ABSTRACT
Background: Lung atelectasis is a common complication post-cardiac surgery that can affect patient’s outcomes significantly. The current study aimed to evaluate the efficacy of transalveolar pressure measurement (PTA) using esophageal manometer as a monitoring parameter during a modified stepwise staircase lung recruitment employing adaptive ventilation mode (AVM) in postcardiac surgery hypoxic patients.Settings and Design: This study was a prospective case series study.Methods: The study was carried out on 62 adult patients who were undergone on-pump cardiac surgeries. After haemodynamic stabilization of the patient in ICU, esophageal manometer catheter had been inserted then a modified stepwise staircase alveolar recruitment maneuver was done with the use of the transalveolar pressure as the main parameter for the monitoring of the effectiveness and safety of the recruitment maneuver. Agreement between parameters was done and weighted kappa, standard error and confidence intervals at 95% (95% CI) were calculated.Results: During the alveolar recruitment maneuver, the PTA Insp detected 96.7% of the patients with alveolar overdistention and the PTA Exp detected 98.3% of the patients with alveolar optimum PEEP. Statistical significant improvement in both hypoxic index and ultrasound lung aeration score from before to after alveolar recruitment.Conclusion: Transalveolar pressure inspiratory and expiratory were accurate monitoring parameters for alveolar overdistention and optimum PEEP detection selectively.
Abbreviations: ALI: Acute lung injury; ARDS: Adult respiratory distress syndrome; AVM: Adaptive ventilation mode; Cdyn: Compliance Dynamic; ETT: Endotracheal tube; IBW: Ideal body weight; ICU: Intensive care unit; MBP: Mean blood pressure; MVTarget:Minute volume target; PEEP: Positive end expiratory pressure; PES: Esophageal pressure; PLimit: Pressure limit; PPL: Pleural pressure; PTA: Transalveolar pressure measurement; PTA Exp: Expiratory transalveolar pressure; PTA Insp: Inspiratory transalveolar pressure; RM: Recruitment maneuvers; SpO2: Percutaneous Oxygen saturation
1. Introduction
Pulmonary dysfunction is a common complication post-cardiac surgery that can affect patient’s outcomes and health economics. It is recognized that many patients post-cardiac surgery will have altered pulmonary mechanics which may appear in a wide range of manifestations, from mild atelectasis which is the commonest to life-threatening acute lung injury (ALI) or adult respiratory distress syndrome (ARDS) [Citation1].
Postcardiac surgery hypoxia due to alveolar atelectasis results in prolongation of the mechanical ventilation time, intensive care unit (ICU) stay, need for tracheostomy, increased costs and resource utilization. It can be detected using hypoxic index, oxygenation index and oxygen saturation index [Citation2].
Alveolar recruitment maneuvers (RM) are procedures that are very important to increase transpulmonary pressure to promote the opening of the largest possible number of alveoli aiming to improve gas distribution within the alveoli [Citation3].
Different types of alveolar recruitment maneuvers have been described including sustained inflation, three consecutive sighs, extended sigh (e-sigh), RAMP and Stepwise staircase recruitment maneuver [Citation4].
Stepwise staircase recruitment maneuver may allow better oxygenation and less haemodynamic instability than sustained inflation one. However, the optimal RM (with the best balance of benefit and harm) is still under discussion [Citation5].
Esophageal pressure (PES) can be used as a substitute for pleural pressure (PPL) to calculate the elastic and resistive forces in the lung. To separate the pressure needed to expand the lung and the pressure needed to expand the chest wall the recording of esophageal pressure is necessary. Esophageal Pressure can be measured by esophageal manometer and then the transpulmonary pressure can be calculated by: PAW- PPL = PTP [Citation6].
The transalveolar pressure (PTA) is the difference between alveolar pressure and pleural pressure which is calculated after tube resistance compensation so it is more precise than transpulmonary pressure [Citation7].
Ultrasound has favorable features to assess RM due to its high specificity and sensitivity to detect lung collapse together with its non-invasiveness, availability and simple use at the bedside especially with the high-risk patient of transportation like post-cardiac surgery patient [Citation8].
Adaptive ventilation mode (AVM) is a new ventilatory mode, which uses a closed-loop system. The operator just sets a maximum plateau pressure and percentage of minute ventilation support which is measured based on the patient’s ideal weight. It automatically selects the target ventilatory pattern based on user inputs, taking into account the respiratory mechanics data from the ventilator monitoring system (resistance, compliance and auto-PEEP) [Citation9].
