ABSTRACT
Background
Anesthesiologists in Egypt as a representative of developing countries with large populations and shortage of trained personnel and extended working hours that may reach 30 continuous hours are susceptible victims of fatigue and sleep deprivation.
Objectives
To evaluate and compare differences in cognitive function of anesthesia residents before and after the 24 hours work shift.
Methods
Prospective, observational, cohort study that was conducted in tertiary care hospital (Kasr El-Aini Hospital, Faculty of Medicine, Cairo University). Fifty anesthesia residents with 24 hours working shift participated in the study. The cognitive function was assessed before and after the shift using Psychomotor Vigilance Task, Karolinska Sleepiness Scale, Epworth Sleepiness Scale and Trail Making Test before and after the shift.
Results
Psychomotor Vigilance Task mean reaction time before and after shift was 302.1 ± 35.2 ms and 371.9 ± 55.4 ms, respectively (P value < 0.001). Karolinska Sleepiness Scale mean before and after shift was 3.34 ± 1.189 and 6.24 ± 1.589, respectively (P value < 0.001). Epworth Sleepiness Scale mean before and after shift was 6.68 ± 2.759 and 14.86 ± 3.423, respectively (P value < 0.001). Trail Making Test mean times in both parts A and B, before shifts were 38.82 ± 8.458 and 63.16 ± 11.557 s, respectively. While, post shifts mean times were 44.86 ± 9.370 and 72.60 ± 12.294 s, respectively (P value < 0.001 for both parts).
Conclusions
Sleep deprivation in night shifts increases the day-time sleepiness and affects the anesthesiologist’ cognitive processes, such as reaction time, alertness, rapid problem solving, psychomotor skills, attention, mental flexibility, and executive functions.
Clinical trial registration ID
clinicaltrials.gov: NCT03784560.
1. Introduction
Serious concerns have been raised about sleep deprivation and its consequences on medical staffs. Being a critical specialty, anesthesiologists may carry special concerns as they are required to have mindful analysis and rapid judicious decisions in most of situations especially in trauma settings and critical circumstances in the operating theatres [Citation1].
In healthy adults, significant levels of cognitive deficits occur when sleeping hours is decreased below 7 hours per night. Multiple studies have declared that partial sleep deprivation is a risk factor for most non-communicable diseases like obesity, diabetes, cardiovascular disease, and hypertension [Citation2]. Besides that, Cheung et al. clearly demonstrated that only one night of acute sleep deprivation increases the oxidative damage of DNA [Citation3]. In addition, fatigue, stress, and sleep deprivation have been recognized as direct causes of increasing numbers of suicides among anesthesiologists [Citation4,Citation5]. In a recent study, Shinde et al. reported their recommendations to reduce the incidence of suicides among anesthesiologists [Citation6].
In anesthesiologists, serious effects of fatigue and sleep deprivation would be beyond the individual health and would extend to affect the quality of patient management and his safety [Citation7,Citation8]. In developing countries like Egypt, due to the huge populations and shortage of trained and qualified personal, anesthesiologists who cover overnight trauma shifts are subjected to long working hours that may reach 24 hours (hrs) or more, which may have a negative impact on their performance leading to decline in psychomotor skills and increase in the rate of false responses to visual stimuli [Citation9,Citation10]. Additionally, disruption of circadian rhythm that accompany work at night shift, increases decline in performance and reasoning abilities in some critical situations [Citation11].
However, some studies concluded that there is inter-individual differences in the effects and responses of sleep deprivation and personal adaptive coping behaviors that lead to improvement in clinical performance and psychological adjustment [Citation12].
In the current study, we hypothesized that there would be a significant decline in variety of cognitive functions after a night shift affecting the anesthesiologist performance, reasoning ability, and decision making. Cognitive functions represented by reaction time (RT), day time sleepiness, alertness, and decision making were assessed by the Psychomotor Vigilance Task (PVT) [Citation13], Karolinska Sleeping Scale (KSS) [Citation14], Epworth Sleepiness Scale (ESS) [Citation15,Citation16], and Trail Making Test [Citation17].
