ABSTRACT
Background
There are many factors affecting knee osteoarthritis (OA) as genetic and metabolic factors, obesity, mechanical trauma, osteoporosis, inflammatory joint disorders, previous joint infection, and laxity of ligaments.
Objectives
The aim of this study was to detect the influence of intra-articular injection (IAI) of both hyaluronic acid (HA) with platelet-rich plasma (PRP) and radiofrequency (RF) of genicular nerve and to compare their effects in the treatment of knee OA pain.
Subjects and methods
After approval of local research committee of anesthesia, Tanta University (committee protocol code 32049/01/18) and written informed consent, this prospective randomized study was done at Tanta University Hospital on 100 patients complaining of knees OA with mild-to-moderate degrees. IAI was performed in a pain clinic and RF was performed in an operating room during the period from April 2018 to January 2019.
Results
In intra-articular knee injection group, results show decreased visual analog scale (VAS) score from (3–10) at 1-week follow-up session to (0–8) in 6-month follow-up session. It also shows reduction of analgesia requirements (etoricoxib 60 and 90 mg) from (60–270) to (0–180) mg/day. In RF group patients, results show decreased VAS score from (0–9) at 1-week follow-up session to (0–5) in 6-month follow-up session. It also shows reduction of analgesia requirements (etoricoxib 60 and 90 mg) from (0–270) to (0–90) mg/day.
Conclusion
Both IAI of PRP with HA and RF of genicular nerves reduced pain of knee OA and reduced analgesic requirements with rapid onset in RF group.
1. Background
Severe pain, incapacity, loss of function, and impaired life quality are the reasons of chronic arthritis; the most common form is knee osteoarthritis (OA) [Citation1].
There are many factors affecting knee OA as genetic and metabolic factors, obesity, mechanical trauma, osteoporosis, inflammatory joint disorders, previous joint infection; and laxity of ligaments [Citation2].
Analgesics, physiotherapy, and activity adjustment are the main treatment of the early stage of knee OA. Analgesics give a great effect on reduction of inflammation and pain but cannot delay disease progression [Citation3].
Early OA treatment combines nonpharmacological techniques with oral pharmacological therapies. Intra-articular injections (IAI) of hyaluronic acid (HA), corticosteroid with local anesthetic or platelet-rich plasma (PRP) are used in progressive or very symptomatic stage. IAI is considered one of first-line treatments in recent studies as it is effective in decreasing pain and safer than oral pharmacological therapies [Citation4].
HA is a polysaccharide which is found naturally in the synovial fluid, making its elasto viscosity [Citation5].
IAI of HA viscosupplemention in knee OA is demonstrated as an actual treatment in refining pain and function because it is lubricant and shock absorbent with great effect on articular cartilage protection [Citation6].
PRP is a platelet concentrate extracted from patient’s own blood by centrifugation with 2–10 higher concentration [Citation7].
Thermal radiation of genicular nerves is used to increase function and relieve pain by damaging nerves innervating painful tissue or by decreasing the spread of signals of pain. Genicular nerves include obturator, saphenous, femoral, common peroneal, and tibial nerves, which supplies the knee. Thermal radiation of genicular nerve is a dependable technique in the managing of knee OA chronic pain [Citation8].
The aim of this study was to detect the influence of IAI of both HA with PRP and radiofrequency (RF) of genicular nerve and to compare their effects in the treatment of knee OA pain.
2. Subjects and methods
This prospective randomized study was done at Tanta University Hospital on 100 knees with mild-to-moderate degree of OA (IAI was done in pain clinic and RF was done in operating room) from April 2018 to January 2019.
2.1. Inclusion criteria
The inclusion criteria of the study were one hundred knees with mild-to-moderate degree of OA and patients aged 45–75 years old (male and female). Of 100 patients, 75 were female. Body mass index (BMI) was 24–42 kg/m2.
2.2. Exclusion criteria
The exclusion criteria of the study were local or systemic infections, knee effusion, coagulopathy, and previous knee surgery (relative contraindication).
2.3. Sample size calculation
The sample size calculation was performed using G.power 3.1.9.2. The sample size was calculated based on the following considerations: 95% confidence limit and 95% power of the study to demonstrate a decrease 1 in visual analog scale (VAS) (the primary outcome) with RF compared to IAI, VAS at 6 months was 2 ± 1.2 with RF according to a previous study [Citation9] and 11 cases were added to each group to overcome dropout.
