ABSTRACT
Background: The aim of this study is to investigate that combinig Lumbar paravertebral block and GA decreases postoperative pain, blood loss and the need for hypotensive drugs.
Methods: After ethical committee approval. A randomized, controlled; double-blinded study registered (NCTR 03422354). The study was conducted in Cairo university hospital from 15/02/2018/to 21/06/2018.
Seventy-four patients were randomly allocated into two groups using computerized generated random tables: Group P: 37 patients received single-shot L1-L2 paravertebral block before GA. And Group G: 37 patients received GA. The primary outcome was the required dose of hypotensive drugs in both groups.
Results: There were no statistical differences in hypotensive drug requirements between both groups. On the other hand, there were remarkable differences in all analgesics that were used in both groups as the total doses were much less in the group (P) than in the group (G).
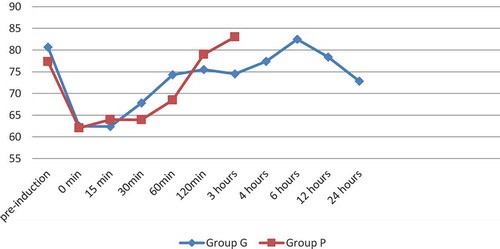
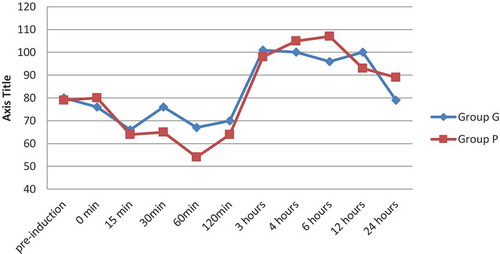
There was a statistically significant decrease in both MBP and HR in the group (P) in 30, 60 and 120 min after induction of anesthesia.
Group P showed a lower level of VAS with statistical differences in the first 30 min after recovery and the subsequent 4 h (2 and 4). After 4 h the VAS was low in both groups and was noncomparable between the two groups.
Conclusion: U/S guided L1/L2 PVB produces proper intraoperative hemodynamic control. It is also a safe and excellent alternative of analgesia that decreases the perioperative opioids requirements. However, there were no difference in the total dose of hypotensive drugs and the total blood loss.
1. Background
Nowadays, there is an increase in the rate of hip joint replacement surgeries. Because of the patient age group (geriatric), comorbidities and postoperative pain management, these type of surgeries rise up a challenge to the anesthetist [Citation1].
There is a debate whether to give general anesthesia or regional anesthesia. The former provides hemodynamic stability, excellent airway control, and patient comfort. On the other hand, the later provides effective pain control, earlier mobilization and potentially low risk of complication such as deep venous thrombosis or bleeding [Citation1,Citation2] another attractive choice is to combine both techniques to have the advantages of both techniques but at the cost of more complications. Peripheral nerve blocks, as a regional modality, are an attractive choice that could achieve a better profile of analgesia with fewer incidences of complications. Lumbar plexus block (LBP) and psoas compartment were tried in hip surgeries and end in perfect results in postoperative period regarding the pain scale and analgesic requirement [Citation3–Citation6].
Lumbar Para-vertebral block (LPB) in a combination with general anesthesia potentially will provide better surgical conditions and less postoperative pain. Moreover, hypothetically it will decrease the blood loss and the need for hypotensive drugs intra-operatively.
In this study, we hypothesize that combined general anesthesia with lumbar paravertebral block will provide better intra- and post-operative outcomes regarding the need for hypotensive drugs, hemodynamics, bleeding and postoperative pain than general anesthesia alone.
2. Methods
After approval of the Ethics commitee (N-37-2017), this is a randomized, controlled; double-blinded study registered in the national clinical trial registry under a number of NCTR 03422354. The study was conducted in Cairo university hospital (orthopedic operating room) from 15/02/2018/to 21/06/2018 after approval of the ethical committee (N-73-2017).
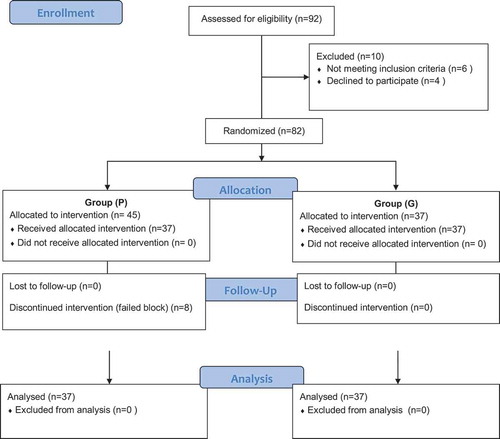
Seventy-four patients scheduled for elective hip surgery were included in the study after a detailed description and signing a detailed informative consent (). The patients were randomized to two groups using a computer-generated list and kept in a sealed envelope into two groups:
Group P: 37 patients were received single-shot L1-L2 paravertebral block before undergoing general anesthesia (GA).