Aim of the work is to evaluate and compare differences in cognitive function of anesthesia residents between before and after the 24 hrs work shift.
2. Methods
This prospective observational study was conducted at Kasr Al-Aini Hospital, Faculty of medicine Cairo University from February 2019 to June 2019 after approval of the scientific and ethical committee and registration at clinicaltrials.gov (NCT03784560).
The current study included 50 anesthesiologists who work in operating theatres, emergency department at Kasr El- Ainy Hospital with different levels of experience and aged between 25 and 28 years after excluding participants with a history of chronic neurological disease, sleep disorders, and psychiatric disorders within the past 2 years.
An anonymous questionnaire included two groups of different items were used. Items of the first group are about the personal data i.e., age, sex, marital status and parenting status, consumption behavior (tea, coffee, carbonated drinks, tobacco, anxiolytics, antidepressants, psychotropic agents, and sport), and professional activity (number of extended worked shifts per month, number of weekends worked per month).
Items of the second group are related to the night shift itself i.e., number of cases and the rest hours during the shift.
As different studies showed that increased sleep deprivation leads to decline in alertness and psycho-motor skills, cumbersome problem-solving, The Psychomotor Vigilance Task (PVT) [Citation13] is used as an assessment tool of neurobehavioral performance with the advantages of being valid, reliable, brief, and easily performed. PVT is a RT assessment that requires sustained attention and measures the speed at which subjects respond to a visual stimulus. In PVT, the participant simply presses a response button as soon as a visual stimulus appears on the screen. There is standard version of the PVT with duration of 10 min. The shorter version, PVT brief, with duration of 3 minutes have been used in the current study using PEBL 2 software computer program and RTs were displayed to the study participants in milliseconds.
Karolinska Sleepiness Scale (KSS) is a self-assessed 9-point Likert scale for subjective assessment of the individual’s level of drowsiness at a time. It has word descriptors to describe the scale points from 1 = “very alert” to 9 = “very sleepy, fighting sleep, an effort to keep awake”. High validity of KSS in assessing sleepiness occurs when comparing it to Electroencephalogram (EEG) changes, as the KSS scores are closely related to EEG and behavioral variables.
Epworth Sleepiness Scale (ESS), being simple and self-administered questionnaire, ESS is most commonly used in assessment that enables the individual to determine own sleep tendency subjectively. By history taking to retrospectively assess sleepiness before and after the shift in the previous period, the subjects are asked to rate on a scale from 0 to 3 their usual probability of dozing off in 8 different situations, with 0 = “would never doze” and 3 = “a high chance of dozing”. The total ESS score, ranging from 0 to 24, is the sum score of the eight times. Normal day time sleepiness is represented with ESS scores from 0 to 10 detect, while increased levels of excessive daytime sleepiness (EDS) are represented with ESS scores of 11–24.
Trail Making Test (TMT) is one of the most commonly used neuropsychological tests that assess different cognitive functions including visual search, scanning, speed of processing, mental flexibility, and executive functions. The TMT is formed of two parts. In TMT-A, the subject is asked to draw lines sequentially connecting 25 encircled numbers distributed on a paper sheet. In TMT-B except, the subject is asked to alternate between numbers and letters (e.g., 1, A, 2, B, 3, C, etc.). Each part is represented by time in seconds that required to finish the task.
2.2. Method of assessment
The working shift duration is 24 hrs, starts at 8:00 am and ends at 8.00 am of the following day. Each participant filled the questionnaires early at morning, just before starting the shift followed by performing the tests, PVT, ESS, KSS, and TMT, to repeat them as soon as the night shift is over. The participants did the tests in an isolated quiet room to insure best atmosphere away from any external stimulus.
The primary outcome was the Psychomotor Vigilance Task. The secondary outcomes were Karolinska Sleepiness Scale, Epworth Sleepiness Scale, and Trail Making Test.
