Abstract
Background
While occupational therapists value occupation-based practice, they appear to spend less time on this approach and more time on impairment-based practices. Several barriers are reported for the occupation-based approach.
Aim
To explore different aspects of occupation-based practice among occupational therapists working in hospitals and rehabilitation institutions, and to examine associations between sociodemographic factors, barriers, and occupation-based practice.
Materials and methods
A cross-sectional survey was conducted. Participants were occupational therapists working in hospitals and rehabilitation institutions in Norway. The data were analysed with descriptive statistics and logistic regression.
Results
The therapists (n = 124) valued occupation-based practice and reported using it frequently and to a large extent. Relatively small proportions of their practice (26% assessments and 38% interventions) were classified as occupation-based. Lack of time, space and equipment were reported as large barriers. Lack of time and lack of equipment were associated with low self-reported level of occupation-based practice.
Conclusions
The participants valued occupation-based practice, while the reported assessment and intervention methods were mainly not occupation-based. Several barriers were reported, and some were associated with less use of occupation-based practice.
Significance
The results can be used to raise awareness of occupational therapists’ use of occupation-based practice and barriers to this approach.
Introduction
In hospitals and rehabilitation institutions, there may be a tension between practice based on a medical approach and practice based on a more holistic, occupation-based perspective. The medical model appears to be dominant, and the use of an occupation-based practice is thus perceived as challenging [Citation1–4]. Some authors have argued that the role and purpose of occupational therapy may be lost in the acute setting [Citation5]. In recent years, there has been discussion about whether occupational therapists have moved away from using occupation as a means to achieve desired patient outcomes [Citation6]. For example, it has been argued that occupational therapists in hospitals tend to use a medical approach focussing on bodily functions, rather than an occupation-based approach [Citation5,Citation7]. Impairment-focussed practice is commonly referred to as the bottom-up approach, where the therapist considers problems in underlying bodily or psychological functions (e.g. strength or memory) as possibly causing the patient’s challenges in daily activities [Citation8]. A logical consequence of using an impairment-based model of practice is to target the suggested underlying dysfunctions in interventions.
Several occupational therapists have advocated a different perspective on people’s daily life challenges. In fact, while discussing the impairment-based model, Wilding and Whiteford [Citation9] suggested that ‘philosophically, theoretically and practically, occupational therapy does not fit at all well with medicine’s philosophy, theory and practice’. They argued that the focus of the medical model is about curing illness and injury, while the focus of occupational therapy is about engaging people in occupation.
In line with the latter perspective, occupation-based practice places occupation at the core, both as the intervention and as the desired outcome of the intervention [Citation2]. The term occupation-based practice does not have a universally accepted definition. However, Fisher and Marterella [Citation8] have defined it as evaluations or interventions where the occupational therapist actively engages their patients in a ‘real’ task performance that is personally relevant. Any evaluation method that does not involve an observation of the patient engaged in an occupation is not considered occupation-based. Thus, according to Fisher and Marterella, interviews, questionnaires, evaluations of the environment, and decontextualized tests of underlying body functions are not occupation-based practices. Their definition is used as a basis for the understanding of occupation-based practice in this study.
The literature has shown scientific support for the use of occupation-based therapy. Occupation-based occupational therapy has been found to improve stroke patients’ general health, emotional roles [Citation10] and occupational performance in daily activities [Citation11]. A literature review also found that engagement in meaningful activities enhanced health and well-being, while it also stimulated the neurological system [Citation12]. A meta-analysis additionally suggested that occupation-based cognitive rehabilitation is beneficial for improving daily functioning and psychosocial functions in traumatic brain injury patients [Citation13].
