ABSTRACT
Background: The control of postoperative pain following major lumbar spine surgeries remains a major challenge for anesthesiologists, and many new strategies and methods have been developed for pain control. This study’s main objective was to evaluate the efficacy of the bilateral ultrasound-guided erector spinae plane block (US-ESPB) as a method for perioperative pain management in patients undergoing lumbar spine surgeries.
Methods: This double-blinded prospective randomised controlled study was conducted on 140 patients aged between 18 and 65 years; all were scheduled for elective lumbar spine surgeries. Patients were randomly allocated into one of the two groups: the ESPB group (n = 70) or the control group (n = 70). All patients received bilateral US-ESPB after induction of general anaesthesia, in the ESPB group; 20 mL of levobupivacaine 0.25% were used, while 20 mL normal saline was given to the control group instead. The primary endpoint was the total amount of morphine consumed during the intraoperative and the first 24 postoperative hours. Secondary endpoints included, time to first request of rescue analgesia as well as incidence of adverse effects.
Results: The total amount of morphine consumed during the intraoperative and the first 24 postoperative hours was found to be significantly lower in the ESPB group compared to the control group (P < 0.001). Moreover, the time to first analgesic request was significantly longer in patients receiving ESPB as analgesia (P < 0.001). No statistically significant differences were observed between the two groups regarding complications.
Conclusion: Bilateral US-ESPB is useful intervention for providing adequate pain management in lumbar spine surgeries.
1. Introduction
Lumbar spine surgeries are a widely accepted treatment for patients with pathology in the spine. However, postoperative pain following these surgeries is one of the most common complications. In addition, spinal fusion surgery is one of the most painful surgical procedures, creating a major challenge in pain management [Citation1].
This pain begins with an irritation or inflammatory reaction by surgical trauma of the afferent neuron in different back tissues such as ligaments, nerve root sleeves, intervertebral discs, dura, muscles, facet joint capsules and fascia. This leads to the central and peripheral sensitisation of nociceptive pathways able to induce pain [Citation2,Citation3].
Adequate pain control after spine surgery is an important postoperative care aspect for patients, as it allows for early ambulation, early discharge and improved functional recovery [Citation4]. It also improves patient satisfaction and prevents chronic pain development [Citation5].
Systemic analgesics are used to provide pain control in case of spine surgery procedures, such as opioids, paracetamol and nonsteroidal anti-inflammatory drugs (NSAIDs) . Unfortunately, these agents often cause adverse effects, such as vomiting, nausea, respiratory depression and needing supplemental oxygen when administered in adequate amounts to achieve the desired level of pain relief [Citation4].
Therefore, it is essential to search for other approaches that reduce postoperative opioid needs. Lately, regional analgesia has been a focal point of interest when addressing spine surgery pain management, such as paravertebral blocks, interfacial plane blocks, neuraxial anaesthesia and wound infiltration using local anaesthetic agents [Citation6].
The ultrasound-guided erector spinae plane block (US-ESPB) was proven to be a promising regional analgesic technique when introduced in 2016 in treating thoracic neuropathic pain. It was performed by injecting an agent deep into the erector spinae muscle, affecting both the ventral and dorsal rami of the spinal nerves and the sympathetic nerves on different levels [Citation7].
Many recently published studies have reported the favourable effects of ESPB as postoperative analgesia in different types of surgery, such as breast surgery, abdominal surgery, thoracic surgery and hip reconstructions. However, few of these studies assessed the effect of ESPB as postoperative analgesia in spine surgery, and most of these studies were done on a small number of patients that were not fully blinded to the study [Citation8–11].
This study’s main objective was to evaluate the efficacy of bilateral US-ESPB as a method for perioperative pain management in patients undergoing lumbar spine surgeries. .
2. Materials and methods
This randomised, controlled, double-blinded study was performed at the neurosurgery department in the Cairo University’s teaching hospital from September 2019 to July 2020 after acquiring the Research Ethical Committee of Faculty of Medicine Cairo University (MD-80-2019) approval and clinical trial registration (NCT04110210). The purpose of the study was clarified to all patients in full detail, along with details of the anaesthesia technique to be used by both the surgeon and anaesthetist. Moreover, informed consent was signed by all patients who were scheduled for lumbar spine procedures on any two levels between L1 and L5.
