ABSTRACT
Background:
Parturients scheduled to elective cesarean section usually develop higher anxiety and stress symptoms. Pregabalin decreases preoperative anxiety and intubation stress response; however, its effects on mother and newborn have not been investigated yet. The primary aim of this study was to investigate the effect of single-dose oral pregabalin on preoperative maternal anxiety, and the secondary aims were to assess its effect on attenuating the stress response to laryngoscopic intubation, maternal sedation, and neonatal clinical outcomes in parturients undergoing cesarean section.
Methods:
A prospective double-blind randomized-controlled clinical study. Sixty minutes before induction of anesthesia, 74 parturients scheduled for elective cesarean section under general anesthesia were randomly allocated into two groups: Group A (n = 37) received single oral pregabalin 150 mg capsule and Group B (n = 37) received oral multivitamin capsule.
Results:
Group A showed statistically significant lower number of parturients with moderate and high anxiety [11(29.73%) and 2(5.41%)], respectively, and increasing number of parturients with low anxiety [24(64.86%)] using STAI compared to [13(35.13%) and 14(37.84%)] for moderate and high anxiety, respectively, and [10(27.03%)] for low anxiety in group B and to basal numbers (p = 0.001). Rise in mean (heart rates and arterial blood pressures) from baseline values in both groups at 0 min (at intubation) and both groups were comparable at all measured time points (p > 0.05). Also, rising of mean serum glucose and cortisol levels at 10 min post-intubation from basal in both groups and both groups were comparable (p > 0.05). Mean APGAR scores were normal and both groups were comparable. All parturients were alert by AVPU score and no side effects were detected in both groups.
Conclusion:
Pre-emptive single oral 150 mg pregabalin is effective in decreasing maternal anxiety with good neonatal outcomes, but has no effect on stress response of laryngoscopic intubation during cesarean section.
1. Introduction
Despite the fact that regional anesthesia (RA) represents the method of choice and is superior to general anesthesia (GA) for cesarean section delivery, there are situations where GA is a better choice such as the presence of contraindications to RA and parturients refusal. Maternal anxiety is increased by anesthesia, cesarean delivery, and the experience of childbirth. It is associated with increasing risk of preterm delivery, low birth weight, and increasing severity of postoperative pain. Anxiety exaggerates the autonomic stress response causing uterine arteries vasoconstriction which leads to fetal distress [Citation1–3].
During cesarean delivery, the induction-delivery time is usually performed under light anesthesia due to the risk of anesthesia-induced respiratory depression of the neonate. The risk of such approach is the increased probability of maternal awareness intra-operatively and exaggerated cardiovascular stress response and neuroendocrine to laryngoscopy and endotracheal intubation. Mechanical stimulation of laryngeal proprioceptors elicits increased secretion of cortisol and catecholamine with subsequent elevation of blood pressure from 40 to 50% and heart rate up to 20% during direct laryngoscopy and endotracheal intubation [Citation4,Citation5].
The use of nonopioid drugs such as gabapentinoid has taken a part of the multimodal regimen for reducing anxiety and the intubation response. Pregabalin is a gabapentinoid with anxiolytic, sedative, antinociceptive, antihyperalgesic, and antiallodynic effects. It is absorbed completely after oral administration with little side effects [Citation6,Citation7].
Some studies investigated the use of pregabalin in pregnant mothers and proven clinically no adverse effects on newborn were detected but in the field of analgesia [Citation8,Citation9]. However, to the best of our knowledge, there is no available literature until now to investigate its effects on preoperative anxiety, stress response to intubation among parturients and neonatal outcomes after cesarean delivery. The primary aim of this study was to investigate the effect of pre-emptive single-dose oral pregabalin on maternal anxiety, and the secondary aims were to assess its effect on attenuating stress response to laryngoscopic intubation, maternal sedation, and neonatal clinical outcomes in parturients undergoing cesarean section.
2. Materials and methods
After approval of our University’s Institutional Review Board (IRB #6408-11-10-2020) and registered on clinicaltrials.gov. (NCT04622202 date: 6–11-2020), written informed consent was obtained from all parturients participating in the trial before enrollment.