As demonstrated from previous studies, most occupational therapists have been found to report benefits from using occupation in treatment [Citation1,Citation7,Citation14–16]. However, daily use of occupation-based assessment and treatment methods appears to occur infrequently among them [Citation7]. A study by Lloyd et al. [Citation17] showed that occupational therapists spent 34% of their time on occupation-based interventions. Comparably, Colaianni and Provident [Citation14] reported from the hand therapy setting that occupational therapists spent a lower percentage of their time engaging clients in occupation-based interventions (21–30%), and a higher percentage of their time engaging clients in rote exercise (41–50%). Munin et al. [Citation18] discovered that almost half of the reported interventions aimed at strengthening the limbs were performed through exercise. Similarly, Mulligan et al. [Citation2] found that the vast majority (86%) of participants agreed that their interventions should directly address the patients’ occupational needs, and 73% responded that they always or often used occupation-based practice. However, while examining their assessment practice, only 22% of the stated assessment methods reflected this view and were classified as occupation-based, while 44% were classified as an assessment of body functions. In Mulligan et al.’ study, therapists with longer experience tended to work more occupation-based than more inexperienced therapists. In a scoping review by Murray et al. [Citation19] hardly any evidence was found that occupational therapists practiced occupation-based in the acute hospital setting. In summary, while occupational therapists have been found to share positive attitudes regarding occupation-based practice, their attitudes seem to have a limited impact on their actual practice.
In the literature, various barriers to implementing occupation-based practice in hospitals and rehabilitation institutions have been highlighted. Hospital departments have been perceived as artificial, with limited space and resources to engage patients in occupation [Citation5,Citation17,Citation20]. Lack of time to practice occupation-based was shown to be a barrier due to the high volume of patients and the perception that it took too much time, compared with body function training [Citation17,Citation21]. Furthermore, the multidisciplinary teams’ attitudes towards the importance of occupation have been identified as a barrier [Citation21], and referrals from other professions that focus on the patients’ impairment may limit the occupational therapists’ focus on occupation [Citation20,Citation22]. In the hand therapy setting, treatment restrictions and protocols have been identified as barriers [Citation14]. Another barrier is the occupational therapists’ attitudes towards occupation-based practice, as some report lack of imagination, effort and experience to engage their patients in occupation as they were more familiar with practices targeting body functions [Citation17,Citation23]. Lastly, the patient’s point of view and perception of what occupational therapy is, and what they should do in occupational therapy sessions, has been perceived as a barrier in several studies [Citation14,Citation17,Citation21].
In summary, previous research has shown that occupation-based practice is a valued approach amongst occupational therapists. Nonetheless, occupational therapists are inclined to use a medical approach with a focus on body functions, rather than an occupation-based approach. As a result, there may be a tension between occupational therapists’ occupation-based mindset, and their practices, which are often targeting their patients’ bodily functions. An exploration of the current practices in the hospital and rehabilitation setting can provide useful information about the use of, and attitudes towards, occupation-based practice. Moreover, it can inform about barriers for occupation-based practice as perceived among occupational therapists, and how such barriers are related to their occupation-based practice. Studies linking barriers with actual practices are currently lacking.
Study aim
The aim of this study was to explore three aspects of occupation-based practice among occupational therapists working in hospitals and rehabilitation institutions: their attitudes towards occupation-based practice, their use of it and their perceived barriers for implementing it. Further, the study aimed to examine associations between sociodemographic factors, work experience, reported barriers and occupation-based practice.
Materials and methods
Design
This study had a cross-sectional explorative design based on survey methodology.
Participants and procedure
Eligible participants were occupational therapists employed at hospitals or rehabilitation institutions in Norway. The survey took place in the beginning of 2021. On behalf of the project group, contact persons at hospitals and rehabilitation institutions were asked to forward an e-mail with the survey to occupational therapists employed at their site. Although it is difficult to know precisely how many therapists received the link, it was estimated that approximately 470 occupational therapists received the link, based on information provided from the contact persons. The survey was closed after three weeks, and all data were transferred to the project group.
The survey tool
A survey was developed specifically for this study. The survey was designed inspired by previous research [Citation2,Citation7] and Fisher and Marterellas’s theory of occupation-based practice [Citation8]. A draft questionnaire was set in ‘Nettskjema’, an electronic survey programme. Six selected occupational therapists working in hospital and rehabilitation settings agreed to pilot the electronic survey. Based on their feedback, the questionnaire was revised and finalized. The questionnaire contained information about what was meant with the terms ‘occupation’ and ‘occupation-based’. The final version of the questionnaire consisted of the questions as outlined below.
Sociodemographics
We collected demographic information: age, gender, highest completed education (bachelor’s degree, bachelor’s degree with further education, master’s degree and doctoral degree), years of experience and area of practice (general health, occupational health, paediatric health, geriatric health, public health, mental health and somatic health).