Patients included were between 18 and 65 years of age, with an American Society of Anesthesiologists (ASA) score I–II and no contraindications to regional blocks. Subjects were eliminated from the study if they refused to participate, were unable to evaluate their level of pain, had an allergy to the study drugs, suffered from morbid obesity (body mass index>45), or underwent a procedure on more than two intervertebral spaces.
Three anaesthetists were involved in the research: one responsible for performing the randomisation procedure, one experienced in the block technique for performing said block and one attending anaesthesiologist responsible for recording the intraoperative and postoperative measurements and data collection. All patients, surgeon, Investigators, and research assistants were not aware of patient allocation.
One day prior to operation, patients were assessed by taking a complete comprehensive medical history, physical examination and routine investigations (CBC, PT, PC, INR, ALT, AST, urea and creatinine). Moreover, the numeric visual analogue scale (VAS) pain score was thoroughly explained to all patients (a scale from 0 to 10; 0, no pain; 10, the worst imaginable pain).
Upon verifying a fasting time of 6 h, the patients were taken to the preparation room. Then, a 20-G intravenous cannula was inserted, and intravenous 0.1 mg/kg of metoclopramide, 0.15 mg/kg of ondansetron and 0.01 mg/kg of midazolam were given as premedication. Patients were then moved to the operating theatre where typical monitoring techniques (electrocardiography, pulse oximeter and noninvasive blood pressure) were applied. All patients received standardised general anaesthesia, where an induction was achieved (after preoxygenation with 100% oxygen through a face mask for 3 min) using 1–2 mg/kg of propofol, 0.05 mg/kg of morphine sulfate and 0.15 mg/kg of cisatracurium. Positive pressure ventilation with face mask was then used to deliver 2–3% isoflurane until adequate relaxation was achieved. Intubation was performed with a suitably sized endotracheal tube.
After the endotracheal tube was secured, ESPB group received the block under complete aseptic conditions, with patients in prone position. The subjects were casually allocated into two groups guided by a computerised randomisation table. After induction of anaesthesia, the ESPB group received bilateral ultrasound-guided ESPB with levobupivacaine 0.25% 20 mL, while control group received same block but with 20 ml of normal saline 0.9%.
2.1. ESPB
A low-frequency curved array ultrasound probe (Siemens ACUSON X300 Ultrasound System with curved probe) was placed in a transverse location at the operating level to visualise the tip of the transverse process, which was then centred on the ultrasonography device screen. The probe was then turned longitudinally 2–3 cm lateral to vertebral column, where the skin, subcutaneous tissue and erector spinae muscle could be seen over the acoustic shadows of the transverse processes. After proper sterilisation of the skin, an 18-G Tuohy needle was inserted parallel to the ultrasound beam in a cranial-to-caudal direction until it reached the transverse process. Confirmation of the proper location for the needle tip was achieved by injecting 0.5–1-mL saline, followed by lifting the erector spinae muscle off the transverse process without muscle distension. Afterward, either 20 mL of 0.25% levobupivacaine was injected for each of the patients in the ESPB group or 20 mL normal saline was used for each of the patients in the control group. All previous steps were then repeated on the contralateral side.
At the end of block, the average duration to induce block was calculated from the time taken from the point of visualising and identifying rhomboid major, trapezius and erector spinae muscle at spinous process to the point of visualising the spread of local anaesthetic agent ultrasonographically into the fascial plane between the transverse process and erector spinae muscle. If there was an increase in heart rate (HR) and mean arterial blood pressure (MAP) more than 20% of pre-block baseline values after skin incision, the block was considered a failure. In case of block failure, the patient was excluded from the study and anaesthesia was conducted according to the protocol of Kasr Alainy hospitals for spine surgery anaesthesia.
Anaesthesia was maintained by an air/oxygen mixture and isoflurane with cisatracurium as a continuous infusion (1–2 mcg/kg/min), and bolus doses of morphine sulfate (0.02 mg/kg) were regulated to keep the HR and MAP within 20% of the preinduction readings. HR and MAP were recorded every 15 min throughout surgery.
At the end of the procedure, isoflurane was stopped, and neuromuscular blockade was reversed using 0.04 mg/kg of intravenous neostigmine and 0.01 mg/kg of atropine, followed by endotracheal tube removal. After surgery, the patients were taken to the postanaesthesia care unit for a full recovery. During this time, HR and MAP were recorded; after transferring patients to the ward zone, HR and MAP were recorded every 4 h for 24 h.
