ABSTRACT
Purpose
The aim of this study was to evaluate the effect of recruitment maneuvers (RMs) and positive end expiratory pressure (PEEP) on diaphragmatic function and atelectasis areas during pneumoperitoneum and the trendelenburg position in laparoscopic sleeve gastrectomy (LSG) patients.
Methods
This prospective double-blinded randomized clinical study was conducted on 69 obese patients undergoing LSG. Patients were randomly allocated to one of the three groups, Group I (control group) patients were mechanically ventilated without PEEP or RM, Group II received PEEP of 5 cmH2O, and Group III received 5 cmH2O PEEP, and intermittent four times RM consisting of maintaining airway pressure 40 cmH2O for 40 s. Primary outcome was diaphragmatic excursion (DE). Secondary outcomes were atelectasis area, Forced Vital Capacity (FVC), Forced Expiratory Volume in 1 s (FEV1), Peak Inspiratory Pressure (PIP), and any complications.
Results
DE decreased in all investigated groups after anesthesia induction till the end of procedure compared to pre-induction values, and it was statistically significant lower in control group compared to the two interventional groups with no significant difference between PEEP and PEEP+RM groups. Atelectasis volume according to lung aeration score was significantly increased in control group compared to the other two groups, while there was no statistical significant difference in PEEP+RM compared to PEEP in all the times except before induction of anesthesia there was no significant difference among the three groups.
Conclusion
The application of RM and PEEP are helpful for preserving DE and improving lung aeration during laparoscopic sleeve gastrectomy.
1. Introduction
Bariatric surgery is the most effective treatment for morbid obesity and its secondary co-morbidities. Although there is no gold standard surgical procedure for obesity management, laparoscopic sleeve gastrectomy (LSG) is considered to be the first choice procedure, and recently it becomes the most commonly bariatric surgical procedure performed worldwide [Citation1,Citation2]. LSG is preferred to open techniques because it is associated with less incisional pain, shorter operative time, fewer pulmonary complications, and earlier hospital discharge [Citation3,Citation4].
However, laparoscopic procedures are operated under general anesthesia that decreases functional residual capacity (FRC) and enhances atelectasis [Citation5]. Also, it is performed in conjunction with intra-abdominal CO2 insufflations and subsequent increase in the intra-abdominal pressure [Citation6,Citation7]. This CO2 pneumoperitoneum together with the steep Trendelenburg position, which is maintained for long period in LSG, results in cephalic displacement of the diaphragm leading to several respiratory changes as decreased FRC and vital capacity (VC) [Citation8,Citation9], decrease pulmonary compliance, consequently resulting in atelectasis formation in the dependent lung regions [Citation10,Citation11]. Moreover, obese patients are more prone to develop perioperative atelectasis and postoperative pulmonary complications that is almost twice the risk among healthy subjects [Citation12,Citation13].
This alteration in FRC and lung volumes is more clinically relevant as it can result in small airway closure and further ventilation–perfusion mismatch that may lead to postoperative hypoxemia and respiratory complications [Citation14]. Several studies revealed that this lung volumes decrease and its ensuing complications are not only due to cephalic displacement of the diaphragm, but also due to decreased diaphragmatic excursion (DE) [Citation15,Citation16].
Several strategies have been proposed to reduce the incidence of atelectasis and other pulmonary complications such as induction of anesthesia in the head up position [Citation17] with or without a continuous positive airway pressure (CPAP) [Citation18], use of intra-operative positive end expiratory pressure (PEEP) [Citation10,Citation19] and implementation of alveolar recruitment maneuver (RM) [Citation10,Citation20] but it seems that the latter may be an effective method according to several studies conducted on morbid obese patients undergoing laparoscopic surgery and demonstrated that intra-operative recruitment of lung volume improves the respiratory mechanics and oxygenation [Citation21,Citation22]. While, other studies showed that application of PEEP intra-operatively is helpful for preserving DE and consequently reduce the incidence of atelectasis [Citation23].
It is worth mentioning that ultrasonography (US) can play an important role in evaluating the diaphragmatic structure and function by measuring diaphragmatic thickness and DE (Diaphragmatic Displacement DD) [Citation23,Citation24]. It is a promising bedside test to evaluate the structure and dynamic function of diaphragm peri-operatively and in critically ill patients to predict the outcome [Citation25,Citation26].
