ABSTRACT
Background
Spinal anesthesia has been favored by many anesthesiologists due to the simplicity of the technique, the lower incidence of complications like delirium and thromboembolic events. However, severe pain, encountered during positioning for spinal anesthesia, can complicate the technique and worsen the patient experience. Different regional blocks were employed to facilitate patient positioning for spinal anesthesia. Pericapsular nerve group (PENG) block is a recently regional technique based on blocking the articular branches to the hip joint. In our study, the PENG block was used for analgesia during positioning of patient with hip fractures for spinal anesthesia.
Methods
In this study, patients randomly divided into two groups, using closed envelope technique in blocks of 10; Control group (n = 30), and PENG group (n = 30). In the PENG group, the block was performed 30 minutes before spinal anesthesia, with the patient in the supine position using ultrasound guidance. Patient experience during positioning for spinal anesthesia was assessed and compared to the control group.
Results
The PENG block was associated with statistically significant lower pain levels (p 0.00), better patient sitting angle (p 0.00) during positioning for spinal anesthesia compared to the control group.
Conclusion: Preoperative PENG block is an effective option to control positioning related pain during spinal anesthesia, improved patient sitting angle, thus decreased the time required for spinal block and improved the anesthesiologist and patient experience.
1. Introduction
Proximal femur fractures are one of the commonest fractures especially in the elderly population. Early surgical fixation is the best analgesic for associated pain [Citation1]. Spinal anesthesia has been favored by many anesthesiologists due to the simplicity of the technique, the better analgesic profile, and the lower incidence of complications like delirium and thromboembolic events [Citation2–4]. However, severe pain, encountered during positioning for spinal anesthesia, can complicate the technique and worsen the patient experience. Different regional blocks were employed to facilitate patient positioning for spinal anesthesia including femoral nerve block (FNB), fascia iliaca compartment block (FICB), and lateral cutaneous nerve block (LCNB) [Citation5–8].
Pericapsular nerve group (PENG) block is a recently regional technique based on blocking the articular branches to the hip joint with a single injection and is utilized for perioperative analgesia in hip surgery [Citation9]. In our study, the PENG block will be conducted before patient transfer to the operating theater for spinal anesthesia. The primary outcome was the pain profile during positioning for the neuroaxial block. Secondary outcomes included the best angle obtained during patient positioning, time to CSF flow, patient experience (pain during positioning and sitting angle), and perioperative complications including quadratus muscle weakness, nausea, vomiting, shivering, and delirium.
2. Materials and methods
This prospective randomized blinded study was conducted in Mansoura University Hospitals, after approval of the institutional research board (R.20.1.721), and trial registry (PACTR202002906402947). Informed consents were obtained from patients scheduled for hip surgery under spinal anesthesia. Patients with bleeding tendency, local infection at the injection site, and difficulty to express pain scores were excluded from the study. The candidates were randomly divided into two groups, using closed envelope technique in blocks of 10; Control group (n = 30), and PENG group (n = 30) see .
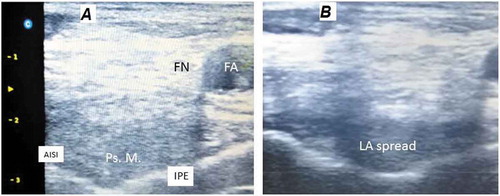
On arrival in the operating theater, automatic noninvasive blood pressure, electrocardiograph, and pulse oximetry were recorded and a wide bore cannula (18 G) was secured. In the PENG group, the block as described by Girón-Arango et al. [Citation10] was performed with the patient in the supine position using ultrasound guidance (high-frequency probe, L7M-A probe7.5 MHz, CHISON, Jiangsu, China). The probe was initially placed in a transverse plane over the anterior inferior iliac spine (AIIS), and then rotated 45 degrees anticlockwise to be roughly aligned with the pubic ramus. As shown in , after keeping the iliopectineal imminence| (IPE), the iliopsoas muscle and tendon, the femoral artery, and pectineus muscle were maintained in the view, a 22-gauge, 80-mm needle was introduced from lateral to medial in an in-plane approach. When the tipoff the needle is visualized in the musculofascial plane between the psoas tendon anteriorly and the pubic ramus posteriorly, 20 ml of local anesthetic (LA) solution (bupivacaine 0.25%) was injected in 5-mL increments while observing for adequate fluid spread. Negative aspiration is performed at the start of the injection and after each 5 mls of the injectate. Patients arterial blood pressure and electrocardiographic tracings, respiratory rate, and pulse oximetry were evaluated noninvasively at 5 min intervals for 30 min after the injection. Also, patients were carefully observed to detect any symptom of LA toxicity of the anesthetic agent.
