ABSTRACT
Background: Acute kidney injury (AKI) is a common complication associated with cardiac surgery with cardiopulmonary bypass (CPB) with a deleterious effect on morbidity and mortality. The current study aimed to determine the efficacy of preoperative creatine kinase-MB (CK-MB) level for the prediction of occurrence and severity of AKI.
Settings and Design: This study was a prospective cross-sectional observational study.
Methods: The study was carried out on 74 pediatric patients aged less than 18 years scheduled for elective congenital cardiac surgery using CPB. The prevalence of AKI within 72 hours was defined according to the three-stage Acute Kidney Injury Network (AKIN) criteria. Logistic regression analysis was done and adjusted odds ratio (OR) and confidence intervals at 95% (95% CI) were calculated.
Results: AKI had developed in 25 patients (33.78%) by the second postoperative day. Patients who developed AKI had higher mean levels of preoperative CK-MB compared with patients without AKI (P = 0.002). Lower mean age, longer duration of surgery, bypass time, and cross-clamp time were independently associated with AKI (p < 0.015, 0.001, 0.001and 0.001, respectively). Patients who developed AKI had a longer duration of mechanical ventilation (MV) (OR 1.3, 95% CI 1.147–1.691) so; they required longer intensive care unit (ICU) stay.
Conclusion: CK-MB can be a useful biomarker for detecting early AKI after congenital cardiac surgery and predicting adverse clinical outcomes.
1. Introduction
Congenital cardiac disease is one of the most common congenital anomalies and around half of the cases will require surgical repair. The incidence of AKI after pediatric cardiac surgery is between 9.6% and 52% with an associated mortality of 20% to 79% [Citation1]. The pathogenesis of AKI is multifactorial, including exogenous, e.g., nephrotoxic drugs and endogenous toxins, metabolic abnormalities, ischemia and reperfusion injury, neurohormonal activation, inflammation, and oxidative stress [Citation2].
AKI after cardiac surgery is characterized by an abrupt deterioration in kidney function evidenced by a reduction in the glomerular filtration rate (GFR). Importantly, this impairment may not be detected in the first 24–48 hours using conventional monitoring by serum creatinine levels because of the dilutional effects of the CPB pump prime [Citation3]. The advent of novel biomarkers of AKI has opened a new era of early detection and prognosis prediction for cardiac surgery-associated AKI such as; urine and plasma neutrophil gelatinase‑associated lipocalin (NGAL), brain natriuretic peptide (BNP), and IL-18 have been well‑studied and associated with AKI [Citation4].
NGAL is a protein secreted in the urine and produced in renal tubules after ischemic injury. Urinary NGAL in the first 2 postoperative hours could predict patient outcomes, duration of mechanical ventilation, ICU, and hospital stays [Citation5].
Preoperative elevations in cardiac biomarkers may indicate the severity of the underlying cardiac disease, whereas postoperative levels of cardiac biomarkers indicate the complexity of the surgery and the degree of intraoperative cardiac damage, which can increase patients’ risk of postoperative complications, such as AKI [Citation6].
The primary outcome in this study was to examine the efficacy of preoperative CK-MB level for the prediction of occurrence and severity of AKI. While the secondary outcome was to correlate preoperative CK-MB level with the postoperative level of the urine NGAL for prediction of acute kidney injury among pediatric patients undergoing cardiac surgery using CPB and also to assess the relationship between AKI and ICU stay.
2. Patients and methods
After approval of the Local Ethics Committee and with written informed consent from patients’ parents, this study was conducted in Alexandria Main University hospital between February and August 2019 on 74 pediatric patients aged less than 18 years scheduled for elective cardiac surgery using CPB. The spectrum of surgeries included ventricular septal defect closure, atrial septal defect closure, tetralogy of Fallot correction, atrioventricular canal repair, resection of the subaortic membrane, and Glenn shunt.
