ABSTRACT
Background
This trial aimed to evaluate the effect of the use of triple the ED95 of rocuronium and vecuronium on the onset of relaxation and the intubation score in morbidly obese patients.
Methods
Sixty adult morbidly obese patients were included in this trial and were randomly assigned according to the muscle relaxants used to the ROC group, in which patients received rocuronium (0.9 mg/kg), and VEC group, in which the patients received vecuronium (0.15 mg/kg). The onset and duration of relaxation, the time of intubation, and the intubation scores were assessed. Additionally, the response of hemodynamic parameters to the injection of muscle relaxants and to the intubation was recorded.
Results
The onset of relaxation was significantly lower in ROC group (57.5 ± 19.9 sec) than in VEC group (105.0 ± 18.8 sec) (P < 0.0001). Additionally, the time for intubation was significantly shorter in ROC group (69.00 ± 19.4 sec) than in VEC group (120.8 ± 17.7 sec) (P < 0.0001). Moreover, there was a significant increase in the duration of relaxation in ROC group (85.5 ± 19.2 min) compared with VEC group (72.00 ± 22.65 min) (P = 0.016). However, there was no significant difference between the two groups in the intubation score (P = 0.656) and the changes in the hemodynamic parameters (P > 0.05).
Conclusion
The use of triple the ED95 of rocuronium in morbidly obese patients significantly shortened the onset of relaxation and the timing of intubation compared to vecuronium. However, the intubation score and the hemodynamic changes during intubation were comparable.
1. Introduction
Rapid sequence induction may be defined as the act of minimizing the time elapsed between the loss of protective airway reflexes and inflation of the endotracheal tube cuff [Citation1]. Rapid sequence induction is widely used in anesthetic practice in urgent and emergent procedures [Citation2]. Additionally, this method is used in elective procedures in patients with an increased risk of aspiration, such as patients with gastroesophageal reflux, pregnancy, or obesity [Citation3]. Succinylcholine has traditionally been used in rapid sequence induction techniques due to its rapid onset and short duration of action. However, its use has been limited by the potential side effects associated with its use [Citation4].
Nondepolarizing neuromuscular blocking agents, such as pancuronium, vecuronium, atracurium, and cisatracurium, may be alternative agents to succinylcholine. However, these blocking agents have a delayed onset and a prolonged duration of action when used in the standard doses [Citation5]. Rocuronium has a rapid onset of action and a moderate duration of action and can be used in rapid sequence induction [Citation6]. The development of sugammadex has allowed the evaluation of the use of the steroid group of the nondepolarizing neuromuscular blocking agents in rapid sequence induction, as sugammadex allows the rapid reversal of these nondepolarizing neuromuscular blocking agents in cases of failed intubation [Citation7,Citation8]. The clinical trial by Duarte et al revealed that the ideal body weight (IBW) should be used in the calculation of a sugammadex dose in the reversal of a moderate neuromuscular block in morbidly obese patients [Citation9].
The use of triple the 95% mean effective dose (ED95) of rocuronium or vecuronium may shorten the time of onset of intubation and facilitate the intubation process as early as possible. This clinical trial aimed to compare the use of triple the ED95 of rocuronium with that of vecuronium in rapid sequence induction of morbidly obese patients undergoing laparoscopic bariatric surgeries. The primary outcome was the onset of relaxation, and the secondary outcome was the intubation score.
2. Material and methods
This randomized double-blind clinical trial was conducted at Tanta University Hospitals after being approved by the Research Ethics Committee of the Faculty of Medicine at Tanta University, with an approval number of 32,142/02/2018. Then, the trial was registered prior to patient enrollment in the Pan-African Clinical Trial Registry, with an identification number of PACTR201804003260153 (Principle investigator: Sameh Abdelkhalik Ahmed, Date of registration: 5 February 2018). Informed written consent was obtained from the patients who had agreed to participate in the research study. The study lasted for 18 month (February 2018-July 2019).
Morbidly obese patients who had a body mass index (BMI) ranging from 40–50 kg/m2, were aged between 25 and 45 years, were classified as American Society of Anesthesiologists class (ASA class) III and were scheduled for laparoscopic bariatric surgeries were included in this study. Patients who refused to participate in this research study, were pregnant or lactating, or had a BMI greater than 50 kg/m2 were excluded from the study. Additionally, the patients with major cardiac, pulmonary, hepatic, or renal comorbidities were excluded from the study.
Patients were randomly allocated by computer software into two groups of equal size: the ROC Group, for whom endotracheal intubation was facilitated by rocuronium (0.9 mg/kg) ideal body weight (IBW), and the VEC Group, for whom vecuronium (0.15 mg/kg) IBW was used for the facilitation of intubation.
