelling is a way to act on this barrier, which is used by people with Parkinson’s disease and their family members, presumably sometimes after advice from health care staff such as occupational therapists. For some participants such modifications had probably been implemented between T1 and T2, which resulted in fewer barriers at T2. This is one example of easily-implemented changes in the home environment that could be useful in rehabilitation for people with Parkinson’s disease.
Notably, even if this barrier was ranked lower at T2 (no. 11) it generated significantly more accessibility problems than at T1. The lower rank at T2 may appear a little contradictory, but is probably due the fact that other environmental barrier generated even greater accessibility scores and were ranked higher at this occasion. Regarding the significantly higher magnitude of accessibility problems for this barrier at T2, insufficient manoeuvring space generates increased accessibility problems particularly in relation to dependence on mobility devices. Therefore, even if environmental modifications were implemented for some participants, with the increase from 25% to 56% in the use of mobility device in our sample (see ), this was not sufficient to counteract the generation of increased accessibility problems at T2. It is therefore essential that both components of the P-E fit [Citation15] are taken into account when evaluating and planning for individual housing adaptations. Additional research is warranted to address the P component of the P-E interaction and how it contributes to accessibility problems over time in people with Parkinson’s disease.
Implications on societal level
Already in 1986, the WHO stated in the Ottawa declaration that health professionals should work towards health promotion by, for example, building health policies and supportive environments to promote public health [Citation41]. Occupational therapy theories and practices models have also stressed the need for occupational therapists to contribute to work on the societal level to promote public health [Citation17,Citation18,Citation19,Citation42]. Still this focus is not common and deserves more attention. Knowledge gained from this study could be used to develop strategies for such contributions. For example, to better plan for housing meeting the specific needs of people ageing with Parkinson’s disease, it is informative to map out where in the housing environment the environmental barriers that caused an increase in accessibility problems over time are situated. Accordingly, a detailed examination of the summed magnitude scores of accessibility problems per housing section (i.e. close exterior surroundings, entrances or indoors) could be useful.
The present study shows that exterior surroundings is the section where accessibility problems increased significantly for people with Parkinson’s disease over the 3-year period (see ). One plausible explanation for the increase of accessibility problems in the exterior surroundings is that individual housing adaptations are most commonly implemented indoors [Citation26]. The legislation regulating housing adaptations in Sweden has an individual focus and adaptation is granted to the person applying for it when approved [Citation25], based on certifications issued by qualified health care professionals. Accordingly, even if community areas used by many people often are perceived as challenging in terms of accessibility problems by individual users, societal planning should take the needs of specific populations groups, such as those living and ageing with disorders such as Parkinson’s disease, into account.
That said, with the specific knowledge on common environmental barriers related to P-E fit, occupational therapist have the potential to assume an expert role in health promotion, to work towards more accessible housing and neighbourhood environments on the societal level [Citation43] as well as for sub-groups with specific diagnoses and related needs. Our results demonstrate that entrances, bathrooms and kitchens are environments with barriers that generate accessibility problems for people with Parkinson’s disease (). This is true for other sub-groups of the population as well, such as people with multiple sclerosis [Citation44] or other diagnoses and functional limitations [Citation45–46]. This shows that people with similar functional limitations but with different diagnoses could have similar accessibility problems and thus benefit from the same kind of interventions. Knowledge about the needs of specific diagnose groups in the general population as well as knowledge about manifestations of functional limitation across diagnose groups is important for occupational therapists.
One specific example from this study, which indicates that some environmental barriers should be considered on the aggregated level is ‘Refuse bin difficult to reach’ (exterior surrounding). This barrier increased significantly regarding both frequency and accessibility problems from T1 to T2, indicating a change that at least was partially related to higher demands in the environment. A potential reason for the increase is probably that the standards of waste management have changed in Sweden. For example, which garbage types that have to be sorted and how, including the location and design of rubbish stations. Some of these changes do not benefit people with functional limitations and should be addressed on the societal level, which requires systematic approaches based on objective and reliable data. Consequently, the use of valid and reliable instruments that are based on national standards for housing design is critical, rather than addressing subjective, individual perspectives when evaluating accessibility problems and environmental barriers for actions on societal level [Citation43].
Much of the detailed knowledge on environmental barriers and accessibility problems reported in this study could be used in public health policies. This is in line with the World Report of Disability [Citation14], which acknowledges that housing standards fostering accessibility can create enabling environments. However, the knowledge of housing standards is generally low and therefore not sufficiently applied even if issues related to housing accessibility have been discussed for decades. This is in line with a recent published article using a five-dimension framework to further the understanding of crucial variables in decision-making about housing accessibility [Citation47], where the authors highlight that in the housing sector, the socioeconomic dimension is more in focus than the biophysical. While adhering to housing standards more systematically in the planning and building sector has the potential to enable people with disabilities to live more active and independent lives, knowledge based on the realities of people living and ageing with Parkinson’s disease could be used to communicate issues with actors in the housing provision section in a concrete manner.
