ABSTRACT
Background
A reflex sympathoadrenal response could be elicited by laryngoscopy and intubation in the form of tachycardia and hypertension. These responses could be attenuated to decrease cardiac work and oxygen demands. This study was conducted to assess the role of oral gabapentin in decreasing the stress response associated with intubation.
Objective
This study was conducted to assess the role of oral gabapentin in decreasing the stress response associated with intubation.
Patients and methods
A total of 70 cases who underwent intracranial surgery in Mansoura University Hospitals were included. They were divided into two groups; group C who received placebo, and group G who received gabapentin 1000 mg orally. Heart rate, blood pressure, and catecholamine levels were measured prior to intubation, then after 1, 5, 10, and 15 minutes.
Results there is no correction
When given 1 hr prior to surgery, gabapentin effectively attenuated blood pressure, heart rate, and catecholamine levels compared to the placebo after intubation, although no statistical differences were detected statistically before intubation.
Conclusion
Pre-treatment with 1000 mg oral gabapentin before induction of anesthesia is both safe and effective in reducing the stress response to laryngoscopy and intubation.
1. Introduction
Endotracheal intubation is considered an integral part of the anesthesiologist’s contribution in patient care. However, it is a noxious stimulus that may initiate a transient sympathetic response in the form of increased heart rate, blood pressure, and arrhythmias. Moreover, this response may be marked in some cases [Citation1].
Multiple measures have been used to decrease this stress response upon intubation including; lidocaine spray, deepening of anesthesia, intravenous lignocaine, opioids, sodium nitroprusside, nitroglycerine ointment, or oral clonidine [Citation2].
Gabapentin belongs to the second generation of anticonvulsant agents that are also effective in the management of neuropathic pain. It acts by decreasing the synthesis of glutamate in the CNS. Also, it can bind to voltage-gated calcium channels (alpha 2 delta subunits). Nevertheless, it does not inhibit GABA uptake or degradation although it has a structural mimicry to it [Citation3].
In the current literature, there is a growing evidence that pre-operative administration of analgesics has a greater impact on preoperative anxiolysis, stress response attenuation, and postoperative analgesia [Citation4].
Recently, gabapentin was successfully used to attenuate the hemodynamic stress response to endotracheal intubation [Citation5].
This study was conducted to evaluate the effect of preoperative intake of gabapentin on the stress response to laryngoscopy and intubation in intracranial surgeries.
2. Patients and methods
2.1. Study design
This is a prospective double-blinded, randomized, and controlled study that was conducted at the Mansoura University Anesthesia Department to evaluate the outcome of oral gabapentin intake on the laryngoscopic stress response.
2.2. Study cases
A total of 70 cases who underwent intracranial surgery were included in the study and they were divided randomly into two equal groups by sealed envelope method; Group C included 35 cases who received the placebo, while group G included the remaining 35 cases who received 1000 mg of oral gabapentin 1 hr prior to the operation.
2.3. Patient consent
A written informed consent was obtained from all cases before participating in our study after the explanation of the advantages and drawbacks of the tested drug. Moreover, the study was approved by the local ethical committee (IRB) with a reference number R.20.01.708 at 14/1/2020.
2.4. Inclusion criteria
American Society of Anesthesiologists (ASA) physical status: Ι-Ш
Age: 20–60 years.
Gender: either sex.
Patients with Glasgow coma scale score above 10/15.
2.5. Exclusion criteria
Patient’s refusal.
Any known allergy or contraindication to drugs used.
Pregnancy, lactating mother, and children.
Subjects who were sleepy or hypotensive within 24 hours before surgery.
Severe uncompensated diseases (cardiac, respiratory, hepatic, or renal disease).
Morbidly obese patients.
Significant gastrointestinal disorders (e.g. peptic ulcer disease or gastroesophageal reflux disease).
2.6. Patient preparation
A: The day before surgery:
Patients were kept fasting for 8 hours.
In the preoperative visit: all patients were evaluated for (full medical and clinical examination including the manifestation of increased intracranial tension, Glasgow coma scale, ECG, and routine pre-operative laboratory investigations).