Figure 2. Ultrasound view showing land marks for the PENG block (A) and local anesthetic spread (B).
The control group was transferred to the O.R. table once the fluid preload was finished, while patients of the PENG group waited for 30 min after the block. Patients were helped to take a proper sitting position for spinal anesthesia. The spinal anesthesia technique was standardized for both groups. The attending anesthetist was blinded for the patient group.
Pain during positioning for spinal anesthesia was assessed and categorized into one of the following grades as modified from previous studies [Citation6,Citation11,Citation12]; grade 1: Sitting without pain and with minimal help, grade 2: patient complains of mild pain detected by grimacing or verbal expression, grade 3: patient expresses severe pain but can tolerate positioning with help, grade 4: patient cannot tolerate positioning and required additional analgesia. Also, the best angle obtained by the patient during spinal anesthesia was classified into the following categories; A: Good flexion (angle more than 90), B: average flexion (angle less than 90) without twisting or using the hands for support, and C: Poor flexion and/or twisting or hand support. A member of the research team surveyed the anesthesiologists performing the block for operator satisfaction after the procedure (Excellent, Good, Average, and Poor). The time required by the anesthesiologist for a successful spinal injection and the number of trials were recorded. VAS will be monitored before and after PENG block and at the time of positioning for spinal anesthesia (i.e., 30 min after PENG block)
2.1. Sample size and study power calculation
G*power software version 3.1.9.4 was employed to compute the required sample size, using the data of a pilot study conducted among 10 patients, where patients given the PENG block had a lower pain score (mean decrease = 1.5) compared to the control group during positioning. A total sample size of 60 patients was sufficient to achieve a target study power of 95% power with an accepted level for alpha error of 0.05.
2.2. Statistical analysis
Perioperative data was tabulated and analyzed using IBM SPSS software version 22. Continuous data were presented as mean±SD or median (IQR) according to the normality of distribution. Nominal and categorical data were presented as numbers and percentages. Independent sample T-test, Mann-Whitney test, chi-square test, or Kruskal–Wallis test were applied to detect statistical differences between the study groups.
3. Results
In this study, 61 patients were assessed for eligibility criteria; one patient was excluded due to the preference of general anesthesia, see . Demographic characteristics, preoperative laboratory data, medical history, and basal pain scores of the included patients are included in .
Table 1. Basal characteristics for the included patients in the two study groups. Data are presented as mean±SD, median (interquartile range).
shows a stacked column comparison between the pain levels during positioning for spinal anesthesia in the two study groups. The PENG block was associated with a statistically significant lower pain levels compared to the control group. Other spinal anesthesia trial outcomes are shown in . The PENG block was associated with a statistically significant better patient sitting angle during positioning for spinal anesthesia. The time required for CSF flow and the number of trials was lower in the PENG group when compared to the control group but did not reach statistical significance. Also, Anesthesiologist satisfaction was significantly higher in PENG group than in the control group.
Table 2. Spinal anesthesia trial outcomes in the two groups. Data are presented as mean±SD or n (%).
Figure 3. Pain profile expressed by the patients during positioning for spinal anesthesia.
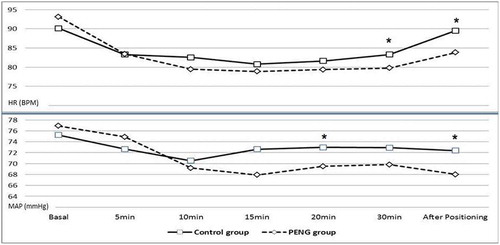
Hemodynamic parameters for the study groups are compared in . A significant decrease in the HR and MAP is noticed, reaching statistical significance at 30 min and after positioning for HR (p 0.03, p 0.02, respectively) and at 15 min after injection and after positioning for MAP (p 0.01, p 0.01, respectively) indicating lower pain scores and reduced stress response.
Figure 4. Hemodynamic parameters (HR, MAP) for the study groups before at admission to OR and at 5, 10, 15, 20, and 30 minutes after the block and immediately after positioning for spinal anesthesia.
No perioperative complications including quadratus muscle weakness, nausea, vomiting, shivering, and delirium were recorded in the study groups.
4. Discussion
In this study, 60 patients scheduled for hip surgery under spinal anesthesia were included. Patient experience during positioning for spinal anesthesia was assessed; PENG block was associated with better patient experience and anesthetist satisfaction. Pain levels were lower in PENG group, which subsequently resulted in a better sitting position for neuroaxial procedure. Furthermore, the number of trials and the time required by the anesthesiologist to give spinal anesthesia were lower in the PENG group.
