ABSTRACT
Background: Increased intracranial pressure (ICP) is a serious problem that may potentially cause significant neurological complications. Multiple means of assessment have been used to identify patients with increased ICP. These methods are invasive, sophisticated and time-consuming, whilst optic nerve sheath diameter (ONSD) by ultrasonography is postulated as a non-invasive, fast and accurate measure to diagnose increased ICP.
Patients and methods: A cross-sectional study was performed on 20 ASA physical status I and II female patients undergoing elective gynecological laparoscopic surgeries requiring pneumoperitoneum and Trendelenburg positioning. We investigated the change in ONSD in response to the change in positional change as well as to pneumoperitoneum in order to assess their effect on ICP in laparoscopic surgeries.
Results: An analysis of variants comparing values of ONSD at different time points demonstrated that sagittal and transverse ONSD in both right and left eyes were significantly higher at all time points except for the time of assessment, after induction and at 30 min after extubation, all of which were statistically non-significant compared to baseline values. It also showed that, although values of ONSD after induction were non-significantly different from baseline, they rose significantly after insufflation and did not return to baseline until 30 min after extubation.
Conclusion: ONSD is an accurate noninvasive modality for the assessment of raised ICP by ocular sonography. We recommend that duration and positioning should be optimized for such prolonged surgery in the Trendelenburg position.
1. Introduction
The laparoscopic approach has become a common technique for many types of surgical procedures, including gynecology, general surgery, and urology. Gas insufflation causing pneumoperitoneum (PP) and increased intra-abdominal pressure (IAP) can have many systemic physiological consequences such as decreased venous return, cardiac output, increased heart rate, mean arterial pressure, and systemic vascular resistance. Moreover, carbon dioxide (CO2) gas insufflation can cause hypercapnia and respiratory acidosis due to the absorption of the gas across the peritoneal surface. [Citation1,Citation2]
The effects on the respiratory and cardiovascular system are usually mild and well-tolerated. Moreover, some authors have documented severe neurological complications during laparoscopy. [Citation3,Citation4] These studies have attributed neurological deficits to cerebral ischemia and cerebral edema, related to increased ICP.
Suitable surgical exposure in gynecological laparoscopic surgeries requires a steep head-down position, up to 30-degree Trendelenburg position (TP) to facilitate the procedure and maintain adequate visualization. In this position, there is a remarkable reduction in pulmonary compliance and increase peak airway pressures due to cephalad movement of the diaphragm and abdominal contents as well as increases venous return and pulmonary capillary wedge pressure (PCWP), which prevents the decline in cardiac output (CO) after abdominal insufflation [Citation1].
In general, the effect of IAP and Trendelenburg position on ICP cannot be easily determined intraoperatively, but there is increasing evidence that reveals a positive correlation between increased IAP and ICP [Citation5]. Unfortunately identifying the effect of PP and the TP on ICP cannot be easily determined during surgical procedures because of possible complications of invasive ICP monitoring. Therefore, during laparoscopic surgery in patients with a risk of developing intracranial hypertension, a non-invasive method to monitor ICP would be necessary [Citation6]. The mechanisms of increase of ICP during laparoscopic surgeries are most probably as follows: increased IAP, Imbalance between CSF absorption and CSF drainage of the lumbar venous plexus, higher pressure in the vascular network of sacral spaces, Trendelenburg position, and cerebral vasodilation due to hypercarbia [Citation7]. In 2014 an important study was performed on laparoscopic surgeries, demonstrating that ICP was linearly increased up to 25 mmHg measured invasively by ventriculoperitoneal shunt placement. [Citation8]
The optic nerve sheath is an anatomical extension of the dura mater and the subarachnoid space around the optic nerve is continuous with the intracranial subarachnoid space. Any pressure rises within the intracranial compartment impacts on the optic nerve head as swelling of the optic disc and papilledema. Papilledema develops over time, maybe a late sign and requires a trained physician for accurate documentation. Increase ONSD shows earlier manifestation of increased ICP. [Citation9]
Promising research shows that ocular U/S can detect increased ICP non-invasively. If the CSF pressure increases, the retrobulbar segment of the ONS which is enclosed by a distensible subarachnoid space can inflate. [Citation10] ONS measurement using ocular sonography has been performed for more than 10 years.
