ABSTRACT
Background and Objective:
Erector spinae plane block (ESPB) has been reported to provide analgesia in open abdominal surgeries in case reports or case series. We aimed to compare the effectiveness of ESPB and anterior Quadratus Lumborum block (QLB III) as a postoperative analgesic for open nephrectomy.
Methods:
Seventy five patients scheduled for open nephrectomy were randomly allocated into three equal groups (25 each); group (C) patients operated under general anesthesia while in (QLB and ESPB) groups, patients received general anesthesia followed by unilateral (QLBIII or ESPB) respectively, with 0.3–0.4 ml/kg of bupivacaine 0.25%. The primary outcome was the 24 h cumulative morphine given postoperatively. The secondary outcomes were the first rescue analgesic time, postoperative pain score, time to perform technique and sensory block coverage.
Results:
The 24 cumulative morphine consumption and first rescue analgesic time were significantly higher and shorter, respectively, in control group compared to the QLB and ESPB groups with no significant difference between interventional groups. VAS score at rest and during movement was significant higher in control group at all different timing measurements compared to the interventional groups. The block performing time was significant shorter in ESPB compared to QLB and the coverage of QLB extends from T8 to L2 and ESPB from T6 to T12.
Conclusion:
The ESPB is as efficient as QLB III to provide analgesia and decrease perioperative opioid consumption, taking into account the technically challenging and the time consuming of QLB III making ESPB a highly promising alternative for postoperative pain relief following open nephrectomy.
1. Introduction
Open surgery remains one of the approaches used for those patients requiring partial or radical nephrectomy and is associated with a high incidence of intense immediate postoperative pain and chronic pain the months following surgery [Citation1,Citation2]. Acute pain physiopathology is explained as it is mediated by inflammatory cell infiltration, activation of spinal cord pain pathways, and also by reflexive muscle spasm. All of these three mechanisms of acute pain are typically ameliorated during the postoperative recovery [Citation3].
Regional anesthesia techniques are commonly recommended for pain management in open nephrectomy as they decrease parenteral opioid requirements and improve patient satisfaction [Citation4].
Erector Spinae Plane block (ESPB), was initially described by Forero et al., 2016 for analgesia in thoracic neuropathic pain [Citation5] and despite its recent description in literature it has also been widely used in both adults and children at different levels for different indications such as chronic shoulder pain (T2), thoracic surgery and breast surgery (T4-5) and upper abdominal surgery (T7-8) [Citation6–9], however, most of the published trials regarding its analgesic effect following major open abdominal surgeries are case reports and rare. In this ultrasound-guided (USG) approach, a local anesthetic (LA) is injected between the erector spinae muscle and the transverse process of the thoracic vertebrae leading to spread of LA cephalad, caudally and through the paravertebral space [Citation5,Citation6,Citation9].
Quadratus Lumborum block (QLB) is a widely used regional anesthesia technique as well. It has been used for reducing postoperative pain after cesarean section, laparotomy or laparoscopic procedure and hip surgery [Citation10–12]. It was defined for the first time by Blanco in 2007, where the LA was injected at the anterolateral aspect of the QL muscle (type I QLB) [Citation13]. Later, Børglum et al.,2013 used posterior transmuscular approach by detecting Shamrock sign and injecting the LA at the anterior aspect of the QL (type III QLB) [Citation14]. Blanco and McDonnell, described another approach by injecting the LA at the posterior aspect of the QL muscle (type II QLB) [Citation15]. Finally, the intramuscular QLB (type IV QLB) was performed by injecting LA directly into the QL muscle [Citation16].
We hypothesized that ultrasound-guided ESPB block has a comparable effect or is even considered a better choice than QLB III as a postoperative analgesia for patients undergoing open nephrectomy under general anesthesia.
2. Patients and methods
2.1. Study population
This Prospective randomized double-blind controlled study was conducted in Zagazig University Hospitals from March 2020 to August 2020. Approval of institutional review board (The research ethical committee of Faculty of Medicine, Zagazig University) with the reference number (ZU-IRB#: 6004/12-4-2020) was obtained and it was registered with ClinicalTrials.gov (NCT04361383).
Adult patients aged 21–60 years old, of either sex, BMI ≤ 30 kg/m2, ASA II or ASA III were scheduled for elective open nephrectomy with flank incision under general anesthesia. Patients were operated with rooftop or chevron (trans-abdominal) incision, those with history of allergy to the LA agents used in this study, Skin lesion at needle insertion site, those with bleeding disorders, sepsis, liver disease, and psychiatric disorders were excluded from this study.