With proximal femur fractures, passive movement during positioning for spinal anesthesia can cause severe patient pain and discomfort [Citation13]. One-third of the patients with a hip fracture will show signs of severe pain at rest, and the percentage increases to three quarters on movement and friction or overlapping of the fracture ends [Citation14,Citation15], this can negatively affect proper positioning for anesthesia [Citation16,Citation17].
Several strategies have been utilized to alleviate pain during positioning for spinal anesthesia including; NSAIDs, paracetamol, systemic opioids, and regional nerve blocks [Citation18–21]. Since most hip fractures occur in the elderly population, associated comorbidities will complicate pharmacological approaches of pain management [Citation18]. Opioids are associated with confusion, respiratory drive affection, and delayed mobilization. Also, NSAIDs can worsen the renal dysfunction that is reported in nearly 40% of these patients [Citation13,Citation22,Citation23].
To reach an effective regional block, the sensory innervation of the hip joint was extensively studied [Citation24]. The hip joint and the supero-anterior part of its capsule receives sensory innervation via articular branches of the femoral nerve (L2–4) and the obturator nerve (L2–4), while the posteroinferior capsule is innervated through branches of the sciatic nerve (L4–S3). Anesthesia for skin incision (the lateral cutaneous nerve of the thigh (L2, 3), and rarely, the lower thoracic cutaneous nerves) is out the scope of this study [Citation10,Citation24,Citation25].
Increasingly, regional analgesia is encouraged to alleviate pain and decrease opioid requirements in the preoperative period. Also, regional blocks are considered as adjuncts for both general and neuroaxial anesthesia. In the context of positioning pain, regional nerve blocks, either as a single dose or continuously infusion, were administered via a variety of techniques (e.g., femoral nerve block [Citation26,Citation27], 3-in-1block [Citation28,Citation29], fascia iliaca block [Citation30–32], and lumbar plexus block [Citation33]).
However, none of the above-mentioned blocks is assumed to produce a perfect block for the hip joint. LPB is a deep block that is not preferred in patients with bleeding tendency and can be associated with serious complications like hematoma formation and renal trauma [Citation22]. In FICB and 3in1 block, the LA extension is not always consistent, and sometimes the FN and the ON may not be covered. Additionally, in FNB, the articular branches that generate higher at L4 or 5 may not be blocked in the classic approach [Citation17]. Similarly, the AON passes deep and medial to the psoas muscle at the level of L5. Moreover, weakness due to quadriceps femoris (QF) muscle involvement often impedes mobility in the immediate postoperative period and increases the fall risk [Citation21,Citation34,Citation35].
In contrast to the above, PENG block targets the articular branches of FN and AON between the AIIS and IPE, while LA spread, also, to the subpectineal plane is assumed to block the branches of the ON [Citation10]. Thus articular branches to the anterior capsule of the hip joint will be completely blocked using this approach.
In our results, the PENG block succeeds to reduce pain profile during positioning for spinal anesthesia, and this improved patient position. Our results are consistent with the results of previous case series. In the early report of the PENG block, the analgesic effect was superior with a mean reduction of the VAS scale by 7 points on the decimal scale [Citation9]. Furthermore, the analgesic effect of the blocks was moderate with a mean decrease of 3.4 out of 10 in the VAS scale [Citation36]. Also, In a recent report of five cases with the fractured hip joint, the PENG block succeeded to decrease pain levels at rest and during positioning for spinal anesthesia [Citation37].
However, the PENG block will not relieve the pain related to the skin incision and subcutaneous dissection which is covered by the lateral cutaneous nerve. A combination of the LFCN block to PENG block was suggested to give a better form of analgesia than PENG block alone [Citation38,Citation39]. The scope of this study was to evaluate the preoperative analgesic effect of PENG block during positioning for anesthesia before the start of the skin incision. Also, complete anesthesia of the hip joint is assumed to require a sciatic nerve block, however, it is the anterior capsule that receives most of the sensory innervation of the jip joint [Citation5,Citation40].
Our study has some limitations. Catheter techniques and continuous blocks can provide the patient a pain-free whole perioperative journey [Citation41], however, surgical fears of infections could not be alleviated. A future extension of the study protocol using Catheter technique is already planned in our center to assess the effect of continuous PENG block on postoperative analgesia after hip surgeries. Complete anesthesia of the hip joint is assumed to require a sciatic nerve block, however, it is the anterior capsule that receives most of the sensory innervation of the jip joint [Citation5,Citation40]. Time to spinal should have been measured starting from patient positioning on the OR table. The measurement from the start of the trial resulted in the omission of the time spent for positioning that is expected to be shorter in the PENG group due to lower pain levels. Additional time, required to assure full analgesic effect [Citation5], can be compensated by proper coordination and earlier call for the recruited cases.