As regards the comparison of ONSD with invasive ICP monitoring, the literature shows a wide variation in optimal values between 4.8 and 5.9 mm. Alternatively, when MRI scans in healthy subjects were used to assess accuracy, OSND was found to have levels as high as 6.4 mm. [Citation11]
In a previous study on 585 Korean healthy volunteers Kim and his colleagues [Citation12] measured the optic nerve sheath diameter and studied its association with eyeball transverse diameter, they demonstrated that ONSD ranged from 3.30 mm to 5.20 mm, and 95% subjects revealed a mean ONSD in the range of 4.09 mm to 4.14 mm, and there was no significant difference in ONSD between the right and left eyes. They also found that there was a strong correlation between ONSD and eyeball transverse diameter ETD is the first to establish a normal value for the ONSD/ETD ratio using ultrasonography. They also suggested that an ultrasound measurement of the ONSD/ETD ratio could be the more accurate and helpful marker of elevated ICP compared with ONSD alone and recommended further studies.
A valuable study on ultrasonographic measurement of ONSD during robot-assisted laparoscopic radical prostatectomy with steep Trendelenburg positioning revealed that there was a 12.5% increase in ONSD consistently with increased ICP. [Citation13]
However, few studies on changes of ONSD according to the positional change during laparoscopic surgeries of short procedure time have been reported. We hypothesized that if ICP during pneumoperitoneum in gynecological laparoscopic surgeries is increased according to the position, ONSD would likewise be increased.
2. Patient and methods
The target population was female patients ASA I & II who were undergoing elective laparoscopic gynecological surgeries (hysterectomy) taking approximately 2 h with a 30° Trendelenburg position. The patients had no history of any neurological disorder, risk factors for high ICP, coagulopathy or concurrent treatment with anticoagulant drugs. Our study commenced after obtaining approval from the hospital ethics committee and taking written informed patient consent. The study was carried out on 20 patients at Suez Canal University Hospital. Our primary objective was studying the effect of pneumoperitoneum and Trendelenburg position (30° incline) on ICP as measured by U/S ONSD to detect increased ICP non-invasively and recognize symptoms of increased ICP postoperatively.
The sample size is calculated from this equation: [Citation14]
N = 2 δ2 (Zα + Zβ) 2/∆2 Where– N = the number of the subject of each group.
Zα = the value of standard normal distribution for p-value 5% for a two-sided test = 1.96. Zβ = the value of a standard normal for the desired statistical power 90% and it equals 1.28
∆ = the detectable difference between the mean values of optic nerve sheath diameter 10 min after induction of general anesthesia in the supine position [4.8 mm] and 10 min after 30-degree Trendelenburg positioning with CO2 pneumoperitoneum [5.4 mm] and it equals 0.6 mm. [Citation13]
δ = the highest within-group standard deviation of 0.5.
By calculation: N = 14.5 and as we expected a drop out of 15% these were added with a total of 20 patients for each group.
3. Pre-operative assessment
The patient’s age, BMI, and ASA status were recorded. The patients were clinically assessed by a complete physical examination and investigations.
4. Intra-operative measures
No premedication was given to patients, they were just reassured, and the procedure was explained. The whole technique and anesthetic procedures were performed by the same anesthesiologist to avoid variations in skills. A 20-gauge cannula was inserted into the forearms of all patients. Airway devices, the anesthesia machine, ventilator, flowmeters, and equipment were checked before induction. Routine monitoring equipment (Datex-Ohmeda™) was attached to the patients including 5-lead ECG, non-invasive blood pressure and pulse oximetry. Baseline hemodynamic data were charted. Measures to maintain body temperature was taken to avoid inadvertent intraoperative hypothermia. Preparation for general anesthesia and resuscitation drugs was prepared.
