ABSTRACT
Background: Glenn procedure is a Palliative surgical procedure performed as a step of staged repair for patients with single ventricle such as tricuspid atresia and hypoplastic left heart syndrome. It is usually performed at about three to six months of age, directs systemic venous blood directly from the superior vena cava to the pulmonary circulation. A significant burn injury affects almost all organs. Understanding the complex and pathophysiological responses in the early and late phases of injury is imperative to provide care in the acute and perioperative period. Large airway and lung edema can occur rapidly and unpredictably after burn. Hemodynamics changes in the early phase of severe burn injury are characterized by a reduction in cardiac output and increased systemic and pulmonary vascular resistance.
Case Summary: We report the management of a single ventricle patient with its challenges and unique consideration and major burn with its problems. She underwent serial debridement, extensive skin grafting to all burn areas. The patient had hemoglobin of 8.7 g/dl, she was on dopamine infusion to maintain blood pressure which was difficult to measure by BP cuff, the extremities were not an option to use as monitoring sites. Upon arrival, her oxygen saturation (SpO2) was being monitored with a disposable pulse oximetry sensor through the ear lobule, at times monitoring was disrupted and disappeared. We managed to use an oral airway to measure oxygen saturation through soft palate successfully and after transfusion we could wean off inotropic support.
Conclusion: Patients with Glenn shunt whose acceptable oxygen saturation is 75–80% need hemoglobin level above 13 g/dl. Measurements of capillary density using reflectance oximetry through the soft palate provide very reliable SpO2 measurements.
1. Background
The Glenn procedure is one of the steps of palliative surgeries performed to correct hypoplastic left heart syndrome and other single- ventricle heart defects. It is usually performed about six months after birth. In this operation, the superior vena cava is connected to the right pulmonary artery. Venous return from the head and upper limbs passively flow into the pulmonary artery and proceeds to the lungs to be oxygenated. However, oxygen-poor blood returning to the heart from the lower body through the inferior vena cava will mix with oxygen-rich blood in the left heart and circulate to the body so that the saturation remains in the low 80% range. This operation is preparation for the final step which is the Fontan procedure [Citation1–3].
Major Burns cause massive tissue destruction and result in activation of a cytokine-mediated inflammatory response that leads to dramatic pathophysiologic effects at sites local and distant from the injury [Citation4]. The clinician needs to provide early resuscitation and perioperative care for burn patients to know the pathophysiology of burns, the conflicts, the challenges of the anesthesia during the surgery, and the hemodynamic goals of the single ventricle physiology and keeping proper tissue perfusions.
2. Case summary
We report here the anesthetic management of a single ventricle patient who had major burn. Our patient is 2 and half years old female, weighing 14 kg. She presented with 3rd-degree chemical burn involved 60% of her total body surface area. The patient was transferred to our hospital from outside city. She was intubated and sedated. Her blood pressure was not reliable due to the dressing over the four limbs, her pulse was 160/minute, and oxygen saturation was 65%. The physical examination showed deep burn to the left side of the face, ears, left side of the chest, abdomen, left scapular area, and all the four limbs, including full-thickness circumferential injury with cold soles and palms due to impending compartment syndrome. Bilateral escharotomies were done before arrival. Our patient had tricuspid atresia, pulmonary stenosis, post-Glenn procedure. She was on oral aspirin 50 mg once per day. In PICU she was started on inotropic support of dopamine at a dose of 10 mcg/kg/min to maintain blood pressure. Oxygen saturation was maintained at 76% with FiO2 of 0.6 and above on SIMV mode. She had a triple lumen central line in the left internal jugular vein. Her investigations revealed Hemoglobin of 8.7 g/dl, while platelet count, coagulation profile, renal profile and serum electrolytes were unremarkable. Chest x-ray showed no focal parenchymal lung lesion or consolidation. Echocardiography showed good left ventricle function, patent Glenn anastomosis, patent left pulmonary artery, good atrial communication, unobstructed systemic outflow, and no pericardial effusion. She underwent serial debridement, extensive skin grafting to all burn areas. We transfused packed red blood cells to keep Hemoglobin around 13 g/dl to maintain adequate oxygen delivery, as the oxygen carrying capacity should be optimized by maintaining a hematocrit of 40% to 45% [Citation5]. After blood transfusion, we were able to titrate the dopamine down to off. Beside maintaining hemoglobin, fluid management, infective endocarditis prophylaxis, active warming, monitoring the blood pressure and oxygen saturation were challenging. This procedure was split skin graft of extensive granulating burn site.
