ABSTRACT
Objectives: Airway manipulations induce marked fluctuations in heart rate and blood pressure. Strict narcotic legislations limit availability of fentanyl. This study was designed to compare the attenuating effects of intravenous magnesium sulfate with fentanyl on cardiovascular and arousal response following laryngoscopy and intubation, while ensuring anesthetic depth with Bispectral index monitoring.
Methods: Seventy-five female patients ASA 1 or 2, scheduled for elective surgery under general anesthesia were randomized into three groups: Group M received 40 mg/kg magnesium sulfate, Group F, 2 μg/kg fentanyl, and Group C received saline prior to induction of anesthesia. Systolic and diastolic blood pressure (SBP, DBP), heart rate (HR), and bispectral index (BIS) were measured at various time points. Maximum change in hemodynamic parameters and arousal response were calculated (ΔSBP, ΔDBP, ΔHR, ΔBIS). Adverse effects related to study drugs were recorded.
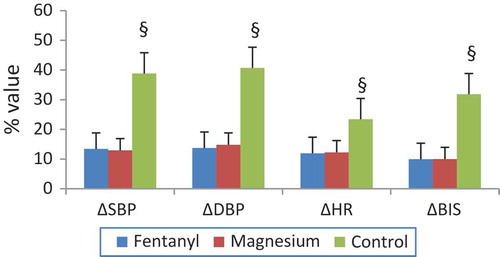
Results: There was a statistically significant increase in BP and HR following intubation in all three groups compared to prelaryngoscopy levels. ΔSBP and ΔDBP were comparable in M and F groups, but p < 0.000 when compared with control group. Following infusion of the study drug, HR increased in M group p = 0.002, while decreased in F group, p < 0.001. BIS also increased significantly after intubation compared to prelaryngoscopy levels, ΔBIS was 9.2 (SD 2.4)%, 9.9 (1.9)% in F and M groups compared to 31.8 (7.8) in group C, p < 0.000. Hypertension, although transient, occurred in 44% in control group compared to none in other groups.
Conclusion: Magnesium sulfate infusion prior to anesthesia induction effectively attenuated hemodynamic and arousal response to tracheal intubation comparable to fentanyl in normotensive patients.
Clinical trial registration: The trial was registered in Pan African Clinical Trials Registry (ID: PACTR201802003104179), http://www.pactr.org/
1. Introduction
Airway manipulations such as laryngoscopy and naso or oropharyngeal intubation during general anesthesia are considered noxious stimuli that result in undesirable responses as tachycardia, hypertension, arrhythmia, pulmonary hypertension, and increased airway reactivity. Laryngoscopy causes at least 20 mmHg increase in systolic blood pressure [Citation1]. Intracranial pressure increases at least 5 mmHg with simple tracheal suction [Citation2]. But, endotracheal intubation is the most invasive stimulus to laryngeal or pharyngeal tissues [Citation3]. This response is primarily due to catecholamine release from the adrenal medulla and norepinephrine from the adrenergic nerve terminals [Citation4].
Although the stress response is transient, it occurs 30 s after intubation persisting less than 10 min [Citation5] and easily tolerated by healthy individuals, lethal side effects can occur in patients with cardiovascular or intracranial pathology or reactive airways. Without preventive measures, almost half coronary artery disease patients experience episodes of myocardial ischemia during intubation [Citation6].
Fentanyl effectively blunts the hemodynamic response to intubation [Citation3], but adverse effects as chest wall rigidity or respiratory depression may occur [Citation7]. Due to its central vagotonic and sympatholytic action, it may augment the increased risk of reflex bradycardia in major abdominal surgery [Citation8]. Moreover, narcotic legislation in many areas including Egypt may limit its availability.
Magnesium sulfate (MgSO4) by virtue of its calcium antagonism can inhibit catecholamine release and effectively attenuate the pressor response to intubation [Citation9]. It also has the advantage of arteriolar dilatation with minimal effect on the venous system thus maintains cardiac filling and enhances the cardiac output [Citation10].
The primary end point of this study was to assess the attenuating effects of magnesium sulfate and fentanyl on SBP following intubation. Secondary end points included the changes in SBP, DBP, HR, and BIS due to study drug administration, endotracheal intubation, and their changes up to 15 min post intubation. Maximum change in hemodynamic parameters (ΔSBP, ΔDBP, ΔHR) and ΔBIS. Related adverse events.