3. Statistical Methods
3.1. Sample size
Sample size was calculated using G-power software. Considering a study power if 0.8 and a P value of 0.05 to be statistically significant. The sample size was calculated based on data derived from a similar study [Citation18] (PVT = 266 ± 38.5 in one group and 298 ± 83.7 in the other group). The total sample size was 46 residents and we increased it to 50 to compensate for drop-outs.
4. Statistical analysis
Data were statistically described in terms of mean ± standard deviation (± SD), median and range, or frequencies (number of cases) and percentages when appropriate. Comparison of numerical variables between the different units was done using Kruskal Wallis test. Within group comparison of numerical variables was done using paired t test. Correlation between various variables was done using Pearson moment correlation equation for linear relation of normally distributed variables and Spearman rank correlation equation for non-normal variables/non-linear monotonic relation. p values less than 0.05 was considered statistically significant. All statistical calculations were done using computer program IBM SPSS (Statistical Package for the Social Science; IBM Corp, Armonk, NY, USA) release 22 for Microsoft Windows.
5. Results
Fifty-four residents agreed to participate and written consent was obtained, 4 were excluded due to incomplete data leaving only 50 participants, 23 male (46%), and 27 female (54%). Age group ranged from 25 to 28 years old with a mean 26.88 ± 1.043. Nineteen residents were married (39%), 31(61%) were not, and out of these 19 participants, only 9 parenting from 1 to 3 kids. Only 5 participants were exercising regularly, 48 of 50 participants were found to drink coffee, tea or carbonated beverages during their work day ranging from 1 cup to 11 cups per day with mean 3.26 ± 2.155 cup ().
Table 1. Personal data and professional activity.
The number of 24 hrs shifts per months, number of weekend shifts, hours of sleep before the shift, and hours of rest during shift are presented in .
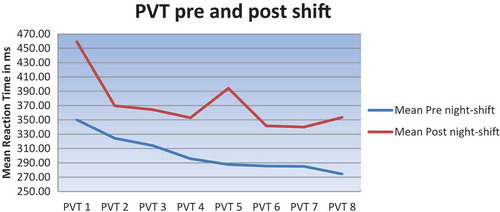
As for the tests’ results, PVT mean RT of the residents showed statistically significant decrease after the shift 371.9 ± 55.4 ms in comparison to the mean RT before the shift 302.1 ± 35.2 (P value < 0.001) denoting increased sleep deficit which correlates with deteriorated alertness, slower problem-solving, declined psycho-motor skills, and increased rate of false responding (; ).
Table 2. Comparing assessment tools pre and post night shift.
KSS mean scores showed significant increase following the shift 6.24 ± 1.589 in comparison to mean scores before shift 3.34 ± 1.189 (P value < 0.001) ().
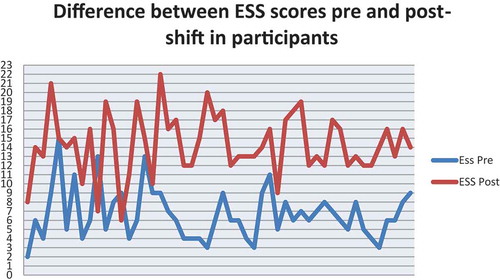
While ESS scores showed higher scores among residents after the shift with mean 14.86 ± 3.423 while mean score before the shift was 6.68 ± 2.759 (P value < 0.001) ( and ).
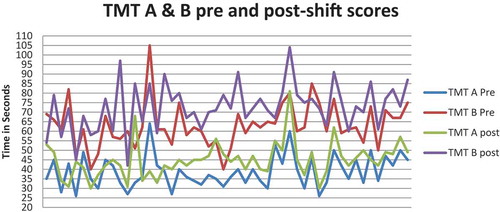
Regarding TMT results, in both part A and part B, participants showed increase in time needed to complete tests after the shifts with mean 44.86 s ± 9.370 s and 72.60 s ± 12.294 s, respectively, when compared to time needed for participants to finish part A and B before the shift with mean 38.82 s ± 8.458 s and 63.16 s ± 11.557 s with P value < 0.001 and P value < 0.001 for both parts, respectively ( and ).