The patients were pre-oxygenated for 3 min, general anesthesia was induced by 1 mcg/kg Fentanyl, 2 mg/kg propofol and 0.5 mg/kg atracurium. After confirmation of adequate anesthesia, endotracheal intubation was performed, and a morphine bolus of 0.15 mg/kg was given. Maintenance of anesthesia was done by isoflurane 1–2.5% in air/oxygen adjusted for patient MAC 50 for age. Top-up doses of atracurium 0.1 mg/kg 20–45 min after the initial dose to maintain the neuromuscular block were given. Ventilator settings were standardized, with pressure-controlled ventilation mode, and ventilation was adjusted to deliver a tidal volume of 6–8 ml/kg by setting Peak Inspiratory Pressure (PIP) 30 cm H2O. The respiratory rate (RR) was set at 12/minute with an inspiratory-to-expiratory ratio of 1:2. The RR was adjusted to maintain the end-tidal CO2 between 35 and 40 mmHg.
5. Optic nerve sheath diameter assessment
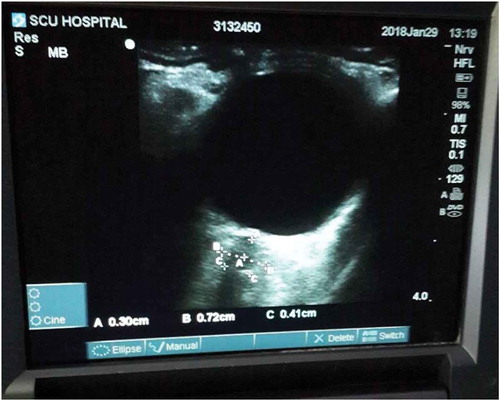
The patient was placed in a supine position. A thick layer of gel was applied over the closed upper eyelid. The 7.5-MHz linear probe was placed only on the gel in the temporal area of the eyelid, not on the eyelid itself, to prevent pressure being exerted on the eye. The placement of the probe was adjusted to give a suitable angle for displaying the entry of the optic nerve into the globe. The two-dimensional mode was used, and ONSD was measured 3 mm behind the globe using an electronic caliber and an axis perpendicular to the optic nerve. For each eye, two measurements were made, one in the sagittal plane and the other in the transverse plane by rotating the probe clockwise .
Figure 1. U/S image of ONSD measurement. It shows the U/S measurement of op in centimeters. The caliper “A” measures the depth at which the ONSD must be measured (3 mm). “B” measures the ONSD (7.2 mm) at this depth.
This process was carried out 8 times:
1st Baseline
2nd After induction in the supine position.
3rd 5 min just after abdominal insufflation and Trendelenburg position.
4th 15 min after insufflation.
5th 30 min after insufflation.
6th just before extubation in the supine position again.
7th just after the extubation
8th 30 min after the extubation.
The process of abdominal insufflation with CO2 was carried out with precautions not to exceed a pressure of insufflation re than 16 mm Hg and EtCO2 not to increase more than 40 mm Hg to exclude hypercarbia.
6. Recordings and measurements
ONSD was assessed in eight Timings.
Patients mean arterial pressure (MAP), heart rate (HR) and end-tidal carbon dioxide (EtCO2) were recorded with each ONSD reading.
Symptoms of increased intracranial pressure were observed and recorded postoperatively such as Behavior changes, disturbed level of consciousness, headache, lethargy, neurological symptoms, including weakness, numbness, eye movement problems, and double vision, seizures, nausea &vomiting, drowsiness, and ocular palsies.
7. Results
This prospective observational study included 20 female patients undergoing elective laparoscopic hysterectomies in Suez Canal University Hospital. All patients’ ages ranged from 18 to 60 with a mean of 30 years while their body mass index (BMI) was about 30 kg/m2. ()
Table 1. Demographic characteristics of the study patients and intraoperative data.
As demonstrated in , the optic nerve sheath sagittal and transverse diameters were non-significantly different in both right and left eyes at all time points. Post hoc analysis for repeated measures ANOVA comparing readings at different time points showed that sagittal and transverse ONSD in both right and left eyes were significantly higher at all time points (p value <0.05) except for changes after induction and 30 min after extubation which was statistically non-significant compared to baseline values. It also demonstrated that although readings after induction were non-significantly different than baseline, sagittal and transverse ONSD in both right and left eyes rose up significantly after insufflation and did not return to non-significantly different values until 30 min after extubation. Also, readings at 30 min after the insufflation time point was significantly higher than all-time points (p value <0.05) except for changes 15 min after insufflation.
Table 2. Comparison between optic nerve sheath sagittal and transverse diameters in both right and left eyes at different time points.