2.4. Potential risks
Any risks that were not expected during the whole study was explained to participants and the ethical committee on time.
2.5. Monitoring of data
Data had been recalled in a confidential manner and the privacy of all patients will be maintained
2.5.1. All patients were subjected to the following
1. An informed consent will be obtained from all participants in this research.
2. Personal history: Name, age, occupation, life style and special habits as smoking.
3. Past history:
Medical diseases: if the patient is suffering from autoimmune diseases affecting knee joint as in rheumatoid arthritis.
Drug therapy: if the patient is taking any other medication for another diseases also amount of analgesia taken by the patient to overcome the pain of OA is reported. Knee surgeries or allergy.
4. General and local clinical examination: To evaluate BMI (BMI) and to exclude general diseases, autoimmune diseases, infections or any abnormalities in knee joint.
2.5.2. Preprocedure preparation
For all patients: Full clinical examination, laboratory investigations, and radiological examination (antero–posterior and lateral view plain X-ray for knee joint).
3. Groups and techniques
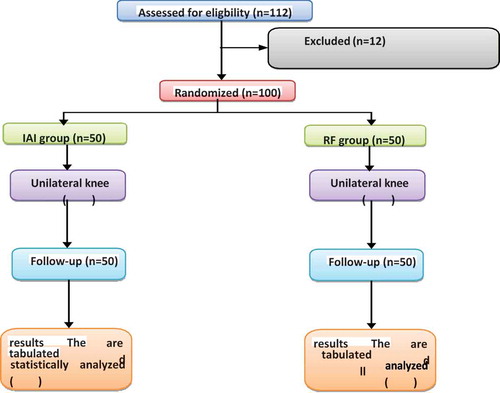
The primary outcome is VAS and pain relief. The secondary outcome is the postprocedure analgesic consumption (after the procedure all analgesics taken by the patient is stopped and only etoricoxib (Arcoxia 60 and 90 mg) “selective COX 2 inhibitor” is given and we changed the dose according to the patient’s need and complain. In this study, 112 patients were considered for eligibility, 8 patients did not meet inclusion criteria (five patients had knee inflammation with effusion and three patients with coagulopathy), and 4 patients rejected to contribute in the study.
All patients were allocated into two groups ().
4. Group A (IAI of HA and PRP) (50 knees)
All patients in group A was given 2 mL of high-molecular-weight HA that content is 22 mg/mL and concentration is 2 million Dalton. Also we arranged PRP by taking 10 mL of blood of the patient, collected in GEL and MACD7 sterile PRP collecting tube, which is a sterile tube containing sodium citrate as an anticoagulant. Then centrifugation of blood was done with 3500 rpm for 5 min by duo-spin technique producing three layers: RBCs, plasma, and buffy coat (platelet). PRP is nearly 3–3.5 mL with mean platelet 1.4–1.6 106/μL. Injection of PRP was for two times with two weeks apart.
5. IAI (patella-femoral joint space) administration
Position of the patients was supine, with flexion of the knee 90º. Also patient could sit with legs hanging over. Skin covering the knee joint was sterilized by alcohol solutions. By a 22-gauge needle, slowly injection of PRP through the anterolateral “soft spot.” followed by HA injection were done. Then knee exercises by passive gentle flexion and extension were done. Patients were supervised for 10 min before discharge. To prevent efficacy reduction of PRP, local ice was applied for 1 week after that. The whole process lasted approximately 20 min ( and ).
6. Group B: Thermal radiation of genicular nerve (50 knees)
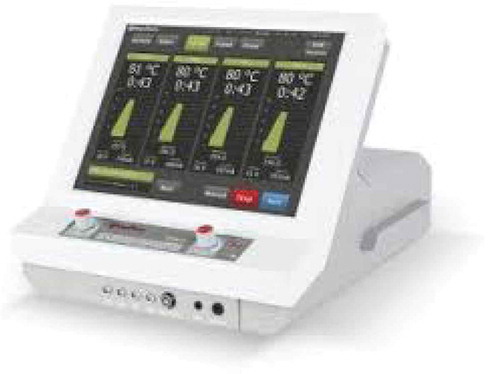
Neurotherm NT 2000 RF was used for thermal radiation by four electrodes pain with independent accurate control for every electrode ().