This was a prospective double-blind randomized-controlled clinical study, conducted on 74 parturients from November 2020 to February 2021. The age range of parturients included in this study was from 21 to 38 years, belonging to American Society of Anesthesiologist (ASA) I and II physical status with body mass index (BMI) 25–35 kg/m2 scheduled to elective cesarean section under general anesthesia. Parturients with altered mental status, known history of allergy to pregabalin, uncontrolled diabetes mellitus, bleeding and coagulation disorders, hepatic, renal, cardiovascular, respiratory disease, neuropsychiatric disorders, receiving anticonvulsants or antidepressants, pregnancy-induced hypertension, intrauterine growth restriction, or fetal compromise were excluded from this study.
The parturients and the outcome assessors (anesthesiologists collecting the data) were blinded to study drugs.
3. General anesthesia
All parturients were hospitalized and visited a day before the surgery, full history with physical examination and routine investigations were done; the nature and complications of the study were explained in details to all parturients, and informed written consent was obtained from every woman.
All parturients were kept nil orally 8 h before the operation except for clear fluid. Preoperative anxiety was assessed using a State-Trait Anxiety Inventory (STAI) questionnaire to all parturients (Supplemental Table 1) [Citation10] consists of the State Anxiety Scale, which assesses the current state of anxiety and the Trait Anxiety Scale which measures feelings in general. The parturient was asked to sign one of the following options (never, sometimes, frequently or almost always). The STAI includes 40 items, positive scores were set for items 3, 4, 6, 7, 9, 12, 13, 14, 17, and 18, while negative scores were set for items 1, 2, 5, 8, 10, 11, 15, 16, 19, and 20. Scores between 1 (or −1) and 4 (or−4) were set for every item in accordance with the negative and positive scores and 50 were counted to the gained total scores. The lowest and highest scores were 20 and 80, respectively.
Interpretation:
STAI from 20–37 = low anxiety
STAI from 38–44 = moderate anxiety
STAI from 45–80 = high anxiety
Sixty minutes before induction of anesthesia, 74 parturients were randomly allocated into two groups (group A and Group B). Using computer-generated randomization table, each group consists of 37 parturients.
3.1. Group A (pregabalin group) (n = 37)
Received oral pregabalin 150 mg capsule.
3.2. Group B (control group) (n = 37)
Received oral placebo in the form of oral multivitamin capsule.
In the preparatory room, i.v. line was inserted and 8 ml/kg crystalloids fluid was started. Basal heart rate and mean arterial blood pressure, serum glucose and cortisol level were recorded. Then, parturient was transferred to the operating room where a full standard monitor was applied: five leads electrocardiography (ECG), non-invasive blood pressure (NIBP), and pulse oximeter (SPO2).
After completing 60 min and before induction of anesthesia, anxiety was assessed using State-Trait Anxiety Inventory (STAI) questionnaire [Citation10] and maternal sedation score was assessed using AVPU scale (A = alert, V = respond to verbal, P = respond to pain, U = unresponsive.) [Citation11].
Start pre-oxygenation by 100% oxygen for 3–5 min followed by induction of anesthesia by rapid-sequence induction with 2 mg/kg i.v. propofol and 1.5 mg/kg succinylcholine. If there was more than one attempt or took more than 40 sfor endotracheal intubation, the parturient was excluded from the study. Muscle relaxation was maintained with 0.5 mg/kg atracurium within few minutes after succinylcholine administration, and mechanical ventilation was started to maintain the end-tidal CO2 30–35 mm Hg.
Heart rate and mean arterial blood pressure were recorded at 0 (at intubation) 1, 3, 5, and 10 min after intubation. Serum glucose and cortisol level were measured at 10 min after intubation. Maintenance of anesthesia using 0.75% isoflurane in gas mixture 40: 60 (oxygen: air) by a circle circuit with 6 L/min fresh gas flow till the delivery time.
