ABSTRACT
Background: The COVID-19 outbreak was induced by a novel coronavirus initially discovered in Wuhan, Hubei province of China, in December 2019. The frontline anesthesiologists working in intensive care units at quarantine hospitals are under tremendous pressure and at risk of contracting COVID-19 since the beginning of the quarantine. This overwhelming situation can make them prone to psychological stress and burnout.
Materials and Methods: We did self ‑ administered questionnaire‑based observational cross‑sectional study that sent by e-mail to Egyptian anesthesiologists.
Objectives: The objectives were to measure levels of stress and burnout in frontline anesthesiologists working at ICU of the quarantine hospitals ICU during the current COVID-19 outbreak and to investigate the potential sociodemographic features, job characteristics, and working conditions associated with distress among anesthesiologists.
Results: Of 150 participants, continuous working shift for 2 weeks, young age, and lack of support during work time were significantly associated with higher stress scores with increased values ranged from 2.5 points for lack of support to 3.7 for continuous work shift. As for burnout, continuous working shift for 2 weeks, young age, and having duties all shift time were significantly associated with higher burnout score with increased values ranged from 1.1 for high duties to 3.7 for continuous work shift.
Conclusion: Stress and burnout among anesthesiologists were caused by the continuous work regime, overloaded work, and lack of support. Identifying the triggering factors during this study with targeted interventions and psychosocial support will help to change the environment of the work to minimize the sources of stress.
1. Background
On 31 December 2019, the China office of the World Health Organization (WHO) was notified of the occurrence of cases of pneumonia of unknown cause in Wuhan City of Hubei province. Later, this unknown disease was termed “coronavirus disease 2019” (COVID-19) by the WHO. On 11 March 2020, COVID-19 was announced as a pandemic due to the rapid worldwide spread of the disease [Citation1].
All infectious disease outbreaks are well known to have a psychological impact on both healthcare workers and the general population [Citation2]. Increased risk of to COVID19 exposure with getting the infection and high possibilities of transmitting the infection to their loved ones render that the health‑care professionals are the vulnerable group to psychological stress [Citation3]. From the other side, the load of a rapidly increasing number of patients on limited facilities of health‑care also leads to an increase in duties and working hours, depletion of personal protective equipment (PPE), and separation and isolation from family members. All these factors can contribute to more prone for anxiety and stress. The mental health and decision-making of healthcare workers are seriously affected as results to feelings of anxiety, loneliness, helplessness, and resultant insomnia [Citation4].
A notable example would be the psychological sequelae experienced during the outbreaks of Middle East respiratory syndrome (MERS) and severe acute respiratory syndrome (SARS), where Frontline healthcare worker staff had reported high levels of stress [Citation5]. Anesthesiologists are always at the frontline to deal with emergencies, epidemics, and disasters. As they are good experienced in dealing with emergency airway, resuscitation of patients, and critical care management, the anesthesiologists are playing a major role in the COVID‑19 pandemic. [Citation6] Frontline healthcare anesthesiologists in Egypt have been under tremendous pressure and risk of contracting COVID-19 since the beginning of the quarantine. They used to work in the intensive care units (ICU) to manage COVID-19 critically ill patients.
They are susceptible to contracting the infection due to their involvement in droplets and aerosols generating procedures such as laryngoscopy, tracheal intubation and extubation, and suctioning of oral secretions [Citation7]. As this situation is very stressful due to long working hours, fatigue, challenging interpersonal relations, the need for sustained vigilance, and unpredictability of work, these experiences are consistent with increased psychological symptoms and conditions in anesthesiologists during and after the epidemic [Citation8]. Stress is an emotional, mental, and physical strain or tension which results from an interaction between professional traits and personal traits (perceived stress) [Citation9]. Why some individuals subjected to the same stressors during the same period are more prone to stress than others who depend mainly on the way they perceive stress and their personality traits [Citation10]. Excessive and prolonged stress can lead to the syndrome of burnout [Citation11].
A number of psychological and physical symptoms and signs of burnout may develop, which will significantly affect their overall quality of life. Mental burnout may be displayed with reduced performance, lack of productivity, depersonalization, and absenteeism, while physical symptoms include headache, exhaustion, hypertension, gastrointestinal disorders, and muscle tension. [Citation11,Citation12]
During the pandemic, the negative impact on the environment is the foremost cause of burnout syndrome. Working with this acute illness that pose grave threats to life, this life-threatening dimension requires high professionalism, mental accuracy, and quick reaction constant vigilance to give help the COVID-19 patients. [Citation12] Therefore, anesthesiologists are in a state of high physical and mental load which makes them most vulnerable to stress burnout. [Citation11]
In spite of the increasing importance of this subject, there are yet no studies focusing on stress in frontline Egyptian anesthesiologists during an outbreak.