2. Patients and methods
After approval of the Alexandria University Local Ethics Committee and with written informed consent from each patient, the present prospective case series study had been carried out in cardiac surgery ICU of Alexandria Main University hospitals on 62 adult patients who were undergone on-pump cardiac surgeries.
Patients with the following criteria had been excluded: contraindications for the use of esophageal catheter including esophageal ulcerations, tumors, diverticulitis, bleeding varices, recent esophageal or gastric surgery, sinusitis, epitaxis and recent nasopharyngeal surgery, postoperative severe haemodynamic instability on high inotropic support, ejection fraction less than 35%, severe restrictive or obstructive lung disease, extremes of age (<19 and >75 years) and morbidly obese patients with BMI > 40 kg/m2.
After the patient arrival to the ICU, the patient had been mechanically ventilated using AVM mode in Bellavista 1000 e ventilator with the following basal settings: Patient’s height in cm (the ventilator had measured the ideal body weight (IBW) and the target minute volume (MVTarget)), 100% minute ventilation support which was adjusted according to PaCO2 level of the ABG (between 30 and 35 mmHg), PEEP 5 cmH2O, pressure limit (PLimit) 35 cmH2O, oxygen percentage (O2%) 80% which had been decreased gradually over one hour to reach 50%.
Sedation with propofol 10% infusion 50–150 mcg/kg/min and fentanyl infusion 1–2 mcg/kg/hour IV. Basal hypoxic index (<250) and ultrasound-guided lung aeration score (>score 3) [Citation10] () had been done to detect atelectatic hypoxia.
Table 1. Ultrasound-guided lung aeration score [Citation10]
Patients had been examined by C60x transducer 2–5 MH of SonoSite M-Turbo ultrasound machine. Six basic regions had assessed for each lung. Each hemithorax was divided into anterior, lateral and posterior regions by the anterior and posterior axillary lines. The regions had been further subdivided into upper and lower areas.
After haemodynamic stabilization of the patient, esophageal manometer catheter had been inserted through the patient’s nostril towards the lower part of the esophagus with the same technique of nasogastric tube insertion. The estimated depth in which to place catheter could be measured by the distance from nostril to ear tragus to xyphoid.
The balloon of the catheter had been inflated, stylet of the catheter had been removed. The cardiac oscillations and the esophageal and the transalveolar pressure curves could be noticed on the ventilator screen then the catheter had been secured with tape to prevent motion removal or displacement.
A modified stepwise staircase alveolar recruitment maneuver had been used. In which stepped increase in the PEEP level 2 cm H2O every 2 minutes and the AVM mode would maintain the driving pressure to maintain tidal volume. The stepped increase was done till near overdistention.
Alveolar over distention criteria included: inspiratory transalveolar pressure (PTA Insp) >15 cm H2O [Citation11] and (or) dynamic compliance (Cdyn) decreased from its previous reading, SpO2 decreased 1% from its previous reading and MBP decreased 25% from the baseline [Citation12,Citation13].
After detection of the alveolar overdistention, a stepped decrease in the PEEP level 2 cmH2O every 3 minutes till the derecruitment which was detected by expiratory transalveolar pressure (PTA Exp), Cdyn and SpO2 then return to the PEEP level 2 cmH2O above the derecruitment one which was the optimal PEEP.
Alveolar derecruitment criteria included: transalveolar pressure expiratory (PTA Exp) <1 cmH2O [Citation11] and (or) dynamic compliance (Cdyn) decreased from its previous reading and SpO2 decreased 1% from its previous reading.
After the alveolar recruitment maneuver was done, another hypoxic index and ultrasound-guided lung aeration score were done to confirm the effectiveness of the recruitment maneuver.
Score 0–3: Successful recruitment. Score > 3: Failed recruitment.
3. Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. Qualitative data were described using number and percent. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level.
The used tests were
1 – Kappa (κ)
Kappa test for agreement was used.
2 – Sensitivity
The capacity of the test to correctly identify diseased individuals in a population “TRUE POSITIVES”. The greater the sensitivity, the smaller the number of unidentified case “false negatives”
3 – Specificity
The capacity of the test to correctly exclude individuals who are free of the disease “TRUE NEGATIVES”. The greater the specificity, the fewer “false positives” will be included
4 – Positive Predictive value (PPV)
The probability of the disease being present, among those with positive diagnostic test results
5 – Negative Predictive value (NPV)
The probability that the disease was absent, among those whose diagnostic test results were negative
6 – Accuracy
Rate of Agreement = (True positives + True negatives)/Total tested x 100
7 – Paired t-test
For normally distributed quantitative variables, to compare between two periods.