In conclusion, preoperative PENG block is an effective option to control positioning related pain during spinal anesthesia, improved patient sitting angle, thus decreased the time required for spinal block and improved the anesthesiologist and patient experience.
Disclosure statement
The authors report no conflict of interest.
References
- Griffiths R, Alper J, Beckingsale A, Goldhill D, Heyburn G, Holloway J, et al. Management of proximal femoral fractures 2011. Anaesthesia . 2012 Jan;67(1):85–98. Available from: http://doi.wiley.com/10.1111/j.1365-2044.2011.06957.x
- Van Waesberghe J, Stevanovic A, Rossaint R, et al. General vs. neuraxial anaesthesia in hip fracture patients: a systematic review and meta-analysis. BMC Anesthesiol. 2017;17. DOI:10.1186/s12871-017-0380-9.
- Kowark A, Rossaint R, Coburn M. General versus spinal anesthesia for the elderly hip fractured patient. Curr Opin Anaesthesiol. 2019;32:116–119.
- Atallah M, Abdel Dayem O. Effect of different baricities of intrathecal bupivacaine on the quality of spinal block in elderly patients undergoing transurethral resection of the prostate. Res Opin Anesth Intensive Care. 2015;2:121.
- Iamaroon A, Raksakietisak M, Halilamien P, et al. Femoral nerve block versus fentanyl: analgesia for positioning patients with fractured femur. Local Reg Anesth. 2010;3:21–26.
- Lee KH, Lee SJ, Park JH, et al. Analgesia for spinal anesthesia positioning in elderly patients with proximal femoral fractures: dexmedetomidine-ketamine versus dexmedetomidine-fentanyl. Medicine (Baltimore). 2020;99:e20001.
- Amin NH, West JA, Farmer T, et al. Nerve blocks in the geriatric patient with hip fracture: a review of the current literature and relevant neuroanatomy. Geriatr Orthop Surg Rehabil. 2017;8:268–275.
- Madabushi R, Rajappa GC, Thammanna PP, et al. Fascia iliaca block vs intravenous fentanyl as an analgesic technique before positioning for spinal anesthesia in patients undergoing surgery for femur fractures—a randomized trial. J Clin Anesth. 2016;35:398–403.
- Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:1.
- Girón-Arango L, Peng PWH, Chin KJ, et al. Pericapsular nerve group (PENG) block for hip fracture. Reg Anesth Pain Med. 2018;43:859–863.
- Sia S, Pelusio F, Barbagli R, et al. Analgesia before performing a spinal block in the sitting position in patients with femoral shaft fracture: a comparison between femoral nerve block and intravenous fentanyl. Anesth Analg. 2004;99:1221–1224.
- Kumar A, Sinha C, Kumar A, et al. Positioning of fracture femur patients for spinal anaesthesia: femoral nerve block or intravenous fentanyl? Bali J Anesthesiol. 2018;2:61.
- Scurrah A, Shiner CT, Stevens JA, et al. Regional nerve blockade for early analgesic management of elderly patients with hip fracture – a narrative review. Anaesthesia. 2018;73:769–783.
- Hsu YP, Hsu CW, Chu KCW, et al. Efficacy and safety of femoral nerve block for the positioning of femur fracture patients before a spinal block – A systematic review and meta-analysis. PLoS One. 2019;14:1–20.
- Maxwell L, Frca M, Frca SW, et al. Anaesthetic management of patients with hip fractures: an update. Contin Educ Anaesth Crit Care Pain. 2013;13:179–183.
- Fettes PDW, Jansson J-R, Wildsmith JAW. Failed spinal anaesthesia: mechanisms, management, and prevention. Br J Anaesth. 2009;102:739–748.
- Durrani HD, Butt KJ, Khosa AH, et al. Pain relief during positioning for spinal anesthesia in patients with femoral fracture: a comparison between femoral nerve block and intravenous nalbuphine. Pak J Med Health Sci. 2013;7:928–932.
- Dyer SM, Crotty M, Fairhall N, et al. A critical review of the long-term disability outcomes following hip fracture. BMC Geriatr. 2016;16:158.
- Anaesthetic management of patients with hip fractures: an update. Contin Educ Anaesth Crit Care Pain. 2013;13:179–183.
- Dawe H. Modernising Hip Fracture Anaesthesia. Open Orthop J. 2017;11:1190–1199.