In both groups, the same postoperative analgesic protocol was prescribed: 30 min prior to the end of the procedure, 30 mg of IV ketorolac was administered and repeated every 8 h postoperatively. IV morphine was given when subjects requested a postoperative pain control agent in a loading dose of 0.05 mg/kg. Afterward, the patients were connected to a disposable silicon PCA infusion device (M5015L Accufuser 300 mL) containing 30 mg of morphine. The PCA was programmed to provide 5 mL/h (0.5 mg morphine per hour) by continuous infusion and 1 mL bolus dose (0.1 mg morphine per dose) whenever needed, with a lockout interval of 15 min. Additional IV bolus doses of morphine were given as a rescue analgesic dose for patients who had a VAS score≥4 or when experiencing pain between the assessment intervals. A dose of 0.15 mg/kg of IV metoclopramide was designated to patients suffering from nausea or vomiting.
The primary outcome was defined by the cumulative morphine required during the intraoperative and the first 24 postoperative hours (in mg). The secondary outcomes included the time between the end of the procedure and the first analgesic dose needed (min). Moreover, the subjects’ demographic data (age, gender, BMI, ASA, comorbidities and history of analgesic drug that already taken and basic VAS) as well as operative data [type of surgery and level of surgery] were recorded. The duration of surgery (min) and duration of anaesthesia (min) were subsequently recorded. All mentioned factors were compared in both groups. Postoperative pain assessment using VAS score was conducted preoperatively, after complete recovery and every 4 h for a further 24 h. The duration of hospital stay and the occurrence of complications, either in the form of opioid-related side effects (nausea/vomiting) or toxicity from the local agent levobupivacaine in the form of cardiovascular collapse (bradycardia or hypotension) were recorded. Moreover, the surgeon’s and patients’ satisfaction with this technique were rated using 1–4 scales (1, bad; 2, moderate; 3, good; 4, excellent; and 1, poor; 2, fair; 3, good; 4, excellent, respectively).
2.2. Statistical analysis
Power analysis was done using G power program for morphine consumption independent sample student T-test because it was the primary outcome in this study. A preceding study observed that morphine consumption in the first 24 h following extubation was 23.8 ± 10.9 mg [Citation12]. On the basis of the assumption that erector spinae block will decrease 24-h morphine consumption by 30%, the sample size was calculated to be 70 patients in each group (total 140) to identify a noticeable difference of 30% or more in morphine requirement, with a power of 95% and a significance level of 5%. The assessment of categorical variables was done using the chi-squared or Fischer’s exact test. The mean±SD represented data that was normally distributed. Morphine consumption, fentanyl consumption and time to first analgesic need were analysed using an independent T-test, as appropriate. The median (range) represented the data that were not normally distributed (by the Kolmogorov–Smirnov test) and was analysed with the Kruskal–Wallis test, as appropriate. The software SPSS v25.0 for Windows (SPSS, Inc., Chicago, IL, United States) was used for statistical analysis. P < 0.05 was considered statistically significant.
3. Results
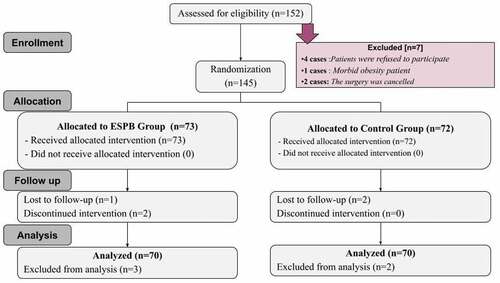
We recruited 152 patients and tested them for eligibility. We excluded 12 patients due to incomplete data collection records, block failure, surgery cancellation, or falling within exclusion criteria. All 140 patients (70 patients in each of the two groups) completed the study and were analysed ().
There were no statistically noticeable differences in both groups concerning demographic (age, gender, BMI, ASA and comorbidity) or operative data [type of surgery, level of surgery, length of the procedure (min) and extent of anaesthesia (min)] or the average time to perform block ().