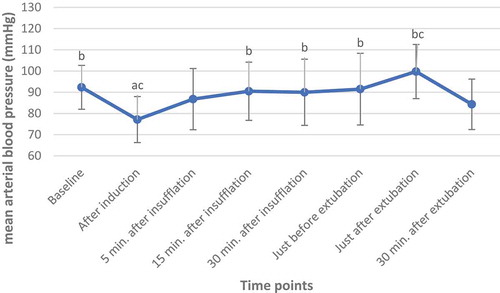
shows that mean arterial blood pressure (MAP) readings were significantly different among various time points. Post hoc analysis for repeated measures ANOVA comparing readings at different time points showed that mean arterial blood pressure was significantly lower only immediately after induction (p value <0.05) compared to baseline values. However, mean arterial blood pressure after induction was significantly lower than all readings at different time points. Also, MAP just after extubation was significantly higher than at 30 min after insufflation time points (p value <0.05).
Graph 1. Comparison of mean arterial blood pressure (MAP) at different time points.
aP value for Post Hoc test (LSD) compared to baseline time point bP value for Post Hoc test (LSD) compared to after induction time point cP value for Post Hoc test (LSD) compared to 30 min after insufflation time point
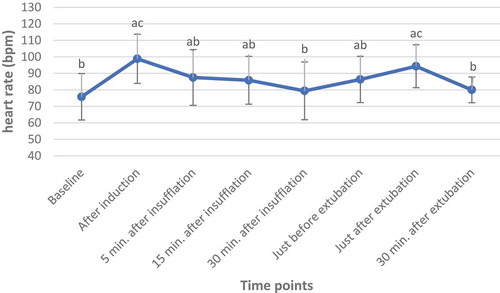
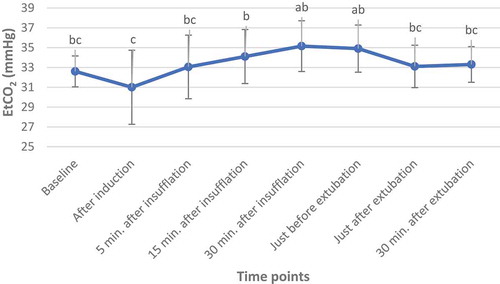
Heart rate readings were significantly different among various time points. Post hoc analysis for repeated measures ANOVA comparing readings at different time points showed that heart rate was significantly higher in all time points (p value <0.05) compared to baseline values except for 30 min after insufflation and 30 min after extubation. Also, the heart rate after induction was significantly higher than all readings at different time points except just after extubation. Moreover, the heart rate at 30 min after the insufflation time point was significantly lower than after induction and just after extubation (p value <0.05). () demonstrates that, as regard end-tidal partial pressure of CO2 (EtCO2) readings, it was significantly different among various time points. Post hoc analysis for repeated measures ANOVA comparing readings at different time points shows that end-tidal partial pressure of CO2 (EtCO2) was significantly higher at 30 min after insufflation and just before extubation (p value < 0.05) compared to baseline values. However, the end-tidal partial pressure of CO2 (EtCO2) at all different time points, except for baseline, was significantly higher than after induction. Additionally, EtCO2 at 30 min after insufflation time points was significantly higher than readings at all time points except at 30 min after insufflation and just before extubation time points (p value <0.05). ()
Graph 2. Comparison of Heart rate at different time points.
aP value for Post Hoc test (LSD) compared to baseline time point bP value for Post Hoc test (LSD) compared to after induction time point cP value for Post Hoc test (LSD) compared to 30 min after insufflation time point
Graph 3. Comparison of end-tidal partial pressure of CO2 (EtCO2) at different time points.
aP value for Post Hoc test (LSD) compared to baseline time point bP value for Post Hoc test (LSD) compared to after induction time point cP value for Post Hoc test (LSD) compared to 30 min after insufflation time point
All the predictable postoperative complications that were observed in this study were statistically non-significant except for nausea which occurred only in 10% of patients.