Attitudes towards occupation-based practice
The questionnaire included four statements about attitudes. The statements were ‘I think occupation-based practice is important’, ‘the use of occupation-based practice is valued by my colleagues’, ‘the use of occupation-based practice is valued by the administration where I work’ and ‘I think all occupational therapy practices should contain occupation-based practice’. The response categories were ‘strongly disagree’, ‘slightly disagree’, ‘neutral’, ‘slightly agree’ and ‘strongly agree’.
Assessment and intervention practices
The participants were asked ‘which five assessment methods do you use most frequently in your workday?’, with five open spaces where they could respond as they wished. Then they were asked ‘how often do you conduct assessment methods where the patient is engaged in an occupation?’ with the response categories ‘every working day’, ‘weekly’, ‘monthly’ and ‘less often than monthly’. The next question was ‘to what extent do you think that the assessment methods you use are occupation-based?’ with the response categories ‘not occupation-based’, ‘slightly occupation-based’, ‘quite occupation-based’ and ‘very occupation-based’. The participants were asked if they conducted interventions in their workday. If their answer was ‘yes’, the same questions and response categories as with assessments were repeated, changing ‘assessments’ with ‘interventions’. If the respondents answered ‘no’ they automatically skipped the questions regarding interventions.
Barriers for occupation-based practice
A question about barriers followed: ‘To what extent are the following barriers an obstacle for occupation-based practice in your workday?’, the barriers listed are ‘lack of time to plan’, ‘lack of time to conduct’, ‘lack of time to document’, ‘lack of space’, ‘lack of equipment’, ‘other professions do not value it’, ‘occupational therapy colleagues do not value it’, ‘own inadequate skills’, ‘restrictions from guidelines and procedures’ and ‘the patients’ lack of understanding of the purpose’. The response categories were ‘not a barrier’, ‘small barrier’, ‘quite large barrier’, ‘large barrier’ and ‘very large barrier’.
Data analysis
Responses to the open-ended questions regarding which five assessment and intervention methods the participants used most frequently were divided into categories. First, the categories were formulated after studying the content of the responses. Second, Fisher and Marterella’s [Citation8] definition of what an occupation-based assessment or intervention should contain was used when categorizing the responses as ‘occupation-based’.
The quantitative data were analysed descriptively, using frequencies and percentages for categorical variables and means and standard deviations for continuous variables. As a preliminary step in the logistic regression analysis, the dependent variables were dichotomized from an ordinal scale: responses indicating ‘very’ and ‘quite’ occupation-based were recoded to represent ‘high level of occupation-based practice’ whereas responses indicating ‘slightly’ and ‘not’ were recoded to represent ‘low level occupation-based practice’. The education level variable was dichotomized, representing bachelor’s degree versus higher (the latter category including further education, master’s degree and doctoral degree). Single and multiple logistic regression analyses were used to examine the associations between demographic variables, work experience, perceived barriers for occupation-based practice and the level of occupation-based practice in assessments and interventions. Separate analyses were performed for assessment and intervention, respectively. The strength of associations (effect sizes) was reported as odds ratio (OR), with 95% confidence interval (CI) calculated for the OR. An OR below 1 indicates reduced odds for ‘high level of occupation-based practice’, whereas an OR above 1 indicates increased odds. The significance level was set at p < 0.05. Data were analysed using SPSS version 27 (IBM Corp., Armonk, NY) [Citation24].
Ethics
Approval for the study was obtained from the Norwegian Centre for Research Data (project number 174,813). Participants were informed that participation was voluntary and that their responses would be treated confidentially. Informed consent to participate was collected electronically as a part of the survey.
Results
Participant demographics
A total of 124 surveys were completed. Based on an estimated eligible sample of 470 occupational therapists, the response rate was approximately 26%. In the sample, the mean age was 40.6 years (SD = 11.3) and 111 (89.5%) were women. There were 98 (79%) occupational therapists working in somatic health and 77 (62.1%) of the participants had at least one year of further education after completing a bachelor’s degree. The average length of work experience was 15.5 years (SD = 10.3). The sample characteristics are displayed in .
Table 1. Sample characteristics (n = 124).