- Guay J, Johnson RL, Kopp S. Nerve blocks or no nerve blocks for pain control after elective hip replacement (arthroplasty) surgery in adults. Cochrane Database Syst Rev. 2017;2017. DOI:.1002/14651858.CD011608.pub2.
- Rk C, Frca G, Checketts MR. Analgesia for primary hip and knee arthroplasty: the role of regional anaesthesia. Contin Educ Anaesth Crit Care Pain. 2008;8:56–61.
- Tyagi A, Salhotra R. Total hip arthroplasty and peripheral nerve blocks: limited but salient role? J Anaesthesiol Clin Pharmacol. 2018;34:379–380.
- Short AJ, Barnett JJG, Gofeld M, et al. Anatomic study of innervation of the anterior hip capsule: implication for image-guided intervention. Reg Anesth Pain Med. 2018;43:186–192.
- Ahamed Z, Sreejit M. Lumbar plexus block as an effective alternative to subarachnoid block for intertrochanteric hip fracture surgeries in the elderly. Anesth Essays Res. 2019;13:264.
- Jadon A, Kedia SK, Dixit S, et al. Comparative evaluation of femoral nerve block and intravenous fentanyl for positioning during spinal anaesthesia in surgery of femur fracture. Indian J Anaesth. 2014;58:705–708.
- Hsu YP, Hsu CW, Chu KCW, et al. Efficacy and safety of femoral nerve block for the positioning of femur fracture patients before a spinal block – a systematic review and meta-analysis. PLoS One. 2019;14:e0216337.
- Christos SC, Chiampas G, Offman R, et al. Ultrasound-guided three-in-one nerve block for femur fractures. West J Emerg Med. 2010;11:310–313.
- Taherzadeh D, Jahanian F, Montazer H, et al. A comparison of ultrasound-guided 3-in-1 femoral nerve block versus parenteral morphinesulfate for pain management in fractured femur in emergency department. J Clin Trials. 2015;5:3.
- Candal-Couto JJ, McVie JL, Haslam N, et al. Pre-operative analgesia for patients with femoral neck fractures using a modified fascia iliaca block technique. Injury. 2005;36:505–510.
- Yun MJ, Kim YH, Han MK, et al. Analgesia before a spinal block for femoral neck fracture: fascia iliaca compartment block. Acta Anaesthesiol Scand. 2009;53:1282–1287.
- Diakomi M, Papaioannou M, Mela A, et al. Preoperative fascia iliaca compartment block for positioning patients with hip fractures for central nervous blockade: a randomized trial. Reg Anesth Pain Med. 2014;39:394–398.
- Wolff AB, Hogan GW, Capon JM, et al. Pre-operative lumbar plexus block provides superior post-operative analgesia when compared with fascia iliaca block or general anesthesia alone in hip arthroscopy. J Hip Preserv Surg. 2016;3:hnw021.
- Aydin ME, Borulu F, Ates I, et al. Indication of pericapsular nerve group (PENG) block: surgical anesthesia for vein ligation and stripping. J Cardiothorac Vasc Anesth. 2019;1–3. DOI:10.1053/j.jvca.2019.08.006
- Sardesai A, Biyani G. Pericapsular nerve group block: innovation or just a fad? Indian Anaesth Forum. 2020;21:1.
- Guay J, Parker MJ, Griffiths R, et al. Peripheral nerve blocks for hip fractures. Cochrane Database Syst Rev. 2017;2017. DOI:10.1002/14651858.CD001159.pub2.
- Acharya U, Lamsal R. Pericapsular nerve group block: an excellent option for analgesia for positional pain in hip fractures. Case Rep Anesthesiol. 2020;2020. DOI:10.1155/2020/1830136.
- Roy R, Agarwal G, Pradhan C, et al. Total postoperative analgesia for hip surgeries, PENG block with LFCN block. Reg Anesth Pain Med. 2019;44:684.
- Girón-Arango L, Tran J, Peng PW. Reply to Aydin et al.: a novel indication of pericapsular nerve group block: surgical anesthesia for vein ligation and stripping. J Cardiothorac Vasc Anesth. 2019;l:1–2.
- Shukla U, Jahan M, Naaz S, et al. USG guided femoral nerve block vs fascia iliaca compartment block as post-operative analgesia in hip fracture patients. Int J Res Med Sci. 2018;6:3057.
- Soares J, Veiga M, Galacho J, et al. ESRA19-0060 Efficacy of continuous pericapsular nerve group (PENG) block for pain relief after hemiarthroplasty of the hip: a case report. Reg Anesth Pain Med. BMJ 2019;44:A210.2-A210. .