8. Discussion
The laparoscopic approach has become a common technique for many types of surgical procedures, including gynecology, general surgery, and urology. During gas insufflation [pneumoperitoneum (PP)], increased intra-abdominal pressure (IAP) can cause decreased venous return, cardiac output, increased heart rate, mean arterial pressure, and systemic vascular resistance Moreover, carbon dioxide (CO2) gas insufflation can cause hypercapnia and respiratory acidosis due to absorption of the gas across the peritoneal surface [Citation1,Citation2]. The effects on the respiratory and cardiovascular system are usually mild and well-tolerated.
Moreover, there have been reports of severe neurological complications with laparoscopies [Citation3,Citation4]. These studies have attributed neurological deficits to cerebral ischemia and cerebral edema, related to increased ICP. In the context of patients at an increased risk to develop intracranial hypertension, but for whom laparoscopic surgery is indicated, monitoring ICP non-invasively would be preferable. One proposed method that would allow early detection of elevated ICP is non-invasive ocular ultrasonography.
In our study, repeated measures ANOVA comparing values of ONSD at different time points showed that there was no significant difference in ONSD between the right and left eyes but sagittal and transverse ONSD in both right and left eyes were significantly higher at all measured points, with the exception of assessment after induction and at 30 min after extubation. These latter values did not differ significantly from baseline values. It also showed that although values of ONSD after induction were non-significantly different than baseline, sagittal and transverse ONSD in both right and left eyes rose up significantly after insufflation and did not return to non-significantly different values until 30 min after extubation. Also, readings at 30 min after the insufflation time point were significantly higher than all time points (p value <0.05) except for changes 15 min after insufflation.
Similarly, Chiara Robba et al. [Citation15] in their landmark study in which they assessed the effects of pneumoperitoneum and Trendelenburg position on intracranial pressure using various non-invasive methods concluded that all non-invasive methods evaluated in their study demonstrated increased ICP when TP was in combination with PP. They also concluded that patients undergoing this kind of laparoscopic surgery who needed TP and PP should be counseled about the risks of intracranial hypertension.
In 2018 Chhavi et al. [Citation16] performed a prospective, observational, non-interventional and open study. They measured the ONSD of 30 patients undergoing robotic/laparoscopic pelvic surgeries in steep Trendelenburg position lasting more than 4 h (Group I) and compared them with 30 patients undergoing donor hepatectomy in supine position without Trendelenburg position (Group II). A significant increase in ONSD in prolonged steep Trendelenburg position with pneumoperitoneum was observed. They concluded that the magnitude of increase was not enough to be labeled as intracranial hypertension and that ONSD was a good noninvasive modality for assessment of raised ICP secondary to cerebral edema. It may be used to initiate timely interventions.
Similar to our study, in 2018 nine observational studies and one randomized controlled trial, with a total of 460 subjects, were analyzed. ONSD was found to be significantly increased in the early and late periods in comparison to baseline results. ONSD during early and late periods did not significantly change with time. ONSD values in both the early period (0–30 min) and late period (30–120 min) of CO2 pneumoperitoneum were significantly greater than those after anesthesia induction. These changes in ONSD seemed to be a reversible phenomenon during laparoscopic procedures, given that ONSD returned to its original level after CO2 desufflation [Citation17].
Another study in 2014 by Verdonck P et al. [Citation18] carried out on 20 patients ASA I-II demonstrated contradicting results during Robot-Assisted Laparoscopic Radical Prostatectomy (RALRP). ONSD was assessed at many different times. Cerebral perfusion pressure (CPP) was determined by subtracting central venous pressure (CVP) from the mean arterial (MAP) minus. There was no significant change in ONSD with the head-down position, despite the finding that there was an average increase in CVP from 4.2 mm Hg to 27.6 mm Hg. The CPP always dropped after 70 min of the Trendelenburg position and continued to stay at a lower level until 15 min after returning to the supine position but remained above 60 mm Hg. The lack of an increase in ONSD during head-down positioning and pneumoperitoneum contradicts previous findings of increased ICP in these situations. These findings demonstrate the increase in intracranial blood volume is not significant enough that CSF migration as a compensatory mechanism becomes exhausted, suggesting that any increases in ICP are likely to be small. It was documented that near 10 patients undergoing this study were hypertensive, so cerebral autoregulation is already adjusted to elevated blood volume without ICP change.