When correlating the results of the used tests with number of cases that residents worked during the shift, they were statistically insignificant apart from TMT B, as shown in .
Table 3. Correlation between number of cases in the shift and test post-shift results.
6. Discussion
It has been established in literatures that sleep deprivation has a role in neurobehavioral functions impairment [Citation19–Citation23]. Some studies found out that the performance impairment of being awake for more than 24 consecutive hours is equivalent to a blood alcohol concentration of 1 g/L during simulated driving test [Citation24,Citation25] In a large retrospective study performed on surgeons using simulated laparoscopic surgery, sleep deprivation has been proven to increase the surgery duration and the rate of complications during complex surgical procedures [Citation26,Citation27]. In addition, physical and mental fatigue has been suggested to be associated with some major pharmacological errors like syringe swap, wrong drug and wrong dose [Citation28]. It is also reported that sleep deprivation is associated with some disorders such as neuropsychological illness i.e., depression and anxiety, metabolic syndrome i.e., obesity, and cardiovascular diseases [Citation29–Citation35].
National Academy of Science, Institute of Medicine (Washington, DC) declared fatigue as an important factor in medical errors and has a partial responsibility for 44 000–98 000 annual deaths in hospitals [Citation36]. Multiple recommendations concerning occupational safety, regulations, and job performance have been studied and published in government agencies like the National Highway Traffic Safety Administration and the National Aeronautics and Space Administration, and in occupational societies like truck drivers and airline pilots [Citation37–39].
Following these continuous reports and studies of sleep deprivation and fatigue negative effect on individual performance and cognitive functions, several recommendations have been raised for physicians and patients safety and asked for an increase in education about sleep deprivation and adopted different policy to reduce the working hours between medical personnel. However, regarding anesthesia and ICU residents, a very little has been changed in their scheduled working hours due to lack of the well trained anesthesiologists who should deal with the continued emergencies that happen 24 hours/day.
In Kasr Al-Aini Hospital, Cairo University, working hours for anesthesiology residents may extend to 36 continuous hrs, as after the end of the emergency shift, the residents continue work in the scheduled operating theatres. Being a tertiary care center, Kasr Eleni Hospital receives hundreds of patients daily from all over Egypt and sometimes from nearby countries. Scheduled operation theatres and emergency operating theatres have about 90 operating tables and 697 Surgical ICU beds, a large number which is not met by the same large number of anesthesia residents leaving a shortage in covering the day and night shifts which compensated by extending the working hours to 24–36 hrs.
The current study evaluated effect of sleep deprivation following night shifts on the resident’s some cognitive functions such as RT, alertness, rapid problem solving and psychomotor skills using PVT, TMT that provides information on visual search, scanning, speed of processing, mental flexibility, and executive functions, KSS that measures day time sleepiness and gives subjective assessment of the subject’s level of drowsiness at the time, and ESS that measures chance of dozing, fatigue, and day time sleepiness. Fifty residents were selected ranging in age between 25 and 28 years old including juniors and seniors with full-time residency program in Kasr Al-Aini teaching hospitals.
Mean sleeping hours at home were 7.16 ± 1.390 hrs, which reduced only to 2.88 ± 1.081 hrs during the night shift. The study found that there was a significant decrease in PVT mean RT post-shift 371.9 ± 55.4 ms as compared to pre-shift mean RT 302.1 ± 35.2 ms (P value < 0.001), which is highly significant and therefore correlates with deteriorated alertness, slower problem-solving, and declined psycho-motor skills of residents following overnight shift.