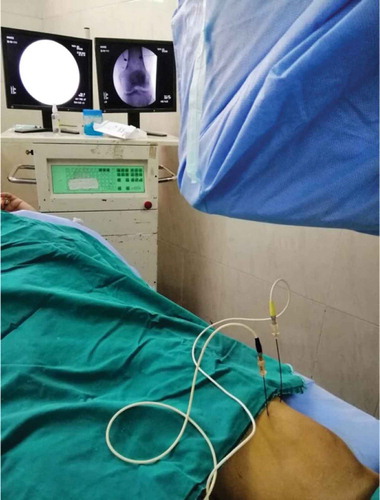
Position of the patients was supine, with support of the knee using a small pillow put under the popliteal fossa. RF cannula (NeuroThermTM) which is 10-cm, 22-gauge with a 10 mm active tip had been placed for each genicular nerve. Position of the RF cannula tip was confirmed by multiple anterior–posterior and lateral fluoroscopic images that were obtained to confirm the place of the needle. After confirming the place of the cannula tip through electrical stimulation, conventional RF thermal lesion had been performed by rising the electrode tip temperature to 80°C for 90 s and the procedure had been repeated for each cannula ().
6.1. Statistical analysis
Statistical presentation and analysis of this study was conducted using the mean, standard deviation, and chi-square test by SPSS V.22.
7. Results
100 knees with OA were divided randomly into two groups, 50 knees in each group.
In demographic data (n) means number of patients which is 50 patients in each group.
In other results (n) means number of knees with OA which is 50 knees in each group.
All patients were included in the follow-up and analysis.
The results were summarized, tabulated, and statistically analyzed in the following tables and figures.
8. Demographic data
The mean age was 60.9 years (45–75); 75 patients (75%) were female. In all of the 100 patients, a mild adverse reaction in the form of a knee swelling was reported 3–5 days after the application. It was not reported as a major complication by any patient. It was observed that 80% of the patients were overweight through BMI in all the groups of treatment. The majority of the population has comorbidities as dyslipidemia (80%) and hypertension (65%). 50% of the patients in all the groups were physically active, practicing walking or aquatic activities, without axial impact.
VAS was measured just before the procedure and after the procedure at 1-week, 1-month, 3-month, and 6-month follow-up session. No statistically significant difference was found between the two groups in baseline VAS. It was verified by VAS that IAI group continued with significant more pain than RF group anterior–posterior and lateral fluoroscopic images had been obtained to confirm the p. This was observed on the follow-up sessions on 1 week with p = 0.005, 1 month with p = 0.001, 3 months with p = 0.001, and 6 months with p = 0.016 ( and ).
Table 1. VAS changes in IAI and RF groups before the procedure.
Table 2. VAS changes in IAI and RF groups throughout the study.
It was found that analgesia requirements were significantly decreased in RF group more than in IAI group in all follow-up sessions in 1 week with p = 0.003, 1 month with p = 0.002, 3 months with p = 0.007, and 6 months with p = 0.041 ().
Table 3. Changes in analgesic requirements (Etoricoxib “Arcoxia” 60 and 90 mg) in IAI and RF groups throughout the study.
In this study, we observed from 1-week follow-up session that in RF group the onset of action was earlier than that in IAI group ()
Table 4. Changes between VAS and analgesic requirements in both groups at 1 week follow-up session.
In 6-month follow-up session, results were nearly the same but RF group still shows better results than IAI group ().
Table 5. Changes between VAS and analgesic in both groups at 6 months follow-up session.
9. Discussion
Patients suffering from knee OA are a huge economic burden on countries as it cost the country rehabilitation, functional medical management, loss of occupation efficiency due to their disability and arthroplasty [Citation10].
In our study, we targeted patients who used to take analgesics for temporary relief of pain and cannot stop them to resume the daily activities. It was expected for this study to have a great enhancement of life quality of and control of pain by usage of HA plus PRP or thermal RF to the genicular nerves [Citation1].