An anesthetist who did not participate in the study helped prepare the neuromuscular blocking agents in uniform syringes and placed them in a sealed envelope.
Patients were connected to a basic monitoring system consisting of five leads for the electrocardiogram (ECG), a pulse oximeter, and noninvasive device for blood pressure (Datex-Ohmda Avance CS2, USA) once they were admitted to the operating room. Then, intravenous access was established with the peripheral insertion of a 20-gauge cannula and a fluid preload of 10 ml/kg of lactated ringer solution was introduced over 20 minutes.
The neuromuscular functions were monitored by acceleromyography (TOF-watch-SX, MSD BV, Oss, The Netherlands); the response of the adductor pollicis muscle was detected by two electrodes placed over the path of the ulnar nerve: the first was placed over the lateral side of the flexor carpi ulnaris muscle, and the second was placed 1 cm proximal to the wrist joint. A sensor was placed on the tip of the thumb to detect the contractions of the ipsilateral adductor pollicis muscle. The thumb was placed in a flexible adapter to generate preload while the rest of the hand was fixed. Calibration of the train-of-four monitor was carried out after the induction of anesthesia but before the injection of the muscle relaxants.
The patient was positioned in a ramped sniffing position, and anesthesia was induced after 5 minutes of preoxygenation using 80% oxygen through a well-fitted face mask with fentanyl (1.5 µg/kg IBW) and propofol (2 mg/kg IBW). Then, supramaximal stimulation by the train-of-four (TOF) monitor was delivered every 20 seconds until stable twitch heights that were considered as controls were obtained. Then, the preprepared intubating dose of nondepolarizing muscle relaxants was injected. Mask ventilation was continued until 95% suppression of the height of the twitches was achieved, and video laryngoscopy (C-Mac) was used to assess the intubation score, which is a score from a four-point scale: an excellent score: showing a relaxed jaw, abducted immobile vocal cords, and no diaphragmatic movement; a good score: showing a relaxed jaw, abducted immobile vocal cords, and some diaphragmatic movement; a poor score: showing a relaxed jaw, moving vocal cords, and coughing on intubation; and an inadequate score: not showing a relaxed jaw, showing adducted vocal cords, and intubation is impossible) [Citation10]. If the intubation score was excellent or good, a suitably sized endotracheal tube was inserted; however, if the intubation score was poor or inadequate, the face mask ventilation was continued and the trial of intubation was postponed for another 30 seconds until the score was good or excellent. After endotracheal intubation, the patients were connected to the mechanical ventilator of the anesthesia machine that was adjusted to protect the lung and to maintain the end-tidal CO2 between 32 and 36 mmHg. Additionally, recruitment maneuvers were used to maintain adequate aeration of the basal alveoli. General anesthesia was maintained by isoflurane 1.5% and an incremental dose of the nondepolarizing muscle relaxants.
The primary outcome of our study was the onset of relaxation, which represented the duration of time from when the neuromuscular blocking agents were injected to when 95% suppression of the height of the twitches was achieved. The secondary outcome was the intubation score in the first trial of video laryngoscopy. Furthermore, the time for intubation (the time elapsed between the intravenous administration of the muscle relaxants and successful intubation) was calculated and recorded. In addition, the duration of time for which the muscle relaxed, which was from the time at which 95% suppression of the TOF twitches was achieved to the time at which 25% of the twitch height was regained, was recorded. When failure of intubation occurred after two trials by an expert anesthesiologist, the muscle relaxation process was reversed by sugammadex 4 mg/kg (IBW), which could be repeated and by switching off the anesthesia until the patient regained spontaneous ventilation and a conscious level; these patients were excluded from the study.
The hemodynamic parameters, including heart rate and mean arterial blood pressure, were recorded just before the induction of anesthesia (baseline), after the induction of anesthesia but before the injection of the muscle relaxants, after the injection of the muscle relaxants but before intubation, after endotracheal intubation, and at the beginning of the surgery.
At the end of the surgery, the inhalational anesthesia was switched off. The muscle relaxation process was reversed by neostigmine 0.05 mg/kg (IBW) and atropine 0.01 mg/kg (IBW) when the TOF reached 70%. Awake tracheal extubation was performed by transferring the patients to the PACU for adequate postoperative oxygenation using a nasal cannula at a flow rate of 2–3 l/min and monitoring the patients. For postoperative analgesia, all the patients received 3 mg of morphine intravenously with 1 g paracetamol by IV infusion. Any adverse events that occurred from the induction of anesthesia until the discharge of the patient from the PACU, including oxygen desaturation (decrease SpO2 less than 90%), bronchospasm, or skin reactions, were recorded.