2. Patients and methods
The trial was registered in Pan African Clinical Trials Registry ID:PACTR201802003104179.
This prospective, randomized, double blind, and controlled study was conducted after approval by our Institutional Ethics Committee. After a written informed consent, 75 females ASA 1 or 2, between 20 and 50 years, scheduled for elective surgery with orotracheal intubation, were enrolled. Excluded were patients with chronic hypertension, known ischemic heart disease, cardiac arrhythmia, or heart block of any degree. Patients with heart or renal failure, and those on beta or calcium channel blockers, or drugs that may affect hemodynamic or arousal response were also excluded. Also patients who were expected difficult intubation were not included.
Randomization of patients was done using computer generated random numbers. Each assignment slip was placed in a sealed envelope to be opened after patient recruitment. An anesthesiologist, not otherwise involved in the study, prepared the study drug in an unmarked 50 mL syringe for infusion. Neither the patient nor the attending anesthetist knew the contents of that syringe.
Upon entrance into the operating room, standard monitoring was attached. Electrocardiogram, noninvasive blood pressure, pulse oximetry (Space-lab monitor, Spacelabs healthcare company, USA). For BIS monitoring, silver pre-gelled electrodes (Aspect Medical Systems, Natick, MA, USA) were applied to the left and right frontal regions and referred to a vertex electrode which computed the BIS.
No premedication was given to patients. Prior to induction, the study drug, diluted in 50 mL 0.9% saline, was infused over 10 min according to patient allocation. Group M: received 40 mg/kg MgSO4 (Magnisol, 500 mg MgSO4/5 mL ampoule, Memphis Pharmaceuticals). Group F: received 2 µg/kg fentanyl and Group C: received 0.9% saline.
After preoxygenation, induction of general anesthesia by propofol 2 mg/kg and cisatracurium 0.15 mg/kg to facilitate orotracheal intubation. Laryngoscopy was performed 3 min after the end of cisatracurium injection if the BIS value was ≤50. If BIS values were ˃50, increments of propofol (1 mg/kg) were added. Macintosh laryngoscope size 3 and tracheal tube size 7 internal diameter were used. Laryngoscopy and intubation was performed in all cases by an experienced anesthetist noting that the patients who required more than 1 attempt at intubation, or in whom laryngoscopy and intubation took >20 s were excluded from the study. Intubation time was from insertion of laryngoscope until proper positioning of endotracheal tube. Any event related to intubation as coughing, tearing, eye opening, or movement was noted. Anesthesia was maintained with 2% sevoflurane and cisatracurium. Sevoflurane concentration was then adjusted to maintain BIS value between 45 and 55. Surgery was not allowed to commence before 10 min postintubation. At the end of the study period and prior to surgical incision, 2 µg/kg fentanyl was given to the control group. Measurements of systolic blood pressure (SBP), diastolic BP (DBP), heart rate (HR), and BIS values were taken before injection of study drug (baseline), after infusion of study drug, post-induction and postintubation at 1, 2, 4, 6, 8, 10, 12 and 15 min. Changes in SBP (ΔSBP), DBP (ΔDBP), HR (ΔHR), BIS (ΔBIS) were calculated as the difference between preintubation values and highest value recorded within 4 min following intubation. Hypertension was considered if SBP >25% of baseline values or >150 mmHg. Hypotension was considered if SBP <25% of baseline values or <90 mmHg. Bradycardia if HR<50 b/min and tachycardia if HR >100 b/min.
2.1. Sample size estimation and statistical analysis
Our primary outcome was SBP following intubation. Considering a 20% effect difference, a two-tailed alpha error of 5% and a power of 80%, the calculated sample size was 23 patients. Compensating for potential dropouts, we enrolled 25 patients per group. Statistical analysis was done using SPSS software version 21 (SPSS, Chicago, IL, USA). Quantitative data are described as means±standard deviation and compared using one-way analysis of variance (ANOVA) tests. For serially measured values, repeated-measures ANOVA followed by Bonferroni’s post hoc test was used. Student T test was used for intragroup analysis. Comparison of different groups was carried out for various categorical variables using Chi-square test. A p-value < 0.05 was considered significant.