B: The day of surgery:
On arrival to the preanesthetic room, all patients were placed in supine position then a wide bore (18 G) intravenous cannula was inserted into a suitable peripheral vein then 5 ml/kg of normal saline was infused.
Baseline data were recorded as HR and NIBP. Additionally, a blood sample was taken for the measurement of adrenaline and noradrenaline levels by using Human Epinephrine and Norepinephrine ELISA Kit from Bioassay Technology Laboratory from SHANGHAI CRYSTAL DAY BIOTECH CO., LTD. All these parameters were measured and recorded before induction of general anesthesia (basal), at induction, and then 1 minute, 5 minutes, 10 minutes, and 15 minutes after intubation, respectively.
After pre-oxygenation, anesthesia was induced with injection of Fentanyl 1 μg/kg, propofol 1.5–2.5 mg/kg and atracurium 0.5 mg/kg to facilitate intubation. Patient was intubated with appropriately sized tube. Laryngoscopy and intubation time were kept minimum (15 sec). If more than 3 attempts of laryngoscopy were done, the patient was excluded from our study.
Anesthesia was maintained by oxygen 30% in air mixture, isoflurane (MAC = 1.2), and atracurium at incremental doses 0.1 mg/kg every 20 minutes. Volume controlled mode of mechanical ventilation was attained. Minute volume was modified to keep end-tidal CO2 about 35 mm Hg. High flow>0.5-minute volume was used for 20 minutes after induction and before extubation while low flow was used all through the procedure.
Warm saline 0.9% was infused to keep CVP about 5 mm Hg. Blood was transfused in a trial to keep HB ≥10 gm/dl or HCT about 30% mannitol (20%) 1 gm/kg during craniotomy via central line.
At the end of surgery, residual neuromuscular blockade was reversed using the injection of neostigmine 0.05 mg/kg and atropine 0.02 mg/kg, and the patient was extubated and then transferred to the surgical intensive care.
2.7. Sample size calculation
The power of this clinical trial was prospectively calculated using the G Power analysis program version 3. Using priory power analysis with accuracy mode calculations with catecholamine level as the primary variant and assuming type-I error protection of 0.05 and an effect size convention of 0.8, a total sample size of 70 patients produced a power of 0.90.
2.8. Data analysis
IBM’s SPSS statistics (Statistical Package for the Social Sciences) for windows (version 25, 2017) was used for statistical analysis of the collected data. Shapiro–Wilk test was used to check the normality of the data distribution. All tests were conducted with 95% confidence interval. P (probability) value <0.05 was considered statistically significant. Charts were generated using SPSS’ chart builder and Microsoft Excel for windows 2019. Quantitative variables were expressed as mean and standard deviation while categorical variables were expressed as frequency and percentage. Independent sample T and Mann Whitney tests were used for inter-group (between subjects) comparison of parametric and non-parametric continuous data with no follow-up readings, respectively. For pair-wise comparison of data (within subjects), the follow-up values were compared to their corresponding basal value using paired samples T-test or Wilcoxon matched-pairs signed ranks test. Fisher exact and Chi-square tests were used for inter-group comparison of nominal data using the crosstabs function.
3. Results
The mean age of the included cases was 39.69 and 43.40 years for the control and gabapentin groups, respectively. In the control group, 20 males and 15 females were included, whereas the gabapentin group included 15 males and 20 females. Diabetes was present in six cases (17%) in the control group, while it was present in five cases (14%) in the gabapentin group. In addition, hypertension was present in 13 cases (37%) and 10 cases (39%) in both groups, respectively. None of the previously discussed variable was significantly different between the two study groups (p > 0.05). The laryngoscopy duration did not differ significantly between the two groups (p = 0.75). These data are illustrated in .
Table 1. Demographic data, medical history, RAAS, and intubation time in both groups.