Studies have confirmed the ability of HMW HA to decrease the gene expression of OA related to enzymes and cytokines in fibroblast like synoviocytes (FLS), to control the suppressor T cells for cell proliferation and its anti-inflammatory property. It also confirmed that HMW HA usually stays for a prolonged time than LMW HA in the synovial joint making the benefit of HMW HA higher in stopping release of glycosaminoglycan from the articular cartilage with better outcome for longer periods [Citation11].
So, in our study, we found more significant improvement during 6-month evaluation compared to 1-week, 1-month, and 3-month postinjection evaluation as reflected in VAS score.
In this study, we used a mixture of HA and PRP as different experimental study to stimulate cartilage repair. PRP is a biological treatment; its concentrated platelets make healing and renewal of articular cartilage more rapid. PRP has a huge number of vital growth factors that induce differentiation of mesenchymal stem cells into chondrocytes and thereby increase cell proliferation [Citation12].
Moreover, PRP inhibits inflammatory mediators (e.g., interleukin 1), enhances deposition of the matrix, and makes degeneration slower. Growth factors were found to have the ability to stabilize cartilage homeostasis and help in articular cartilage repair. Allergic reaction and probable transmission of infections are avoided by taking autologous venous blood instead of artificial chemicals [Citation12].
Recent studies have shown that mixing plasma rich in growth factors with HA (+212% in contrast to growth factors alone, and +335% compared with HA alone) amplified the migratory capability of the proliferative cells. Thus, it leads to better regenerating ability and it decelerates the natural progression of the disease. Combination of HA and plasma rich with growth factors also stops the degeneration procedure. This interaction increases the value of this IAI treatment, making it better than analgesics alone which only afford short-term relief and do not treat the pathology [Citation13].
Significant short-term and long-term clinical improvements were observed in the results of patients from both groups. These results indicate that either procedure is a safe and efficient treatment method.
Lana, José FSD assessed the clinical effects of PRP and HA as specific treatments of knee OA and it also inspects the synergistic effects of PRP in mixture with HA. Research continued to examine the therapeutic value of HA and PRP as autologous injectable treatments for knee arthritis. Three IAIs of the knee were received by each patient of their allocated substance; there were 2 week intervals between each injection. Western Ontario, McMaster Universities Arthritis Index (WOMAC) and VAS questionnaire were used to assess clinical results at baseline and after 1, 3, 6, and 12 months. The study revealed that the PRP group has a significant reduction in VAS scores at 1, 3, 6, and 12 months when equated to HA. The PRP group showed better improvement in WOMAC physical activity scale at 12 months when equated to the HA group [Citation14].
Conjoining HA and PRP caused a major decrease in pain and functional limitation when compared to HA alone at 1 year after the treatment and significantly increased physical function at 1 and 3 months when equated to PRP alone [Citation14].
Wong et al. found that old patients with multiple medical comorbidities were afraid of the idea of total knee arthroplasty. Fluoroscopic-guided techniques for RF ablation of the genicular nerves and a cadaveric study recommended that ultrasound-guided genicular nerve blocks can be done precisely [Citation15].
In this study, at 6-month postinjection when IAI of PRP compared to HA, results showed a better outcome in PRP group in pain reduction according to the VAS and numeric rating scale (standardized mean difference −0.92; 95% CI −1.20 to −0.63; p < 0.00001). Nearly all trials discovered a high risk of bias. On the basis of the present evidence, PRP injections decreased pain more efficiently than did placebo injections in OA of the knee (level of evidence: restricted due to a high risk of bias) [Citation16].
This significant consequence on pain was also seen when PRP injections were equated to HA injections (level of evidence: moderate due to a high risk of bias). Moreover, function developed significantly more when PRP injections were equated to controls (limited to moderate evidence). Larger randomized studies of good value and low risk of bias are needed to check whether PRP injections should be a repetitive part of management of patients with OA of the knee [Citation16].
Limitations of the study were as follows: number of knees could be more, but the cost was high and follow-up knee X-rays could be done to follow-up the pathology of knee OA, but the cost was high.
10. Conclusion
Both IAI of PRP with HA and RF of genicular nerve reduced pain of knee OA and reduced analgesia requirements with rapid onset in RF group.