3. Results
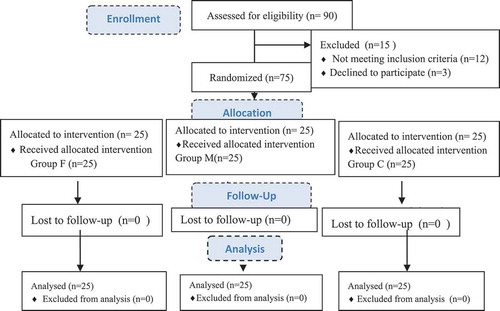
Flow diagram for approached and included patients is shown in . No statistical significance was found in patient characteristics or duration of laryngoscopy () among the three groups.
Table 1. Patient characteristics.
Baseline values for SBP, DBP, HR, and BIS for the three groups were comparable. There was a tendency toward decrease in SBP and DBP following infusion of study drugs and induction of anesthesia p < 0.05 Group C compared to Group F. Significant increase in SBP, DBP, and HR occurred in all three groups following laryngoscopy and intubation p < 0.000 compared to preintubation values. Maximum increase was in first minute postintubation followed by gradual decrease in all three groups (). ΔSBP and ΔDBP postintubation compared to preintubation values shows no significant difference between F and M groups, but p < 0.000 when compared with group C ().
Figure 2. Mean systolic (SBP) and diastolic (DBP) blood pressure over time. ‡ p < 0.05 F vs.C group. *p < 0.000 C vs. F&M groups. §p < 0.05 M vs. C group.
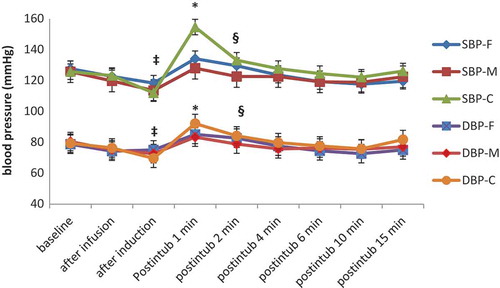
Figure 3. Changes in mean heart rate over time. ‡p < 0.000 M vs F&C groups *p < 0.001 C vs F group. °p = 0.002, ¤ p < 0.001 vs baseline. Inf = infusion, ind = induction, intub = intubation.
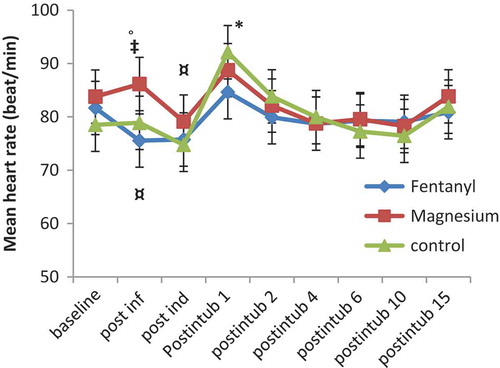
There was a tendency toward decrease in HR following fentanyl infusion p < 0.001 and increase following magnesium p = 0.002 when compared to baseline values. Significant increase in HR occurred after intubation p < 0.000 compared to preintubation in all three groups. Maximum increase was 1 min postintubation followed by gradual decrease (). Changes in HR values (ΔHR) was significantly higher in group C compared to groups F and M, p < 0.000 when preintubation was compared to postintubation values ().
Figure 4. Mean Bispectral index (BIS) values over time. †p < 0.000 F vs M&C group. *p < 0.000 Group C vs F&M groups. Inf = infusion, ind = induction, intub = intubation.
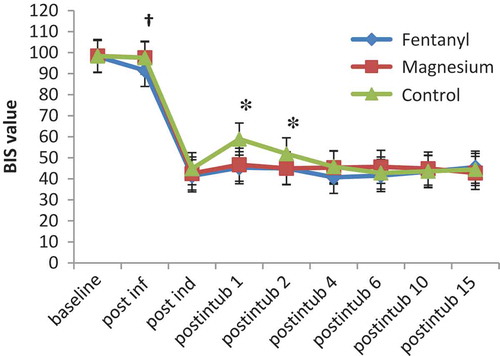
BIS values showed gradual decrease up to induction then significantly increased after intubation in all groups p = 0.000 (). Maximum increase in BIS values were 9.2 ± 2.4%, 9.9 ± 1.9% in F and M groups compared to 31.8 ± 7.8% in group C, p < 0.000 compared to preintubation values ().
Figure 5. (Δ)Maximum change in mean SBP, DBP, HR and BIS compared to preintubation values. §p < 0.000 C vs F&M groups.