We hypothesized that performing RM in addition to PEEP may have an impact on improving diaphragmatic function in terms of DE and accordingly decreasing incidence of atelectasis evaluated by ultrasonography in obese patients undergoing LSG. Therefore, it may decrease the incidence of postoperative pulmonary complications.
2. Patients and methods
2.1. Study population and design
This prospective, double-blinded randomized controlled study was conducted on 69 ASA II and III patients aged 21–60 years with body mass index (BMI) ≥35 kg/m2 undergoing elective LSG under general anesthesia. Institutional Review Board (IRB) approval and the patient’s informed written consent were obtained. Our study was carried out in Zagazig University Hospitals from February 2019 to February 2020, and it was registered with ClinicalTrials.gov (NCT04130217).
Patients with preoperative diagnosis of obstructive sleep apnea by using the STOP-BANG questionnaire (Snoring, Tiredness during daytime, observed apnea, high blood Pressure, BMI over 35 Kg/m2, Age, Neck circumference, and Gender) [Citation27], history of pneumothorax, right side heart failure, chronic respiratory disease, diaphragmatic disease, neuromuscular disease, any contraindication for laparoscopic surgery or head-down position, and any history of thoracic surgeries were excluded from this study.
All participating patients were visited the night before the operation to discuss the goal and endpoints of the study to clarify the advantages and possible side effects of the strategy and to take an informed written consent regarding the procedure from every patient. On physical examination, special attention was given to document airway assessment, vital signs, cardiac and chest condition, and exclude contraindications. All patients were investigated by complete blood count, coagulation profile, blood sugar levels, a lipid profile, serum electrolytes, pulmonary function test, Liver functions test, and kidney functions test.
All patients were premedicated with Enoxaparine 0.5 mg/kg of lean body weight (LBW) 12 h before the intervention and elastic stockings (to be removed intra-operatively), were applied as a prophylaxis against deep venous thrombosis. Cefuroxime 1.5 g was given 30 min before the intervention as a preoperative antimicrobial prophylaxis and 10 mg Metoclopramide as well as 150 mg Ranitidine were given 1 h before surgery.
2.2. Sample size calculation
Sample size is calculated using (open Epi) program, assuming that DE after Trendelenburg position was (2.78 ± 0.56 cm) in mechanically ventilated group without PEEP versus (3.24 ± 0.78 cm) in mechanically ventilated group with PEEP of 5 cmH2O [Citation23]. The sample found to be 69 cases divided into three groups, (23 patients in each group), at confidence interval 95% and power of test 80.
2.3. Randomization
This study was conducted in a double-blinded manner (neither the patient nor the anesthetist who did the ultrasonographic assessment knew the randomization).The cases were randomly selected by a computer-generated randomization table which was used to randomly allocate patients equally into 3 study groups.
Group I (control group): patients were mechanically ventilated without PEEP or RM
Group II (PEEP group): patients were mechanically ventilated with PEEP of 5 cmH2o
Group III (PEEP+RM group): patients were mechanically ventilated with 5 cmH2o PEEP and intermittent 4 times RM consisting of maintaining airway pressure 40 cmH2o for 40 s, after procedures that have the potential to induce more atelectasis (post-induction of anesthesia, 2 min after completion of pneumoperitoneum, 2 min after placing the patient in Trendelenburg position, and finally 2 min after exsufflation of pneumoperitoneum) to be followed by maintaining 5 cmH2o PEEP [Citation21].
On entering the patient in the operating room, intravenous access was secured with an 18G cannula, standard monitors: electrocardiogram, pulse oximetry, non-invasive blood pressure monitor, and capnograph were attached and baseline parameters were recorded. In addition, a sequential pneumatic compressions device was applied to the patient’s calves.
Forced Vital Capacity (FVC) and Forced Expiratory Volume in the 1 s (FEV1) were measured in the sitting position by Microlife PF 100 spirometry (Microlife, Inc., Los Angels, USA) and baseline parameters were recorded.