2.2. Sample size calculation
Assuming that mean ± SD of cumulative morphine requirement in control group versus QLB group was (4 ± 1.7 mg versus 3 ± 1.3 mg, respectively) [Citation17], so sample size was calculated by (open Epi) program to be (75 cases) allocated into three equal groups, (25) in each group, with confidence level of 95% and power of test 80% with taking in consideration 10% non-response rate.
2.3. Randomization
The patients enrolled in this study were randomly allocated into three equal groups (25 of each) by a computer-generated randomization table; group (C) (Control group) where patients were operated under general anesthesia, group (QLB): patients received general anesthesia initially then unilateral QLB type III with a volume of 0.3–0.4 ml/kg of bubivacaine 0.25% was performed, group ESPB: patients received general anesthesia initially then unilateral ESPB with a volume of 0.3–0.4 ml/kg of bupivacaine 0.25% was performed. The study was a prospective double-blinded study (The patients and the investigators who were responsible for assessing outcomes were blinded to study group assignment.)
2.4. Preoperative assessment
During their preoperative planning, all participating patients were visited to discuss the purpose and endpoints of the research, to explain the benefits and possible side effects of the technique, and to obtain informed written consent from each patient about the procedure. Particular attention was paid to recording vital signs during physical examination; cardiac and chest symptoms and excluding contraindications. All patients were investigated by complete blood count, coagulation profile, blood sugar levels, and serum urea, serum electrolytes, Liver and kidney functions tests. Patients were taught to measure postoperative pain based on a visual analog score (VAS) on a scale of 0–10, where 0 = no pain and 10 = maximum worst pain. Patients were kept nil per oral for 6–8 h for solid meal and 2 hours for clear fluid prior to the operation.
2.5. Intraoperative
Intravenous access was ensured when the patient entered the operating room with 18 G cannula standard monitors: electrocardiogram, pulse oximetry, non-invasive blood pressure monitor and capnograph, and baseline parameters were registered. Preoxygenation with 100% O2 (4 l/min of O2 for 5 min) was carried out. Anesthesia was induced using fentanyl 1 μg/kg, propofol (1.5–2) mg/kg, endotracheal intubation was facilitated with atracurium 0.5 mg/kg. Anesthesia was maintained with (O2, Sevoflurane mixture), Lungs were ventilated using volume-controlled ventilation and the tidal volume and ventilation rate were adjusted to maintain end-tidal carbon dioxide concentration (EtCO2) at 35–45 mmHg through (Drager ventilator AG, Lubeck, Germany).
Fentanyl was given intraoperatively as an additional bolus dose of 1 μg/kg with an increase in MAP or HR more than 20% from baseline values, atracurium 0.1 mg/kg every 20 to 45 min was given as maintenance of muscle relaxation.
2.6. In the (QLB III) group
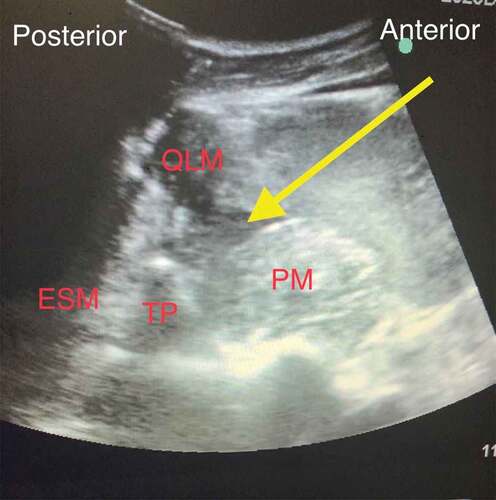
The patient was placed in the lateral decubitus position according to the selected site of surgical intervention. The low-frequency convex probe of Sonosite M Turbo ultrasonography (FUJIFILM Sonosite, Inc., Bothell, WA, USA) was positioned horizontally in the anterior axillary line halfway between the subcostal margin and iliac crest after sterilization of the skin and draping, to locate the triple abdominal muscle layers, then the probe was relocated subsequently to the posterior axillary line until the quadratus lumborum muscle could be visualized with its attachment to the lateral edge of the transverse process of the L4 vertebral body, With the psoas major muscle places anteriorly, the erector spinae muscle posteriorly and the quadratus lumborum muscle adherent to the apex of the transverse process, this is a well-recognizable pattern of a shamrock with three leaves [Citation18]. A 22-gauge, 80 mm needle (Stimuplex D, B-Braun, Germany) was inserted in plane relative to the ultrasound probe passing in posterior to anterior direction through the QL muscle to reach the border between the QL and psoas major muscle (). After confirmation of negative blood aspiration, 1 ml of normal saline for hydro-dissection sign was injected to verify the needle tip and then a volume of 0.3–0.4 ml/kg 0.25% bupivacaine with a maximum volume of 30 ml was injected [Citation17].