Methodological considerations
The HE instrument is a standardised assessment instrument, which was developed and used mainly in research and practice targeting older adults in general [Citation6,Citation27]. As psychometric properties are sample dependent [Citation48], it is vital to highlight that those prior psychometrical evaluations [Citation34] did not explicitly address people with Parkinson’s disease, which could affect the results of this present study. Norin et al. [Citation49] addressed accessibility problems for people with spinal cord injury and specific considerations when HE is used in samples with high frequencies of complex housing adaptations (e.g. lifts) and/or use of specific mobility devices. For example, one recommendation is to make a distinction between manual and powered wheelchairs, as well as between rollators and other walking assistance devices in the P component in order to improve the construct validity of the instrument [Citation49]. That is, the magnitude of accessibility problems may be overestimated as rollators and powered wheelchairs compensate for some environmental barriers. As rollators are the most commonly-used mobility devices among people with Parkinson’s disease [Citation12], these issues may therefore be essential for this Parkinson’s disease population as well. Our results should therefore be interpreted in the light of the information on mobility devices presented in .
The findings that the barrier ‘Insufficient manoeuvring spaces around white goods/storage units’ (kitchen) increased in frequency as well as in magnitude of accessibility problem at T2 compared to T1 indicate a worsening of the environment over the 3 years studied. However, it cannot be ruled out that this result is influenced by variations in the assessments on the two data collection occasions. That is, different data collectors were involved at T1 and T2, which may have affected the results. The data collectors did undergo project-specific training to ensure reliable assessments, and previous studies have demonstrated sufficient inter-rater reliability of the HE [Citation50]. However, some items are dependent on rater judgement and thus more susceptible to variation [Citation51].
Another methodological matter is that although we performed several statistical comparisons, we did not formally correct for multiple testing by using for example the Bonferroni correction. However, the latter is sensitive to Type II errors, meaning that it could fail to recognize valid significant differences even if they are there [Citation52]. With this in mind, we advise cautiousness when interpreting p-values just below 0.05 and consider them more as a trend than a definite significant finding.
Conclusions
To the best of our knowledge, this is the first study aimed at identifying the environmental barriers that generate the most severe accessibility problems over time for people with Parkinson’s disease living in ordinary housing. The knowledge gained from this study has the potential to contribute to the development of more foresighted and sustainable individual housing adaptations supporting ageing-in-place for people with Parkinson’s disease. Moreover, supported by this study occupational therapy has the potential to contribute with knowledge on the aggregated level. That is, the new knowledge reported in this study can also be utilized on the societal level to address accessibility problems systematically, thus contributing evidence to support the development of housing provision and public health policies taking the needs of people living and ageing with Parkinson’s disease into account. Future studies need to investigate how environmental barriers and accessibility problems evolve over longer time periods, and to further explore how the P component impacts the evolvement of P-E fit over time among people with Parkinson’s disease.
Acknowledgements
The authors thank the participants of the HHPD project for their contributions to research and to enabling this study. This study was conducted within the context of the Centre for Ageing and Supportive Environments (CASE) and the Strategic Research Area in neuroscience (MultiPark) at Lund University, Sweden. The first author’s (NA) learning process was supported by the National Graduate School of Competitive Science on Ageing and Health (SWEAH).
Disclosure statement
The Housing Enabler is a commercial product sold by Veten & Skapen HB and Slaug Enabling Development with Iwarsson and Slaug as copyright holders and owners. The remaining authors have no conflict of interest.
Data availability statement
The data used in this study contains sensitive information about the study participants and they did not provide consent for public data sharing. The current approval by the Regional Ethical Review Board in Lund, Sweden (nos. 2012/558 and 2015/611) does not include data sharing. Data that supports the findings in this study could be shared on request from a qualified academic investigator for the sole purpose of replicating the present study, provided the data transfer is in agreement with EU legislation on the general data protection regulation and approval by the Swedish Ethical Review Authority.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
Additional information
Funding
References
- Hariz GM, Forsgren L. Activities of daily living and quality of life in persons with newly diagnosed Parkinson's disease according to subtype of disease, and in comparison to healthy controls. Acta Neurol Scand. 2011;123(1):20–27.
- Jankovic J. Parkinson's disease: clinical features and diagnosis. J Neurol Neurosurg Psychiatry. 2008;79(4):368–376.