2.4. Performance of the diaphragmatic ultrasound and lung ultrasound (LUS)
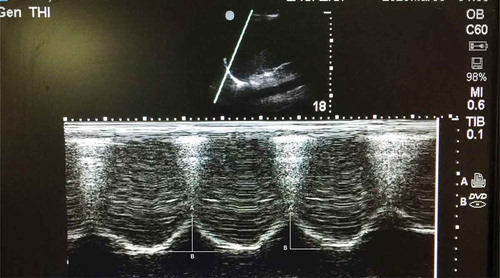
Before induction of anesthesia, while the patient was in supine position the right diaphragmatic cupola was examined by low frequency (2–5 MHz) convex probe of Sonosite M Turbo ultrasonography (FUJIFIM sonosite, Inc., Bothell, WA, USA), as it has a better sonographic window provided by the liver [Citation23]. The probe was placed at the right subcostal region midway between the anterior axillary line and the mid- clavicular line, then directed backwards, upwards and slightly medially till the dome of the diaphragm appeared. Subsequently, using an M-mode, DE was evaluated by detecting craniocaudal displacement of diaphragm that measured in centimeters on the vertical axis of tracing from the baseline to the point of end of inspiration on the graph (). Two readings were taken and the average was recorded.
Figure 1. M-mode ultrasonography of diaphragmatic excursion. A: primary position of diaphragm at end of expiration; b: secondary position at end of inspiration. The amplitude of excursion (white line) was measured on vertical axis of the tracing from A B.
Later, LUS was performed with the same convex probe of Sonosite M Turbo ultrasonography. The chest was divided into 12 regions, three longitudinal lines (parasternal, anterior, and posterior axillary) and two axial lines, one above the diaphragm and another one 1 cm above the nipples divided each hemithorax into six sections (anterior, lateral, and posterior fields). Each hemithorax was examined using B-mode to assess degree of lung aeration within the total 12 lung zones. The probe was placed perpendicular to the ribs looking for the bat sign (the pleura and lung tissue between the acoustic shadows of two adjacent ribs), a lung sliding and A lines. Anesthesia-induced atelectasis was seen as juxtapleural consolidations of various sizes and may be associated with other LUS signs as absence of A lines, absence of lung sliding, presence of B lines, that mentioned in lung aeration score previously described for adults () [Citation28]. This score is inversely proportional to the degree of lung aeration.
Table 1. LUS score to assess the degree of lung aeration [Citation28].
Preoxygenation with 100% O2 (4 l/min of O2 for 5 min) was carried out while the patient in ramp position. Anesthesia was induced using fentanyl 1 μg/kg, propofol (1.5–2) mg/kg of LBW (LBW = Ideal Body Weight (IBW) + 20–40% excess of IBW), and succinylcholine 1 mg/kg total body weight (TBW) to facilitate intubation. Anesthesia was maintained with (O2, Sevoflurane mixture), muscle relaxation was maintained with rocuronium 0.6 mg/kg of IBW. Lungs were ventilated using volume-controlled ventilation with a tidal volume of 6–8 ml/kg of IBW, respiratory rate of 12–14 breaths/min. Tidal volume and ventilation rate was adjusted to maintain end-tidal carbon dioxide concentration (EtCO2) at 35–45 mmHg using (Drager ventilator AG, Lubeck, Germany). Patients in Groups II and III will receive 5 cmH2o PEEP.
CO2 was insufflated into the peritoneal cavity till the intra-abdominal pressure reached 15 mmHg and patient was placed in Trendelenburg position.
Fentanyl was given intra-operatively as an additional bolus dose of 1 μg/kg LBW if there was an increase in mean arterial pressure (MAP) or heart rate (HR) more than 20% from baseline values. 0.2 mg/kg rocuronium boluses were given every 30 min as maintenance of muscle relaxation. For intravenous fluids, either lactated Ringer’s solution or normal saline was given at a rate of 10 mL/kg/h of IBW.
At the end of the surgery, reversal of muscle relaxant with sugammadex 2–4 mg/kg of IBW, patients were allowed to awake from anesthesia in the head-up position and all patients were extubated and maintained on O2: air mixture.