4. Results
This case series study was performed in the cardiac surgery ICU of Alexandria Main University hospitals on 62 adult patients after on-pump cardiac surgeries. Twenty-six Patients underwent single valvular replacement surgery, 22 Patients underwent CABG with two or three vessels Surgery, 13 Patients underwent combo CABG and valvular replacement surgery and 1 patient underwent ASD repair surgery.
All Patients starting the study completed it successfully except one patient who was excluded after twice time malpassage of esophageal manometer catheter to the trachea (). Patients were all included in the subsequent statistical analysis.
The included patients were 38 males and 34 females. The patients’ ages were between 20 and 30 years old in 9 patients, 30–40 years old in 18 patients, 40–50 years old in 10 patients, 50–60 years old in 15 patients and 60–70 years old in 10 patients.
The BMI was normal in six patients, overweight in 21 patients, preobese in 13 patients, obese class I in 14 patients and obese class II in 8 patients.
Thirty-five Patients had normal pulmonary function tests, 12 Patients had mild obstructive pulmonary disease, 8 Patients had mild restrictive lung disease, 5 Patients had moderate obstructive pulmonary disease and 2 patients had moderate restrictive pulmonary disease.
All patients before the start of the recruitment maneuver had stable haemodynamics, endotracheal tube (ETT) suction and automatic tube compensation modality had been applied.
Only one patient was excluded from the study due to two times malposition of the esophageal manometer catheter towards the trachea during its insertion and after inflation of the manometer cuff caused partial obstruction of the ETT.
Hypoxic index and ultrasound-guided lung aeration scores were done for all patients before and after the recruitment maneuver to detect the recruitment maneuver effectiveness.
(A) During the ascending part of the recruitment maneuver (detection of alveolar overdistension):
- The PTA Insp detected 96.7 % of the patients with alveolar overdistention ().
-There was poor agreement in the detection of alveolar overdistention between PTA Insp and Cdyn (), SpO2 and MBP (weighed kappa - 0.063, 0.029 and 0.021, respectively).
- The Cdyn detected 62.9 % of the patients with alveolar overdistention ().
- The SpO2 detected 33.8% of the patients with alveolar overdistention.
- The MBP detected 27.4% of the patients with alveolar overdistention.
Table 2. Agreement between Cdyn (ml/cm H₂O) (inspiratory) and PTA Insp (cmH₂O)
(B) During the descending part of the recruitment maneuver (detection of the optimum PEEP):
- The PTA Exp detected 98.3% of the patients alveolar optimum PEEP ().
- There was poor agreement in the detection of the optimum PEEP between PTA Exp and Cdyn () and SpO2 (weighed kappa 0.029 and 0.01, respectively).
- The Cdyn detected 91.9 % of the patients alveolar optimum PEEP ().
- The SpO2 detected 24.1% of the patients alveolar optimum PEEP.
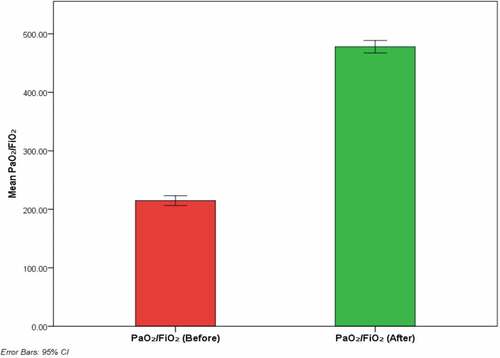
(C) As regards the hypoxic index in the detection of the effectiveness of the lung recruitment maneuver:
- Statistical significant improvement in the hypoxic index after the alveolar recruitment maneuver (P = 0.000) ().