KSS pre-shift mean score changed from 3.34 ± 1.189 to 6.24 ± 1.589 (P value < 0.001) reveals the increase fatigue, decreasing alertness, and increased drowsiness along with working night shifts.
Another subjective assessment of daytime sleepiness following night-shift was done using ESS. The results showed higher scores post night-shift than scores reported in pre-shift, which denoted increased the day time sleepiness, increased chance of dozing and drowsiness following night-shift when compare to earlier results with an average increase 8.18, mean score pre-shift was 6.68 ± 2.759 and mean score post night-shift was 14.86 ± 3.42 (P value < 0.001).
Regarding results of TMT A and B types, which provide information on visual search, scanning, speed of processing, mental flexibility, and executive functions, found that there was decrease in results of both, type A and B in post night-shift 44.86 ± 9.370 s, 72.60 ± 12.294 s, respectively, when compared to pre-shift 38.82 ± 8.458 s, 63.16 ± 11.557 s, respectively (P value < 0.001).
In consistence to the current study, Saadt et al. [Citation18] reported prolongation in RT using PVT in 21 anesthesiologists after a 17-hrs night call duty, 266.58 ± 38.35 ms vs. 297.76 ± 83.75 ms in a regular day (P value = 0.047)
Similarly, Basner et al. [Citation39] studied the effect of sleep deprivation on alertness on 137 interns and 87 PGY-2/3 residents using PVT& KSS to evaluate RT, the number of attentional lapses, and subjective sleepiness that were all negatively affected significantly in the morning after on‐call night shifts compared to daytime shifts.
Banks et al. [Citation40] induced Neurobehavioral deficits on 142 individuals through 5 nights of sleep restricted to 4 hours. Using PVT as primary, they found improvement in these Neurobehavioral deficits after 1 of 6 recovery sleep doses (0, 2, 4, 6, 8, or 10 hrs TIB) for 1 night. The improvement showed dose–response relationship with increasing sleep durations in a single night.
Saxena et al. [Citation41] also found that the overall median RT was significantly slower in the internal medicine residents after night shift (264.7 ± 102.9 ms) vs. day time shift (239.2 ± 26.1 ms) (P value < .001).
In contrast to the current study, Reinke et al. [Citation42] assessed the effect of chronotype on the performance, sleepiness, and fatigue of 96 ICU nurses during morning and night shifts. They found that although fatigue and increased sleepiness, vigilance did not change significantly between participants during the night shift as mean RT during night shift was 403.37 ± 44.59 ms vs. mean RT during morning shift 431.90 ± 70.63 ms with (P value = 0.1282), owing these results to the adaptive ability. These different results may be due to using a longer version of PVT, performing the test during the shift, the effect of chronotype, and less working hours during the night shift.
In agreement with the current regarding KSS, Åkerstedt et al. [Citation43] measured the subjective sleepiness as a sensitive indicator of sufficient sleep in different studies, during the first night shift for a number of studies. The night shift pattern is very similar across studies; early values of approximately KSS = 2–4 develop into values of between 5.5 and 7.5 toward the end of the night shift.
Schwarz et al. [Citation44] studied the effect of partial sleep deprivation on fitness to drive to detect impairments related to sleepiness using different tools including KSS and they found that KSS was significantly higher after partial sleep deprivation (P value = 0.001)
Similar to our results, significant subjective daytime sleepiness after night calls were reported in different residency programs and jobs using ESS. Richter et al. [Citation45] found that the number of extended work shifts was associated with increased daytime sleepiness among Anesthesiologists and intensivists working in French public hospitals, as twice as general population. Arab et al. [Citation46] found similar results regarding the fatigue in approximately 70% of residents after night calls with (P value = 0.01), in spite of the difference in the residency program that limit working hours to 208 hrs per month; that is 52 hrs per week in a 4-week month. Kato et al. [Citation47] evaluated sleepiness during shift work in Japanese nurses, they found mean JESS score was 10.4 ± 3.6; scores were significantly higher in shift workers than those in non-shift workers (P value > 0.05). Murthy et al. [Citation48] assessed subjective sleep quality, day-time sleepiness using different tools including ESS, and they compared the findings between residents in clinical and para-clinical departments. They reported high levels of abnormal day-time sleepiness and less satisfaction with life in residents in clinical faculties compared to those in para-clinical faculties.