Exclusion criteria were preexisting chronic renal insufficiency, patients with a history of dialysis requirement, patients aged more than 18 years at the time of surgery, diabetes mellitus, peripheral vascular disease, and use of nephrotoxic agents before or during the study period. The variables studied were sex, age, Risk Adjustment in Congenital Heart Surgery −1 (RACHS-1) [Citation7], NGAL, CK-MB, bypass time, cross-clamp time, vasoactive-inotropic score (VIS) [Citation8], duration of surgery and duration of mechanical ventilation.
Using AKIN criteria [Citation9] (), patients were further assessed every 24 hours for 3 consecutive days and classified into 2 groups: AKI and Non-AKI group
Table 1. Classification of AKI groups according to AKIN criteria
3. Statistical analysis
The sample size was statistically approved by the Community Medicine Department; Faculty of Medicine by using G power 3.1.9.2 program for sample size calculation and according to data obtained from previous studies [Citation5,Citation6]. A sample size of 74 patients was estimated to achieve a 95% power, level of significance of 5%.
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp) Qualitative data were described using number and percent. The Kolmogorov–Smirnov test was used to verify the normality of distribution Quantitative data were described using range (minimum and maximum), mean, standard deviation, median and interquartile range (IQR). The significance of the obtained results was judged at the 5% level.
The used tests were: Chi-square test (for categorical variables, to compare between different groups), Fisher’s Exact or Monte Carlo correction (correction for chi-square when more than 20% of the cells have expected count less than 5), Student t-test (for normally distributed quantitative variables, to compare between two studied groups), and Mann Whitney test (for abnormally distributed quantitative variables, to compare between two studied groups). Univariate logistic regression analysis was undertaken to assess predictors of adverse clinical outcomes.
4. Results
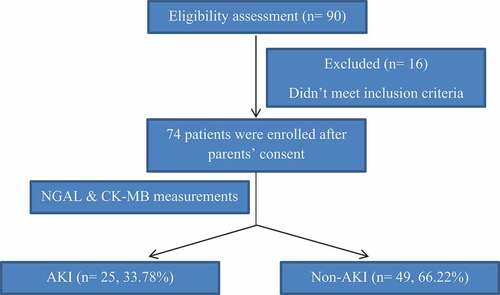
Ninety patients were screened for eligibility to participate in this study and 74 patients subsequently were enrolled in the study, with no patient drop-outs (). Of the 74 patients, 25 (33.78%) developed AKI according to AKIN criteria. Of these 25 patients, 1 (4%) had stage I, 8 (32%) had stage II and 16 (64%) had stage III AKI after 72 hours of ICU admission ().
There was no difference in sex between both groups while the median age was lower in the AKI patients. The median RACHS-1, the mean duration of surgery, bypass time, cross-clamp time, and VIS were higher in the AKI patients ().
Table 2. Demographics and clinical characteristics
The mean serum CK-MB level withdrawn just before the induction of anesthesia was higher in the AKI patients. There was a statistically significant difference between both groups regarding the mean urine NGAL level (). The optimal cutoff value for detecting postoperative AKI was 3 μg/L (sensitivity 80%, specificity 64%) for preoperative CK-MB and 20 ng/mL (sensitivity 96%, specificity 96%) for postoperative NGAL ().
Table 3. Biomarker cutoff values for predicting AKI
4.1. Risk factors associated with AKI
After adjustment of other variables, lower mean age, longer duration of surgery, bypass time, and cross-clamp time were all independently associated with the development of AKI ().
Table 4. Univariate analysis for the parameters affecting AKI (n = 74) and its outcome
4.2. AKI association with outcomes
After adjustment for covariates, patients who developed AKI had greater odds of requiring mechanical ventilation and so, they required longer ICU stay ().