- Freedman VA, Spillman BC. The residential continuum from home to nursing home: size, characteristics and unmet needs of older adults. J Gerontol B Psychol Sci Soc Sci. 2014;69:42–50.
- Habermann B, Shin JY. Preferences and concerns for care needs in advanced Parkinson's disease: a qualitative study of couples. J Clin Nurs. 2017;26(11-12):1650–1656.
- Vossius C, Nilsen OB, Larsen JP. Parkinson's disease and nursing home placement: the economic impact of the need for care. Eur J Neurol. 2009;16(2):194–200.
- Wahl HW, Fänge A, Oswald F, et al. The home environment and disability-related outcomes in aging individuals: what is the empirical evidence? Gerontologist. 2009;49(3):355–367.
- Mahler M, Sarvimäki A, Clancy A, et al. Home as a health promotion setting for older adults. Scand J Publ Health. 2014;42:3–40.
- Bhidayasiri R, Jitkritsadakul O, Boonrod N, et al. What is the evidence to support home environmental adaptation in Parkinson's disease? A call for multidisciplinary interventions. Parkinsonism Relat Disord. 2015;21(10):1127–1132.
- Ramos JB, Duarte GS, Bouça-Machado R, et al. The role of architecture and design in the management of Parkinson's disease: a systematic review. J Parkinsons Dis. 2020;10(4):1301–1314.
- Iwarsson S, Andersson N, Slaug B, et al. People with Parkinson's disease and housing issues: a scoping review. Health Sci Rep. 2022;5(2):e511.
- Raggi A, Leonardi M, Ajovalasit D, et al. Functioning and disability in Parkinson's disease. Disabil Rehabil. 2010;32(sup1):S33–S41.
- Kader M, Jonasson SB, Iwarsson S, et al. Mobility devices in people with Parkinson's disease: a 3-year follow-up study. Acta Neurol Scand. 2018;138(1):70–77.
- World Health Organization (WHO). ICF – international classification of functioning, disability and health. Geneva: WHO; 2001.
- World Health Organization, The World Bank. World report on disability. Geneva: World Health Organisation & The World Bank: 2011.
- Lawton MP, Nahemow L. Ecology and the aging process. The psychology of adult development and aging. Washington DC, US: American Psychological Association; 1973.
- Iwarsson S, Ståhl A. Accessibility, usability and universal design-positioning and definition of concepts describing person–environment relationships. Disabil Rehabil. 2003;25(2):57–66.
- Law M, Cooper B, Strong S, et al. The person–environment–occupation model: a transactive approach to occupational performance. Can J Occup Ther. 1996;63(1):9–23.
- Townsend E, Polatajko H. Enabling occupation II: advancing an occupational therapy vision for health, well-being, and justice through occupation. Ottawa: CAOT Publications ACE; 2007.
- Granbom M, Iwarsson S, Kylberg M, et al. A public health perspective to environmental barriers and accessibility problems for senior citizens living in ordinary housing. BMC Public Health. 2016;16(1):1–11.
- Wahl HW, Iwarsson S, Oswald F. Aging well and the environment: toward an integrative model and research agenda for the future. Gerontologist. 2012;52(3):306–316.
- Sturkenboom IH, Graff MJ, Hendriks JC, et al. Efficacy of occupational therapy for patients with Parkinson's disease: a randomised controlled trial. Lancet Neurol. 2014;13(6):557–566.
- Chapman L, Nelson D. Person-centered, community-based occupational therapy for a man with Parkinson’s disease: a case study. Act Adapt Aging. 2014;38:94–112.
- Meek C, Morgan E, Walker MF, et al. Occupational therapy to optimise independence in Parkinson's disease: the designing and recording of a randomised controlled trial intervention. Br J Occup Ther. 2010;73(4):178–185.
- Malmgren Fänge A, Lindberg K, Iwarsson S. Housing adaptations from the perspectives of Swedish occupational therapists. Scand J Occup Ther. 2013;20(3):228–240.
- Svensk författningssamling, SFS 2018:222. The Housing Adapatation Act. [Swedish].
- Swedish National Board of Housing, Buildning and Planning. Bostadsanpassningsbidragen 2019 [Housing Adaptation Grants 2019]. Boverket. 2020. [cited Feb 23]. Available from: https://www.boverket.se/globalassets/publikationer/dokument/2020/bostadsanpassningsbidragen-2019.pdf.
- Pettersson C, Slaug B, Granbom M, et al. Housing accessibility for senior citizens in Sweden: estimation of the effects of targeted elimination of environmental barriers. Scand J Occup Ther. 2018;25(6):407–418.
- Slaug B, Nilsson MH, Iwarsson S. Characteristics of the personal and environmental components of person–environment fit in very old age: a comparison between people with self-reported Parkinson's disease and matched controls. Aging Clin Exp Res. 2013;25(6):667–675.