Attitudes towards occupation-based practice
As presented in , 90 (72.6%) of the participants strongly agreed that occupation-based practice is important. There were 73 (58.9%) participants that strongly agreed to the statement that all occupational therapy practices should contain occupation-based practice. Half of the participants (90) strongly agreed that the use of occupation-based practice is valued by their colleagues. Only 39 (31.5%) of the participants strongly agreed that occupation-based practice is valued by the administration.
Table 2. Attitudes towards occupation-based practice (n = 124).
The use of occupation-based practice
shows the distribution of how often the participants performed assessments or interventions where the patient is engaged in an occupation. With regard to assessment methods, 94 (75.8%) of the occupational therapists responded that they used assessment methods where the patient is engaged in an occupation every working day or weekly. With regards to interventions, 94 (84%) responded that they performed interventions where the patient is engaged in an occupation every working day or weekly.
Table 3. Frequency of use of occupation-based methods.
shows the distribution of the participants’ attitudes towards their use of occupation-based assessment and intervention methods. With regards to assessment methods, 80 (64.5%) of the participants responded that they think the assessment methods they use are very or quite occupation-based. With regards to intervention, 91 (81.3%) of the occupational therapists responded that the interventions they perform are very or quite occupation-based.
Table 4. Attitudes towards the use of occupation-based methods.
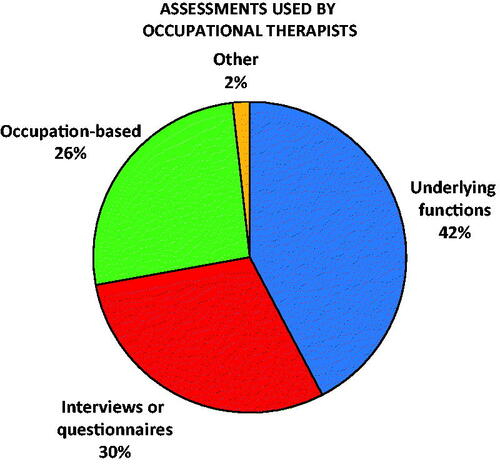
The extent to which respondents engaged in occupation-based practices was then inferred from the specific assessment and intervention methods reported by the occupational therapists. With regards to assessments, the responses were divided into the following categories: ‘underlying functions’ which included assessments of body-, cognitive- and mental functions, ‘interviews or questionnaires’ which included assessments with a focus on occupation or the environment, ‘occupation-based’ assessments where the patient is engaged in a meaningful occupation according to the theory of Fisher and Marterella [Citation8], and lastly ‘other’ which included responses that could not be categorized due to lack of context and responses not reporting an assessment method. shows the distribution of assessment methods within these categories. The participants reported 567 assessment methods.
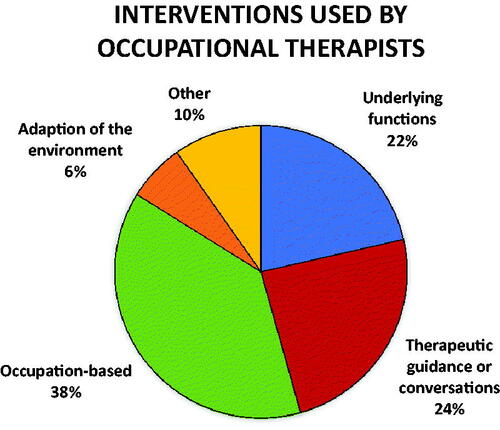
With regard to interventions, the responses were divided into the following categories: ‘underlying functions’ which included rote practice/exercise of underlying functions, ‘therapeutic guidance or conversations’, e.g. guidance in occupational balance or ergonomics, ‘adaptation of the environment’, e.g. wheelchairs or home adaptions, ‘occupation-based’ interventions where the patient is engaged in a meaningful occupation according to the theory of Fisher and Marterella [Citation8], and ‘other’ which contained responses that could not be categorized due to the same reasons as described for assessments. shows the distribution of interventions within these categories. The participants reported 471 intervention methods.
Barriers for the use of occupation-based practice
The participants were asked to what extent several factors served as barriers to occupation-based practice. See for an overview of how the responses were distributed. The barriers with the most responses in the ‘large barrier’ and ‘very large barrier’ categories were ‘lack of time to conduct’, ‘lack of space’ and ‘lack of equipment’. Conversely, most participants (n = 109, 87.9%) responded that ‘occupational therapy colleagues do not value it’ was not a barrier.
