ABSTRACT
Background and aim
Using bispectral index (BIS) guided anaesthesia may affect the quality of recovery and consumption of inhalational anaesthetic agents. The target of our study aimed to evaluate the impact of BIS-guided anaesthesia when compared with standard clinical practice to investigate the quality of recovery and sevoflurane concentration.
Patients and method
54 children (aged3-12 years) go through ambulatory surgery that they randomized to receive sevoflurane anaesthesia controlled either merely by clinical parameters (controlled group), BIS-guided group within the BIS range of 40–60 (BIS group). The primary outcome has recorded the recovery time. The secondary outcome recorded the quality of recovery, which was measured by the Pediatric Anesthesia Emergence Delirium score.
Results
There were no statistically significant differences between Group C and Group BIS as regard age, weight, time of surgery, Time of anaesthesia, sex, ASA, type of surgery, mean value of PAED score at 20,25 and 30 min., heart rate and MAP. On the other hand, there were statistically significant differences between Group C and Group BIS as regarding Time for removal of the laryngeal mask, discharge to PACU, PACU time, PAED score at Baseline, 5, 10 and 15 min., and end-tidal sevoflurane concentration.
Conclusion
Sevoflurane anaesthesia guided by BIS results in decreased recovery and decreased sevoflurane concentration without affecting the quality of recovery in children go through ambulatory surgery.
KEYWORDS:
1. Introduction
The bispectral index (BIS) is an electroencephalographic (EEG) parameter measuring the hypnotic component of anaesthesia that guides the administration of volatile anaesthetics. BIS values less than 60 indicate a low likelihood of recall and intraoperative awareness [Citation1]. The BIS uses a combination of EEG sub-parameters of EEGs to demonstrate specific ranges for varying phases of anaesthetic effect. All parameters were combined to form the optimum formation for monitoring of the hypnotic state [Citation2].
The BIS displayed as a range between 0 and 100, with the lower numbers corresponding to deeper levels of hypnosis [Citation3]. The BIS values 100, 80, 60, 40, and 0 represent awake, sedation, general anaesthesia, deep hypnosis, and an isoelectric electroencephalogram, respectively [Citation4].
Sevoflurane is used as an inhalational anaesthetic for pediatric patients. Sevoflurane induction can be achieved quickly and safely by using of the inhalational mask. Sevoflurane does not cause substantial hemodynamic changes and immediately returns to the preoperative level of consciousness [Citation5].
The use of inhalational anaesthetics is associated with frequent emergence delirium in children as crying, confusing, and thrusting movement of the legs. This leads to more duration of hospital stay with medical intervention to avoid the rising incidence of the surgical bleeding from surgical sites, wound pain and unanticipated removal of intravenous lines [Citation6].
The target of our study is to detect the effect of BIS-guided anaesthesia when compared with standard clinical practice to identify the quality of recovery and sevoflurane concentration.
2. Patients and methods
After local ethical committee approval and patients will be evaluated prospectively at Benha university hospital after obtaining consent at the anaesthesia preoperative clinic. The study was conducted from August 2019 to March 2020.
This prospective, controlled, double-blind, randomized clinical trial performed on 54 children aged 3–12 years, scheduled for elective lower abdominal outpatient surgeries. They had no history of premature delivery, communication abnormalities, significant cardiovascular, respiratory nor neurological diseases, and they did not receive any drug affecting CNS.
Patients were allocated randomly by an online randomization program (http: /www.randomizer.org) into two groups: Group C (Control group) and Group BIS in which depth of anaesthesia conducted by BIS. Patient randomization numbers concealed in opaque envelops which opened by the study investigator.
In the operative theatre, routine monitoring, including ECG, NIBP, capnography, and SpO2, was applied to the patient. The BIS (bispectral) electrodes placed on the forehead in group BIS (a three-point BIS electrodes applied to the forehead before induction of anaesthesia, one at the center of the forehead and one at the temple and one between the other two points). The BIS was measured continuously throughout the operation using a BIS monitor (A. 2000 Aspect Medical System). Anaesthesia induced with sevoflurane via facemask: initially 7% fraction inspired in combination with 100% oxygen.