3. Statistical analysis
The sample size calculation was based on the results of a pilot study that was conducted in 10 patients (not included in the final study) randomly assigned to either the ROC or VEC group (5 patients in each). The results of the pilot study revealed that the onset of relaxation in the ROC group was 48.37 ± 32.83 sec and that in the VEC group was 102.76 ± 29.45 sec. Therefore, at least 27 patients were required in each group to detect a significant difference in the onset of intubation of 30 seconds between the two groups at an α value of 0.05 and 90% statistical power in the study. The statistical analysis of the recorded data was carried out by SPSS 17 (SPSS Inc., Chicago, IL, USA). The quantitative parameters were analyzed by an unpaired t-test and expressed as a mean and standard deviation. The categorical data were analyzed by Fisher’s exact test and represented as numbers and percent. The intubation score was analyzed by the chi-square test. The differences were considered significant when the P value was less than 0.05.
4. Results
Sixty-nine patients were assessed for eligibility to participate in this clinical study; 3 of the patients did not meet the inclusion criteria, and 6 of the patients declined to participate. Sixty patients were distributed randomly into the two study groups (30 patients in each). All the included patients received the allocated intervention, and their data were successfully obtained and analyzed (). The patient characteristics, including age, sex, and body mass index, showed statistically insignificant differences between the two groups (P 0.567, 0.432, and 0.207, respectively). Additionally, the type of surgery was not statistically different between the two groups (P = 0.347) ().
Table 1. Patients and surgical characteristics of the studied patients.
The onset of relaxation was significantly shorter in the rocuronium group than in the vecuronium group (P < 0.0001). Additionally, the time required for intubation was statistically significantly shorter in the rocuronium group than in the vecuronium group (P < 0.0001). Moreover, the duration of relaxation was statistically significantly longer in the rocuronium group than in the vecuronium group (P = 0.016). However, the intubation score was not statistically significant between the two groups (P = 0.656) ().
Table 2. Timing and duration of relaxation.
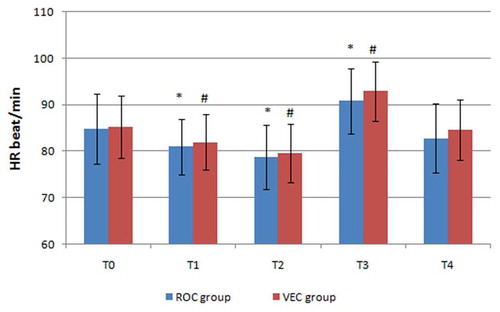
The mean values of the heart rate were not statistically different between the two groups before the induction of anesthesia, after the induction of anesthesia but before the injection of the muscle relaxants, after the injection of the muscle relaxants but before intubation, after intubation, and at the beginning of the surgery (P = 0.815, 0.533, 0.574, 0.222, and 0.311, respectively). In the two study groups and in comparison to the baseline values, the mean values of the heart rate were statistically decreased after the induction of anesthesia but before the injection of the muscle relaxants, significantly decreased after the injection of the muscle relaxants but before intubation (P < 0.05) and significantly increased after endotracheal intubation (P < 0.05) ().
Figure 2. Changes in the mean values of the heart rate in the two groups.
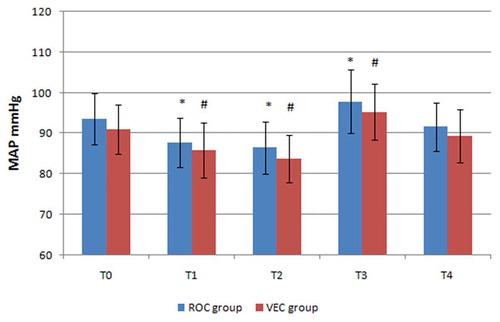
Moreover, the mean values of the mean arterial blood pressure were comparable between the two study groups before the induction of anesthesia, after the induction of anesthesia but before the injection of the muscle relaxants, after the injection of the muscle relaxants but before intubation, after intubation, and at the beginning of the surgery (P = 0.113, 0.263, 0.089, 0.187, and 0.166, respectively). Compared to the baseline values in the two groups, the mean arterial blood pressure was significantly decreased after the induction of anesthesia but before the injection of the muscle relaxants, significantly decreased after the injection of the muscle relaxants but before intubation (P < 0.05), and statistically significantly increased after endotracheal intubation (P < 0.05) (). The incidence of adverse events, including oxygen desaturation, and skin reactions, throughout the whole perioperative period was insignificant between the two groups (P = 0.999, and 0.612, respectively) ().