2. Aim of the work
We proposed to measure levels of stress and burnout in frontline anesthesiologists working at quarantine hospitals ICU using self-reports and questionnaires during the current COVID-19 outbreak. Furthermore, we investigated the potential sociodemographic features, job characteristics, and working conditions associated with distress among anesthesiologists.
3. Patients & methods
This cross-sectional survey study was carried out to examine the psychosocial effect of COVID-19 on frontline anesthesiologists in Egypt; we collected data between April and august 2020 through the electronic mail-based survey. Following the Ethical approval of research ethics committee of the Faculty of Medicine, Alexandria University, and before e-mailing the anesthesiologists, each participant was received a phone call to explain the study and the sorts of the mailed questionnaires and agreements of confidentiality and secrecy.
Data were collected using returned anonymous voluntary self-administered questionnaires that were sent by e-mail to the anesthesiologists from different hospitals across Egypt together with a copy of Ethical approval. This study was conducted as a voluntary survey; each participant anesthesiologist replied to the questions once during the study period after at least 1 month from the beginning of his duty in the quarantine hospital. The anaesthesiologists actively involved in the management of COVID‑19 patients and willing to contribute to the study were only enrolled in this study. The enrolled anesthesiologists were asked to fill out four pages of questionnaires consisting of four parts, aiming to measure the level of stress in anaesthesiologists and to qualify the sources of stress. Self-administered pre-structured questionnaires were used for data collection, in which part 1 included the demographic data (age, sex, marital status, number of offspring, and years in experience).
Part 2 included job characteristics, and working conditions (type of working regime, job demand, and nature of work, job support, and distribution of duties). This questionnaire was adapted from reviewing literatures and work situations at Egyptian hospitals [Citation13].
Part 3 included the Perceived Stress Scale (PSS). PSS is the most commonly used psychological tool for measuring the perception of stress. It is a measure of the degree to which situations in one’s life are appraised as stressful. PSS predicts both objective biological markers of stress and increased risk of diseases among persons with higher perceived stress. PSS is commonly implemented using the 10-item questionnaire to assess the amount of stress in the participants by measuring thoughts and feelings in the previous month [Citation14]. It is entailing of 10 items, each item is responded on a scale from 0 (never) to 4 (very often). Participant scores on the PSS can range from 0 to 40 with higher scores signifying higher recognized stress. Scores ranging from 0 to 13 would be interpreted as low stress. While scores ranging from 14 to 26 and from 27 to 40 would be interpreted as moderate and high perceived stress, respectively.
Part 4 included the subscale of emotional exhaustion, as it sufficiently assesses and validates the burnout. There are three dimensions of burnout: depersonalization, emotional exhaustion, and lack of personal achievement; practically, the subscale of 9-item emotional exhaustion (EE) is used to measure feelings of being emotionally overextended and exhausted by one’s work [Citation15]. The participant was asked to answer each item on a scale from 1 (never) to 7 (every day). The level of burnout (EE score) can vary between 9 and 63, a score of 9 ± 18 signifying a low level, 18 ± 29 a moderate level, and values higher than 29 depicting severe burnout. A pilot study including 15 anaesthesiologists (who were excluded from the main study) was conducted to assess PSS and EE tool reliability. Cronbach’s alpha coefficient of the tools were 0.78 and 0.73, respectively. A panel of three experts reviewed the questionnaire to assess clarity, applicability, and content validity. All suggested modifications after consensus were applied till having the final used questionnaire. The English version of the inventories was used since our participants are Egyptian academic anesthesiologists both educated and working in an English language environment.
4. Data analysis
After data were extracted, it was revised, coded, and fed to statistical software IBM SPSS version 22 (SPSS, Inc. Chicago, IL). All statistical analysis was done using two-tailed tests. P value less than 0.05 was statistically significant. Occupational stress and burnout were assessed by summing up all discrete scores for each scale. Descriptive analysis based on frequency and percent distribution was done for all variables including anaesthesiologist’s demographic data and work-related data.