We were unable to insert a radial arterial line, but we managed to insert it in the right brachial artery guided by ultrasound without complications.
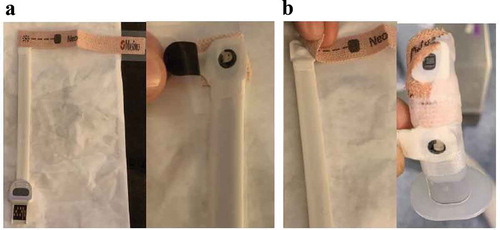
When she arrived to OR, baseline BP was 83/68, Pulse was 136/min, SpO2 was 85%. Fluids and blood were transfused to maintain blood pressure within 20% of the baseline values, and the extremities were not an option to use as monitoring sites, it is important to maintain BP for the perfusion of vital organs and the graft [Citation6]. Oxygen saturation (SpO2) was being monitored with a disposable pulse oximetry sensor through the ear lobule, at times monitoring was disrupted and disappeared. We used our standard disposable pulse oximetry sensor and taped it over an oral airway and then placed in the patient’s mouth in the standard insertion manner for an oral airway (). Once in place, we were able to achieve pulse oximetry readings with an observed consistent waveform We used this monitoring technique for the remainder of the procedure and were able to successfully obtain SpO2 measurements throughout. Oxygen saturation was kept at 75% to 85% during surgery. We removed the brachial arterial line at the end of surgery uneventfully to avoid any postoperative complications. She had serial excisional debridement over 3 months, and they did not insert arterial lines in other procedures and used only non-invasive blood pressure. Oxygen was weaned in stages to room air maintaining the required acceptable oxygen saturation which is 75–85% on room air for Glenn patient. Aspirin was resumed after intermittently being on and off before procedures. Finally, the patient was discharged home on follow up with burn clinic and pediatric cardiology.
3. Discussion
Patients in the post-Glenn stage have half the venous return from superior vena cava passively flowing to the pulmonary circulation; hence, single ventricle is unloaded and less stressed, making this stage the most stable for any non-cardiac surgery. We aim to maintain adequate preload and oxygen delivery keeping Hemoglobin above 13 g/dl, maintaining normal sinus rhythm, adequate ventricular contractility, and attenuating sympathetic response to stress to keep the balance between pulmonary and systemic vascular resistance [Citation7]. The challenge in this case was having a single ventricle patient suffering from a major burn with the potential of hypovolemia, distributive shock, and anemia that need to resuscitate with intravenous fluids, blood, and vasopressors to maintain systemic venous pressure and avoid hypoxemia, hypercarbia, acidosis, stress, and pain. This patient has a baseline oxygen saturation of 75–80%, and needs to maintain and keep oxygen content and delivery through ventilation, transfusion, and maintaining mean arterial blood pressure above 50 mmHg [Citation7–9]. Obtaining vascular access in burn patients is difficult because of the edema, scars, and risk of bloodstream infection. Rapid intravascular volume replenishment is vital. Delayed or inadequate fluid replacement results in hypovolemia, tissue hypoperfusion, shock, and multiple organ failure [Citation10,Citation11]. With extensive debridement and bleeding and when it is difficult to apply BP cuff, an arterial line is required for continuous BP measurement, and sampling. Placement of pulse oximeter is a challenge, if fingers or toes are unavailable, ear, nose, or tongue can be used. Another good option not commonly used is reflectance oximetry through the soft palate. Opioid requirements are increased in burn patients, tolerance makes pain management challenging, Fentanyl infusion at 4 mcg/kg/hour, dexmedetomidine 0.5mcg/kg/hour were needed to control pain in addition to boluses of ketamine 1 mg/kg when needed [Citation4]. For a Glenn shunt, when oxygen saturation is lower than 70%, we lower pulmonary vascular resistance through increasing oxygen concentration, maintaining normocarbia, avoiding increased airway pressure and avoiding atelectasis. Ventilatory strategy includes provision of adequate tidal volume and prolonged expiratory phase with low mean airway pressure simultaneously taking care not to cause hypercarbia. Early institution of spontaneous ventilation improves hemodynamics and also increases Pco2 levels, promoting increase in cerebral blood flow thereby promoting pulmonary blood flow in patients with BDG. Physiological PEEP (3–5 cmH20) is tolerated well without compromising Pulmonary Vascular Resistance (PVR) or cardiac output and helps improve oxygenation and ventilation-perfusion mismatch [Citation7].