Figure 3. Mean arterial blood pressure changes in the two groups.
5. Discussion
The results of our clinical trial revealed that the use of triple ED95 of rocuronium allowed a faster onset of relaxation and timing of intubation than the use of vecuronium, with an insignificant difference in the intubation score, the incidence of complications, and the changes in the hemodynamic parameters. However, the use of rocuronium was associated with a longer duration of relaxation.
As rocuronium was the first nondepolarizing neuromuscular blocking agent to be evaluated in the rapid sequence induction of anesthesia, the optimal dose that can be used to allow safe endotracheal intubation within 60 seconds was assessed by Heier et al [Citation11], who evaluated a wide range of doses of rocuronium (0.4 to 2.0 mg/kg) and revealed that the doses of rocuronium that led to 90% and 95% probabilities of perfect intubation within 60 seconds were 1.85 and 2.33 mg/kg, respectively. The use of rocuronium in the rapid sequence induction of anesthesia was suggested by many clinical trials that compared the use of different doses of rocuronium to the use of suxamethonium, such as those by Singh et al [Citation12], Cooper [Citation13] et al, McCourt et al [Citation14], Sørensen et al [Citation15], Mazurek et al [Citation16], Sparr et al [Citation17], Williamson et al [Citation18], and Andrews et al. [Citation19] Certain clinical trials have suggested that rocuronium is not suitable for rapid sequence induction, such as those by Sluga et al [Citation6], Tran et al [Citation20], and Perry et al [Citation21], but these results can be explained by the use of smaller doses of rocuronium.
Chauvin et al revealed that the use of vecuronium at a dose of 0.1 mg/kg can lead to diaphragmatic paralysis faster than it can lead to adductor pollicis paralysis. Thus, vecuronium can be used in rapid sequence induction [Citation22]. The use of vecuronium in rapid sequence induction has been evaluated in many studies, such as the studies by Boulanger et al [Citation23], Cheng et al [Citation24], and Deepika et al. [Citation25]
The results of this clinical study were in agreement with those presented by Magorian et al, who found that larger doses of rocuronium allowed faster intubation than did vecuronium [Citation5]. Additionally, Doğruel et al compared the use of vecuronium 0.1 mg/kg (with or without a priming dose) versus rocuronium (0.6 or 1.2 mg/kg) in neuroanesthesia. The authors concluded that rocuronium at a dose of 1.2 mg/kg had a significantly shorter onset of action that allows rapid sequence induction compared to vecuronium or smaller doses of rocuronium. Additionally, the use of a larger dose of rocuronium was associated with significant prolongation of the duration of relaxation [Citation26].
6. Limitation of the study
This clinical study was limited by the comparison of only a single dose of either rocuronium or vecuronium. Moreover, the lack of an evaluation of the effect of the priming doses of nondepolarizing muscle relaxants limited the study. Additionally, the lack of a comparison to the use of succinylcholine was a limitation of the study. Furthermore, the muscle relaxation was reversed at the end of the surgery by neostigmine not sugammadex owing to limited resources.
7. Conclusion
It can be concluded that the use of triple the ED95 of rocuronium for the rapid sequence induction of anesthesia in morbidly obese patients allowed rapid and effective tracheal intubation compared to the use of triple the ED95 of vecuronium, with an insignificant difference between the two drugs in the intubation score, the change in the hemodynamic parameters, and the incidence of complications. However, rocuronium use was associated with significant prolongation of the duration of relaxation.
Authors contribution
Mohamed M. Abu Yazed contributed to the formulation of the study design, analysis and interpretation of the data, and final revision and submission.
Sameh Abdelkhalik Ahmed contributed in the study design, collection of the data, drafting, and revising the article. Also, he gave final approval to the final format of the article.
Acknowledgments
We would like to acknowledge all the members of the Department of Anesthesia and intensive care, Faculty of Medicine, Tanta University.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Guirro U, Martins CR, Munechika M. Assessment of anesthesiologists’ rapid sequence induction technique in a university hospital. Rev Bras Anestesiol, 2012;62(3):340–345.
- El-Orbany M, Connolly LA. Rapid sequence induction and intubation: current controversy. Anesth Analg, 2010;110(5):1318–1325.
- Morris J, Cook T. Rapid sequence induction: a national survey of practice. Anaesthesia, 2001;56(11):1090–1115.