Overall mean scores plus standard deviation with ranges were calculated for PSS and burnout. Overall man PSS and burnout scores were related to anaesthesiologists' personal and work data testing significance of differences with independent samples t-test (if two categories) and one-way ANOVA (if more than two categories) after confirming the normal distribution for the overall scores using Shapiro test. Correlational analysis was used to assess the relation between anaesthesiologists’ stress level and burnout. Multiple stepwise linear regression model was used to identify the most significant predictors of stress and burnout adjusting for all other factors.
5. Results
The study included 150 anaesthesiologists whose ages ranged from 20 to 55 years old with a mean age of 28.6 ± 10.8 years old. The majority of anaesthesiologists were males (86.7%; 130) and 90 (60%) were not married. Regarding the number of children, 30 (37.5%) had no children and 25 (31.2%) had more than one child. As for experience years, 120 (80%) anaesthesiologists had experience for less than 5 years and 20 (13.3%) had an experience of more than 8 years.
As for anaesthesiologists' work conditions, 75 (50%) had work shift for continuous 2 weeks and 74 (49.3%) reported that their job demands both physical and mental efforts. Job nature was boring as reported by 85 (56.7%) anaesthesiologists, while 69 (46%) reported that they had job support. An exact of 83 (55.3%) anesthesiologists reported that they are on duty all the shift time ().
shows occupational stress and burnout among frontline Egyptian anaesthesiologists during the covid-19 outbreak in Egypt. As for perceived stress, the anaesthesiologists' score ranged from 15 to 24 with a mean score of 20 out of 40 and a score % of 50% (mild stress). As for burnout, anaesthesiologists' score ranged from 15 to 25 with a mean score of 21 out of 63 and a score % of 33.3% (mild burnout).
Table 1. Occupational stress and burnout among frontline Egyptian anaesthesiologists during the covid-19 outbreak in Egypt
illustrates perceived stress level among Egyptian anaesthesiologists during the covid-19 outbreak by their personal and job-related data. PSS score was significantly higher among young, aged physicians (<35 years) than those who aged above 35 years (20.4 vs. 17.4, respectively; P = .001). Also, mean PSS score among females was 21.1 in comparison to 19.8 for male physicians (P = .028). Un-married physicians had significantly higher PSS scores than the married group (20.2 and 19.5, respectively; P = .081). Besides, the mean PSS score among those with experience years less than 5 years was 20.4 compared to 17.5 for those with experience years more than 8 years (P = .001). The mean PSS score among physicians who had work shifts for 2 weeks continuously was 21.9 compared to 18 for those who had interrupted shifts (P = .001). Those who reported boring job nature had significantly higher PSS score than others (20.7 vs. 19; P = .001). Also, PSS was significantly less among those who had job support (18.9 and 20.8, respectively, P = .001). Mean PSS for anesthesiologists who have duties all the shift time was 20.7 in comparison to 19.1 for others who did not (P = .001).
Table 2. Perceived stress level among Egyptian anaesthesiologists during the covid-19 outbreak by their personal and job-related data
demonstrates the emotional Exhaustion level among Egyptian anaesthesiologists during the covid-19 outbreak by their personal and job-related data. EE score was significantly higher among young, aged physicians (<35 years) than those who aged above 35 years (21.1 vs. 17.4, respectively; P = .001). Besides, the mean EE score among females was 22.0 in comparison to 20.3 for male physicians (P = .007). Un-married physicians had significantly higher EE score than the married group (21.2 and 19.6, respectively; P = .007). Also, the mean EE score among those with experience years less than 5 years was 21.1 compared to 17.5 for those with experience years more than 8 years (P = .001). EE score among physicians who had work shifts for 2 weeks continuously was 22.5 in comparison to 18.6 for those who had interrupted shifts (P = .001). Anaesthesiologists who reported boring job nature had significantly higher EE score than others (21.4 vs. 19.4; P = .001). EE was significantly less among those who had job support (19.4 and 21.5, respectively, P = .001). Mean EE for anesthesiologists who have duties all the shift time was 21.4 in comparison to 19.5 for others who did not (P = .001).
Table 3. Emotional exhaustion level among Egyptian anaesthesiologists during the covid-19 outbreak by their personal and job-related data
Considering the most significant predictors for anaesthesiologists perceived stress and burn out (), linear regression model showed that continuous working shift for 2 weeks, young age, and lack of support during work time were significantly associated with higher PSS scores with increased stress score ranged from 2.5 points for lack of support to 3.7 for continuous work shift. As for burnout, continuous working shift for 2 weeks, young age, and having duties all shift time were significantly associated with higher burnout score with an increase in EE score ranged from 1.1 for high duties to 3.7 for continuous work shift.