Any complications detected intraoperative such as hypotension (mean arterial blood pressure < 65 mmHg), bradycardia (heart rate < 50 beat/min), hypertension (mean arterial blood presure > 20% of basal), and tachycardia (heart rate> 20% of basal) were managed.
Immediately after delivery, 1 µg/kg i.v. fentanyl and i.v. infusion of 20 IU oxytocin in 500 ml normal saline solution were given. Also, the neonatal clinical outcome was assessed using APGAR score (Supplemental Table 2) [Citation12] at 1 and 5 min after delivery. After ending of surgery, the inhalational anesthetic was turned off and reversal of the muscle relaxant using 0.05 mg/kg neostigmine with 0.02 mg/kg atropine. The parturient was extubated and transferred to PACU (Post Anesthesia Care Unit).
3.3. Maternal measurements
Anxiety by State-Trait Anxiety Inventory (STAI) questionnaire before drug administration and 60 min after giving drug (pre-induction).
Heart rate and mean arterial blood pressure were recorded at preoperative baseline, 0 (at intubation) 1, 3, 5, and 10 min after intubation.
Serum glucose and cortisol level were recorded preoperative and at 10 min after intubation.
Sedation level by AVPU scale 60 min after giving drug (pre-induction).
3.4. Neonatal outcome measures
APGAR score at 1 and 5 min after delivery
3.5. Sample size
The sample size was calculated using OPEN EPI program assuming that the mean visual analog scale anxiety score was 49.3 ± 14.1 among oral pregabalin group and was 58.6 ± 14.4 among Placebo group [Citation13]. So, at power of study 80% confidence interval 95%, the sample size was calculated to be 74 cases (37 in each group).
3.6. Statistical analysis
All data were collected, tabulated, and statistically analyzed using IBM Corp. Released 2015. IBM SPSS Statistics for Windows, v.23.0. Armonk, NY: IBM Corp. Quantitative data were expressed, and qualitative data were expressed as absolute frequencies (number) and relative frequencies (percentage). T-test was used to compare between two independent variables of normally distributed. Percentage of categorical variables were compared using chi-squared test. Marginal Homogeneity Test was used to compare two dependent ordinal variables. All tests were two-sided. P-value < 0.05 was considered statistically significant (S), p-value < 0.001 was considered highly statistically significant (HS), and p-value ≥ 0.05 was considered statistically insignificant (NS).
4. Results
Eighty parturients were prepared for the study. However, two parturients had twins; one parturient had two attempts of intubation and three parturients refused to participate. So, 74 parturients were randomly allocated into two groups (37 parturients for each) (). All 74 parturients in the two groups of the study were comparable regarding parturients characteristics ().
Table 1. Parturients characteristics
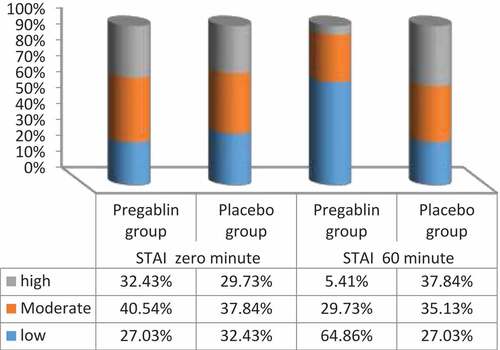
At 0 min (basal), the number of parturients had low, moderate, and high anxiety using STAI was comparable between both groups. While at 60 min after drug intake preoperatively, group A (pregabalin group) showed statistically significant lower number of parturients had moderate and high anxiety [11(29.73%) and 2(5.41%)], respectively, and higher number of parturients had low anxiety [24(64.86%)] using STAI compared to [13(35.13%) and 14(37.84%)] for moderate and high anxiety, respectively, and [10(27.03%)] for low anxiety in group B (placebo group) (p = 0.001) () ().