Using TMT, Suozzo et al. [Citation49] reported that the performance of the residents after a night on call was worse on the TMT A (P value = 0.016). However, their result of TMT B was insignificant. Titova et al. [Citation50] evaluated cognitive disturbance on 7143 middle-aged and elderly humans who had a shift work history and they showed poorer performance on the TMT.
7. Limitations
We haven’t assessed the adverse effects of sleep deprivation on resident’s health, different body systems, and vital signs before and after the night shift.
We haven’t assessed the effect on patients’ outcome.
8. Recommendations
Further studies are recommended to assess the cognitive functions at the end of the whole working hours which extend beyond the 24 hrs shift.
Assessment of the cognitive functions every 8 hrs to determine the exact timing of beginning of cognitive functions decline.
Limit the working duration according to the mean time of beginning of cognitive functions decline.
9. Conclusion
The current study concluded that sleep deprivation in night-shifts not only increases the day-time sleepiness, but also affects the residents’ cognitive processes such as RT, alertness, rapid problem solving, psychomotor skills, attention, mental flexibility, and executive functions The study found no correlation between the number of cases worked during the shift and degree of cognitive functions impairment.
10. Dedications
This work is dedicated to the souls of our beloved colleagues we have lost due to the laborious nature of our work; Dr Ibrahim Badran, who died in a car accident while driving after a long working shift, Dr Hisham El-Waly, Dr Margret Nabil, and Dr Ahmed El-Borg who died from heart attack during the working hours in the operating theatres. May your souls rest in peace.
Availability of data and material
The data that support the findings of this study are the possession of the Cairo University Hospital. However, data are available from the corresponding author upon reasonable request after permission from Cairo University.
Ethics approval and consent to participate
Ethics approval from the Cairo University Hospital Research Committee – Department of Anaesthesia was obtained (N-35-2017). Written informed consent was obtained from the participants before inclusion.
Consent for publication
Not applicable.
Acknowledgments
We would like to thank our professors and colleagues in the anesthesia department of Cairo University for their help and support.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Kuhn G. Circadian rhythm, shift work, and emergency medicine. Ann Emerg Med. 2001;37(1):88–98. 2001.
- Brendel DH, Reynolds CF, Jennings JR, et al. Sleep stage physiology, mood, and vigilance responses to total sleep deprivation in healthy 80-year-olds and 20-year-olds. Psychophysiology. 1990;27(6):677–685.
- Cheung V, Yuen VM, Wong GTC, et al. The effect of sleep deprivation and disruption on DNA damage and health of doctors. Anaesthesia. 2019;74(4):434–440.
- Yentis SM, Shinde S, Plunkett E, et al. Experiences of suicide amongst anaesthetists – an Association of Anaesthetists survey. Anaesthesia. 2019 Nov;74(11):1365–1373.
- Ohtonen P, Alahutra S. Mortality among Finnish anaesthesiologists from 1984–2000. Acta Anaesthesiol Scand. 2002;46(10):1196–1199.
- Shinde S, Yentis SM, Asanati K, et al. Guidelines on suicide amongst anesthetists 2019. Anesthesia 2019 Nov 14. https://doi.org/10.1111/anae.14890
- Budhiraja R, Quan SF. Sleep-disordered breathing and cardiovascular health. Curr Opin Pulm Med. 2005;11(6):501–506.
- Budhiraja R, Sharief I, Quan SF. Sleep disordered breathing and hypertension. JCSM. 2005;1(4):401–404.
- Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12(1):1–12.
- Josten EJC, JEE N-A-T, Thierry H. The effects of extended workdays on fatigue, health, performance and satisfaction in nursing. J Adv Nurs. 2003;44(6):643–652.