Table 4. Multiple stepwise linear regression for predictors of anaesthesiologists' perceived stress and burnout
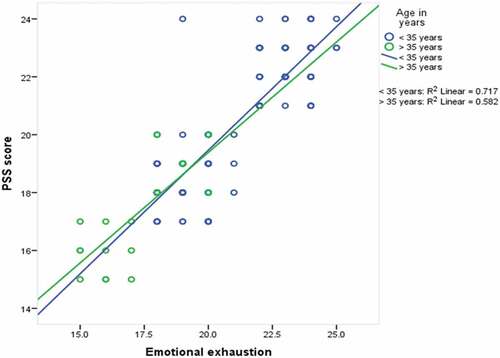
Regarding the correlation between PSS and EE scores among Egyptian anesthesiologists during the covid-19 outbreak, shows that there a significant positive strong correlation (r = .87; P < .001) which was higher among the young aged group (r = .84 vs 76, respectively).
6. Discussion
This study was designed to evaluate the incidence of job stress and burnout among frontline anesthesiologists working in Egyptian quarantine hospitals during COVID-19 epidemics and also to evaluate the influence of work conditions and organizational items on both of them. Many studies during previous outbreaks have revealed that medical personnel are not only suffering from stress and burnout during epidemics, but they may also experience psychological drawback even after the termination of the initial outbreak [Citation16].
This study showed that young, unmarried, less experienced, and female frontline anesthesiologists expressed more job stress and this stress was significantly correlated with increased emotional subscale of burnout rate when compared to older, married, more experienced, and male anesthesiologists. Moreover, this study confirmed the valuable influence of work conditions and organizational items (work regime-job support) over personal factors (except age) on job stress and burnout. These results could be attributed to the fact that perception of work conditions as stressful is mainly related to anesthesiologist’s social, personal, and biological issues beside work status with subsequent direct impact on job strain and burnout [Citation13]. So, it is extremely important to correlate job and social characteristics of anesthesiologists that could be related to job stress and burnout.
Young anesthesiologists are exposed to more heavy work demands, physical and mental efforts, while older and more experienced anesthesiologists found this burden much less stressful and easier to be adapted due to past years of experience and efficacy of managing and coping with stressors [Citation13]. Moreover, when compared to men, female anesthesiologists had higher grades of burnout and stress [Citation17]. This could be related to overcrowded tasks with their contribution to fulfill more than workload (home, family, work) [Citation18].
In the current situation, frontline anesthesiologists were suffered from severe physical and psychological strains. They are daily facing a progressive increase in covid-19 patients together with abnormal medical atmosphere due to restricting obligation of wearing personal protective equipment’s (PPE), working long hours without suitable air-condition, and the settled phobia of getting infection and/or transmitting it to their families [Citation18]. Abut et al. [Citation19] found that young trainees suffered from feeling of inadequacy with personal accomplishment low scores, and this may explain why anesthesia residents suffer from increased perceived stress scale. Calumbi et al. [Citation20] confirmed that female anesthesiologists had a high incidence of stress and burnout when compared to male counterparts.
The present study also revealed the protective role of marriage and bringing children on stress and burn out incidences. These results could be explained as marriage, family duties, and responsibilities could be a part of social support which is reflected on stress perception and suffering from burnout [Citation21]. Abut et al. [Citation19] again reported that married anesthesiologists with more than two children had low emotional exhaustion and stress when compared to others. Castelo-Branco et al. [Citation22] reported that stress and burnout developed as a result of being single. In fact, during infectious outbreaks, being single or married, female or male, having children or not should be rapidly and adequately adapted by health authorities because, during epidemics, the health system is in need for everyone to share whatever is demographic background, and as a consequence, the main objective is to find out the strongest predictor of job stress and burnout. The sudden covid-19 outbreak was accompanied by a huge number of sufferers in need of urgent management, incomplete medical supplies, swinging management procedures, and shortage of medical personnel due to infection and quarantine; all these factors upgraded the work stress [Citation23].
According to linear regression analysis of our data, besides age, the most strong predictors of perceived stress were continuous 2-week work regime and lack of support during work time. Burnout was also dependent on age, continuous 2-week regime, and having duties during all shift time. At the beginning of quarantine hospital work, doctors only attended their work through the continuous 2-week work regime. This system was initially obligatory and followed by the same period of rest at home or hospital isolation before resuming the original job again. Following few months later, this system was replaced to interrupted working shifts in which doctors can come to and go from the hospitals.