2.7. In the ESPB group
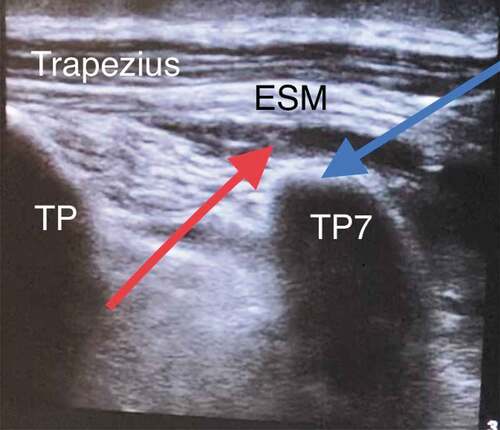
The patient was placed in the lateral decubitus position according to the selected site of surgical intervention. After sterilization and drapping of the skin of the upper back, counting down from seventh cervical vertebrae spine to identify the spine of the seventh thoracic vertebrae (T7). This was related to the tip of the scapular spine. A high-frequency probe of Sonosite M Turbo ultrasonography (FUJIFILM sonosite, Inc., Bothell, WA, USA) was placed across the T7 spine and the probe was moved laterally to identify the transverse process of T7. Thereafter, the probe was moved to a sagittal plane to visualize the erector spinae muscles lying underneath the trapezius muscle. A 22-gauge, 80 mm needle (Stimuplex D, B-Braun, Germany) was inserted medially in-plane relative to the ultrasound probe and directed towards the transverse process. Once the needle was underneath the anterior fascia of the erector spinae muscle (), 1 ml normal saline was injected for hydro-dissection sign to verify the needle tip, and then a volume of 0.3–0.4 ml/kg 0.25% bupivacaine with a maximum volume of 30 ml was injected under the erector spinae muscle into the newly formed space [Citation19].
Figure 2. Performance of the erector spinae plane block (ESPB). TP 7: transverse process of the seventh thoracic vertebra, Trapezius muscle, ESM: erector spinae muscles, Blue arrow: injection point, Red arrow: pointed to the spread of local anesthetic under ESM, lifting it off the transverse processes
Thirty minutes before the end of the surgery regardless of the group allocations all patients were given a mixing of i.v acetaminophen (15 mg/kg) and i.v ketorolac (0.5 mg/kg) for postoperative pain management.
Muscle relaxant reversal with neostigmine 0.04–0.07 mg/kg and atropine 0.02 mg/kg was permitted to wake up from anesthesia, extubated, and maintained on O2: air mixture in the postoperative anesthesia care unit (PACU).
Postoperative analgesia was given in the ward using a fixed scheme in the form of acetaminophen (15 mg/kg 4/day) and ketorolac (0.5 mg/kg 3/day). If the postoperative VAS score ≥3 or patient requested additional analgesia in between VAS score measurement times, rescue analgesia in the form of i.v bolus dose of 1 mg morphine was given.
2.8. Parameters evaluation
Patients’ characteristics: Age, sex, BMI, ASA physical status.
Time needed to perform technique (min): which was defined as the time needed for adequate ultrasonic visualization, needle introduction, and drug injection (time from placement of ultrasound probe on the patient′s skin to the end of local anesthetic injection) [Citation20].
Heart rate (HR), mean arterial blood pressure (MAP), were measured at baseline before induction of anesthesia and then continuously monitored and recorded every 10 min intraoperatively, but recorded at baseline, immediately after induction, at 20 min, 40 min, 1h, 2h after induction and finally at the end of surgery.
Intraoperative cumulative fentanyl (µg).
Number of blocked dermatomes: were assessed after recovery of anesthesia using pinprick and cold loss sensation with iced solutions.
Visual analogue scale (VAS) [Citation21]: was assessed at rest and during movement at 30 min, 1, 3, 6, 12, 24 h postoperatively.
▪1st time to rescue analgesic (min): is the time to ask for the first postoperative analgesia (morphine), and was calculated from the end of operation to patient reporting VAS ≥ 3.
▪Total dose of rescue analgesia (morphine) (primary outcome), that was consumed in the first 24 h postoperatively.
▪Operative time (min) and hospital stay (days).