In the control group, the first anesthesiologist was responsible for the administration of sevoflurane and monitoring of the depth of anaesthesia by using standard clinical signs to maintain hemodynamic stability and respiratory pattern while avoiding patient movement. The inspired sevoflurane concentration subsequently titrated by 0.5% increments depending on the patient’s clinical symptoms. In the BIS group, a second anesthesiologist makes sure the proper functioning of the monitors and after that titrated the inspired sevoflurane concentration by 0.5% increments to maintain the BIS value within the range of 40–60. Patients not paralyzed during the whole of our study using the laryngeal mask airway in both groups.
At the end of the surgery, sevoflurane stopped. A third anesthesiologist (the only observer in this study), who was also unaware of the grouping of Assuming adequate spontaneous ventilation and when returned eyelash reflex, the laryngeal mask airway was removed before the patient started to cough or moved their head to decrease the incidence of laryngospasm. On arrival at the post-anaesthesia care unit (PACU), the patient’s behaviour was assessed by using the pediatric anaesthesia emergence delirium (PAED) scores every 5 minutes after awakening for 30 minutes ()[Citation7].
Table 1. Pediatric anesthesia emergence delirium (PAED) scales
The primary outcome has recorded the recovery time. The secondary results were hemodynamic variables (heart rate, mean arterial pressure) every 5 minutes till 30 minutes, anaesthesia time (from induction of anaesthesia till discontinuation of sevoflurane), and surgery time (from incision till the time of final surgical suture), Time to the removal of LMA (from discontinuation of sevoflurane till the elimination of LMA), the time at first movement response after discontinuation of sevoflurane, PAED, end-tidal sevoflurane concentration and hospital stay time.
2.1. Statistical analysis
Analysis of data done by using SPSS version16. Quantitative data were presented as mean ± Standard deviation and analyzed by using the unpaired student t-test. Qualitative data were showed as percentages and numbers and analyzed by using the Chi-square test and Fisher exact test.
Quantitative data of repeated measures in the same group were analyzed by using repeated-measures ANOVA test, and the significant rules detected by post-hoc analysis. P-Value <0.05 was considered statistically significant, and P-Value<0.01 was considered statistically highly significant. The calculated sample size was based on the primary outcome (Recovery time) calculated by using a pilot study of the first seven patients using a power 80% and α error 0.05. The calculated effect size was 0.821, 27 patients were considered in each group.
3. Results
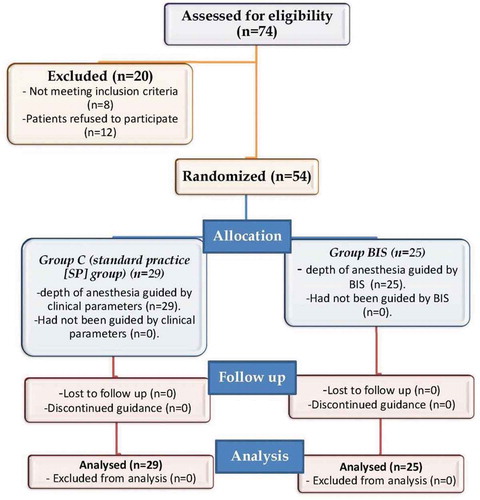
Seventy-four patients were assessed for eligibility, eight patients did not meet the inclusion criteria, and 12 patients did not participate in the study since their parents refused. So, the remaining 54 patients enrolled in the study ().