Post-operatively, All the patients were taken to the intensive care unit (ICU), placed in their bed at 30° to 45°degree upright and receive O2 via non-rebreathing mask with reservoir bag. Post-operative analgesia was in the form of local anesthetic wound infiltration of the port sites with 0.125% bupivacaine, paracetamol (1 g IV four times a day) and diclofenac (75 mg IV twice a day).
2.5. Parameters evaluation
- Patients’ characteristics: Age, sex, BMI, ASA physical status.
- Duration of anesthesia (min) and of pneumoperitoneum (min).
- FVC and FEV1 were measured in the sitting position: before the surgery, 12 and 24 h postoperatively by Microlife PF 100 spirometry (Microlife, Inc., Los Angels, USA).
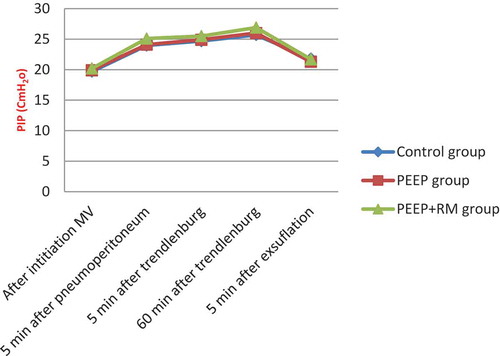
- Peak Inspiratory Pressure (PIP) was measured by anesthesia machine (Drager ventilator AG, Lubeck, Germany) after initiation of mechanical ventilation, 5 min after completion of pneumoperitoneum, 5 min after adopting Trendelenburg position, 60 min later with pneumoperitoneum and Trendelenburg position, and 5 min after exsufflation of pneumoperitoneum.
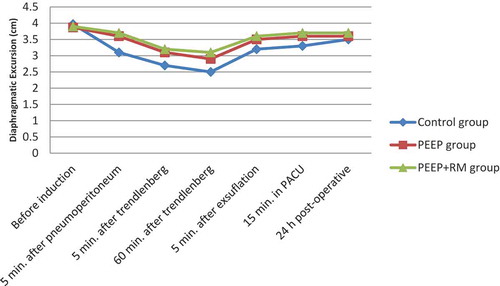
- DE (primary outcome): was measured before induction of anesthesia, 5 min after completion of pneumoperitoneum, 5 min after adopting Trendelenburg position, 60 min later with pneumoperitoneum and Trendelenburg position, 5 min after exsufflation of pneumoperitoneum and patient placed back in the supine position, 15 min after arrival of patient in the recovery room and 24 h postoperatively.
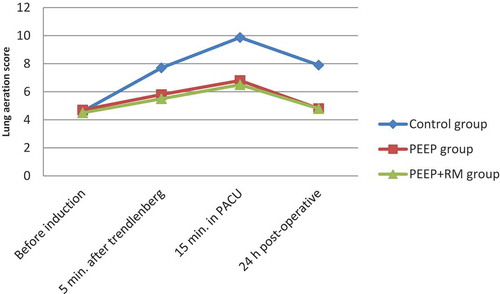
- Incidence of atelectasis and total lung aeration score were assessed before induction of anesthesia, 5 min after adopting Trendelenburg position, 15 min after arrival of the patient in the recovery room and 24 h postoperatively.
- Complications that may happen due to intraoperative PEEP and RM as transient hypotension, oxygen desaturation, barotrauma in the form of (pneumothorax), and postoperative complication as hypoxemia or respiratory distress that may require CPAP, Bi-level Positive Airway Pressure (BiPAP) or reintubation in the first postoperative 24 h were recorded.
2.6. Statistical analysis
Data were analyzed using IBM SPSS 23.0 for windows (SPSS Inc., Chicago, IL, USA) and NCSS 11for windows (NCSS LCC., Kaysville, UT, USA). Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage; the following tests were used to test differences for significance; difference and association of qualitative variable by Chi- squared test (χ2). Differences when comparing between more than two means by Analysis of variance (ANOVA), Krusskal–wallis test when comparing more than two means of not normally distributed data and Paired t-test (Wilcoxon test for non-parametric data) for change of continuous data of the same group. P value was set at <0.05 for significant results & <0.001 for high significant result.