- Nilsson MH, Haak M, Iwarsson S. Housing and health: very old people with self-reported Parkinson's disease versus controls. Parkinsons Dis. 2013;2013:1–8.
- Nilsson MH, Ullén S, Ekström H, et al. The association between indicators of health and housing in people with Parkinson's disease. BMC Geriatr. 2016;16:146–153.
- Slaug B, Iwarsson S, Ayala JA, et al. Housing accessibility problems for people with Parkinson's disease. Acta Neurol Scand. 2017;136(5):501–510.
- Nilsson MH, Iwarsson S. Home and health in people ageing with Parkinson's disease: study protocol for a prospective longitudinal cohort survey study. BMC Neurol. 2013;13:142–149.
- Iwarsson S, Haak M, Slaug B. Current developments of the housing enabler methodology. Br J Occup Ther. 2012;75(11):517–521.
- Iwarsson S, Slaug B. Housing enabler – a method for rating/screening and analysing accessibility problems in housing. 2nd ed. Lund & Staffanstorp (Sweden): Veten och Skapen HB & Slaug Enabling Development; 2010.
- Iwarsson S, Löfqvist C, Oswald F, et al. Synthesizing ENABLE-AGE research findings to suggest evidence-based home and health interventions. J Housing Elder. 2016;30(3):330–343.
- Hoehn MM, Yahr MD. Parkinsonism: onset, progression and mortality. Neurology. 1967;17(5):427–442.
- Fahn S, Elton RL. Unified Parkinsons disease rating scale. In: Fahn S, Marsden CD, Goldstein M, Calne DB, editors. Vol. 2, Recent developments in Parkinsons disease. Florham Park (NJ): Macmillan Healthcare Information; 1987. p 153–163.
- Nasreddine ZS, Phillips NA, Bédirian V, et al. The montreal cognitive assessment, MoCA: a brief screening tool for mild cognitive impairment. J Am Geriatr Soc. 2005;53(4):695–699.
- Hobson JP, Edwards NI, Meara RJ. The Parkinson's disease activities of daily living scale: a new simple and brief subjective measure of disability in Parkinson's disease. Clin Rehabil. 2001;15(3):241–246.
- Malmgren Fänge A. Strategies for evaluation of housing adaptations – accessibility, usability and ADL dependence. Lund (Sweden): Division of Occupational Therapy; 2004.
- World Health Organization (WHO). The Ottawa charter for health promotion. 1986. [cited 2021 Oct 01]. Available from: https://www.who.int/publications/i/item/ottawa-charter-for-health-promotion.
- Carlsson G, Slaug B, Månsson Lexell E. Assessing environmental barriers by means of the Swedish Craig Hospital Inventory of Environmental Factors among people post-stroke. Scand J Occup Ther. 2021;28(5):366–374.
- Iwarsson S. Assessing the fit between older people and their physical home environments – an occupational therapy research perspective. In: Wahl HW, Scheidt R, Windley P, editors. Focus on aging in context: socio-physical environments. Annual review of the Gerontological Society of America. New York: Springer Publishing Company, Inc; 2004. p. 85–109.
- Bishop M, Sheppard-Jones K, Roessler RT, et al. Specialized housing needs of Americans with multiple sclerosis: descriptive results of a national analysis. J Vocational Rehab. 2013;39(2):111–125.
- Ahrentzen S, Tural E. The role of building design and interiors in ageing actively at home. Building Res Inform. 2015;43(5):582–601.
- Namkee C. Stability and changes in living arrangement among unmarried older persons. J Housing Elder. 2004;18:69–89.
- Jonsson O, Frögren J, Haak M, et al. Understanding the wicked problem of providing accessible housing for the ageing population in Sweden. IJERPH. 2021;18(3):1169.
- Hobart J, Cano S. Improving the evaluation of therapeutic interventions in multiple sclerosis: the role of new psychometric methods. Health Technol Assess. 2009;13(12):1–177.
- Norin L, Iwarsson S, Haak M, et al. The housing enabler instrument: assessing threats to reliability and validity. Br J Occup Ther. 2019;82(1):48–59.
- Helle T, Nygren C, Slaug B, et al. The Nordic housing enabler: inter-rater reliability in cross-Nordic occupational therapy practice. Scand J Occup Ther. 2010;17(4):258–266.
- Slaug B, Schilling O, Helle T, et al. Unfolding the phenomenon of inter-rater agreement: a stepwise analytic approach for in-depth examination was proposed. J Clin Epidemiol. 2012;65:1016–1025.
- Feise R. Do multiple outcome measure require p-value adjustments? BMC Med Res Methodol. 2002;2:4.