▪Intraoperative and postoperative complications related to the blocks as local anesthetic toxicity, needle injury to essential organs, retroperitoneal hematoma, hypotension, lower limb weakness, … etc
2.9. Statistical analysis
The Collected data were statistically analyzed using Statistical Package for Social Science software (version 20, SPSS Inc., Chicago, IL). Continuous variables with a normal distribution were reported as mean ± SD and range. Categorical variables were summarized as frequencies and percentages. Numerical data were evaluated using Analysis of variance (ANOVA), and Least Significant Difference (LSD) was used to detect significant difference between each 2 separate group, while qualitative data were evaluated by Chi square test (χ2). P values <0.05 and <0.001were considered statistically significant and highly statistically significant, respectively, P values >0.05 considered non-significant
3. Results
A total of 82 patients scheduled for elective open nephrectomy under general anesthesia, were assessed for eligibility to participate in this study, 7 patients were excluded; 3 patients refused to participate and the other 4 had one or more of the exclusion criteria so the study included 75 patients randomized into three equal groups of 25 each as shown in the CONSORT flow diagram ().
There was no statistically significant difference (p > 0.05) between the studied groups regarding age, sex, BMI, ASA physical status and operative time. As regarding to the intra-operative fentanyl, there was a statistically significant higher dose given in control group compared to the other two groups with no significant difference between the interventional groups. It was also noticed that the time of performing the block was statistically significant shorter (p < 0.001) in ESPB group compared to QLB group ().
Table 1. Patients’ and operative characteristics
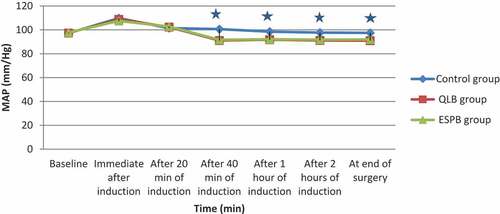
The MAP was comparable at baseline reading, immediately after induction and at 20 minutes after induction, with no significant difference between the studied groups, later on the MAP was statistically significantly reduced in QLB and ESPB groups compared to higher pressure among control group at 40 min, 1 h, 2 hours, and at the end of surgery with no significant difference was noticed in MAP between the two interventional groups at different timings. Also, changes within each group throughout the surgery compared to baseline values were statistically significant, but all were within the clinically accepted range ().
Figure 4. Intraoperative mean arterial pressure (MAP) among the studied groups
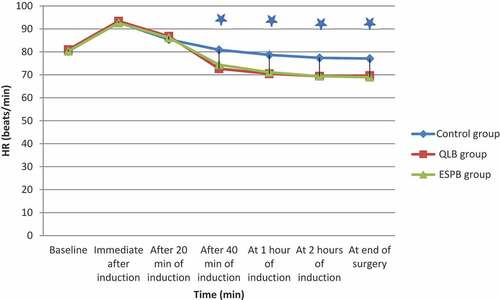
shows that the HR was comparable at baseline reading, immediately after induction and at 20 min later with no significant difference between the studied groups, then HR was statistically significantly reduced in QLB and ESPB groups compared to higher rate among control group at 40 minutes, 1 hour, 2 hours and at the end of surgery, with no significant difference was noticed in HR between the two interventional groups at different timings, as well changes in each group were statistically significant but all were within the clinically accepted range.
Figure 5. Intraoperative heart rate (HR) among the studied groups
The first time to rescue analgesic, total consumed morphine and hospital stay were highly statistically significant shorter, higher and longer, respectively (p < 0.001) in control group compared to the other two interventional groups with no significant difference between these two interventional groups ().
Table 2. Postoperative findings among the studied groups
As regarding VAS at rest and during movement there was highly statistically significant higher scores in control group compared to the interventional groups (with no significant difference between QLB and ESPB group) at all different timing measurements except at 24 hours postoperatively where the three studied groups were comparable at their values ().
Figure 6. Mean postoperative visual analogue score (VAS) at rest and during movement among the studied groups
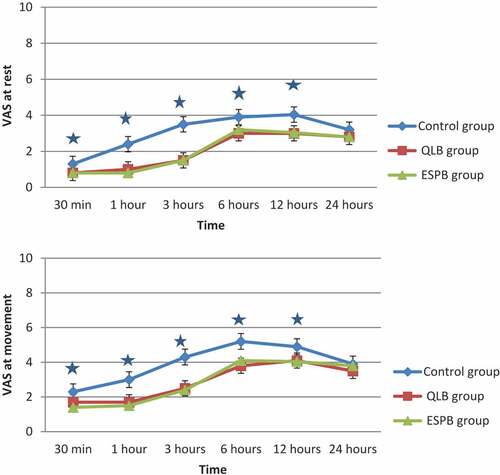
It also was noticed that there was statistically significant increase in VAS score values at rest and during movement within each group following the first 4 hours postoperatively compared to the former postoperative values at 30 min. 1 h and 3 hours ().