- Combs J, Combs G, editors. A literature review of the newest muscle relaxant: ORG 9426. the clinical forum for nurse anesthetists, 1994; 5(3): 104–112.
- Magorian T, Flannery K, Miller RD. Comparison of rocuronium, succinylcholine, and vecuronium for rapid-sequence induction of anesthesia in adult patients. Anesthesiology, 1993;79(5):913–918.
- Sluga M, Ummenhofer W, Studer W, et al. Rocuronium versus succinylcholine for rapid sequence induction of anesthesia and endotracheal intubation: a prospective, randomized trial in emergent cases. Anesth Analg, 2005;101(5):1356–1361.
- Schaller SJ, Fink H. Sugammadex as a reversal agent for neuromuscular block: an evidence-based review. Core Evid, 2013;8:57.
- Abrishami A, Ho J, Wong J, et al. Sugammadex, a selective reversal medication for preventing postoperative residual neuromuscular blockade. Cochrane Database Syst Rev. 2009(4):CD007362.
- da Conceição Duarte NM, Caetano AMM, Neto S, et al. Sugammadex by ideal body weight versus 20% and 40% corrected weight in bariatric surgery–double-blind randomized clinical trial. Braz J Anesthesiol, 2018;68(3):219–224.
- Fuchs-Buder T, Sparr H, Ziegenfuss T. Thiopental or etomidate for rapid sequence induction with rocuronium. Br J Anaesth, 1998;80(4):504–506.
- Heier T, Caldwell JE. Rapid tracheal intubation with large-dose rocuronium: a probability-based approach. Anesth Analg, 2000;90(1):175–179.
- Singh AV, Madan A. A compartive study of intubating conditions after using rocuronium and suxamethonium. Inter J Scient Res, 2018;7(3): 5–7
- Cooper R, Mirakhur R, Clarke R, et al. Comparison of intubating conditions after administration of Org 9426 (rocuronium) and suxamethonium. Br J Anaesth, 1992;69(3):269–273.
- McCourt K, Salmela L, Mirakhur R, et al. Comparison of rocuronium and suxamethonium for use during rapid sequence induction of anaesthesia. Anaesthesia, 1998;53(9):867–871.
- Sørensen M, Bretlau C, Gätke M, et al. Rapid sequence induction and intubation with rocuronium–sugammadex compared with succinylcholine: a randomized trial. Br J Anaesth, 2012;108(4):682–689.
- Mazurek AJ, Rae B, Hann S, et al. Rocuronium versus succinylcholine: are they equally effective during rapid-sequence induction of anesthesia? Anesth Analg, 1998;87(6):1259–1262.
- Sparr H, Luger T, Heidegger T, et al. Comparison of intubating conditions after rocuronium and suxamethonium following “rapid‐sequence induction” with thiopentone in elective cases. Acta Anaesthesiol Scand, 1996;40(4):425–430.
- Williamson R, Mallaiah S, Barclay P. Rocuronium and sugammadex for rapid sequence induction of obstetric general anaesthesia. Acta Anaesthesiol Scand, 2011;55(6):694–699.
- Andrews J, Kumar N, Van Den Brom R, et al. A large simple randomized trial of rocuronium versus succinylcholine in rapid‐sequence induction of anaesthesia along with propofol. Acta Anaesthesiol Scand, 1999;43(1):4–8.
- Tran DT, Newton EK, Mount VA, et al. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev, 2015(10):CD002788.
- Perry JJ, Lee JS, Sillberg VA, et al. Rocuronium versus succinylcholine for rapid sequence induction intubation. Cochrane Database Syst Rev, 2008(2)CD002788.
- Chauvin M, Lebrault C, Duvaldestin P. The neuromuscular blocking effect of vecuronium on the human diaphragm. Anesth Analg, 1987;66(2):117–122.
- Boulanger A, Hardy J-F, Lepage Y. Rapid induction sequence with vecuronium: should we intubate after 60 or 90 seconds? Can J Anaesth, 1990;37(3):296–300.
- Cheng W, Wong Y, Hui Y, et al. Rapid sequence induction and tracheal intubation with vecuronium–with or without a priming dose. Ma zui xue za zhi= Anaesthesiol Sinica, 1993;31(1):15–18.
- Deepika K, Bikhazi GB, Mikati HM, et al. Facilitation of rapid-sequence intuhation with large-dose vecuronium with or without priming. J Clin Anesth, 1992;4(2):106–110.
- Doğruel B, Varnalı G, Selek Ç, et al. Comparison of different induction doses of rocuronium and vecuronium in neuroanaesthesia practice. Turk J Anaesthesiol Reanim, 2014;42(1):6.