Hypertension occurred in 11 patients (44%) in group C. No interventions were required to treat hypertension as it was transient following intubation. No abnormal movement, coughing, tearing, or arrhythmia occurred following laryngoscopy and intubation in any of the groups.
4. Discussion
Results of our study show that fentanyl 2 µg/kg and magnesium sulfate 40 mg/kg infusion over 10 min prior to induction of anesthesia effectively attenuated the hemodynamic and arousal response to laryngoscopy and endotracheal intubation.
Fentanyl maintained stable hemodynamics but did not completely abolish the pressor response to intubation. Similar results were found by Adachi and coworkers [Citation3].
Kautto proposed a graded response, 2 µg/kg fentanyl prior to induction in normotensive patients effectively attenuated the hemodynamic response to intubation while 6 µg/kg completely abolished them [Citation11]. Bruder et al. proposed that the protective effect of fentanyl begins at 2 µg/kg and is maximum at 8 µg/kg [Citation6].
Timing is also important as it was reported that fentanyl requires 10 min to achieve peak effect [Citation12]. To achieve effect-site equilibrium after IV administration of fentanyl and propofol it requires at least 6.4 and 2.9 min, respectively [Citation4]. Therefore, the common mistake of administering narcotics with induction may not be effective due to inadequate dose or just inappropriate timing. Rather, it may explain the drop in blood pressure often seen prior to skin incision.
Magnesium in a dose of 40 mg/kg was also effective in attenuating the pressor response to tracheal intubation. This is partly due to magnesium’s ability to attenuate the increase in plasma norepinephrine and epinephrine levels following endotracheal intubation [Citation9].
Similar results were found by Lee and Kwon [Citation13], where magnesium 45 mg/kg showed better hemodynamic stability and lower bispectral index than 30 mg/kg.
Although in a dose finding study where different doses of magnesium have been studied, Panda et al. [Citation14] suggested 30 mg/kg was the optimal dose compared to 40 and 50 mg/kg. The higher dose led to more episodes of hypotension (30% and 80% in 40 and 50 mg/kg groups, respectively). In our study no significant difference in incidence of hypotension between the groups was noticed. Perhaps because Panda’s study was on hypertensive patients who are known to elicit more excessive hemodynamic response than normotensive patients [Citation3]. Also, maintenance of anesthesia was by propofol infusion which could have contributed to the increased incidence of intraoperative hypotension as 63% of patients who developed hypotension were managed by reduction of propofol infusion only. Hypotension caused by magnesium is due to vasodilation either directly or indirectly through catecholamine inhibition. However, in normotensive patients, significant hypotension does not usually occur due the concomitant increase in cardiac output [Citation15].
Meanwhile, Puri et al. [Citation16] used 50 mg/kg in coronary artery disease patients undergoing coronary artery bypass grafting (CABG). Magnesium effectively attenuated pressor response to intubation without significant increased incidence of hypotension compared to control group. No patients had ST segment depression compared to three in Lidocaine group. This is probably due to its coronary vasodilator properties, which is an added advantage to magnesium use.
HR increased following infusion of magnesium compared to baseline value, although clinically insignificant, which was due to inhibition of acetylcholine release from vagal nerve endings. Similar results were reported in previous studies [Citation17–Citation19] despite different doses used 20, 30, and 60 mg/kg.
No significant hypotension, bradycardia, tachycardia, or arrhythmia requiring treatment occurred probably because drugs were given as infusion as slow administration of magnesium over >10 min reduces incidence of cardiovascular side effects [Citation20].
We insured BIS values below 50 prior to intubation to exclude effect of light anesthesia on hemodynamic response. Both fentanyl and magnesium pretreatment effectively attenuated the arousal response to intubation. Previous studies show fentanyl has a variable effect on BIS when used as sole induction agent but when added to propofol, loss of consciousness occurs at higher BIS values suggesting potentiation [Citation21]. Magnesium also seems to have a potentiating effect on depth of anesthesia. It greatly decreased intraoperative propofol requirement during total intravenous anesthesia [Citation22].
Limitations of this study is that the studied population was normotensive, and we cannot extrapolate the results on hypertensive or elderly patients without further research on this “at risk” group of patients.