Group G: 37 patients were received GA.
Patient selection was based on the following inclusion criteria: age from 20 to 60 years, male or female and ASA I–II. On the other hand, patients who known to be allergic to local anesthetic, infection at the puncture site, coagulopathy (INR > 1.5, <12 h post-LMWH, thrombocytopenia less than 100,000/ml or history of bleeding tendency disease), sepsis and pre-existing neurologic disease were excluded from the study.
Patients were assessed clinically and a thorough examination was done. Moreover, full labs were requested to assess eligibility (complete blood count (CBC), prothrombin time and concentration (PT& PC), partial Thromboplastin Time (PTT); kidney and liver function tests).
All patients were admitted to the operating room and full monitoring was connected (ECG, NIBP, pulse oximetry) intravenous access (IV) was inserted and IV crystalloid (15 ml/kg) was given as a preload, nasal oxygen was connected and sedation was given in the form of 2 mg midazolam.
Those patients who were assigned in group P (Paravertebral block group) were positioned laterally and bending with the side to be blocked upward.
Using an ultrasound machine (8–14 MHz curved array probe in Siemens ACUSON X300 Ultrasound System), the level between the transverse process of L1 and L2 and the depth was identified and a skin wheal was raised using lidocaine 1%. Then, a 22 G Touhy needle 8 cm length (Perifix Epidural Needle) was advanced via an out of the plane approach to hitting the transverse process then was moved up or down, without ultrasound, to reach the paravertebral space. Space was identified by loss of resistance to normal saline. The depth was watched correlated as expected by ultrasound, and then 20 ml of Bupivacaine 0.25% was injected after negative aspiration. The success of the block was approved if a loss of sensation to a pin-prick was determined at the dermatomes distribution of L1-L4 roots. Those patients who were assigned to group G were also having the same position and sterilization. Using the ultrasound machine and probe, saline was injected and sensory examination was done to ensure blindness to the patients.
The patient then was shifted to the operating room and general anesthesia was conducted. All patients in the study received general anesthesia after being attached to routine monitoring (ECG, NIBP, pulse Oximetry and Capnography). Propofol 2 mg/kg, atracurium 0.5 ml/kg, fentanyl 100 µg were used in induction; the endotracheal tube was inserted, checked and fixed then the patient was connected to the mechanical ventilator and ventilated.
The anesthesia was maintained using Isoflurane 1.2% and 10 mg atracurium every 20 min.
Systolic blood pressure was taken preoperative as a baseline value, intra-operative after induction of anesthesia, 15, 30, 60, 120, 180 min and then postoperative after 2, 4, 6, 12, 24 h.
The target of the mean blood pressure was to be more than 50 mm Hg while the systolic pressure to be between 80 and 100 mm Hg and the diastolic blood pressure targeted to be 50 to 70 mmHg. To achieve these targets of blood pressure the following drugs were used in the following protocol:
First line is propranolol (0.5 then 1 mg intravenous slowly over 10 min) if blood pressure was not controlled by propranolol or if contraindicated such as in patients with a history of bronchial asthma or heart block then the second line is Nitroglycerine intravenous infusion (starting from 0.5 µg/kg/min and increased slowly to reach a maximum of 20 µg/kg/min if needed) started the infusion rate with 0.5 µg/kg/min and the rate increased according to blood pressure.
Fentanyl increments of 50 µg were used intra-operatively as analgesia and the total dose required was recorded. Moreover, all intra-operative medications that were given were recorded in both groups.
Post-operative pain was assessed and recorded using visual analogue scale (VAS) after 30 min, 2 h, 4 h, 6 h, 8 h, 12 h and 24 h. If VAS was ranging from 0 to 2 nothing was given, if ranging from 3 to 5 Paracetamol 1-g slow intravenous infusion was used (the maximum daily dose of 4 g/24 h), and if the VAS level is more than 5 we used Pethidine (1 mg/kg intramuscular).
The primary outcome of this study was the required dose of hypotensive drugs in both groups. While the secondary outcome parameters were the total dose of opioids, pain assessment by the aid of visual analogue scales (VAS) and the need for intraoperative blood transfusion.
This study was double-blinded to both the patient and the researcher. This was achieved by assign different physicians. The physician who gave the regional block was different from the one who conduct general anesthesia or who follow-up the patient intraoperative or post-operative.