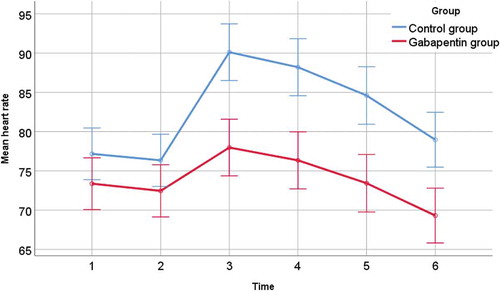
There was a significant variation in the heart rate throughout follow-up period (F = 201.5, df 2.62, P = <0.001). There was a significant variation due to the treatment regimen between groups (F = 42.15, df 2.62, P = <0.001). In average, the overall readings of Gabapentin group were significantly lower than those of Control group by an average of 8.75 throughout the study (95% CI: 3.92, 13.58, p = <0.001).
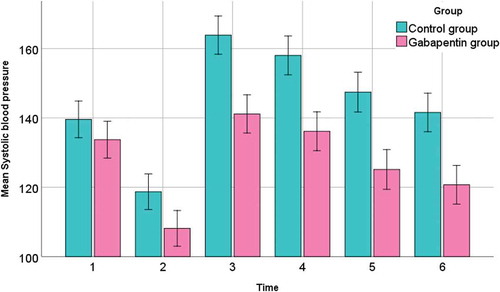
There was a significant variation in the SBP throughout follow-up period (F = 574.6, df 2.59, P = <0.001). There was a significant variation due to the treatment regimen between groups (F = 40.82, df 2.59, P = <0.001). In average, the overall readings of Gabapentin group were significantly lower than those of Control group by an average of 17.36 throughout the study (95% CI: 9.89, 24.82, p = <0.001).
There was a significant variation in the DPB throughout follow-up period (F = 43.64, df 5, P = <0.001). There was a significant variation due to the treatment regimen between groups (F = 5.5, df 5, P = <0.001). In average, the overall readings of Gabapentin group were significantly lower than those of Control group by an average of 10.95 throughout the study (95% CI: 6.16, 15.75, p = <0.001). These data are shown in and and .
Table 2. Basal and follow-up hemodynamics of both groups.
By comparing basal and follow-up values of the vital signs in both groups, we noticed reduced elevation in the three parameters (HR, SBP, DBP) in the Gabapentin group after the intubation compared to the control group. It is worth mentioning that the follow-up reading in the Gabapentin group dropped below the basal level at some instances, unlike the control group which remained above the baseline at all times.
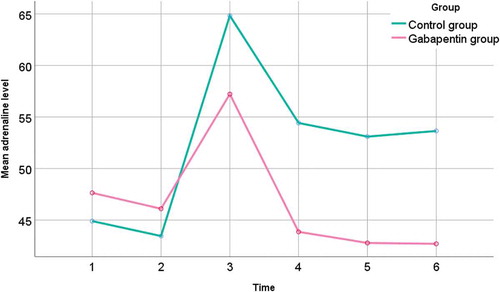
There was a significant variation in the adrenaline throughout follow-up period (F = 140.7, df 1.64, P = <0.001). There was a significant variation due to the treatment regimen between groups (F = 44.9, df 1.64, P = <0.001). In average, the overall readings of Gabapentin group were significantly lower than those of Control group by an average of 5.67 throughout the study (95% CI: 0.91, 10.43, p = 0.020).
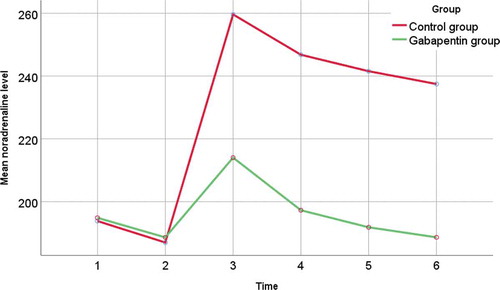
There was a significant variation in the noradrenaline throughout follow-up period (F = 391, df 1.29, P = <0.001). There was a significant variation due to the treatment regimen between groups (F = 197.8, df 1.29, P = <0.001). In average, the overall readings of Gabapentin group were significantly lower than those of Control group by an average of 31.84 throughout the study (95% CI: 27.97, 35.71, p = <0.001). These data are illustrated in and and .
Table 3. Basal and follow-up adrenaline and noradrenaline of both groups.