Table 3. Agreement between Cdyn (ml/cm H₂O) (expiratory) and PTA Exp (cmH₂O)
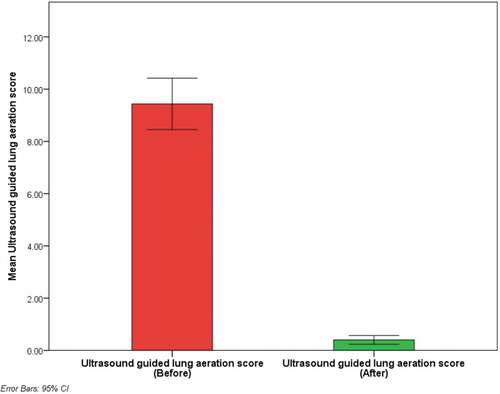
(D) As regards the ultrasound lung aeration score in the detection of the effectiveness of the lung recruitment maneuver:
- Statistical significant improvement in the ultrasound lung aeration score after the alveolar recruitment maneuver (P = 0.000) ().
5. Discussion
In the current study, the modified stepwise staircase alveolar recruitment maneuver could effectively recruit the atelectatic alveoli and maintain them opened which was expressed by improvement of oxygenation, hypoxic index and decreased ultrasound lung aeration score.
As regards the duration of the maneuver, it was relatively long. It was around 25 minutes. This long duration of the maneuver might of benefits as it allowed gradual opening of the alveoli, avoided sudden overdistention and permitted a good time to notice the changes in all measured monitoring parameters.
Regarding the haemodynamic changes during the maneuver, the significant decrease in the MBP 25% from the baseline (overdistention) had been occurred in 15 patients out of the total 62 patients. This decrease in the MBP might be due to mild hypovolemia that was not detected at the time of the maneuver and this decrease in MBP had no harmful effects on the patient as it was immediately overcome by a decrease in the PEEP level to the descending limb of the maneuver.
In agreement with the current study, a meta-analysis including 12 trials had been published by Cui et al. [Citation14] about the use of stepwise staircase alveolar recruitment maneuver post cardiac surgery. The results emphasized the effectiveness in the management of postoperative pulmonary complications without significant haemodynamic instability.
However most of the studies published about post-cardiac surgery lung recruitment were sustained inflation. Celebi et al. [Citation15] reported in a study about the use of two different techniques in the sustained inflation maneuver post cardiac surgery. The conclusion was that the sustained inflation maneuver with slightly lower PEEP (20 cmH2O) was effective in lung recruitment as the higher PEEP (40 cmH2O) but with more haemodynamic stability.
The explanation of the frequent use of the sustained inflation maneuver than the stepwise staircase alveolar recruitment might be the duration of the maneuver. However both maneuvers are effective in the alveolar inflation and more or less the haemodynamic effects.
The monitoring parameters during the lung recruitment maneuver are more important than the maneuver itself, they act as a guide to allow safe and effective maneuver.
Regarding the use of PTA Insp for the detection of the alveolar overdistention. In the present study PTA Insp detected 96.7% of the patients with alveolar overdistention during the ascending limb of the recruitment maneuver.
The overdistention PEEPs in the current study were between 9 cmH2O as the least overdistention PEEP in the study and 19 cmH2O as the highest overdistention PEEP. These PEEPs were correlated with the pre-recruitment hypoxic index and ultrasound lung aeration score.
In agreement with the current study in the use of PTA Insp in the detection of the alveolar overdistention, Arnal et al. [Citation11] reported that the transalveolar pressure inspiratory should be kept below 15 cmH2O and the increase above this pressure was considered as an alveolar overdistention. Also authors reported that the transalveolar pressure was more accurate than transpulmonary pressure in evaluation of the alveolar condition during inflation and deflation.
In the present study, accurate detection of the optimum PEEP in the current study had been done by PTA Exp (98.3%) which decreased less than 1 cmH2O at the atelectatic PEEP level so the optimum PEEP was the PEEP level 2 cmH2O above the atelectatic one that maintains PTA Exp > 1 cmH2O.
Arnal et al. [Citation11] reported that the transalveolar pressure expiratory should be kept above 1 cmH2O to keep the alveoli patent and prevent recollapsing after recruitment.
There are different image modalities that can be used for the diagnosis of atelectasis and recruitment effect post-cardiac surgery including lung ultrasound, chest x-ray and CT chest.
Lung ultrasound detected all hypoxic patients with atelectasis postoperative and differentiated between different grades of atelectasis which was correlated with the degree of hypoxia detected by the hypoxic index. Also it was accurate in the detection of the effectiveness of the lung recruitment maneuver.