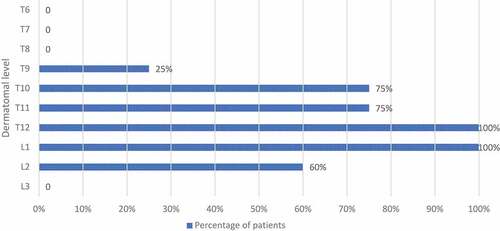
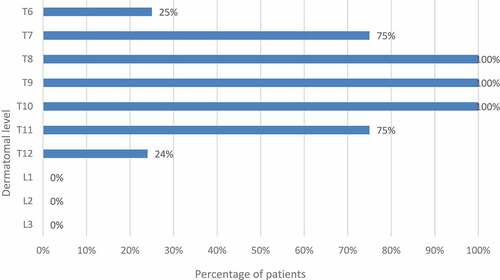
The bar graphs in () demonstrate the variable percentage of spread of sensory block in both QLB and ESPB; where in QLB the majority of patients had lost the cold and pinprick sensation from T9-L2, compared to those in ESPB who had lost cold and pinprick sensation at higher levels from T6-T12.
Figure 8. Multiple bar chart showing dermatomal levels in the Erector spinae plane block (EPSB) studied group
There were no complications reported regarding to the block placement or signs suggesting local anesthetic toxicity in our interventional groups
4. Discussion
Acute pain management following open nephrectomy is a challenging issue due to the large subcostal flank incision that generally employed to offer a wide operative field but unfortunately, it requires a considerable amount of muscle cutting giving raise to somatic pain transmitted through intercostals nerves at (T9-T11), constitute for 70–75% of the postoperative pain and lasts for 72 h [Citation19,Citation22], in addition to visceral pain through sympathetic fibers (T8-T12 spinal segment) which is severe but usually lasts for 24–36 h [Citation19,Citation23]. Poor postoperative pain management leads to restrict ambulation and movement as well as increases pneumonia, thromboembolism, wound dehiscence, chronic pain and prolongs the recovery period [Citation24].
The key to enhanced recovery after open abdominal surgeries is the optimal dynamic analgesia. In the last decade there has been a remarkable shift away from thoracic epidural analgesia which has been long known as the gold standard technique and thus due to the associated difficulty of ambulation, hypotension, excessive i.v fluid administration and complications of neuraxial technique [Citation25].
Anterior quadratus lumborum block (QLB III) is a technique that has the potential to alleviate somatic and visceral pain following abdominal surgeries through spread of local anesthetics into the thoracolumbar fascia which has extensive sensory innervation by both A- and C-fiber nociceptors and mechanoreceptors as well as high-density network of sympathetic fibers to reach to the thoracic paravertebral space [Citation17] however, previous studies revealed some limitations as possible sparing of the upper thoracic dermatomes [Citation26], unexpected motor weakness of lower limb due to possibly involvement of lumbar plexus [Citation27] and also may be complicated with direct needle trauma of the kidney and risks of retroperitoneal spread of hematoma [Citation28].
The ESPB can be used to provide regional analgesia for a wide range of surgical procedures in the anterior, posterior, and lateral thoracic and abdominal regions [Citation7,Citation8] and also to treat acute and chronic pain syndromes [Citation5]. The mechanism of analgesic action of ESPB is reported to be through spread of local anesthetics into the paravertebral space and intercostal spaces of multiple levels with blockade of dorsal and ventral rami with sympathetic fibers leading to somatic and visceral pain relief [Citation9]. In abdominal surgery, the use of the ESPB as a technique for analgesia is relatively minimal and appears in just limited publications. This is the reason why we believe any new trial to use ESPB as a modality for abdominal surgery analgesia is a nobel contribution.
Our study suggested that ESPB has a comparable analgesic effect with QLB III in patient undergoing open nephrectomy, where our results revealed that intraoperative fentanyl consumption and 24 cumulative morphine consumption after surgery were statistically significant higher in control groups compared to the QLB and ESPB group with no significant difference between our two interventional groups.
As well, VAS score at rest and during movement was higher in control group compared to the other two interventional groups (with no significant difference between QLB and ESPB group) at all different timing measurements through the first postoperative day except at 24 hours postoperatively where the three studied groups were comparable at their values, and as a result of this, our results recorded a significant shorter time needed for giving the first rescue analgesic as well as longer hospital stay in the control group compared to QLB and ESPB groups.