- Barger LK, Ayas NT, Cade BE, et al. Impact of extended-duration shifts on medical errors, adverse events, and attentional failures. PLoS Med. 2006;3(12):e487.
- Satterfield BC, Wisor JP, Field SA, et al. TNFa G308A polymorphism is associated with resilience to sleep deprivation-induced psychomotor vigilance performance impairment in healthy young adults. Brain Behav Immun. 2015;31:66–74.
- Loh S, Lamond N, Dorrian J, et al. The validity of psychomotor vigilance tasks of less than 10-minute duration. BehavRes Methods Instrum Comput. 2004;36(2):339–346.
- Kaida K, Takahashi M, Åkerstedt T, et al. Validation of the Karolinska sleepiness scale against performance and EEG variables. Clin Neurophysiol. 2006 Jul 1;117(7):1574–1581.
- Johns MW. A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep. 1991;14(6):540–545.
- Kaminska M, Jobin V, Mayer P, et al. The Epworth Sleepiness Scale: self administration versus administration by the physician, and validation of a French version. Can Respir J. 2010;17(2):e27–e34.
- Tombaugh TN. Trail Making Test A and B: normative data stratified by age and education. Arch Clin Neuropsychol. 2004;19(2):203–214.
- Saadat H, Bissonnette B, Tumin D, et al. Effects of partial sleep deprivation on reaction time in anesthesiologists. Cravero J, editor. Pediatr Anesthesia. 2017 Apr 1;27(4):358–362.
- McCormick F, Kadzielski J, Landrigan CP, et al. Surgeon fatigue: a prospective analysis of the incidence, risk, and intervals of predicted fatigue-related impairment in residents. Arch Surg. 2012;147(5):430–435.
- Arora VM, Georgitis E, Woodruff JN, et al. Improving sleep hygiene of medical interns: can the sleep, alertness, and fatigue education in residency program help? Arch Intern Med. 2007;167(16):1738–1744.
- Amirian I, Andersen LT, Rosenberg J, et al. Working night shifts affects surgeons’ biological rhythm. Am J Surg. 2015;210(2):389–395.
- Anderson C, Sullivan JP, Flynn-Evans EE, et al. Deterioration of neurobehavioral performance in resident physicians during repeated exposure to extended duration work shifts. Sleep. 2012;35(8):1137–1146.
- Lockley SW, Cronin JW, Evans EE, et al. Effect of reducing interns’ weekly work hours on sleep and attentional failures. N Engl J Med. 2004;351(18):1829–1837.
- Dawson D, Reid K. Fatigue, Alcohol and performance impairment. Nature. 1997;388:235.
- Maruff P, Falleti MG, Collie A, et al. Fatigue-related impairment in the speed, accuracy and variability of psychomotor performance: comparison with blood alcohol levels. J Sleep Res. 2005;14(1):21–27.
- Rothschild JM, Keohane CA, Rogers S, et al. Risks of complications by attending physicians after performing nighttime procedures. JAMA. 2009;302(14):1565–1638.
- Taffinder NJ, McManus IC, Gul Y, et al. Effect of sleep deprivation on surgeons’ dexterity on laparoscopy simulator. Lancet. 1998;352(9135):1191.
- Morris GP, Morris RW. Anaesthesia and fatigue: an analysis of the first 10 years of the Australian Incident Monitoring Study 1987-1997. Anaesth Intensive Care. 2000;28(3):300–304.
- Lindfors PM, Nurmi KE, Meretoja OA, et al. On-call stress among Finnish anaesthetists. Anaesthesia. 2006;61(9):856–866.
- Meretoja OA. We should work less at night. Acta Anaesthesiol Scand. 2009;53(3):277–279.
- Lindfors PM, Meretoja OA, Luukkonen RA, et al. Suicidality among Finnish anaesthesiologists. Acta Anaesthesiol Scand. 2009;53(8):1027–1035.