Table 5. The distribution of reported barriers for occupation-based practice (n = 124).
Factors associated with occupation-based practice
None of the sociodemographic variables were found to be associated with occupation-based practice, consequently these variables were excluded from the adjusted analysis. shows the associations between the independent variables and a high level of occupation-based assessment practice. With regards to assessment methods, when running the logistic regression with all predictors included, higher perceived levels of the barrier ‘other professions do not value it’ was associated with a higher likelihood of occupation-based assessment practice (OR: 2.03, p = 0.04). Perceiving ‘lack of time to conduct’ to be a more important barrier was associated with lower likelihood of occupation-based assessment practice (OR: 0.43, p = 0.004).
Table 6. Associations with a high level of occupation-based assessment practice (n = 124).
Factors associated with high level of occupation-based interventions are shown in . Regarding interventions, when adjusting for other predictors, perceiving more barriers related to lack of equipment (OR: 0.33, p = 0.01) was associated with lower likelihood of occupation-based intervention practice.
Table 7. Associations with a high level of occupation-based intervention practice (N = 112).
Discussion
The study found that the occupational therapists self-reported a high level of occupation-based practice. However, when examining the specific assessment and intervention methods reported, only 26% of the assessments and 38% of the interventions were classified as occupation-based. Lack of time, lack of space and lack of equipment were considered prominent barriers to occupation-based practice, and the lack of time and equipment were found to be significantly associated with self-reported occupation-based practice.
In this survey, 76% answered that they used occupation-based assessments daily or weekly. This is similar to the results reported by Grice [Citation7], whose findings showed that 77% answered likewise. In our survey, it was also found that 64.5% of the participants responded that they think the assessment methods they use are very or quite occupation-based. By examining the stated assessment methods, it was found that only 26% of the assessment methods mentioned were occupation-based while 42% of the methods were related to underlying functions. This is similar to the findings in Mulligan et al. [Citation2] which showed that of the assessments methods mentioned, 22% were categorized as occupation-based and 44% as impairment-based. Studies by Alotaibi et al. [Citation25] and Robertson and Blaga [Citation26] also reported that most assessments used by occupational therapist focussed on bodily functions. The lack of availability [Citation7,Citation25], and lack of knowledge and familiarity [Citation7,Citation27] has been shown to explain the somewhat low use of occupation-based practice in assessments.
It was found that 84% of the participants stated that they use occupation in intervention daily or weekly, and 81% responded that they use occupation-based approaches in interventions to a very large or quite large extent. These findings are coherent with the findings in Mulligan et al. [Citation2] demonstrating that 73% of participants in medical settings reported that they always or often used occupation-based activities. Similarly, Grice [Citation7] found that most participants (85%) believed they were utilizing occupation-based interventions. However, in our study, while examining the five most frequently used intervention methods, it emerged that only 38% of the intervention methods stated by the occupational therapists were occupation-based. This is similar to the findings in Lloyd et al. [Citation17] which found that the participants spent an average of 34% of their time on occupation-based interventions. Similarly, in Mulligan et al. [Citation2] of the intervention activities or modalities mentioned, 20% were occupation-based activities and 50% were associated with rote exercise of bodily functions. A higher percentage of interventions targeting bodily functions was also found in Colaianni and Provident [Citation14] and Munin et al. [Citation18].
Most participants (72.6%) in our study stated that occupation-based practice is important, likewise, several other studies also reported participants stating that there are benefits of using occupation in treatment [Citation14] and that it is important to use occupation as treatment [Citation2,Citation16]. To summarize the findings, it seems clear that it is a discrepancy between the self-reported use and attitudes towards occupation-based practice and the actual use analysed by classifying the reported methods. The subjective belief of the occupational therapists is that they practice occupation-based, but based on the actual measures and interventions used, their practice appears not to be as occupation-based as they thought. This is similar to Mulligan et al. [Citation2] who also found this in their sample, which suggests that this is a relevant concern also in other countries.