According to our results, the continuous regime was accompanied by more stress and burnout among frontline anesthesiologists when compared to the interrupted regime. We also consider that this system was accompanied by lack of support and was affecting the distribution of duties all through the shifts with subsequent more stress and burnout occurrence. We could explain our findings based on previous observations that long working hours with extended duration of isolation and quarantine often result in anxiety, irritability, and stress. High levels of stress to cope with adequate patient care quality with disturbed sleep and life pattern of frontline doctors and separation away from home for long time are leading to anxiety and insomnia, which result in more stress and burnout. Fatigue is also the result of failure to get adequate rest occurred. Fatigue and disturbed sleep patterns may result in disturbed cognition, stress, and burnout [Citation24]. On the other side, some authors reported that support can lessen job stress. Lack of support together with immature ability to deal with stressful situations could lead to emotional exhaustion in young anesthesiologists [Citation25].
Many studies reported that continuous overloaded work results in deterioration of the level of support and supervision from senior medical staff with subsequent elevation of occupational stress among health care workers [Citation26]. Burnout is directly related to stress. Work burnout could be related to unclear job requirements, inadequate time to cope with job responsibilities, non-adequate post-work recovery time, leadership absence, and high unusual job demands [Citation27]. McManus et al. [Citation28] evaluated stress and burnout causal link. They reported that emotional exhaustion with high levels leads to stress and that stress leads to higher levels of emotional exhaustion with the perception of work as boring. During the SARS outbreak in Hong Kong, a frontline health care worker survey revealed that 57% of workers suffered from psychological distress [Citation29]. A higher percentage of Wuhan (China) health care workers expressed psychological abnormalities during the covid-19 epidemic. This could be attributed to accelerated high patient numbers, high mortality, and heavy workload for a prolonged time. It was also notified that frontline workers were more suffering from psychological distress than were other workers because they were in direct communication with covid-19 patients in different situations for long times, so they might be panic about their safety [Citation30].
Our study confirmed the finding of JAIN et al. [Citation18] where they recommended to provide an adequate work environment and regulate working hours with a sufficient period of physical and mental rest for covid-19 frontline health care workers to avoid stress. CAI et al. [Citation31] also enumerate factors that lead to work stress reduction during the covid-19 outbreak. They recommended adequate rest, sleep hygiene, yoga, relaxation, and musical therapy.
This study had some limitations: this study was of short duration conducted between April and August 2020. Data were based on subjective responses using questionnaires and should be in the future studies confirmed with objective measurement of stress. Using a self-reported tool at one point in time was adequate in saving time; however, it was not completely detecting the anesthesiologist’s feelings. We need to increase the number of participants in the forthcoming studies for more clear data. In conclusion, working outside working hours with overloaded work could happen during outbreaks. The authority and hospital administrations should cope and lessen the resultant stress and burnout by facilitating an adequate work environment, providing adequate break during the day for rest, and eating. Insure interrupted shift regime instead of continuous 2-week type, with medical, social, and emotional support. Change the environment of the work to diminish the sources of stresses. Friends and family’s support to anesthesiologists to continue working during the outbreak.
Contribution
Tarek Ismail participated in the study design, conduct of the study, data collection, data analysis, and manuscript preparation.
Rabab Saber participated in the study design, conduct of the study, data collection, data analysis, and manuscript preparation.
Shehata F. Shehata participated in the study design, conduct of the study, data collection, data analysis.
Disclosure statement
No potential conflict of interest was reported by the authors.
Additional information
Funding
References
- Qiu J, Shen B, Zhao M, et al. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: implications and policy recommendations. Gen Psychiatry. 2020;33:e100213.
- McAlonan GM, Lee AM, Cheung V, et al. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can J Psychiat. 2007;52(4):241–247.
- Zhang C, Yang L, Liu S, et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front Psychiatry. 2020;11:306.
- National Health Commission of China. Notice on the issuance of guidelines for emergency psychological crisis intervention in pneumonia for novel coronavirus infections; [ updated 2020 May 25]. Available from: http://www.nhc.gov.cn/xcs/zhengcwj/202001/6adc08b966594253b2b791be5c3b9467.shtml
- Lee SM, Kang WS, Cho A, et al. Psychological impact of the, 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr Psychiatry. 2018;87:123–127.
- Yang M, Dong H, Lu Z. Role of anaesthesiologists during the coronavirus disease 2019 outbreak in China. Br J Anaesth. 2020;124(6):666–69.