5. Conclusion
Magnesium sulfate is a good alternative to fentanyl for attenuation of the hypertensive and tachycardiac response to laryngoscopy and endotracheal intubation, especially in places where narcotics are not readily available.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Xue FS, Zhang GH, Sun HY, et al. Blood pressure and heart rate changes during intubation: a comparison of direct laryngoscopy and a fibreoptic method. Anaesthesia. 2006;61:444–448.
- Rudy EB, Turner BS, Baun M, et al. Endotracheal suctioning in adults with head injury. Heart Lung. 1991;20:667–674.
- Adachi YU, Satomoto M, Higuchi H, et al. Fentanyl attenuates the hemodynamic response to endotracheal intubation more than the response to laryngoscopy. Anesth Analg. 2002;95:233–237.
- Joffe AM, Deem SA. Physiologic and pathophysiologic responses to intubation. In: Benumof and Hagberg’s airway management. 3rd ed. Philadelphia, PA: Elsevier Inc; 2012. p. 193–212.
- Gupta A, Wakhloo R, Gupta V, et al. Comparison of Esmolol and Lignocaine for attenuation of cardiovascular stress response to laryngoscopy and endotracheal intubation. JK Sci. 2009;11:0–3.
- Bruder N1, Ortega D, Granthil C. Consequences and prevention methods of hemodynamic changes during laryngoscopy and intratracheal intubation. Ann Fr Anesth Reanim. 1992;11:57–71.
- Stanley TH. The fentanyl story. J Pain. 2014;15:1215–1226.
- Kim JK, Park JM, Lee C-H, et al. Dose fentanyl injection for blunting the hemodynamic response to intubation increase the risk of reflex bradycardia during major abdominal surgery? Korean J Anesthesiol. 2012;63:402–408.
- James MF, Beer RE, Esser JD. Intravenous magnesium sulfate inhibits catecholamine release associated with tracheal intubation. Anesth Analg. 1989;68:772–776.
- James MF, Cork RC, Dennett JE. Cardiovascular effects of magnesium sulphate in the baboon. Magnesium. 1987;6:314–324.
- Kautto U-M. Attenuation of the circulatory response to laryngoscopy and intubation by fentanyl. Acta Anaesthesiol Scand. 1982;26:217–221.
- Bennett GM. Cardiovascular effects of fentanyl during enflurane anesthesia in man. Anesth Analg. 1979;58:179–182.
- Lee DH, Kwon IC. Magnesium sulphate has beneficial effects as an adjuvant during general anaesthesia for caesarean section. Br J Anaesth. 2009;103:861–866.
- Panda NB, Bharti N, Prasad S. Minimal effective dose of magnesium sulfate for attenuation of intubation response in hypertensive patients. J Clin Anesth. 2013;25:92–97.
- Mroczek WJ, Lee WR, Davidov ME. Effect of magnesium sulfate on cardiovascular hemodynamics. Angiology. 1977;28:720–724.
- Puri GD, Marudhachalam KS, Chari P, et al. The effect of magnesium sulphate on hemodynamics and its efficacy in attenuating the response to endotracheal intubation in patients with coronary artery disease. Anesth Analg. 1998;87:808–811.
- Kothari D, Mehrotra A, Choudhary B, et al. Effect of intravenous magnesium sulfate and fentanyl citrate on circulatory changes during anaesthesia and surgery: a clinical study. Indian J Anaesth. 2008;52:800.
- Mendonça FT, de Queiroz LM, Guimarães CC, et al. Effects of lidocaine and magnesium sulfate in attenuating hemodynamic response to tracheal intubation: single-center, prospective, double-blind, randomized study. Braz J Anesthesiol. 2017;67:50–56.
- Nooraei N, Dehkordi ME, Radpay B, et al. Effects of intravenous magnesium sulfate and lidocaine on hemodynamic variables following direct laryngoscopy and intubation in elective surgery patients. Tanaffos. 2013;12:57–63.
- Do SH. Magnesium: a versatile drug for anesthesiologists. Korean J Anesthesiol. 2013;65:4–8.
- Barr G1, Anderson RE, Owall A, et al. Effects on the bispectral index during medium-high dose fentanyl induction with or without propofol supplement. Acta Anaesthesiol Scand. 2000;44:807–811.
- Telci L, Esen F, Akcora D, et al. Evaluation of effects of magnesium sulphate in reducing intraoperative anaesthetic requirements. Br J Anaesth. 2002;89:594–598.