Table 1. Demographic and clinical characteristics of the two studied groups. [Data are presented as mean ± SD, n (%) and median (IQR)]
However, a statistically significant difference was found in the total amount of morphine consumed both intraoperatively and postoperatively (mg) between the ESPB and the control groups, with values of 14.02 ± 1.7 mg and 30.83 ± 2 mg, respectively (p < 0.001). Furthermore, the ESPB group was found to consume less morphine intra-operatively when compared to the control group with values of 4.83 ± 0.8 mg and 9.41 ± 1.7 mg, respectively, as well as less postoperative morphine consumption with values of 8.9 ± 1.2 mg and 21.3 ± 0.9 mg, respectively (P < 0.001).
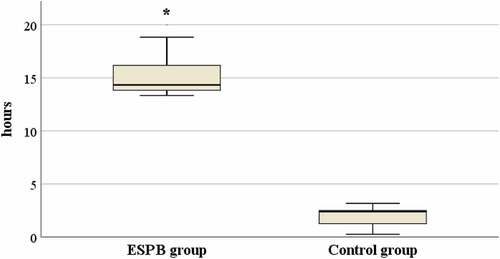
Moreover, the mean duration of the first analgesic requirement was significantly higher in the ESPB group (15.03 ± 1.6 hours versus 1.97 ± 0.8 hours in the control group) (P < 0.001) ().
Figure 2. The total amount of morphine consumed (intraoperative and postoperatively) (mg) in both groups
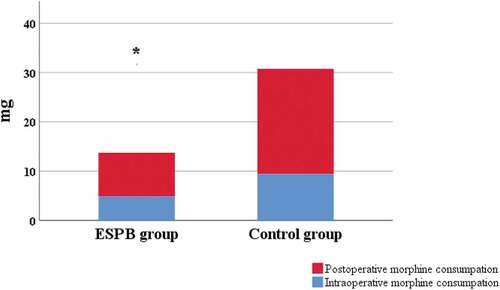
Figure 3. The mean duration of the first analgesic requirement in both groups
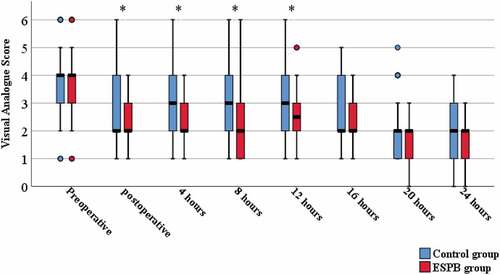
The VAS score was significantly lower in the ESPB group when compared to the control group in the first 12 h after the operation with P < 0.001. However, after 12 h post-surgery, no differences were observed between the two groups ().
Figure 4. Postoperative visual analogue score over time in both groups
Complications in the form of nausea were recorded in four cases (5.7%) in the ESPB group and eight cases (11.4%) in the control group, while vomiting was recorded in two cases (2.9%) in the ESPB group and four cases (5.7%) in the control group. Moreover, patients suffering from both, nausea and vomiting, were recorded in two cases (2.9%) and six cases (8.6%) in the ESPB and control groups, respectively. However, the frequency of complications was not significantly different (P = 0.181). No another complication was detected in the form of respiratory depression or needing supplemental oxygen. At the end of surgery, we asked the surgeons about their satisfaction with the US-ESPB technique and found that they were highly satisfied by the outcome in the ESPB group patients (P = 0.004). Furthermore, the day after surgery, all patients were asked about the level of pain relief experienced under this technique. Most reported being satisfied with the block with (P < 0.001), but there was no statistically significant difference between both study groups concerning length of hospital stay (P = 0.126) ().
Table 2. Comparison of the postoperative complication and Scoring of postoperative surgeon satisfaction and patient satisfaction in both groups. [Data are represented as No. (%) and mean ± SD]
4. Discussion
This study showed a clear reduction in intraoperative and postoperative opioid consumption following the application of bilateral ultrasound-guided ESPB as a preemptive analgesic technique in patients undergoing lumbar spine surgeries. Moreover, US-ESPB also significantly prolonged the time to first analgesic use and improved both surgeon and patient satisfaction, as well as significantly reduced postoperative VAS scores in the first 12 h after surgery, without a significant difference in intraoperative or postoperative complications.