2.1. Statistical analysis
Categorical variables were presented as counts and percentages, represented graphically using tables and bar charts, and analyzed using Fisher’s exact test. Metric variables were summarized using mean ± SD, represented graphically using box plots and analyzed using the unpaired t-test or mixed ANOVA for variables with repeated measures. P-values less than 0.05 were considered significant. All analyses were done using IBM SPSS v.24.
Categorical variables were presented as counts and percentages, were represented graphically using tables and bar charts, and were analyzed using Fisher’s exact test. Metric variables were summarized using mean ± SD, were represented graphically using box plots and were analyzed using the unpaired t-test or mixed ANOVA for variables with repeated measures. P-values less than 0.05 were considered significant. All analyses were done using IBM SPSS v.24.
2.2. Sample size
Using the primary outcome of the required doses of hypotensive drugs, the power analysis was performed using student t-test based on a previous study [Citation7] that reported a dose of 0.8 mg nitroglycerin as a mean with a standard deviation 0.231. We assumed that 30% reduction of the total dose has a clinical significance between the two groups and for a power of 0.8 and an alpha error of 0.05, a minimum sample size of 66 patients (33 in each group) was calculated for each group. Expecting 12% of drop out, the sample size was increased to 74 patients (37 in each group)
3. Results
Ninety-two patients were assessed for eligibility, 82 of them were eligible and randomized to either group P or G.37 patients were assigned to group G while 45 patients were assigned to group P 8 of them were dropped out because of failed block while 37 were retained in the study till the end in this group (P) ().
Regarding the demographic data and duration of surgery, there were no statistical differences between both groups regarding age, sex and duration of surgery ().
Table 1. Age, gender, and duration of surgery
Regarding the hypotensive drugs doses (propranolol and nitroglycerin) there were no statistical differences between both groups. On the other hand, there were remarkable differences with p-value <0.05 in all analgesics that were used in both groups as the total doses were much less in the group (P) than in the group (G). ()
Table 2. Drug dosages
Regarding the vital signs, there was a statistically significant decrease in both mean blood pressure and heart rate in the group (P) in30, 60 and120 min after induction of anesthesia with p-value <0.05 ( and ).
Regarding the visual analogue scale (VAS), Group P showed a lower level of VAS with statistical differences in the first 30 min after recovery and the subsequent 4 h (2 and 4) with a p-value less than 0.05 (). After 4 h the VAS was low in both groups and was not comparable between the two groups.
Table 3. Visual analog scale (VAS)
Lastly, regarding the total blood loss between the two groups, there was no statistical difference between the two groups as it was 617.17 (131.718) ml in group G and 576.67 (153.765) ml in group P with p-value 0.1 (). Only three patients required blood transfusion in group P and 6 patients in group G.
Table 4. Blood loss
4. Discussion
This study showed that opioids and Paracetamol doses (intraoperative and postoperative) were decreased in the group of the paravertebral block. Also, the Paravertebral group showed less pain score at the 30 min, 2 h and 4 h time points. After the 4th hour postoperatively, the severity of the pain subsides and was non-significant between the two groups.
Moreover, systolic blood pressure and the heart rate showed a difference between the two groups which may show that the paravertebral block provides an adequate degree of sympathectomy which is favorable to decrease both intraoperative blood loss and hypotensive drugs requirements. However, these changes have no clinical significance (regarding blood loss or hypotensive medications) and may be explained by the effect of the solid paravertebral block. Conversely, there was no statistical difference in the first 30 min from induction and for the next 24 h and this may be explained by the strong analgesics that were given after the surgery. On the other hand, the intraoperative hypotensive drugs requirement (propranolol and nitroglycerine) showed an increase with no statistical significance in the control group. Regarding the blood loss and blood transfusion requirement, there were no significant differences between the two groups. Lumbar paravertebral block at the level of L1 and L2 will cover the surgical area of the hip surgery. The caudal spread of the local anesthetic provides analgesia to the femoral and obturator nerve distribution as well, with sparing of the Quadriceps motor supply and this is in favor of early ambulation and rehabilitation and subsequently, early discharge [Citation8]. Also, it showed a decrease in the blood loss which may be explained by the hemodynamic stability and more pain control [Citation9,Citation10].
Wardhan R et al. studied the use of L1 to L2 single-shot lumbar paravertebral blocks and found that there is an opioid-sparing effect with fewer complications such as epidural spread. Moreover, it maintains hip flexor and quadriceps strength more than the lumbar plexus block with an advantage of early ambulation and discharge [Citation11]. Also, the use of lumbar plexus block decreases morphine consumption not as much as with continuous L2 lumbar paravertebral block. Likewise, there was no difference between both techniques regarding motor power preservation. Finally, they found that there is no real advantage in switching to L2 lumbar paravertebral block. On the other hand, the authors recommend the use of lumbar paravertebral block as an alternative to lumbar plexus block in the terms of safety as there is a high potential for complications in lumbar plexus block.