Table 2. Preoperative maternal anxiety using (STAI) between two groups at measured time points
In group A, The number of parturients at 60 minafter drug intake preoperatively had moderate and high anxiety was statistically significant decreased compared to basal numbers with significant increased number of parturients had low anxiety (p < 0.001). However in group B, there was no statistically significant difference between two measured times (p = 0.297) () ().
Mean (heart rates and arterial blood pressures) raised from baseline values in both groups during laryngoscopy and intubation (at 0 min) and both groups were comparable at all measured time points (p > 0.05) ().
Table 3. Mean heart rates and mean arterial blood pressures at measured time points between two groups
At 10-min post-intubation, the mean serum glucose levels (110.68 ± 10.26 and112.19 ± 9.97) mg/dl raised from basal values (93.65 ± 7.71 and 92.89 ± 6.802) mg/dl in group A and B, respectively, and both groups were comparable (p > 0.05) ().
Table 4. Mean serum glucose, serum cortisol and APGR score at measured time points for both groups
Also, rising in the mean serum cortisol levels at 10-min post-intubation (23.06 ± 1.847 ug/dl) in group A and (24.046 ± 2.46 ug/dl) in group B from basal values (19.78 ± 1.54 and 20.103 ± 1.67) ug/dl in group A and B, respectively, and both groups were comparable (p > 0.05) ().
All the mean APGAR scores were within normal and there were no statistically significant changes in the mean APGAR scores at one and five minutes after delivery between the two groups (p > 0.05) ().
All parturients were alert by AVPU score and no side-effects in both groups.
5. Discussion
Many literatures demonstrated that hospital anxiety and stress symptoms are common in parturients starting from only tension till reaching a panic attacks resulting in negative impacts on maternal and neonatal outcomes [Citation14–16].
The current study demonstrated that pre-emptive single oral 150 mg pregabalin is effective in decreasing maternal anxiety with good neonatal clinical outcome but has no effects on maternal stress response to laryngoscopic intubation during cesarean section.
In a recent meta-analysis done by Torres-González et al. [Citation17], it was reported that administration of 150 mg as a single oral dose preoperatively produced effective anxiety control and this was coincided with the results of the present study. Also, Singh et al. [Citation13] concluded that 150 mg pregabalin, 60 min before induction of anesthesia was effective in preventing preoperative anxiety in patients undergoing laparoscopic cholecystectomy.
In spite of the name “pregabalin” denotes binding to receptors or transporters of γ- aminobutyric acid (GABA) type A or B, it has no clinical relation to them. Pregabalin acts through binding to α2δ type one protein of voltage-gated Ca++ channel leading to decrease in the intracellular Ca++ which is needed for membrane fusion and neurotransmitter release at the synaptic cleft, hence inhibiting the release of mono-amine oxidase (MAO) and glutamate neurotransmitter involved in anxiety mechanism [Citation18]. This stands in contrast to the action of benzodiazepines as MAO neurotransmitter of which acts by exaggerating the inhibitory effect of GABA receptors [Citation19]. The above facts explain that 150 mg single oral dose of pregabalin was effective in attenuating maternal anxiety without any sedation effect on mothers in the current study.
In contrast to previous studies Singh et al. [Citation13] and Doddaiah et al. [Citation20], the present study results revealed no effects of single oral dose of 150 mg pregabalin on maternal mean heart rates, mean arterial blood pressures, serum glucose, and cortisol levels during intubation and these finding can be explained first, pregabalin attenuate stress response in a dose-dependent manner in accordance with Meena et al. [Citation21] who studied the effects of two different oral doses of pregabalin 150 mg and 300 mg one hour before surgery compared to oral placebo for attenuating cardiovascular response to laryngoscopy and intubation in controlled hypertensive patients and found that 150 mg oral pregabalin and oral placebo were associated with significant rising in the heart rate and mean arterial blood pressure compared to 300 mg after instrumentation of airway. Second, the mechanism by which pregabalin attenuates the stress response of intubation is still unknown and all explanations are just diligence as it may act on inhibiting Ca++ outflow from muscles with squally inhibition of relaxation of smooth muscles [Citation22].