There was no significant difference between groups regarding Demographic characteristics, time of surgery and time of anaesthesia. ()
Table 2. Demographic characteristics, time of surgery and time of anaesthesia
There was no significant difference between groups regarding the type of surgery. ()
Table 3. Type of surgery
Time to LMA removal and Time to PACU discharge was significantly shorter in group BIS in comparison to group C. End-tidal sevoflurane concentration was reduced considerably in group BIS in contrast to group C. No statistically significant difference between groups regarding hospital stay time. ()
Table 4. Time to LMA removal, time to PACU discharge, hospital stay time and end-tidal sevoflurane concentration
There was a statistically significant difference between groups as regarding PAED at Baseline, 5 min, 10 min and 15 min. (, )
Table 5. PAED score
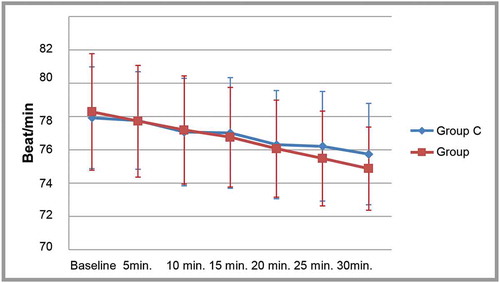
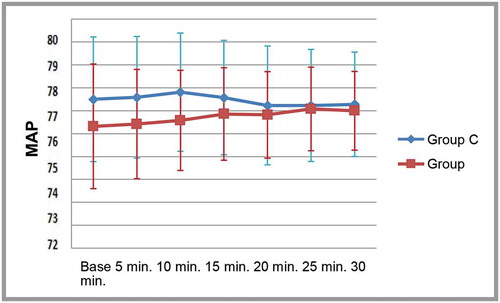
The mean values of MAP and H.R. were statistically non-significant (&).
4. Discussion
The BIS is a numerical value derived from the frequency and amplitude of electroencephalography. It is used to monitor the level of sedation and hypnosis for patients, on a unitless scale from 0 to 100. A BIS value of less than 60 indicates a low probability of recall and intraoperative awareness; therefore, the maintenance of BIS between 40 and 60 is recommended for adequate depth of anaesthesia. A BIS value of between 60 and 70 is associated with light anaesthesia and patients are at higher risk of awareness and postoperative recall [Citation4].
Our study showed that there was no statistically significant differences between Group C and Group BIS as regard age, weight, time of surgery, time of anaesthesia, sex, ASA, type of surgery, mean value of PAED score at20,25and30min., heart rate and MAP. On the other hand, there were statistically significant differences between Group C and Group BIS as regarding Time for removal of the laryngeal mask, discharge to PACU, PAED at Baseline, 5, 10 and 15 min., and end-tidal sevoflurane concentration.
In this study, there were no statistically significant differences between Group C and Group BIS as regarding demographic data, and these were the same results found by Liao et al. [Citation4]. However, studies carried out by Wu et al. [Citation8] comparing the relationship between sevoflurane and BIS in children appeared to be age-dependent.
In the present study, there was no statistically significant difference between Group C and Group BIS as regarding the type of surgery. This agreed with Oliveira et al. [Citation9]who found that the type of operation like herniorrhaphy, circumcision, orchiopexy or varicocele ligation did not differ between Group C and group BIS.
Also, this study has shown that the mean value of time to discharge to PACU was significantly higher among the standard practice group than Group BIS (P < 0.001). As well as, the mean value of PACU time (min.) was also statistically significantly higher among standard practice group than Group BIS (P < 0.001). The results of this study were similar to that of Dowidar et al. [Citation10] who stated that the use of the BIS index, in adult patients undergoing abdominal surgery under general anaesthesia, significantly decreases isoflurane consumption and improves recovery profile.
The present study has shown that there was no statistically significant difference between Group C and Group BIS as regard heart rate and means arterial blood pressure at baseline, 5 min, 10 min, 15 min, 20 min, 25 min, and 30 min. However, Balc et al. [Citation11] found that blood pressure values obtained were very low at equivalent BIS values, and when these blood pressure values were compared with the initial BP values, they were statistically significant (p < 0.05).
This study found that the mean value of End-tidal sevoflurane concentration was statistically significantly higher among Group C than Group BIS (P < 0.001), and this was the same results found by Yılbaş et al. [Citation12] and Fang et al. [Citation13].