5. Discussion
The findings of this study are similar to the current evidence that AKI after cardiac surgery is common [Citation10], with an incidence of 33.78% in this sample. The present study utilized NGAL as an early sensitive postoperative biomarker collected 2 hours postoperatively for detection of AKI among pediatric patients undergoing cardiac surgery with CPB. It also investigated preoperative CK-MB withdrawn just before induction of anesthesia as a predictor of postoperative AKI. This early prediction may allow AKI prevention by minimizing CPB time, avoiding nephrotoxic medications, and optimizing hemodynamics through fluid management and inotropic support.
Univariate modeling demonstrated that younger age, longer durations of surgery, cardiopulmonary bypass, and cross-clamp time were associated with the development of AKI. Analysis of preoperative risk factors revealed that younger children are at greater risk of AKI. This may be because maximum GFR is not reached until about the age of two years, so children younger than this may be more vulnerable to the ischemic and inflammatory hazards caused by cardiac surgery [Citation11]. This is consistent with studies by Bucholz and colleagues [Citation6] and Aydin and associates [Citation12]. Unlikely, Lee et al. [Citation13] found no significant correlation which may be due to lower body indices and/or to poor general condition.
RACHS-1 category was found to be a risk factor associated with AKI after congenital cardiac surgeries. This is supported by Simon et al. [Citation14], Cardoso et al. [Citation15], and Wakamatsu et al. [Citation16] while, Lee et al. [Citation13] found that RACHS did not influence AKI incidence which may be attributed to their selection of RACHS-1 score ≥3 as a risk factor for AKI while 67 patients in that study had a lower score.
As a predictor of the incidence of AKI, the current study found that CK-MB provides good discrimination of patients who develop AKI which is consistent with a study by Bucholz et al. [Citation6] Also, NGAL was utilized to detect AKI like the results obtained by Yoneyama et al. [Citation17], and Bennett et al. [Citation18].
During the intraoperative period, the present study detected that the duration of surgery, total bypass time, and cross-clamp time are risk factors for AKI that should be taken into consideration. These results are consistent with studies conducted by Amini S et al., Aydin and associates [Citation12], and Simon and colleagues [Citation14]. Unlikely, Lee et al. [Citation13] found no significant correlation between bypass time and cross-clamp time and the incidence of AKI which may be attributed to the shorter median bypass and cross-clamp time in that study (55 min, 23 min for AKI group, respectively) compared to the current study (270 min, 180 min for AKI group, respectively).
Regarding the intraoperative highest VIS, there was a significant difference between the AKI and the non-AKI groups. This is consistent with the results of the study conducted by Sethi et al. [Citation19]. Lee et al. [Citation13] found no significant difference between both groups. This may be due to the lack of postoperative assessment of inotropic agents on AKI incidence in that study.
As a consequence of AKI, MV duration was found to be prolonged among AKI patients leading to prolonged ICU and hospital stay. Similarly, Park et al. [Citation20], and Lee et al. [Citation13] concluded the same result. On the contrary, Kumar et al. [Citation21] found no significant association which may be due to the well-defined perioperative strategy dealing with patients undergoing pediatric cardiac surgery as they said.
6. Conclusion
CK-MB can be a useful biomarker for detecting early AKI after congenital cardiac surgery and predicting adverse clinical outcomes. Lower mean age, longer duration of surgery, bypass time, and cross-clamp time are all independently associated with the development of AKI. Patients who develop AKI after congenital cardiac surgery are at a greater risk of requiring mechanical ventilation and so, they require prolonged ICU stay.
7. Limitations
There were several limitations in the present study, being a small-sized, single-center study. Urine output was not evaluated as a determinant of AKI because 90% of the patients in our unit receive diuretics within 12 hours of ICU admission, which may limit the reliability of urine output to be a direct indicator of innate renal function.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Piggott KD, Soni M, Decampli WM, et al. Acute kidney injury and fluid overload in neonates following surgery for congenital heart disease. World J Paediatr Congenit Heart Surg. 2015;6:401–406.
- Rosner MH, Portilla D, Okusa MD. Analytic reviews: cardiac surgery as a cause of acute kidney injury: pathogenesis and potential therapies. J Intensive Care Med. 2008;23(1):3–18.