- Reddy R, Guntupalli K, Alapat P, et al. Sleepiness in medical ICU residents. Chest. 2009;135(1):81–85.
- Gander P, Millar M, Webster C, et al. Sleep loss and performance of anaesthesia trainees and specialists. Chronobiol Int. 2008;25(6):1077–1091.
- Rauchenzauner M, Ernst F, Hintringer F, et al. Arrhythmias and increased neuro-endocrine stress response during physicians’ night shifts: a randomized cross-over trial. Eur Heart J. 2009;30(21):2606–2613.
- Malmberg B, Persson R, Jo ¨nsson BAG, et al. Physiological restitution after night-call duty in anaesthesiologists: impact on metabolic factors. Acta Anaesthesiol Scand. 2007;51:823–830.
- Kohn LT, Corrigan JM, Donaldson MS. To err is human: building a safer health system. Washington, DC: National Academy of Science, Institute of Medicine, 2002. ISBN 978-0-309-06837-6. 10.17226/9728.
- National Sleep Foundation. State of the States Report on Drowsy Driving. Washington, D.C.: national Sleep Foundation. 2008. http://drowsydriving.org/resources/2008state-of-the-states-report-on-drowsy-driving Accessed on 2016 Apr 14
- Caldwell JA Jr, Caldwell JL, Brown DL, et al. The effects of 37 hours of continuous wakefulness on the physiological arousal, cognitive performance, self-reported mood, and simulator flight performance of F-117A pilots. Mil Psychol. 2004;16(3):163.
- Basner M, Dinges DF, Shea JA, et al. Sleep and Alertness in Medical Interns and Residents: an Observational Study on the Role of Extended Shifts. Sleep. 2017 Apr 1;40(4):4.
- Banks S, HPA VD, Maislin G, et al. Neurobehavioral Dynamics Following Chronic Sleep Restriction: dose-Response Effects of One Night for Recovery. Sleep. 2010 Aug 1;33(8):1013–1026.
- Saxena AD, George CFP. Sleep and motor performance in on-call internal medicine residents. Sleep. 2005 Nov;28(11):1386–1478.
- Reinke L, Özbay Y, Dieperink W, et al. The effect of chronotype on sleepiness, fatigue, and psychomotor vigilance of ICU nurses during the night shift. Intensive Care Med. 2015;41(4):657–724. 12.
- Åkerstedt T, Anund A, Axelsson J, et al. Subjective sleepiness is a sensitive indicator of insufficient sleep and impaired waking function. J Sleep Res. 2014;23(3):242–297. 1.
- Johanna FA, Schwarz PG, Hajak G, et al. The effect of partial sleep deprivation on computer-based measures of fitness to drive. Sleep Breathing. 2016;20(1):285–292.
- Richter E, Blasco V, Antonini F, et al. Sleep disorders among French anaesthesiologists and intensivists working in public hospitals: A self-reported electronic survey. Eur J Anaesthesiol. 2015;32(2):132–140.
- Arab AA, Khayyat HY. Risk of fatigue among anesthesia residents in Saudi Arabia. Saudi Med J. 2017;38(3):292–296.
- Kato C, Shimada J, Hayashi K. Sleepiness during shift work in Japanese nurses: A comparison study using JESS, SSS, and actigraphy. Sleep Biol Rhythms. 2012;10(2):109–126.
- Murthy V, Nayak A. Assessment of sleep quality in post-graduate residents in a tertiary hospital and teaching institute. Ind Psychiatry J. 2014;23(1):23–26.
- Suozzo AC, Malta SM, Gil G, et al. Attention and memory of medical residents after a night on call: a cross-sectional study. Clinics. 2011;66(3):505–513.
- Titova OE, Lindberg E, Elmståhl S, et al. Association between shift work history and performance on the trail making test in middle-aged and elderly humans: the EpiHealth study. Neurobiol Aging. 2016;45:23–29.