- Bajwa SJS, Sarna R, Bawa C, et al. Peri‑operative and critical care concerns in coronavirus pandemic. Indian J Anaesth. 2020;64:267–74.
- Wu P, Fang Y, Guan Z, et al. The psychological impact of the SARS epidemic on hospital employees in China: exposure, risk perception, and altruistic acceptance of risk. Can J Psychiatry. 2009;54:302‑11.
- Weeks AM, Buckland MR, Morgan EB, et al. Chemical dependence in anaesthetic registrars in Australia and New Zealand. Anaesth Intens Care. 1993;21:151±5.
- De Oliveira GS, Ahmed S, Stock MC, et al. High incidence of burnout in academic chairpersons of anesthesiology: should we be taking better care of our leaders? Anesthesiology. 2011;114:181–193.
- Smith M, Segal J, Segal R. Preventing burnout: signs, symptoms, causes and coping strategies; 2012 Jul. Available from: http://www.helpguide.org/mental/burnout_signs_symptoms.htm
- Ozyurt A, Hayran O, Sur H. Predictors of burnout and job satisfaction among Turkish physicians. Q J Med. 2006;99:161–169.
- Shams T, El-Masry R. Job stress and burnout among academic career anaesthesiologists at an Egyptian university hospital. Sultan Qaboos Univ Med J. 2013 May;13(2):287.
- Cohen S. Contrasting the hassle scale and the perceived stress scale. Am Psychol. 1986;41:716–719.
- Maslach C, Jackson SE, Leiter MP. Maslach burnout inventory. 3rd ed. Palo Alto, CA: Consulting Psychologists Press; 1996.
- Gee S, Skovdal M. The role of risk perception in willingness to respond to the, 2014 – 2016 West African Ebola outbreak: a qualitative study of international health care workers. Glob Health Res Policy. 2017;2:21.
- Kluger MT, Townend K, Laidlaw T. Job satisfaction, stress and burnout in Australian specialist anaesthetists. Anaesthesia. 2003;58:339‑45.
- Jain A, Singariya G, Kamal M, et al. COVID-19 pandemic: psychological impact on anaesthesiologists. Indian J Anaesth. 2020 Sep 1;64(9):774.
- Abut YC, Kitapcioglu D, Erkalp K, et al. Job burnout in 159 anesthesiology trainees. Saudi J Anaesth. 2012;6:46–51.
- Calumbi RA, Amorim JA, Maciel CM, et al. Evaluation of the quality of life of anesthesiologists in the city of Recife. Rev Bras Anestesiol. 2010;60:42‑51.
- Kain ZN, Chan KM, Kaz JD, et al. Anesthesiologists and acute perioperative stress: a cohort study. Anesth Analg. 2002;95:17–83.
- Castelo-Branco C, Figueras F, Eixarch E, et al. Symptoms and burnout in obstetric and gynaecology residents. Br J Gynecol. 2007;45:63–84.
- Dai Y, Hu G, Xiong H, et al. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. medRxiv. 2020. Erişim Tarihi. 2020;22. DOI:10.1101/2020.12.10.20247205
- Akerstedt T. Psychosocial stress and impaired sleep. Scand J Work Environ Health. 2006;32:493‑501.
- Cohen S, Wills TA. Stress, social support and the buffering hypothesis. Psychol Bull. 1985;98:310±57.
- Domagala A, Bala MM, Storman D, et al. Factors associated with satisfaction of hospital physicians: a systematic review on European data. Int J Environ Res Public Health. 2018;15(11):2546.
- Scott E. Job burnout: job factors that contribute to employee burnout. What makes some jobs more stressful?; 2010 Feb. Available from: www.stress.about.com
- McManus IC, Winder BC, Gordon D. The causal links between stress and burnout in a longitudinal study of UK doctors. Lancet. 2002;359:2089–2090.
- Tam CW, Pang EP, Lam LC, et al. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: stress and psychological impact among frontline healthcare workers. Psychol Med. 2004;34(7):1197–1204.
- Dai Y, Hu G, Xiong H, et al. Psychological impact of the coronavirus disease 2019 (COVID-19) outbreak on healthcare workers in China. MedRxiv. 2020 Jan 1.
- Cai H, Tu B, Ma J, et al. Psychological impact and coping strategies of frontline medical staff in Hunan between January and march 2020 during the outbreak of coronavirus disease 2019 (COVID‑19) in Hubei, China. Med Sci Monit. 2020;26:e924171.