The occupational therapists used occupation-based practice more frequently in interventions than with assessments. This is possibly connected to several causes such as expectations from other professions or lack of easy access to occupation-based assessment tools. It may be easier to conduct occupation-based interventions due to less pressure from others and fewer constraints regarding how the intervention should be conducted. This may be a challenge with assessments as some facilities have constraints on what assessment tools the therapists have to use. Occupational therapists have been found to struggle to maintain an occupational focus due to the conflict between the holistic occupation-focussed values, and the routines and expectations of the medical setting [Citation9]. An explanation for the struggle can be the use of inconsistent terminology, a proposed solution can be to alter the language to focus on ‘occupation’ rather than ‘function’ [Citation19]. It is promising that while the percentage of therapists using occupation-based practice in assessments was low, more therapists are implementing occupation in interventions. Possibly, occupational therapists may need to explain to their collaborating partners that occupational therapy assessments are aimed at occupation, rather than bodily functions. This may help the team understand the purpose of the profession and increase referrals focussing on occupations.
In this study, ‘lack of time to conduct’ was reported as a major barrier and perceiving it as a large barrier was associated with lower likelihood of occupation-based assessment practice. Multiple other studies have found lack of time to be a barrier against occupation-based practice [Citation14,Citation17,Citation21,Citation23]. The reasons most commonly stated for the lack of time in these studies are high caseload of patients, patients being discharged quickly and limited occupational therapy services. According to Murray et al. [Citation19] the fast-paced and discharge-oriented nature of acute settings often made it difficult for therapists to remain occupation-based. It has also been reported that occupational therapists had a perception that occupation-based assessments were more time consuming compared to body function training [Citation17,Citation21]. A scoping review by Spalding et al. [Citation28] suggests that occupation-based group programs can be used to achieve more therapy time.
‘Lack of equipment’ was also reported to be a large barrier, this is similar to the findings in several other studies [Citation14,Citation17,Citation21]. Perceiving ‘lack of equipment’ as a large barrier was in our study associated with lower likelihood of using occupation-based methods in interventions. The available equipment at hospitals has been found to be aimed at impairment-based treatment [Citation21]. A suggestion proposed by Bynon et al. [Citation29] on how to overcome this barrier, was to use the patients’ belongings in the therapy, therapists in Grice [Citation7] study, also found this to be a way to work around this barrier.
In this survey, most participants stated ‘other professions do not value it’ as a minor barrier. In contrast, several other studies have shown that the lack of understanding from other disciplines [Citation17], multidisciplinary team members’ perception of movement and strength as the main requirement for function, and lack of awareness about the role of the occupational therapists [Citation21] were barriers for the use of occupation-based practice. In our study, we found that higher perceived levels of the barrier ‘other professions do not value it’ were in fact associated with a higher likelihood of occupation-based assessment practice. It could be that when other professions do not value the approach, the occupational therapists become more determined to use it to assert themselves and show the uniqueness of the profession. Alternatively, the association may be oppositely directed – occupational therapists who are eager to practice occupation-based may feel discouraged by a perceived lack of valuation from their colleagues with other professional backgrounds.
‘Lack of space’ was the barrier with the most answers in ‘large barrier’ and ‘very large barrier’. This is consistent with the findings in Colaianni and Provident’s [Citation14] study where 27% reported this as a major challenge to the use of occupation-based treatment. As found in the scoping review by Murray et al. [Citation19] hospitals’ physical environments are often not encouraging occupation-based practice as the hospital wards are perceived as artificial, with limited space to support occupational engagement. Estes and Pierce [Citation23] also reported that there was a lack of easy available designated spaces, crowding influencing the patient and lack of storage. Bynon et al. [Citation29] described the environment of hospitals as designed for people to rest and recover in bed, rather than actively being engaged in occupations. The proposed solution is to use other areas of the hospitals [Citation29] and mimic more natural environments by being creative and thereby expanding the available space [Citation30].
Study limitations
A limitation in this study was the low response rate and the relatively small sample size. The survey was distributed as an open link and thus, although it is unlikely, we cannot know if someone answered the survey more than once. The majority of the participants worked in somatic health practice, which means that the responses largely represent this group. The survey did not ask whether the occupational therapists worked in a hospital or in a rehabilitation institution. Future research studies may benefit from including background questions that will enable group comparisons based on the participants’ practice setting.