Regarding the end-tidal partial pressure of CO2 (EtCO2), it was significantly higher at 30 min post-insufflation and just before extubation compared to baseline values. However, EtCO2 at all different time points, except for baseline, was significantly higher than after induction. Moreover, EtCO2 at 30 min after insufflation time points was significantly higher than values at all time points except at 30 min after insufflation and just before extubation time points.
Our results as regard EtCO2 were similar to Kim’s results [Citation13] in which the EtCO2 and PaCO2 increased significantly after CO2 pneumoperitoneum in comparison with the baseline values without neurological complications.
Dinsmore and his colleagues in a recent research study carried out on healthy volunteers assessed the effects of acute controlled changes in EtCO2 on the diameter of the optic nerve sheath and demonstrated that the ONSD changes rapidly with increases in PETCO2 and returns to baseline. [Citation19]
Similarly, Chiara Robba et al. [Citation15] found that end-tidal CO2 was significantly increased after PP and after PP in TP compared to baseline (B): B versus PP; B versus TP+PP, but the application of Trendelenburg position itself did not significantly increase ETCO2 (PP versus TP+PP). After PP deflation and in the supine position, ETCO2 had similar values compared to baseline, and it was significantly decreased compared to values found after PP or PP in TP.
Regarding arterial blood pressure in our study repeated measures ANOVA comparing readings at different time points, show that mean arterial blood pressure was significantly lower only immediately after induction compared to baseline values. However, there was a significantly lower arterial blood pressure after induction compared to values at different time points. Also, MAP just after extubation was significantly higher than at 30 min and after insufflation time points. Similar to our results, Chiara Robba and his colleagues found that MAP at the end of the procedure was significantly lower compared to all the other time points;, but compared to baseline, it did not change significantly during PP or Trendelenburg position. The application of the Trendelenburg position itself did not significantly increase ABP.
Regarding postoperative symptoms in our study, only two patients developed nausea; other symptoms related to increased intracranial pressure were fortunately absent. A case report in 2014 documented a 51-year-old female with cervical cancer who underwent a robotic-assisted radical hysterectomy. Operative complications led to a prolonged procedure. After elective ventilation and sedation postoperatively, there was difficult extubation on day 2. Because of persistent agitation, a brain CT was performed where cerebral edema was discovered. [Citation20] Another example of how prolonged surgery in a head-down position may lead to cerebral edema was reported with two patients who underwent robotic radical cystectomy and experienced neurological deterioration after extubation. The researcher had interesting recommendations about this kind of procedure they suggest adjusting duration and positioning during prolonged surgery in a steep head-down position. [Citation3]
Other studies, even those with results that were significant regarding ONSD, pneumoperitoneum and TP, denied the presence of post-operative symptoms of increased ICP, such as that conducted by Kim et al. [Citation13] Twenty patients undergoing elective RALRP were included in this study, ONSD and regional cerebral oxygen saturation (rSO2) were measured via ocular ultrasonography and near-infrared spectroscopy. There were no reports of neurological complications or decreased rSO2 in these patients.
There are some limitations in this study: sample size should be larger to make the study stronger. Larger multicenter studies are essential to support our results. We conducted this study only in gynecological cases. Additionally, urological operations use steep Trendelenburg position in radical-assisted laparoscopic prostatectomies. During such operations, to decrease the risk of intracranial pressure increase, we should limit the time of steep Trendelenburg, the amount of fluids infused, the intra-abdominal insufflation pressure to 8 mm Hg and the operative time when possible.
9. Conclusion
Trendelenburg positioning causes an increase in ICP. It can be monitored easily by ocular sonography which measures the changes in ONSD to detect raised ICP, and it has been shown that very small increases in the sonographic ONSD correspond to increased ICP. This early recognition of raised ICP has great value so management can be initiated in order to lower ICP. In our study ONSD in both right and left eyes rose significantly after insufflation and did not return to non-significantly different values until 30 min after extubation. The measurement of ONSD by ocular ultrasound is easy to master, quick, and, most importantly, is a noninvasive technique that can be performed in any patient position. It does not involve extra cost as most operating rooms are equipped with point of care ultrasound machines.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Tamara A, George G, Brandson T, et al. Cardiovascular and ventilatory consequences of laparoscopic surgery. Circulation. 2017;135:700–710.