Lumbar spine surgeries have been rated as one of the top six surgeries that result in the highest level of postoperative pain [Citation1]. Pain results from the activation of several processes that include nociceptive, neuropathic and inflammatory mechanisms [Citation1,Citation13]. Thus, postoperative pain management is considered essential for these patients due to its strong influence on a better surgical outcome, as it allows early mobilisation and hospital discharge, which in turn decreases the development of thromboembolic and pulmonary complications, as well as reduces postoperative mortality and morbidity. However, patients may suffer from altered pain perception as a result of chronic pain treatment prior to the operation, including long-term analgesic consumption, making postoperative pain control a very challenging task [Citation14]. Therefore, these patients need a multimodal analgesic regimen aimed at providing effective, safe and high-quality analgesia to reduce side effects, such as vomiting , nausea and respiratory depression resulting from the administration of high doses of opioids. The multimodal analgesic regimen, which is a goal of the enhanced recovery programme, was established with the application of a preemptive regional anaesthetic, together with postoperative non-opioid agents and opioids [Citation15].
One of the novel ultrasound-guided paraspinal plane blocks is the ESPB, where a local agent is injected below the erector spinae muscle. It can be performed simply, quickly and safely with fewer hazards when compared with the other regional block procedures [Citation16]. Since 2016, many studies that discussed the ESPB as case reports or clinical studies showed that the US-ESPB is effective in controlling pain postoperatively after different abdominal [Citation9,Citation17], thoracic [Citation18,Citation19] and breast surgeries [Citation20,Citation21]. There were few randomised controlled studies and case reports about its use as an element of multimodal analgesia in lumbar spinal surgeries [Citation16,Citation22–26].
The observations in this study agree with previous works. Singh and others [Citation16] performed preoperative bilateral US-ESPB and found improved effects on postoperative pain control than conventional postoperative analgesia after lumbar spine procedures. However, the study was conducted on a small number of patients compared to our study, and ESPB was done at the level of T10 regardless of the level of surgery. In our study, the injection was done at the level of surgery in the lumbar region. According to a retrospective study done by Hironobu Ueshima and others [Citation26], where the data were collected from 41 patients in 2017 and analysed retrospectively, ESPB achieved an effective degree of postoperative analgesia for 24 h, with a significant decrease in the fentanyl requirement in subjects having lumbar spine procedures. These results are compatible with our study, in spite of its retrospective nature and small number of patients analysed. Our results are also similar to a study conducted by Ahmet Murat Yayik and others [Citation22], where ESPB was used on 60 patients as part of a multimodal analgesic technique to decrease opioid burden and control acute postoperative pain in subjects having open lumbar decompression procedure. However, the block was performed at the L3 level only. The results showed a favourable response to ESPB regarding its effect on postoperative analgesia and duration. In light of all this previous work, the current study may be considered the biggest double-blinded, prospective, randomised control study done to assess the efficacy of bilateral US-ESPB for intraoperative and postoperative pain control.
Although our research achieved its aims, there were limitations of this study. First, as general anaesthesia was used, the sensory perception of patients could not be assessed after block administration. Second, no information concerning the patients’ preoperative pain ratings was available, which could affect postoperative analgesic consumption. Third, this research focused primarily on the first 24 h following the surgical procedure. However, no data were collected on the ESP block’s effectiveness in reducing chronic pain. Finally, this block needs to be compared with another type of block in this type of surgery. We believe all these limitations must be considered thoroughly in future studies.
5. Conclusions
Bilateral US-ESPB seems to be a useful intervention for providing adequate pain management during both intraoperative and postoperative periods for patients undergoing lumbar spine surgery, as it decreases the opioid requirement. It is simple and safe, which makes it unique when compared with other blocks.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Gerbershagen HJ, Aduckathil S, Van Wijck AJM, et al. Pain intensity on the first day after surgery. Anesthesiology. 2013;118:934–944.
- Prabhakar H. Textbook of neuroanesthesia and neurocritical care. In: Prabhakar H, Ali Z, editors. Textbook of neuroanesthesia and neurocritical care. Vol. I. Singapore: Springer Singapore; 2019. p. 447–455.
- Bernard JM, Surbled M, Lagarde D, et al. Analgesia after surgery of the spine in adults and adolescents. Cah Anesthesiol. 1995;43:557–564.
- Bajwa SJS, Haldar R. Pain management following spinal surgeries: an appraisal of the available options. J Craniovertebr Junction Spine. 2015;6:105–110.
- Kehlet H. Postoperative pain relief—what is the issue? Br J Anaesth. 1994;72:375–378.