There is also a possibility of response bias as some participants may have answered in a way they thought was most desirable. Although the terms ‘occupation’ and ‘occupation-based’ were defined in the questionnaire, it is possible that the definition stated by Fisher and Marterella [Citation8] can be perceived as somewhat strict. Some participants may have had different ideas of what it means to practice occupation-based and may thus have considered themselves to practice more occupation-based, compared to the employed definition. As the term ‘occupation-based’ does not have a universally accepted definition, the term may have been interpreted somewhat differently in this study, compared to previous research.
The survey tool was created by the authors based on previous research and Fisher and Marterella’s theory of occupation-based practice. While securing a strong theoretical basis for the survey and pilot-testing it among members of the target population are two important measures that serve to improve the quality of the survey, a newly developed questionnaire can still have inherent validity challenges. It is a possibility that some questions have been interpreted differently by the participants, compared to the authors who developed them. In turn, such differences will constitute challenges for the interpretation of the results.
The theoretical framework in this study was Fisher and Marterella’s [Citation8] theory of occupation-based practice. The interpretation of the results is closely linked to their definitions. The use of other theories or definitions would have changed the formulation of the questions, and the results would have been different. The study is centred around the term ‘occupation-based’, this may have excluded the other methods that occupational therapists are using that are also considered to be ‘authentic occupational therapy’ according to Fisher and Marterella [Citation8], such as occupation-focussed, client-centred and ecologically relevant approaches.
The interpretation of the stated assessment and intervention methods was conducted by the authors and could have been categorized differently by others. In this study, multiple respondents stated using ‘hand training’ (n = 35) and ‘cognitive training’ (n = 5), without giving a short description of how the training was conducted as requested in the questionnaire. This led to these answers being categorized as ‘other’, because it was impossible to know if the training was conducted using rote exercise or occupation. These answers could have changed the proportion of the categories slightly. The results from the stated assessment and intervention methods were counted. However, while some methods were mentioned more frequently than others, it does not necessarily indicate that these were the methods that the therapist spent the most time on.
This study was a cross-sectional study, and it is thus impossible to establish cause-effect relationships. There could be a possibility of reversed causality, essentially reversing the proposed relationship between the dependent and the independent variables. For example, practicing occupation-based may lead to perceiving potential barriers differently, compared to using a medically oriented approach. The data was collected during the COVID-19 pandemic, this could have influenced the participants’ use of occupation-based practice, while it was not listed as a barrier.
Conclusion
The participants in this study were found to value occupation-based practice and believed they often used this approach and to a large extent. However, the findings concerned with the reports of specific assessments and interventions suggest that the assessment and intervention methods used were mainly not occupation-based. Lack of time to conduct, lack of space and lack of equipment were prominent barriers to occupation-based practice. Lack of time to conduct, and lack of equipment, was significantly associated with lower likelihood of occupation-based practice. Future research may examine occupation-based practice in other settings and areas. Future studies could also examine possible reasons for the discrepancy between the self-reported use of occupation-based practice and the specific methods reported and may explore occupation-based assessment and intervention methods that are time-saving and not in need of much space or equipment.
Acknowledgements
The authors are grateful for the efforts made by the pilot study participants, contact persons at the hospitals, and rehabilitation institutions and the occupational therapists who participated in the study.
Disclosure statement
The authors report no conflicts of interest.
Correction Statement
This article has been corrected with minor changes. These changes do not impact the academic content of the article.
References
- April L, Ganas N, Phiri L, et al. Occupation-based practice in a tertiary hospital setting: occupational therapists' perceptions and experiences. S Afr J Occup Ther. 2017;47(3):25–31.
- Mulligan S, White BP, Arthanat S. An examination of occupation-based, client-centered, evidence-based occupational therapy practices in New Hampshire. OTJR (Thorofare NJ). 2014;34(2):106–116.
- Barker Schwartz K. The history of occupational therapy. In: Cepeau ESCBABS EB, editor. Willard & Spackman's occupational therapy. Vol. 10. Philadelphia (PA): Lippincott: Williams & Wilkins; 2003. p. 5–13.
- Kielhofner G. Conceptual foundations of occupational therapy practice. 4th ed. Philadelphia (PA): F.A. Davis; 2009.
- Britton L, Rosenwax L, McNamara B. Occupational therapy practice in acute physical hospital settings: evidence from a scoping review. Aust Occup Ther J. 2015;62(6):370–377.
- Gray JM. Putting occupation into practice: occupation as ends, occupation as means. Am J Occup Ther. 1998;52(5):354–364.