3. Results
Sixty-nine obese patients undergoing elective LSG under general anesthesia were enrolled in this study. There were no statistical significant differences in the three groups regarding age, sex, BMI, and ASA status as well as the anesthesia and pneumoperitoneum durations ().
Table 2. Patients’ and operative characteristics.
There was no statistical significant difference in the pre-operative FVC and FEV1 measurements between the 3 studied groups. While, the post-operative mean values of FVC and FEV1 (12 and 24 h post-operatively) were highly statistical significant different between the control group compared to the two interventional groups. FVC and FEV1 were markedly decreased in the control group. However, there was no statistical significant difference in their postoperative mean values between PEEP and PEEP+RM groups ().
Table 3. Spirometric parameters of the three studied groups.
While, when comparing the Pre- and post-operative FVC and FEV1 mean values within each group, there was high statistical significant difference as they were significantly decreased in the post-operative period compared to the pre-operative measurements ( and ).
Table 4. Pre- and postoperative FVC within each group.
Table 5. Pre- and postoperative FEV1 within each group.
PIP revealed no statistical significant difference among the three groups all the times throughout the procedure. However, there was significant increase in its values within each group after (pnemoperitoneum and trendeleburg position) compared to after initiation of mechanical ventilation values ().
Regarding the DD, before induction of anesthesia there was no statistical significant difference between the three groups, later on after pneumoperitoneum and throughout the whole procedure up to 24 h postoperatively, there was statistical significant difference between the control group compared to the two interventional groups showing significant decrease in DD in control group. While, there was no statistical significant difference in its values in PEEP+RM group compared to PEEP group ()
However, the DD mean values were statistically significant different within each group. DD was significantly decreased within each group after induction of anesthesia till the end of whole procedure compared to pre induction mean values ().
Regarding the lung aeration score before induction of anesthesia, there was no statistical significant difference among the three groups. However, there was statistical significant difference in the lung aeration score between the control group and the other two groups that means significant loss of lung aeration and increase atelectasis areas in control group more than the other groups in all times with no significant difference in its values in PEEP+RM group compared to PEEP group.
While, comparing the lung aeration score values after induction of anesthesia till the end of the whole procedure, there was statistical significant increase in atelectasis areas compared with its pre-induction of anesthesia values within each group ().
Throughout the entire study, there was no statistical significant difference among three groups regarding occurrence of complications. Also, no barotrauma was occurred in any of the studied groups ().
Table 6. Intra and postoperative complications among studied groups.
4. Discussion
Increased intra-abdominal pressure resulting from Pneumoperitoneum and Trendelenburg position during LSG was found to restrict DD. This mechanical restriction of the diaphragm may induce ventilation/perfusion mismatch and hypoventilation in the ventilator-dependent areas of the lung resulting in reduced pulmonary compliance and FRC that leads to pulmonary atelectasis [Citation29–Citation31].
In our study, the effects of RM and PEEP on diaphragmatic functions during pneumoperitoneum and Trendelenburg position in LSG patients was evaluated in terms of DE and detection of subsequent lung atelectasis by using the ultrasound.
Our results showed that DE is decreased after induction of anesthesia till the end of whole procedure in all enrolled patients compared to the pre-induction values, and it was significantly lower in the control group compared to PEEP and PEEP+RM groups indicating improved of diaphragmatic function in the interventional groups with more improvement in PEEP+RM group but this was not statistically significant than PEEP alone. Also, lung atelectasis volume depending on lung aeration score was significantly increased in the control group compared to the other two groups, while there was no significant difference in its values in PEEP+RM group compared to PEEP group in all the times except before induction of anesthesia there was no significant difference among the three groups.
Despite the fact that our results did not find statistical significant difference in DD and lung aeration scores between PEEP and PEEP+RM groups, we observed that these parameters were improved more with RM addition to 5 cmH2o PEEP with no side effects.
In support to our findings, DE and subsequent lung compliance were decreased with steep trendelenburg position and pneumoperitoneum in Kim et al., study conducted on females undergoing elective pelviscopic radical hysterectomy which had a negative impact on their postoperative pulmonary functions [Citation16]. Also, the same findings was observed in laparoscopic cholecystectomy patients in Andersson et al., study who reported increased mean atelectasis volume within the dependent lung region by 66% [Citation32].