- Zorrilla-Vaca A, Healy RJ, Mirski MA. A Comparison of regional versus general anesthesia for lumbar spine surgery. J Neurosurg Anesthesiol. 2017;29:415–425.
- Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block. Reg Anesth Pain Med. 2016;41:621–627.
- Ayub A, Talawar P, Kumar R, et al. Erector spinae block a safe, simple and effective analgesic technique for major hepatobiliary surgery with thrombocytopenia. Egypt J Anaesth. 2018;34(4):169–172.
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery. Reg Anesth Pain Med. 2017;42:372–376.
- Chin KJ, Adhikary S, Sarwani N, et al. The analgesic efficacy of pre-operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72:452–460.
- Kline J, Chin KJ. Modified dual-injection lumbar erector spine plane (ESP) block for opioid-free anesthesia in multi-level lumbar laminectomy. Korean J Anesthesiol. 2019;72(2):188–190.
- Bellissant E, Estebe J-P, Sebille V, et al. Effect of preoperative oral sustained-release morphine sulfate on postoperative morphine requirements in elective spine surgery. Fundam Clin Pharmacol. 2004;18:709–714.
- Bianconi M, Ferraro L, Ricci R, et al. The pharmacokinetics and efficacy of ropivacaine continuous wound installation after spine fusion surgery. Anesth Analg. 2004;98:166–172.
- Loftus RW, Yeager MP, Clark JA, et al. Intraoperative ketamine reduces perioperative opiate consumption in opiate-dependent patients with chronic back pain undergoing back surgery. Anesthesiology. 2010;113:639–646.
- Dunn LK, Durieux ME, Nemergut EC. Non-opioid analgesics: novel approaches to perioperative analgesia for major spine surgery. Best Pract Res Clin Anaesthesiol. 2016;30:79–89.
- Singh S, Chaudhary NK. Bilateral ultrasound guided erector spinae plane block for postoperative pain management in lumbar spine surgery: a case series. J Neurosurg Anesthesiol. 2019;31:354.
- Tulgar S, Kapakli MS, Senturk O, et al. Evaluation of ultrasound guided erector spinae plane block for postoperative analgesia in laparoscopic cholecystectomy: a prospective, randomized, controlled clinical trial. J Clin Anesth. 2018;49:101–106.
- Cesur S, Ay AN, Yayik AM, et al. Ultrasound-guided erector spinae plane block provides effective perioperative analgesia and anaesthesia for thoracic mass excision: a report of two cases. Anaesth Crit Care Pain Med. 2019;38:189–190.
- Forero M, Rajarathinam M, Adhikary S, et al. Continuous erector spinae plane block for rescue analgesia in thoracotomy after epidural failure: a case report. A A Case Rep. 2017;8:254–256.
- Gurkan Y, Aksu C, Kus A, et al. Ultrasound guided erector spinae plane block reduces postoperative opioid consumption following breast surgery: a randomized controlled study. J Clin Anesth. 2018;50:65–68.
- Kumar A, Hulsey A, Martinez-Wilson H, et al. The use of liposomal bupivacaine in erector spinae plane block to minimize opioid consumption for breast surgery: a case report. A A Pract. 2018;10:239–241.
- Yayik AM, Cesur S, Ozturk F, et al. Postoperative analgesic efficacy of the ultrasound-guided erector spinae plane block in patients undergoing lumbar spinal decompression surgery: a randomized controlled study. World Neurosurg. 2019;126:e779–85.
- Chin KJ, Lewis S. Opioid-free analgesia for posterior spinal fusion surgery using erector spinae plane (ESP) blocks in a multimodal anesthetic regimen. Spine (Phila Pa 1976). 2019;44:E379–83.
- Melvin JP, Schrot RJ, Chu GM, et al. Low thoracic erector spinae plane block for perioperative analgesia in lumbosacral spine surgery: a case series. Can J Anaesth. 2018;65:1057–1065.
- Cesur S, Yayik AM, Ozturk F, et al. Ultrasound-guided low thoracic erector spinae plane block for effective postoperative analgesia after lumbar surgery: report of five cases. Cureus. 2018;10:e3603.
- Ueshima H, Inagaki M, Toyone T, et al. Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective study. Asian Spine J. 2019;13(2):254–257.