The quality indices of recovery in this study were the duration of recovery, emergence delirium. Previous studies have suggested that cerebral monitoring could result in faster emergence and reduction of anaesthetics during general anaesthesia in adults Lio, et al. [Citation4] and children Mc Cann, et al. [Citation14]. Our results were consistent with these findings indicating that both kinds of monitoring could hasten emergence and reduce sevoflurane concentration during the operation.
Gupta et al. found that sevoflurane produces lower BIS, and they concluded that sevoflurane causes a more significant reduction in BIS values when compared to halothane at equal MAC multiples. They showed that the mean BIS value was 54 ± 7 with halothane when compared to 34 ± 6 with sevoflurane at 1 MAC [Citation15].
5. Conclusion
Sevoflurane anaesthesia, guided by BIS, could result in decreased recovery and decreased sevoflurane concentration without affecting the quality of recovery in children go through ambulatory surgery.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Yoo KY, Jeong CW, Kang MW, et al. Bispectral index values during sevoflurane-nitrous oxide general anaesthesia in women undergoing cesarean delivery: a comparison between women with and without prior labour. Anesth Analg. 2008;106(6):1827–1832.
- Avidan MS, Zhang L, Burnside BA, et al. Anaesthesia awareness and the bispectral index. N Engl J Med. 2008;358(11):1097–1108.
- Resow C, Manberg PJ. Bispectral index monitoring. Anesthesiol Clin North Am. 2009;2:89–107.
- Liao W, Wang J, Wugandkuo C. The effect of cerebral monitoring on recovery after sevoflurane anesthesia in ambulatory setting in children: A comparison among bispectral index, A-line autoregressive index, and standard practice. J Chin Med Assoc. 2011;74(1):28–36.
- Somaini M, Shailliog L, Marzorati C, et al. Emergence delirium pain or both. A challenge for clinicians. Pediatr Anesthesia. 2015;25(5):524–529.
- Mason KP. Paediatric emergence delirium: a comprehensive review and interpretation of the literature. Br J Anaesth. 2017;118(3):335–343.
- Somaini M, Engelhardt T, Fumagalli R, et al. Emergence delirium or pain after anaesthesia: how to distinguish between the two in young children: a retrospective analysis of observational studies. Br J Anaesth. 2016;116(3):377.
- Wu ZF, Jian GS, Lee MS, et al. An analysis of anaesthesia-controlled operating room time after propofol-based total intravenous anaesthesia compared with desflurane anaesthesia in ophthalmic surgery: a retrospective study. Anesth Analg. 2014;119:1393–1406.
- Oliveira CR, Bernardo WM, Nunes VM. The benefit of general anaesthesia monitored by bispectral index compared with monitoring guided only by clinical parameters. Systematic review and meta-analysis. Braz J Anesthesiol. 2017;67(1):72–84.
- Dowidar AM, Sadakah NA, Rehab S, et al. The impact of bispectral index on isoflurane consumption and recovery profile in patients undergoing upper abdominal surgery. Med J Cairo Univ. 2018;86(6):1699–1706.
- Balc C, Karabekir H, Sivaci R. Determining entropy values equivalent to the bispectral index values during sevoflurane anaesthesia. Arch Med Sci. 2010;6(3):370–374.
- Yilbas AA, Ayhan B, Akinci SB, et al. The effect of different end-tidal desflurane concentrations on bispectral index values in healthy children and children with cerebral palsy. Turk J Anaesthesiol Reanim. 2013;41(6):200–205.
- Fang W, Jianmin Z, Jie Y, et al. Variation of the bispectral index in children aged 1–12 years under propofol anaesthesia: an observational study. BMC Anesthesiol. 2019;19(1):145.
- McCann ME, de Graaff JC, Absalom AR, et al. Neurodevelopmental outcome at five years of age after general anaesthesia or awake-regional anaesthesia in infancy (GAS): an international, multicentre, randomized, controlled equivalence trial. Lancet. 2019;393(10172):664–677.
- Gupta M, Shri I, Sakia P, et al. Comparison of equi-minimum alveolar concentration of sevoflurane and isoflurane on bispectral index values during both wash in and wash out phases: A prospective randomized study. Indian J Anaesth. 2015;59(2):79–84.