This is in line with earlier case series provided by Niraj and Tariq, showing that continuous ESPB provide effective somatic and some visceral analgesia following major abdominal surgeries with a substantial decrease in postoperative morphine consumption and normal rating score (NRS) values over 48 hours postoperatively [Citation19]. Chin et al., who first described in their pilot study the analgesic effect of ESPB with a single-level injection for laparoscopic ventral hernia repair and other abdominal surgery reported a decrease in the opioid consumption and NRS scores over 24 hours [Citation6]. Later studies of laparoscopic cholecystectomy, ERCP or nephrectomy have also concluded that ESPB can produce effective visceral analgesia following single shot or intermittent catheter injection [Citation29,Citation30]. However on the other side, Tulgar et al., in their retrospective study reported ESPB failure and lack of analgesic efficiency in 12 patients of 182 (6.5%) that underwent ESPB for different laparoscopic and open surgeries. The authors reported no common denominator as regard to application level, applied local anesthetic volume, concentration, or surgical procedures in these patients to explain this failure [Citation31].
As regarding to QLB and in agreement with our results Aditianingsih et al., reported that bilateral anterior QLB had a comparable analgesic effect with continuous epidural analgesia following laparoscopic nephrectomy with no significant difference between two groups regarding 24 h morphine consumption and pain scores [Citation17], Similarly, several studies reported the successful analgesic effect of anterior QLB block in adult patients after percutaneous nephrolithotomy or open kidney surgery [Citation32–34].
In our study, the hemodyamic values (MAP and HR) were statistically significant higher in control group after 20 min of induction of general anesthesia till the end of the surgery compared to the QLB and ESPB groups with no significant difference was noticed between the last two groups, that we believed corresponds to the beginning of analgesic effect of our regional blocks and considered as golden standard clinical indicators of the adequacy of analgesia in the two interventional groups and it was reflected on the significant decrease of their intraoperaftive fentanyl consumption compared to the control group doses.
These results were matched with Siam et al., as they found that the incidence of hemodynamic stability was significantly higher in ESPB combined with general anesthesia group than in conventional general anesthesia with multimodal analgesia group of patients undergoing lumbar spine surgery [Citation35]. As well for QLB, in studies provided by Aditianingsih et al., and Sukmono et al., they recorded that MAP and HR in QL group were relatively steadier than in the epidural group of patients undergoing laparoscopic nephrectomy however, there was no difference in the intraoperative fentanyl consumption in both groups and this of course could be justified as the control group in these studies was the epidural one [Citation17,Citation36].
Speaking about the time and the ease of performing the block that considered as one of the important elements of choice between different regional blocks, our study reported a statistically significant shorter performance time for ESPB compared to QLB performance time, and this attributed to that the anterior QLB need technically full visualization of the needle tip by the convex probe during injection due to the proximity of the injection site to the abdominal structures and the risk of retroperitoneal hematoma, unlike the simplicity of the ESBP thanks to its easily identifiable ultrasonographic landmarks and endpoint for injection aiming to bone structure and not towards paravertebral space near the pleura and major blood vesseles thus reduce the possibility of serious complications.
In agreement with our findings Ökmen and Ökmen, indicated the skill and time required to perform anterior QLB to avoid potential hazards despite its analgesic effect after percutaneous nephrolithotomy compared to patient-controlled analgesia group [Citation32]. Similarly Dewinter et al., referred to the technically demanding and time consuming of QLB furthermore, it did not provide superior postoperative analgesia in the laparoscopic colorectal surgery when compared to systemic lidocaine [Citation37].
No complications have been identified with regard to block placement or signs indicating local anesthetic toxicity in our interventional groups in the current sample.
This is inconsistent with Wikner, who reported a case of lower limb motor weakness following lateral quadratus lumborum block for gynecological laparoscopy and suggested that due to spread of LA either to lumbar paravertebral space or to the lumbar plexus, however this study included one case which makes it difficult to generalize to large sample size [Citation27]. Moreover, Dewinter et al., found that more patients in the QL-group showed subjective symptoms of local anesthetic systemic toxicity even though they did not surpass the reference value for toxicity of plasma ropivacaine-concentration in the blood sample of these patients, but they commented on this, that caution is needed when interpreting these signs as the correlation between signs of toxicity and blood levels is determined by several factors as anatomical, physiological, and pharmacokinetic factors and this made them not recommend the use of QLB as analgesic approach for laparoscopic colorectal surgery [Citation37].