In agreement with the present study, Touw et al. [Citation16] reported in a study on 177 patients aiming to compare between lung ultrasound and chest x-ray in the detection of the post-cardiac surgery pulmonary complications. The results were that the lung ultrasound detected 90% of the pulmonary complications, however the chest x-ray detected only 61% of the complications and concluded the effectiveness of the lung ultrasound over the chest x-ray.
Steppan et al. [Citation17] reported in a study about the feasibility of the use of the lung ultrasound post pediatric cardiac surgery in the detection of pulmonary complications. The results showed that the Lung ultrasound was comparable to the gold standard CT chest in the detection of the pulmonary complications.
6. Conclusion
Stepwise staircase alveolar recruitment maneuver was effective and safe maneuver to inflate the atelectatic alveoli with non-significant complications. It could be monitored accurately by esophageal manometer transalveolar pressure measurement. Also Hypoxic index and ultrasound lung aeration score could be used to detect atelectatic and the effectiveness of the lung recruitment maneuver.
7. Limitations
There were several limitations in the present study, being a small-sized, single-center study. Technical difficulty during esophageal catheter insertion as malpassage of the catheter towards the trachea in one patient. There was no comparison imaging technique to the ultrasound. One patient showed mild bubbling in the chest tubes after the recruitment which might rupture bullous Endotracheal tube.
Disclosure statement
The authors declare that they have no conflict of interest.
Additional information
Funding
References
- Szelowski LA. Postoperative pulmonary complications of cardiac surgery. Curr Probl Surg. 2018;52:531.
- Santos NPD, Mitsunaga RM, Borges DL, et al. Factors associated to hypoxemia in patients undergoing coronary artery bypass grafting. Revista Brasileira De Cirurgia Cardiovascular. 2013;28(3):364–370.
- Suzumura EA, Amato MB, Cavalcanti AB. Understanding recruitment maneuvers. Intensive Care Med. 2016;42:908–911.
- Kallet RH, Lipnick MS. Is there still a role for alveolar recruitment maneuvers in acute respiratory distress syndrome? J Thorac Dis. 2018;10(1):85–90.
- Marini JJ. Should we titrate positive end-expiratory pressure based on an end-expiratory transpulmonary pressure? Ann Transl Med. 2018;6(19):391.
- Gulati G, Novero A, Loring SH, et al. Pleural pressure and optimal positive end-expiratory pressure based on esophageal pressure versus chest wall elastance: incompatible results. Crit Care Med. 2013;41(8):1951–1957.
- Alpert B, Dart R, Quinn D. Oscillometric blood pressure. J Am Soc Hypertens. 2014;8(12):930–938.
- Volpicelli G. Lung Sonography. J Ultrasound Med. 2013;32(1):165–171.
- Branson D. Modes to Facilitate Ventilator Weaning. Respir Care. 2012;57(10):1635–1648.
- Lung LJ. Ultrasound in Critically Ill Patients. Korean J Crit Care Med. 2016;31(1):4–9.
- Jean-Michel A. Esophageal Pressure Curve. In: Arnal J, editor. Monitoring mechanical ventilation using ventilator waveforms. Bonaduz, Switzerland: Springer; 2018. p. 149–180.
- Menon K, Sutphin P, Bartolome S, et al. Chronic thromboembolic pulmonary hypertension: emerging endovascular therapy. Cardiovasc Diagn Ther. 2018;8(3):272–278.
- Nève V, De La Roque ED, Leclerc F, et al. Ventilator-induced overdistension in children: dynamic versus low-flow inflation volume-pressure curves. Am J Respir Crit Care Med. 2000;162(1):139–147.
- Cui Y, Cao R, Li G, et al. The effect of lung recruitment maneuvers on post-operative pulmonary complications for patients undergoing general anesthesia: a meta-analysis. PloS One. 2019;14(5):e0217405.
- Celebi S, Menda F, et al. The pulmonary and hemodynamic effects of two different recruitment maneuvers after cardiac surgery. Anesth Analg. 2007;104(2):384–390.
- Touw HR, Parlevliet KL, Beerepoot M, et al. Lung ultrasound compared with chest X-ray in diagnosing postoperative pulmonary complications following cardiothoracic surgery: a prospective observational study. Anaesthesia. 2018;73(8):946–954.
- Steppan D, DiGiusto M, Steppan J. Perioperative lung ultrasound in the pediatric intensive care unit—beyond the vasculature and parenchyma. J Cardiothorac Vasc Anesth. 2020;34(4):956–958.