Authors’ contributions
Ahmed Mohammed Saber Hamed, Ahmed Saeed Ahmed Elgebaly, Ahmed Essam Salem, and Hagar Mostafa Elsayed Rady designed the study, analyzed data, and prepared the manuscript. All authors reviewed and approved the final manuscript.
Ethics
This study was approved by the review board of Tanta University (Research Ethics Committee).
Approval Number: 32094/01/18
Board Name: Research Ethics Committee
Board Affiliation: Faculty of Medicine, Tanta University
Phone: +20403332033 Email: [email protected]
Address: Tanta University, faculty of Medicine.
Acknowledgments
The author thanks Prof Ahmed Abdalla Mohamed (MD, assistant of anesthesia, Faculty of Medicine, Cairo University. Address: 139 H, Kafra Gate, Hdyk Al Ahram, Cairo, Egypt. Email: [email protected], Tel: +201272222923) as he helped us in preparing the manuscript.
Disclosure statement
The authors declare that they have no competing interests.
References
- Luyten F, Dell’accio F, De Bari C. Skeletal tissue engineering: opportunities and challenges. Best Pract Res Clin Rheumatol. 2008;15:759–769.
- Perrot S. Osteoarthritis pain. Best Pract Res Clin Rheumatol. 2015;29(1):90–97.
- Nelson FR. A background for the management of osteoarthritic knee pain. Pain Manag. 2014;4(6):427–436.
- Ayhan E, Kesmezacar H, Akgun I. Intraarticular injections (corticosteroid, hyaluronic acid, platelet rich plasma) for the knee osteoarthritis. World J Orthop. 2014;5:351–361.
- Bellamy N, Campbell J, Robinson V, et al. Intraarticular corticosteroid for treatment of osteoarthritis of the knee. Cochrane Database Syst Rev. 2006;2:CD005328.
- Raeissadat SA, Rayegani SM, Hassanabadi H, et al. Knee osteoarthritis injection choices: hyaluronic acid versus platelet rich plasma. Clin Med Insights Arthritis Musculoskelet Disord. 2015;7(8):1–8.
- Mishra AK, Skrepnik NV, Edwards SG, et al. Efficacy of platelet-rich plasma for chronic tennis elbow: a double-blind, prospective, multicenter randomized controlled trial of 230 patients. Am J Sport Med. 2014;42(2):463–471. .
- Choi WJ, Hwang SJ, Song JG, et al. Radiofrequency treatment relieves chronic knee osteoarthritis pain: a double-blind randomized controlled trial. Pain. 2011;152:481–487.
- Konya ZY, Akin Takmaz S, Başar H, et al. Results of genicular nerve ablation by radiofrequency in osteoarthritis-related chronic refractory knee pain. Turk J Med Sci. 2020;50(1):86–95.
- Brown GA. AAOS clinical practice guideline: treatment of osteoarthritis of the knee: evidence-based guideline. JAAOS-Journal of the American Academy of Orthopaedic Surgeons. 2013;21(9):577–579.
- Grace H, Michael L, Timothy M. Intra-articular hyaluronic acid in treatment of knee osteoarthritis: a meta-analysis. JAMA. 2003;290:3115–3121.
- Spakova T, Rosocha J, Lacko M, et al. Treatment of knee joint osteoarthritis with autologous platelet-rich plasma in comparison with hyaluronic acid. Am J Phys Med Rehabil. 2012;91(5):411–417.
- Sánchez M, Anitua E, Delgado D, et al. A new strategy to tackle severe knee osteoarthritis: combination of intra-articular and intraosseous injections of platelet rich plasma. Expert Opin Biol Ther. 2016 Mar 16;16:627–643. .
- Lana JFSD. Randomized controlled trial comparing hyaluronic acid, platelet-rich plasma and the combination of both in the treatment of mild and moderate osteoarthritis of the knee. J Stem Cells Regener Med. 2016;12(2):69.
- Wong J, Bremer N, Weyker PD. Ultrasound-guided genicular nerve thermal radiofrequency ablation for chronic knee pain. Case Rep Anesthesiol. 2016;2016:1–3.
- Laudy ABM, Bakker EWP, Rekers M. Efficacy of platelet-rich plasma injections in osteoarthritis of the knee: a systematic review and meta-analysis. Br J Sports Med. 2015;49(10):657–672.