It should be noted that we have attempted to avoid one of the most common limitations in the previous studies relating to ESPB and QLB, namely the evaluation of the dermatoma coverage of each block in the postoperative period in patients undergoing open nephrectomy surgery. In our results, the majority of patients in ESPB group have lost their cold and pinprick sensation from T6 to T12 whereas those in QLB group have lost their cold and pinprick sensation at lower levels from T9 to L2. As a consequence, sensory blockage levels in both groups outweigh the likelihood of having adequate analgesic effects after nephrectomy because the flank incision is fully blocked. However, Warusawitharana et al., stated in their case series study the possibility of sparing of upper thoracic dermatomes with the transmuscular quadratus lumborum block used for analgesia for open renal surgery [Citation26], which could decrease its efficacy as an upper abdominal surgery analgesic. Chin et al., on the other hand, observed radiologically cadaveric distribution of ESPB local anesthetic extending from the injection site to 3 or 4 levels cranially and caudally [Citation6] therefore, we opted to apply a single-level injection at T7 level to block both supra-umbilical and infra-umbilical dermatomes that are inconsistent with the dermatomes affected by open nehprectomy rendering it as effective alternative analgesic technique in such surgeries. Moreover, it could be performed at different levels for different purposes for other clinical situations.
However, our study has some limitations that are needed to be listed. First, a single injection was used for both groups to detect the exact duration of the block however, a catheter insertion for continuous analgesia can be used instead to extend the duration of analgesia and further reduce postoperative morphine consumption but this does not affect our take-home message. Secondly, the extent of the blocks was tested only once after recovery of anesthesia nevertheless, we tried to use the assessment of pain score as an indirect indicator of the block’s continued efficacy. Third, our study focused on short-term outcomes for the first 24 hours after surgery and long-term outcomes are still unclear, therefore future studies may be recommended to research such variable agents.
5. Conclusion
The ultrasound-guided ESPB is as efficient as anterior QLB (III) to provide effective analgesia, decrease intraoperative and postoperative opioid consumption and is beneficial to shorten hospital stay in patients undergoing open nephrectomy. With its ability to block both supra-umbilical and infra-umbilical dermatomes with a single-level injection at the level of the T7 transverse process, taking into account the technically challenging, the time consuming performance and the possibility of sparing of upper thoracic dermatomes and undesirable complications of anterior QLB, ESPB is a highly promising alternative to be enhanced as a modality for postoperative nephrectomy pain management.
Disclosure statement
There are no conflicts of interest.
References
- Gupta V, Yadav SK, Dean E, et al. Paediatric laparoscopic orchidopexy as a novel mentorship: training model. African Journal of Paediatric Surgery. 2013;10(2):117–121.
- Bravi CA, Larcher A, Capitanio U, et al. Perioperative outcomes of open, laparoscopic, and robotic partial nephrectomy: a prospective multicenter observational study (the record 2 project). Eur Urol Focus. 2019;11:S2405-4569(19)30335–9.
- Pöpping DM, Zahn PK, Van AHK, et al. Effectiveness and safety of postoperative pain management: a survey of 18925 consecutive patients between 1998 and 2006 (2nd revision): a database analysis of prospectively raised data. Br J Anaesth. 2008;101(6):832–840.
- Capdevila X, Moulard S, Plasse C, et al. Effectiveness of epidural analgesia, continuous surgical site analgesia, and patient-controlled analgesic morphine for postoperative pain management and hyperalgesia, rehabilitation, and health-related quality of life after open nephrectomy: a prospective, randomized, controlled study. Anesth Analg. 2017;124(1):336–345.
- Forero M, SD A, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627.
- Chin KJ, Adhikary S, Sarwani N, et al. The analgesic efficacy of pre- operative bilateral erector spinae plane (ESP) blocks in patients having ventral hernia repair. Anaesthesia. 2017;72(4):452–460.
- Ueshima H, Otake H. Erector spinae plane block provides effective pain management during pneumothorax surgery. J Clin Anesth. 2017;40:74.
- Restrepo-Garces CE, Chin KJ, Suarez P, et al. Bilateral continuous erector spinae plane block contributes to effective postoperative analgesia after major open abdominal surgery: a case report. A A Case Rep. 2017;9(11):319–321.
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;42:372–376.
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762.
- Abd ESE, Ahmed FM. Ultrasound-guided quadratus lumborum block versus transversus abdominis plane block in children undergoing laparoscopic appendectomy: a randomized controlled study. Research and Opinion in Anesthesia & Intensive Care. 2020;7(2):167–175.
- McCrum CL, Ben-David B, Shin JJ, et al. Quadratus lumborum block provides improved immediate postoperative analgesia and decreased opioid use compared with a multimodal pain regimen following hip arthroscopy. J Hip Preserv Surg. 2018;5(3):233–239.