Within-subject comparison revealed a significant statistical difference between basal value and subsequent readings at all time points for the adrenaline in both groups and for noradrenaline in the control group; however, the gabapentin group reading of the noradrenaline starting from 2 minutes after induction did not show significant statistical variation.
4. Discussion
Gabapentin, which is a structural analogue for GABA (Gamma aminobutyric acid), is widely used in the treatment of seizures, neuropathic pain, and hot flushes. A recent evidence has suggested that it is useful in decreasing the stress response associated with laryngoscopy and intubation [Citation6].
Several workers have found that 300–1200 mg oral gabapentin given 1 hr before surgical stimulus significantly reduces the incidence of pain and postoperative opioid consumption without significant side effects [Citation7].
This study was conducted at Mansoura University Hospitals aiming to assess the effectiveness of gabapentin in the attenuation of hemodynamic stress response to laryngoscopy and intubation.
A total of 70 cases were included, and they were divided into two groups; group C included the controls who received the placebo, while the remaining 35 cases received oral gabapentin 1 hr before surgery. There were no significant differences regarding the demographics between our two study groups (p > 0.05).
Another Egyptian study handling the same perspective included 50 cases who were divided into two equal groups. The authors did not report any significant differences between the two groups regarding demographics [Citation6]. This comes in line with our study results.
The present study demonstrated that a single oral dose of gabapentin before surgery attenuated the hemodynamic stress response to intubation in adults. Moreover, it was successful in attenuation of both epinephrine and norepinephrine levels.
Our results agree with the results published by Memis and his colleagues who reported that the administration of an oral single dose of 400–800 mg gabapentin was significantly successful in reducing mean arterial blood pressure and heart rate during the first 10 minutes after intubation [Citation8].
Doddaiah and his associates found that oral 800 mg of gabapentin attenuated both blood pressure and heart rate at 1 and 5 minutes after intubation [Citation9].
Another study has reported that administration of 1600 mg of oral gabapentin (divided into 4 doses) successfully attenuated the pressor response. However, heart rate was not significantly reduced [Citation10].
In another study, oral gabapentin 1000 mg 1 hr prior to surgery resulted in a significant decrease in mean arterial pressure and heart rate during the study period (p < 0.05). Moreover, the effect was found to be dose-dependent [Citation3].
Kaya and coworkers had studied the effect of preoperative gabapentin 800 mg, given 2 h before surgery on intraocular pressure (IOP) and hemodynamic changes in response to endotracheal intubation and concluded that pretreatment with gabapentin 800 mg effectively suppressed the increase in intraocular pressure and attenuated the increase in the MAP but not the HR associated with tracheal intubation [Citation11].
Ayatollahi and his colleagues have reported that administration of 800 mg of oral gabapentin 1.5 hours prior to surgery was effective in the attenuation of both diastolic and mean arterial pressure. However, both systolic blood pressure and heart rate were not significantly affected [Citation12].
Ifthekahar et al. noticed that the mean arterial pressure was the only variable significantly attenuated by oral 800 mg of gabapentin [Citation13]. Both these workers concluded that gabapentin was ineffective in preventing tachycardia following laryngoscopy. This contradicts with our study findings, but it may be due to different dosages or different surgical operations.
The previously mentioned Egyptian study also reported that gabapentin had failed to decrease catecholamine levels in response to intubation [Citation6]. The results of this study suggest that gabapentin may decrease blood pressure and heart rate without affecting catecholamine secretion. The important determinant of the level of arterial pressure to tracheal intubation may be reactivity to norepinephrine and not the plasma concentration [Citation14].
However, gabapentin was significantly effective in attenuating catecholamine levels compared to our study controls.
A previous study has evaluated the role of gabapentin in decreasing catecholamine release from the chromaffin cells, which are the predominant source of these chemical compounds. Gabapentin did not alter the catecholamine content of the chromaffin cells but produced a statistically significant reduction in secretion evoked by cholinergic agonists or by direct membrane depolarization [Citation15].
The mechanism by which gabapentin attenuates this stress response is still unknown. However, its binding to the calcium-gated channels in the dorsal root ganglia may have a role [Citation2].