- Mao H, Katz N, Ariyanon W, et al. Cardiac surgery-associated acute kidney injury. Cardiorenal Med. 2013;3(3):178–199.
- Koyner JL, Parikh CR. Clinical utility of biomarkers of AKI in cardiac surgery and critical illness. Clin J Am Soc Nephrol. 2013;8:1034–1042.
- Munshi R, Zimmerman JJ. Neutrophil gelatinase‑associated lipocalin can it predict the future? Paediatr Crit Care Med. 2014;15:173–174.
- Bucholz EM, Whitlock RP, Zappitelli M, et al. Cardiac biomarkers and acute kidney injury after cardiac surgery. Pediatrics. 2015 Apr;135(4):945–956.
- Jenkins KJ, Gauvreau K. Center-specific differences in mortality: preliminary analyses using the risk adjustment in congenital heart surgery (RACHS-1) method. J Thorac Cardiovasc Surg. 2002;124(1):97–104.
- Gaies MG, Gurney JG, Yen AH, et al. Vasoactive-inotropic score as a predictor of morbidity and mortality in infants after cardiopulmonary bypass. Pediatr Crit Care Med. 2010;11(2):234–238.
- Sutherland SM, Byrnes JJ, Kothari M, et al. AKI in hospitalized children: comparing the pRIFLE, AKIN, and KDIGO definitions. Clin J Am Soc Nephrol. 2015;10(4):554–561.
- Tóth R, Breuer T, Cserép Z, et al. Acute kidney injury is associated with higher morbidity and resource utilization in pediatric patients undergoing heart surgery. Ann Thorac Surg. 2012;93:19841990.
- Li S, Krawczeski CD, Zappitelli M, et al. Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery: a prospective multicenter study. Crit Care Med. 2011;39:1493–1499.
- Aydin SI, Seiden HS, Blaufox AD, et al. Acute kidney injury after surgery for congenital heart disease. Ann Thorac Surg. 2012;94:1589–1595.
- Lee SH, Kim SJ, Kim HJ, et al. Acute kidney injury following cardiopulmonary bypass in children - risk factors and outcomes. Circ J. 2017;81:1522–1527.
- Simon L, Catherine D, Krawczeski, et al. Incidence, risk factors, and outcomes of acute kidney injury after pediatric cardiac surgery – a prospective multicenter study. Crit Care Med. 2011 June;39(6):1493–1499. .
- Cardoso B, Laranjo S, Gomes I, et al. Acute kidney injury after pediatric cardiac surgery: risk factors and outcomes. Rev Port Cardiol. 2016;35(2):99–104. .
- Wakamatsu Y, Nakanishi K, Matsushita S, et al. Neutrophil gelatinase-associated lipocalin as an early indicator of acute kidney injury following pediatric cardiac surgery. Jpn J Extra-Corporeal Technol. 2020;47(1):8–14.
- Yoneyama F, Okamura T, Takigiku K, et al. Novel urinary biomarkers for acute kidney injury and prediction of clinical outcomes after pediatric cardiac surgery. Pediatr Cardiol. 2020;41:695–702.
- Bennett M, Dent CL, Ma Q, et al. Urine NGAL predicts severity of acute kidney injury after cardiac surgery: a prospective study. Clin J Am Soc Nephrol. 2008;3:665–673.
- Sethi SK, Kumar M, Sharma R, et al. Acute kidney injury in children after cardiopulmonary bypass: risk factors and outcome. Indian Pediatr. 2015;52:223–226.
- Park SK, Hur M, Kim E, et al. Risk factors for acute kidney injury after congenital cardiac surgery in infants and children: a retrospective observational study. PLoS One. 2016;11(11):e0166328.
- Kumar TK, Allen J, Spentzas T, et al. Acute kidney injury following cardiac surgery in neonates and young infants: experience of a single center using novel perioperative strategies. World J Pediatr Congenit Heart Surg. 2016 7;Jul(4):460–466.