Optimization of the PEEP level is considered one of the most important factors in maintaining pulmonary functions during the perioperative period and in accordance with our preference of low level of PEEP in the present study. Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology et al., in their randomized clinical trial reported that intra-operative mechanically ventilated obese patients with higher PEEP level of 12 cmH2O did not reduce post-operative pulmonary complications compared to those ventilated with a lower PEEP of 4 cmH2O, and that higher PEEP was complicated with more intra-operative hypotension and bradycardia [Citation33]. Furthermore, in the study conducted by Rashwan et al. the application of 10 cmH2O PEEP was found to improve DE and reduce incidence of atelectasis more than 5cmH2O PEEP which was not statistically significant but 10 cmH2O PEEP was associated with more complications in the form of significant increase in the PIP, and they concluded that 5cmH2O PEEP is better to be used [Citation23].
The results of the present study were compatible with Acosta et al., who reported that the majority of children patients undergoing laparoscopy have anesthesia-induced atelectasis mostly due to pneumoperitoneum while the lung aeration as well as ultrasound scores were significantly improved with the application of RMs and they concluded that laparoscopy and anesthesia induced lung collapse could be prevented by RMs followed by PEEP [Citation34].
In another study Futier et al., analyzed the effects of RM in patients scheduled for laparoscopic surgery in reverse Trendelenburg position, and they found that PEEP+RM exhibits improvement in End Expiratory Lung Volume, static elastance and overall respiratory mechanics as well as the oxygenation during pneumoperitoneum more than PEEP alone [Citation21]. Additionally, Cinnella et al., reported that RM applied 15 min after induction of pneumoperitoneum followed by 5 cmH2O PEEP till the end of the surgery increased transpulmonary pressure and improved chest wall elastance along with gas exchange improvement in patients undergoing laparoscopic gynecological surgery [Citation35].
In another aspect of our study, we found that pneumoperitonium and Trendelenberg position significantly decrease the spirometric parameters (FVC, FEV1) post-operatively in all patients. On the other hand, we observed that an improvement in the FVC and FEV1 values in both PEEP and PEEP+RM groups compared to the control group. While, applying RM with PEEP did not exhibit statistical significant difference than PEEP alone. In accordance with these findings, Severgnin et al., reported that patients with protective ventilatory strategy of lower tidal volumes, 10 cm H2O PEEP and RM, showed improvement of post-operative pulmonary function tests (FVC and FEV1) more than those with standard ventilation strategy [Citation36].
Contrary to what we found, Defresne et al., concluded that protective mechanical ventilation of low tidal volumes, 10 cm H2O PEEP and two RMs did not improve postoperative pulmonary functions compared to mechanical ventilation of low tidal volume alone in laparoscopic gastric bypass surgery [Citation37]. This could be attributed to the time of post-operative spirometric measurement as it was measured only once at the end of first postoperative day in their study, consequently, the potential benefits of RM throughout early post-operative period were not explored, which we have covered by double measurements through first postoperative day. Moreover, the number of RMs performed could add an explanation as we did it four times versus only two times by Defresne et al..
Finally, our results entrenched that preserving DE is one of the critical factors that maintain adequate pulmonary function and decrease incidence of atelectasis that may occur during major laparoscopic surgery and that applying RM and PEEP is helpful maneuvers in preserving diaphragmatic function.
On the other hand, there were some limitations. Firstly, the inability to have suitable scan of the left diaphragmatic copula due to lack of an acoustic window in some patients, however this limitation did not have a significant effect in this study, as we utilized the right hemidiaphragm for scanning using the liver as an acoustic window. Secondly, the changes in FRC were not measured in our study also; we did not document peri-operative oxygen saturation changes. This study presents the parameters we thought it would prove our hypothesis but we believe that studying the changes of FRC and peri-operative oxygen saturation could support our findings. So, further studies on large-scale populations and different patients’ sub-groups are required to assess who would benefit more from our interventions.
5. Conclusion
In conclusion, our results support that the application of RM and PEEP are helpful for preserving DE and significantly improve lung aeration and decrease atelectasis during laparoscopic sleeve gastresctomy that can be evaluated through diaphragmatic US and lung US. In this study RM followed by PEEP of 5cmH2O improved DE and lung aeration more but not statistically significant than 5cmH2O PEEP alone without the occurrence of side effects calls to limit their use.