- Neudecker J, Sauerland S, Neugebauer E, et al. The European Association for Endoscopic Surgery clinical practice guideline on the pneumoperitoneum for laparoscopic surgery. SurgEndosc. 2002;16(7):1121–1143.
- Pandey R, Garg R, Darlong V, et al. Unpredicted neurological complications after robotic laparoscopic radical cystectomy and ileal conduit formation in steep Trendelenburg position: two case reports. ActaAnaesthesiolBelg. 2010;61(3):163–166.
- Danic MJ, Chow M, Alexander G, et al. Anesthesia considerations for robotic-assisted laparoscopic prostatectomy: a review of 1,500 cases. J Robot Surg. 2007;1(2):119–123.
- Robba C, Bacigaluppi S, Cardim D, et al. Non-invasive assessment of intracranial pressure. Acta Neurol Scand. 2015;32:1587–1597.
- Ficarra V, Novara G, Artibani W, et al. Retropubic laparoscopic and robot assisted radical prostatectomy: a systematic review and cumulative analysis of comparative studies. EurUrol. 2009;55(5):1037–1063.
- Halverson A, Buchanan R, Jacobs L, et al. Evaluation of mechanism of increased intracranial pressure with insufflation. SurgEndosc. 1998;12:266–269.
- Kamine TH, Papavassiliou E, Schneider BE. Effect of abdominal insufflation for laparoscopy on intracranial pressure. JAMA Surg. 2014;149(4):380–382.
- Hansen HC, Helmke K. Validation of the optic nerve sheath response to changing cerebrospinal fluid pressure: ultrasound findings during intrathecal infusion tests. J Neurosurg. 1997;87:34–40.
- Liu D, Kahn M. Measurement and relationship of subarachnoid pressure of the optic nerve to intracranial pressures in fresh cadavers. Am J Ophthalmol. 2000;116:548–556.
- Geeraerts T, Launey Y, Martin L, et al. Ultrasonography of the optic nerve sheath may be useful for detecting raised intracranial pressure after severe brain injury. Intensive Care Med. 2007;33:1704–1711.
- Kim D, Jun J, Kim R. Ultrasonographic measurement of the optic nerve sheath diameter and its association with eyeball transverse diameter in 585 healthy volunteers. Sci Rep. 7:15906..
- Kim MS, Bai SJ, Lee JR, et al. Increase in intracranial pressure during carbon dioxide pneumoperitoneum with steep Trendelenburg positioning proven by ultrasonographical measurement of optic nerve sheath diameter. J Endourol. 2014;28:801–806.
- Greenberg RS, editor. Estimation of sample size requirements for randomized controlled clinical trials. Medical Epidemiology. 2nd ed. Harcourt Brace and company; McGraw Hills Publishing Company; 1996.
- Robba C, Cardim D, Donnelly J, et al. Effects of pneumoperitoneum and Trendelenburg position on intracranial pressure assessed using different non-invasive methods. Br J Anaesth. 2016 Dec;117(6):783–791.
- Chhavi G, Rajat G, Purnima D, et al. Evaluation of optic sheath diameter as a guide for raised intracranial pressure in patients undergoing prolonged laparoscopic robotic surgeries in steep trendelenburg position. IJSR. 2018;7:154–159.
- Kim EJ, Koo BN, Choi SH, et al. Ultrasonographic optic nerve sheath diameter for predicting elevated intracranial pressure during laparoscopic surgery: a systematic review and meta-analysis. SurgEndosc. 2018;32:175.
- Verdonck P, Kalmar AF, Suy K, et al. Optic nerve sheath diameter remains constant during robot-assisted laparoscopic radical prostatectomy. PLoS ONE. 2014 Nov 4;9(11):e111916.
- Dinsmore M, Han S, Fisher J, et al. Effects of acute controlled changes in end-tidal carbon dioxide on the diameter of the optic nerve sheath: a transorbital ultrasonographic study in healthy volunteers. Anaesthesia. 2017;72:618–623.
- Barr C, Madhuri T, Prabhu P, et al. Cerebral edema following robotic surgery: a rare complication. Arch Gynecol Obstet. 2014;290:1041–1044.