- Blanco R. TAP block under ultrasound guidance: the description of a ‘nonpopstechnique’. Reg Anaesth Pain Med. 2007;32:130.
- Børglum J, Moriggl B, Jensen K, et al. Ultrasound-guided transmuscular quadratus lumborum blockade. Br J Anaesth. 2013;111(Issue eLetters Supplement). DOI:10.1093/bja/el_9919
- Blanco R, McDonnell JG. Optimal point of injection: the quadratus lumborum type I and II blocks. Anesthesia. 2013;68:4.
- Murouchi T. Quadratus lumborum block intramuscular approach for pediatric surgery. Acta Anaesthesiologica Taiwanica. 2016;54:135–136.
- Aditianingsih D, Pryambodho AN, Tantri AR, et al. A randomized controlled trial on analgesic effect of repeated quadratus lumborum block versus continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019;19:221.
- Ueshima H, Otake H, Jui-An L. Ultrasound-guided quadratus lumborum block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:1–7.
- Niraj G, Tariq Z. Continuous erector spinae plane (ESP) analgesia in different open abdominal surgical procedures: a case series. J Anesth Surg. 2018;5(1):57–60.
- Carassiti M, Cappiello D, Galli B. One shot six centres: a new strategy in ultrasound guided paravertebral block. J Anesth Clin Res. 2015;6:580–583.
- Katz J, Melzack R. Measurement of pain. Surg Clin North Am. 1999;79:231–252.
- Eand C, Pichel AC. Anaesthesia for nephrectomy. BJA Educ. 2016;16(3):98–101.
- Ness TJ, Gebhart GF. Visceral pain: a review of experimental studies. Pain. 1990;41:167–234.
- Alper I, Yüksel E. Comparison of acute and chronic pain after open nephrectomy versus laparoscopic nephrectomy: a prospective clinical trial. Medicine (Baltimore). 2016;95(16):e3433.
- Hughes MJ, Ventham NT, McNally S, et al. Analgesia after open abdominal surgery in the setting of enhanced recovery surgery: a systematic review and meta-analysis. JAMA Surg. 2014;149(12):1224–1230.
- Warusawitharana C, SHMA B, Jackson BL, et al. Ultrasound guided continuous transmuscular quadratus lumborum analgesia for open renal surgery: a case series. J Clin Anesth. 2017 Nov;42:100–101.
- Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthesia. 2017;72(2):230–232.
- Elsharkawy H, El-Boghdadly K, Barrington M. Quadratus lumborum block: anatomical concepts, mechanisms, and techniques. Anesthesiology. 2019;130:322–335.
- Tulgar S, Selvi O, Kapakli MS. Erector spinae plane block for different laparoscopic abdominal surgeries. Case reports. Anaesthesiol. 2018;39((4):):72–81.
- Kim S, Bang S, Kwon W. Intermittent erector spinae plane block as a part of multimodal analgesia after open nephrectomy. Chin Med J (Engl). 2019;132(12):1507–1508.
- Tulgar S, Selvi O, Senturk O, et al. Ultrasound-guided erector spinae plane block: indications, complications, and effects on acute and chronic pain based on a single-center experience. Cureus. 2019;11(1):e3815.
- Ökmen K, Ökmen BM. Ultrasound-guided anterior quadratus lumborum block for postoperative pain after percutaneous nephrolithotomy: a randomized controlled trial. Korean J Anesthesiol. 2020;73(1):44–50.
- Ueshima H, Otake H. Clinical experiences of unilateral anterior sub-costal quadratus lumborum block for a nephrectomy. J Clin Anesth. 2018;44:120.
- Corso RM, Piraccini E, Sorbello M, et al. Ultrasound-guided transmuscular quadratus lumborum block for perioperative analgesia in open nephrectomy. Minerva Anestesiol. 2017;83:1334–1335.
- Siam EM, Abo ADM, Elmedany S, et al. Erector spinae plane block combined with general anaesthesia versus conventional general anaesthesia in lumbar spine surgery. Egypt J Anaesth. 2020;36(1):201–226.
- Sukmono RB, Rahendra SA, Aditianingsih D, et al. Comparison of intraoperative hemodynamic stability between quadratus lumborum and epidural block in patients who underwent laparoscopic nephrectomy. J Phys Conf Ser. 2019;1246:012064.
- Dewinter G, Coppens S, Van de Velde M, et al. Quadratus lumborum block versus perioperative intravenous lidocaine for postoperative pain control in patients undergoing laparoscopic colorectal surgery: a prospective, randomized, double-blind controlled clinical trial. Ann Surg. 2018;268(5):769–775.