Trial registration
This clinical trial was registered with ClinicalTrials.gov (NCT04130217).
Disclosure statement
There is no conflict of interest
References
- Felsenreich DM, Prager G, Kefurt R, et al. Quality of life 10 years after sleeve gastrectomy: a multicenter study. Obes Facts. 2019;12:157–166.
- Guetta O, Vakhrushev A, Dukhno O, et al. New results on the safety of laparoscopic sleeve gastrectomy bariatric procedure for type 2 diabetes patients. World J Diabetes. 2019;10(2):78–86.
- Sarandan M, Guragata-Balasa C, Papurica M, et al. Anesthesia in laparoscopic bariatric surgery (gastric sleeve) – preliminary experience. TMJ. 2011;61(1):26–31.
- Staehr-Rye AK, Rasmussen LS, Rosenberg J, et al. Minimal impairment in pulmonary function following laparoscopic surgery. Acta Anaesthesiol Scand. 2014;58:198–205.
- Hedenstierna G, Edmark L. The effects of anesthesia and muscle paralysis on the respiratory system. Intensive Care Med. 2005;10:1327–1335.
- El-Dawlatly AA. Hemodynamic profile during laparoscopic cholecystectomy versus laparoscopic bariatric surgery: the impact of morbid obesity. Middle East J Anaesthesiol. 2006;18:733–742.
- Talab HF, Zabani IA, Abdelrahman HS, et al. Intraoperative ventilatory strategies for prevention of pulmonary atelectasis in obese patients undergoing laparoscopic bariatric surgery. Anesth Analg. 2009;109:1511–1516.
- El-Dawlatly AA, Al-Dohayan A, Abdel-Meguid ME, et al. The effects of pneumoperitoneum on respiratory mechanics during general anesthesia for bariatric surgery. Obes Surg. 2004;14:212–215.
- Suh MK, Seong KW, Jung SH, et al. The effect of pneumoperitoneum and trendelenburg position on respiratory mechanics during pelviscopic surgery. Korean J Anesthesiol. 2010;59:329–334.
- Reinius H, Jonsson L, Gustafsson S, et al. Prevention of atelectasis in morbidly obese patients during general anesthesia and paralysis: a computerized tomography study. Anesthesiology. 2009;111:979–987.
- Reber A, Nylund U, Hedenstierna G. Position and shape of the diaphragm: implications for atelectasis formation. Anaesthesia. 1998;53:1054–1061.
- Eichenberger A, Proietti S, Wicky S, et al. Morbid obesity and postoperative pulmonary atelectasis: an underestimated problem. Anesth Analg. 2002;6:1788–1792.
- Las Vegas Investigators. Epidemiology, practice of ventilation and outcome for patients at increased risk of postoperative pulmonary complications: Las Vegas—an observational study in 29 countries. Eur J Anaesthesiol. 2017;34(8):492–507.
- Milic-Emili J, Torchio R, D’Angelo E. Closing volume: a reappraisal (1967–2007). Eur J Appl Physiol. 2007;6:567–583.
- Normando VMF, Brito MVH, de Araújo Júnior FAD, et al. Effects of pneumoperitoneum on the amplitude of diaphragmatic excursion in pigs. J Bras Pneumol. 2006;32(1):16–22.
- Kim K, Jang D-M, Park J-Y, et al. Changes of diaphragmatic excursion and lung compliance during major laparoscopic pelvic surgery: A prospective observational study. plos ONE. 2018;13(11):e0207841.
- Dixon BJ, Dixon JB, Carden JR, et al. Preoxygenation is more effective in the 25 degrees head-up position than in the supine position in severely obese patients: a randomized controlled study. Anesthesiology. 2005;6:1110–1115.
- Coussa M, Proietti S, Schnyder P, et al. Prevention of atelectasis formation during the induction of general anesthesia in morbidly obese patients. Anesth Analg. 2004;5:1491–1495.