4. Conclusion
Measurements of capillary density on the soft palate and tongue have demonstrated the ability to provide very reliable SpO2 measurements. This novel approach to monitoring can be considered and used when the standard, more traditional sights are not an option as in cases of major burns. A patient with a Glenn shunt has oxygen saturation in the range of 75% to 85%; they need to maintain volume, keep maintain a hematocrit of 40% to 45% [Citation5].
Acknowledgments
Thanks to Dr. Mujahed Darwish Pediatric Anesthesia Consultant for his guidance to use reflectance oximetry which is not common to us and was of great value to monitor oxygen saturation reliably when all our traditional sites failed.
Disclosure statement
We have no conflicts of interest to disclose, and no financial disclosures.
References
- Rai V, Gładki M, Dudyńska M. Hypoplastic left heart syndrome [HLHS] treatment options in present era. Indian J Thorac Cardiovasc Surg. 2019;35:196–202.
- Talwar S, Nair VV, Choudhary SK, et al. The Hemi-Fontan operation: a critical overview. Ann Pediatr Cardiol. 2014;7(2):120–125.
- Gobergs R, Salputra E, Lubaua I. Hypoplastic left heart syndrome: a review. Acta Med Litu. 2016;23(2):86–98. PMID: 28356795; PMCID: PMC5088741.
- Bittner EA, Shank E, Woodson L, et al. Acute and perioperative care of the Burn-injured patient. USA: Anesthesiol. 2015;122:448–464.
- Rao PS. Management of congenital heart disease: state of the art-part II-cyanotic heart defects. Children(Basel). 2019 Apr 04;6(4): 54.
- Lingzhong M, Weifeng Y, Tianlong W, et al. Blood pressure targets in perioperative care. Provisional considerations based on a comprehensive literature review. Hypertension. 2018;72:806–817.
- Gupta B, Gupta A, Agarwal M, et al. Shunt Anesthetic concerns for non-cardiac surgery. Northern J ISA. 2017;2:36–42.
- Alatassi A, Mulero SF, Massoud N, et al. A case series of different anesthesia approaches for single ventricular physiology patients in various stages of palliation underwent non-cardiac procedures. Saudi J Anaesth. 2018;12(4):629–633.
- White MC, Peyton JM. Anaesthetic management of children with congenital heart disease for non-cardiac surgery. Cont Educ Anaesth Crit Care Pain. 2012;12:17–22.
- Woodson LC, Sherwood ER, Aarsland A, et al. Anesthesia for burned patients. In: Herndon D, editor. Text book of total burn care. 3rd ed. USA: Elsevier Inc; 2007. p. 196–228.
- Bishop S, Maguire S. Anaesthesia and intensive care for major burns. Cont Educ Anaesth Crit Care Pain. 2012;12:118–122.