The main drawback regarding this study is that it included a relatively small sample size. Therefore, multiple studies including more cases should be conducted in the near future.
5. Conclusion
Pre-treatment with 1000 mg oral gabapentin before induction of anesthesia is both safe and effective in reducing the stress response to laryngoscopy and intubation.
References
- Gehlot RK. Attenuation of pressor response to laryngoscopy and intubation: dexmedetomidine Vs. fentanyl premedication. Indian J Clin Anaesth. 2018;5(4):486–490.
- Aggarwal S, Baduni N, Jain A. Attenuation of pressor response to laryngoscopy and intubation–a comparative study between two doses of gabapentin in patients undergoing laparoscopic cholecystectomy. Anaesthesia, Pain & Intensive Care; 2019. p. 33–36.Apicareonline.
- Bafna U, Goyal VK, Garg A. A comparison of different doses of gabapentin to attenuate the haemodynamic response to laryngoscopy and tracheal intubation in normotensive patients. J Anaesthesiol Clin Pharmacol. 2011;27(1):43.
- Singh D, Yadav JS, Jamuda BK, et al. Oral pregabalin as premedication on anxiolysis and stress response to laryngoscopy and endotracheal intubation in patients undergoing laparoscopic cholecystectomy: A randomized double-blind study. Anesth Essays Res. 2019;13(1):97.
- Hossain MS, Rashid MM, Islam SA. et al. Comparative study of oral clonidine versus gabapentin as premedication for anxiolysis, sedation and attenuation of pressor response to laryngoscopy and tracheal intubation. Anwer Khan Mod Med Coll J. 2018;9(2):131–136.
- Ali AR, El Gohary M, Ashmawi H, et al. Efficacy of preoperative oral gabapentin in attenuation of neuro-endocrine response to laryngoscopy and endotracheal intubation. J Med Sci. 2009;9(1):24–29.
- Shrestha B, Gautam B, Shrestha S, et al. Study of haemodynamic and endocrine stress responses following carbon dioxide pneumoperitonium. J Nepal Health Res Counc. 2012;10(20):41-6.
- Memiş D, Turan A, Karamanlıoğlu B, et al. Gabapentin reduces cardiovascular responses to laryngoscopy and tracheal intubation. Eur J Anaesthesiol. 2006;23(8):686–690.
- Doddaiah DB, Singh NR, Fatima N, et al. A comparative study of oral pregabalin and oral gabapentin in the attenuation of hemodynamic response to laryngoscopy and intubation. J Med Soc. 2017;31(1):14.
- Fassoulaki A, Melemeni A, Paraskeva A, et al. Gabapentin attenuates the pressor response to direct laryngoscopy and tracheal intubation. Br J Anaesth. 2006;96(6):769–773.
- Kaya F, Yavascaoglu B, Baykara M, et al. Effect of oral gabapentin on the intraocular pressure and haemodynamic responses induced by tracheal intubation. Acta Anaesthesiol Scand. 2008;52(8):1076–1080.
- Ayatollahi V, Mirshamsi P, Behdad S, et al. Effect of oral gabapentin on haemodynamic variables during microlaryngoscopic surgery. Anaesthesiol Intensive Ther. 2014;46(1):17–22.
- Iftikhar T, Taqi A, Sibtain A, et al. Oral gabapentin reduces hemodynamic response to direct laryngoscopy and tracheal intubation. Anaesth Pain Intensive Care. 2011;15(1):17–20.
- Sundar AS, Kodali R, Sulaiman S, et al. The effects of preemptive pregabalin on attenuation of stress response to endotracheal intubation and opioid-sparing effect in patients undergoing off-pump coronary artery bypass grafting. Ann Card Anaesth. 2012;15(1):18.
- Todd RD, McDavid SM, Brindley RL, et al. Gabapentin inhibits catecholamine release from adrenal chromaffin cells. Anesthesiol J Am Soc Anesthesiologists. 2012;116(5):1013–1024.
Disclosure statement
No conflict of interest emerged during the implementation of this work. The paper had not been presented at any congress before.