- Jo YY, Lee JY, Lee MG, et al. Effects of high positive endexpiratory pressure on haemodynamics and cerebral oxygenation during pneumoperitoneum in the Trendelenburg position. Anaesthesia. 2013;68:938–943.
- Rothen HU, Sporre B, Engberg G, et al. Re-expansion of atelectasis during general anaesthesia: a computed tomography study. Br J Anaesth. 1993;6:788–795.
- Futier E, Constantin J, Pelosi P, et al. Intraoperative recruitment maneuver reverses detrimental pneumoperitoneum-induced respiratory effects in healthy weight and obese patients undergoing laparoscopy. Anesthesiology. 2010;6:1310–1319.
- Whalen FX, Gajic O, Thompson GB, et al. The effects of the alveolar recruitment maneuver and positive end-expiratory pressure on arterial oxygenation during laparoscopic bariatric surgery. Anesth Analg. 2006;1:298–305.
- Rashwan DAE, Mahmoud HE, Nofal WH, et al. Ultrasonographic evaluation of the effect of positive end-expiratory pressure on diaphragmatic functions in patients undergoing laparoscopic colorectal surgery: a prospective randomized comparative study. J Anesth Clin Res. 2018;9(7):843–851.
- Grosu HB, Lee YI, Lee J, et al. Diaphragm muscle thinning in patients who are mechanically ventilated. Chest. 2012;142:1455–1460.
- Summerhill EM, El-Sameed YA, Glidden TJ, et al. Monitoring recovery from diaphragm paralysis with ultrasound. Chest. 2008;133:737–743.
- Matamis D, Soilemezi E, Tsagourias M, et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 2013;39:801–810.
- Chung F, Abdullah HR, Liao P. STOP-bang questionnaire: a practical approach to screen for obstructive sleep apnea. Chest. 2016;149(3):631–638.
- Soummer S, Perbet H, Brisson H, et al. The lung ultrasound study group: ultrasound assessment of lung aeration loss during a successful weaning trial predicts postextubation distress. Crit Care Med. 2012;40:2064–2072.
- Strang CM, Hachenberg T, Fredén F, et al. Development of atelectasis and arterial to end-tidal PCO2-difference in a porcine model of pneumoperitoneum. Br J Anaesth. 2009;103:298–303.
- Hayden P, Cowman S. Anaesthesia for laparoscopic surgery. Continuing Educ Anaesth Crit Care Pain. 2011;11:177–180.
- Sprung J, Whalley DG, Falcone T, et al. The effects of tidal volume and respiratory rate on oxygenation and respiratory mechanics during laparoscopy in morbidly obese patients. Anesth Analg. 2003;97:268–274.
- Andersson LE, Baath M, Thorne A, et al. Effect of carbon dioxide pneumoperitoneum on development of atelectasis during anesthesia, examined by spiral computed tomography. Anesthesiology. 2005;102:293–299.
- Writing Committee for the PROBESE Collaborative Group of the PROtective VEntilation Network (PROVEnet) for the Clinical Trial Network of the European Society of Anaesthesiology, Bluth T, Neto AS, Schultz MJ, et al. Effect of intraoperative high positive end-expiratory pressure (PEEP) with recruitment maneuvers vs low peep on postoperative pulmonary complications in obese patients: a randomized clinical trial. JAMA. 2019;321(23):2292–2305.
- Acosta CM, Sara T, Carpinella M, et al. Lung recruitment prevents collapse during laparoscopy in children. Eur J Anaesthesiol. 2018;35:573–580.
- Cinnella G, Grasso S, Spadaro S, et al. Effects of recruitment maneuver and positive end-expiratory pressure on respiratory mechanics and transpulmonary pressure during laparoscopic surgery. Anesthesiology. 2013;118:114–122.
- Severgnini P, Selmo G, Lanza C, et al. Protectivemechanicalventilation during general anesthesia for open abdominal surgery improves postoperative pulmonary function. Anesthesiology. 2013;6:1307–1321.
- Defresne AA, Hans GA, Goffin PJ, et al. Recruitment of lung volume during surgery neither affects the postoperative spirometry nor the risk of hypoxaemia after laparoscopic gastric bypass in morbidly obese patients: a randomized controlled study. Br J Anaesth. 2014;113(3):501–507.