- Grice KO. The use of occupation-based assessments and intervention in the hand therapy setting - A survey. J Hand Ther. 2015;28(3):300–306.
- Fisher AG, Marterella A. Powerful practice: a model for authentic occupational therapy. Fort Collins (CO): Ciots; 2019.
- Wilding C, Whiteford G. Occupation and occupational therapy: knowledge paradigms and everyday practice. Aust Occ Ther J. 2007;54(3):185–193.
- Tomori K, Nagayama H, Ohno K, et al. Comparison of occupation-based and impairment-based occupational therapy for subacute stroke: a randomized controlled feasibility study. Clin Rehabil. 2015;29(8):752–762.
- Wolf TJ, Chuh A, Floyd T, et al. Effectiveness of occupation-based interventions to improve areas of occupation and social participation after stroke: an evidence-based review. Am J Occup Ther. 2015;69(1):6901180060p1–690118006011.
- Gutman SA, Schindler VP. The neurological basis of occupation. Occup Ther Int. 2007;14(2):71–85.
- Park HY, Maitra K, Martinez KM. The effect of occupation-based cognitive rehabilitation for traumatic brain injury: a meta-analysis of randomized controlled trials. Occup Ther Int. 2015;22(2):104–116.
- Colaianni D, Provident I. The benefits of and challenges to the use of occupation in hand therapy. Occup Ther Health Care. 2010;24(2):130–146.
- Psillas SM. Occupation-based practice in occupational therapy. Ann Arbor (MI): ProQuest Dissertations Publishing; 2019.
- Kaunnil A, Khemthong S, Sriphetcharawut S, et al. Occupational therapists’ experiences and perspectives towards occupation-based practice in Thailand: a mixed-methods study. Br J Occup Ther. 2021;84(1):54–64.
- Lloyd K, Gee BM, Dunham J, et al. Occupation-based practice: a US survey. Ann Int Occup Ther. 2019;2(3):124–132.
- Munin MC, Putman K, Hsieh C-H, et al. Analysis of rehabilitation activities within skilled nursing and inpatient rehabilitation facilities after hip replacement for acute hip fracture. Am J Phys Med Rehabil. 2010;89(7):530–540.
- Murray A, Tommaso AD, Molineux M, et al. Contemporary occupational therapy philosophy and practice in hospital settings. Scand J Occup Ther. 2021;28(3):213–224.
- Keesing S, Rosenwax L. Is occupation missing from occupational therapy in palliative care? Aust Occup Ther J. 2011;58(5):329–336.
- Daud AZC, Judd J, Yau M, et al. Issue in applying occupation-based intervention in clinical practice: a Delphi study. Soc Behav Sci. 2016;222(C):272–282.
- Wilding C, Whiteford G. Language, identity and representation: occupation and occupational therapy in acute settings. Aust Occup Ther J. 2008;55(3):180–187.
- Estes J, Pierce DE. Pediatric therapists’ perspectives on occupation-based practice. Scand J Occup Ther. 2012;19(1):17–25.
- IBM Corp. IBM SPSS Statistics for Macintosh, version 27.0. Armonk (NY): IBM Corp.; 2020.
- Alotaibi NM, Reed K, Shaban MN. Assessments used in occupational therapy practice: an exploratory study. Occup Ther Health Care. 2009;23(4):302–318.
- Robertson L, Blaga L. Occupational therapy assessments used in acute physical care settings. Scand J Occup Ther. 2013;20(2):127–135.
- Piernik-Yoder B, Beck A. The use of standardized assessments in occupational therapy in the United States. Occup Ther Health Care. 2012;26(2–3):97–108.
- Spalding K, Gustafsson L, Di Tommaso A. Occupation-based group programs in the inpatient hospital rehabilitation setting: a scoping review. Disabil Rehabil. 2020. DOI:10.1080/09638288.2020.1813818
- Bynon S, Wilding C, Eyres L. An innovative occupation-focussed service to minimise deconditioning in hospital: challenges and solutions. Aust Occ Ther J. 2007;54(3):225–227.
- Khayatzadeh Mahani M, Hassani Mehraban A, Kamali M, et al. Facilitators of implementing occupation based practice among Iranian occupational therapists: a qualitative study. Med J Islam Repub Iran. 2015;29:307–307.