Zehra Hatipoglu et al. used Bupivacaine in addition to intravenous tramadol in an Ultrasound-guided lumbar paravertebral block in patients undergoing percutaneous Nephrolithotomy to provide more effective postoperative analgesia. In the postoperative period, ultrasound-guided PVBs using bupivacaine were lead to lower tramadol consumption [Citation12].
In comparison to epidural block, the lumbar paravertebral block showed to be superior to epidural regarding postoperative pain relief, simplicity, and complications after hip surgery [Citation13].
Ke X et al. combined paravertebral block at T12, lumbar paravertebral block, and sacral plexus block without any additional intravenous anesthetic or local anesthetics infiltration to the incision and found that they were successful for the surgery with no patient complained during the operations [Citation14].
5. Conclusion
Ultrasound-guided L1; L2 paravertebral block produces proper intraoperative hemodynamic control. It is also a safe and excellent alternative of analgesia that decreases the perioperative opioids requirements. However, it failed to decrease the total dose of hypotensive drugs and the total blood loss.
Availability of data and materials
The data that support the findings of this study are available from Cairo University hospitals but restrictions apply to the availability of these data which were used under license for the current study, and so are not publicly available. Data are however available from the authors upon reasonable request and with permission of Cairo university hospitals.
Ethical approval
Ethical approval from Cairo university hospitals research committee was obtained (N-73-2017). Approval date: 12-2-2018.
Consent to participate
Written informed consents were obtained from participants before inclusion.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Stein BE, Srikumaran U, Tan EW, et al. Lower-extremity peripheral nerve blocks in the perioperative pain management of orthopedic patients: AAOS exhibit selection. J Bone Joint Surg Am. 2012;94(22):e167.
- Messina A, Frassanito L, Colombo D, et al. Hemodynamic changes associated with spinal and general anesthesia for hip fracture surgery in severe ASA III elderly population: a pilot trial. Minerva Anestesiol. 2013;79(9):1021–1029.
- Birnbaum K, Prescher A, Hepler S, et al. The sensory innervation of the hip joint—an anatomical study. Surg Radiol Anat. 1997;19:371–375.
- YaDeau JT, Tedore T, Goytizolo EA, et al. Lumbar plexus blockade reduces pain after hip arthroscopy: a prospective randomized controlled trial. Anesth Analg. 2012;115(4):968–972. .
- Batra RK, Krishnan K, Agarwal A. Paravertebral block. J Anaesthesiol Clin Pharmacol. 2011;27(1):5–11.
- Vila H, Liu J, Kavasmaneck D. Paravertebral block: new benefits from an old procedure. Curr Opin Anaesthesiol. 2007;20(4):316–318.
- Eroglu A, Uzunlar H, Erciyes N. Comparison of hypotensive epidural anesthesia and hypotensive total intravenous anesthesia on intraoperative blood loss during total hip replacement. J Clin Anesth. 2005;17(6):420–425.
- Lee EM, Murphy KP, Ben-David B. Postoperative analgesia for hip arthroscopy: combined L1 and L2 paravertebral blocks. J Clin Anesth. 2008;20(6):462–465.
- De Leeuw MA, Zuurmond WW, Perez RS. The psoas compartment block for hip surgery: the past, present, and future. Anesthesiol Res Pract. 2011;2011:1–6.
- Duarte LT, Beraldo PS, Saraiva RA. Epidural lumbar block or lumbar plexus block combined with general anesthesia: efficacy and hemodynamic effects on total hip arthroplasty. Rev Bras Anestesiol. 2009;59(6):649–664.
- Wardhan R, Chilly JE, Auroux AS, et al. Is L2 paravertebral block comparable to lumbar plexus block for postoperative analgesia after total hip arthroplasty? Clin Orthop Relat Res. 2014;472(5):1475–1481.
- Hatipoglu Z, Gulec E, Turktan M, et al. Comparative study of ultrasound-guided paravertebral block versus intravenous tramadol for postoperative pain control in percutaneous nephrolithotomy. BMC Anesthesiol. 2018;18(1). DOI:10.1186/s12871-018-0479-7.
- Pankaj NS, Mohan BC. Comparative evaluation of continuous lumbar paravertebral versus continuous epidural block for post-operative pain relief in hip surgeries. Anesth Pain Med. 2012;1(3):178–183.
- Ke X, Li J, Liu Y, et al. Surgical anesthesia with a combination of T12 paravertebral block and lumbar plexus, sacral plexus block for hip replacement in ankylosing spondylitis: CARE-compliant 4 case reports. BMC Anesthesiol. 2017 26;17(1):86.