El Kenany et al. [Citation23] reported that oral 150 mg pregabalin was safer on newborn than 300 mg as all APGAR scores at one and five minutes were between 7 and 9. Also, they did not observe any side effects at dose 150 mg during studying the effect of preoperative pregabalin on post-cesarean delivery analgesia and this was coincided with the current study results.
6. Limitations
First, lack of studies that investigate the effects of pregabalin on attenuating maternal anxiety and stress response to intubation during cesarean delivery. Second, there is still a need to justify the dose of pregabalin taking in mind the maternal benefits and good neonatal outcomes. So, we recommended administration of repeated oral small doses of pregabalin before the cesarean delivery as it acts through a dose-dependent manner.
7. Conclusion
Pre-emptive oral 150 mg pregabalin was effective in decreasing maternal anxiety with good newborn clinical outcomes, but has no effect on stress response of laryngoscopic intubation during cesarean.
Supplemental Material
Download ()Disclosure statement
No potential conflict of interest was reported by the author(s).
Supplementary material
Supplemental data for this article can be accessed here.
References
- Reynolds F. General anesthesia is unacceptable for elective cesarean section. Int J Obstet Anesth. 2010;19:212–217.
- Brown JPR. Recent developments in anaesthesia for caesarean section in the UK. Update Anaesth. 2008;23:3–7.
- Ding XX, Wu YL, Xu SJ, et al. Maternal anxiety during pregnancy and adverse birth outcomes: a systematic review and meta-analysis of prospective cohort studies. J Affect Disord. 2014;159:103–110.
- Kutlesic MS, Kutlesic RM, Mostic-Ilic T. Attenuation of cardiovascular stress response to endotracheal intubation by the use of remifentanil in patients undergoing Cesarean delivery. J Anesth. 2016;30:274–283.
- Dünges B, Heid F, Dauster M, et al. Revisited: haemodynamic instability and endocrine response during endotracheal tube-placement. A prospective, randomized trial using topical lidocaine and a lightwand. Open Anesthesiol J. 2008;2:30–39.
- Gajraj NM. Pregabalin: its pharmacology and use in pain management. Anesth Analg. 2007;105(6):1805–1815.
- Chizh BA, Gohring M, Troster A, et al. Effects of oral pregabalin and aprepitant on pain and central sensitization in the electrical hyperalgesia model in human volunteers. Br J Anaesth. 2007;98:246–254.
- El –guoshy MM, Stohy EMMA, Sale HHK, et al. Clinical Comparative study of the effect of preoperative pregabalin on reduction of the incidence of headache after spinal anesthesia in cesarean section. Egypt J Hosp Med. 2018;73:6507–6514.
- Lavand’homme PM, Roelants F. Evaluation of pregabalin as an adjuvant to patient-controlled epidural analgesia during late termination of pregnancy. Anesthesiology. 2010;113:1186–1191.
- Spielberger CD. Manual for the State-Trait Anxiety Inventory (STAI). Palo Alto, CA: Consulting Psychologists Press; 1983.
- Zadravecz FJ, Tien L, Robertson-Dick BJ, et al. comparison of mental- status scales for predicting mortality on the general ward. J Hosp Med. 2015; (10):658–663. DOI:10.1002/jhm.2415
- Apgar V. A proposal for a new method of evaluation of the newborn infant. Curr Res Anesth Analg. 1953;32:260–267.
- Singh D, Yadav JS, Jamuda BK, et al. Oral pregabalin as premedication on anxiolysis and stress response to laryngoscopy and endotracheal intubation in patients undergoing laparoscopic cholecystectomy: a Randomized Double-Blind Study. Anesth Essays Res. 2019;13(1):97–104.
- Ferreira CR, Orsini MC, Vieira CR, et al. Prevalence of anxiety symptoms and depression in the third gestational trimester. Arch Womens Ment Health. 2014;17:221–228.
- Marcolino JAM, Mathias LAST, Piccinini F, et al. Escala hospitalar de ansiedade e depressão: estudo da validade de critério e da confiabilidade com pacientes no pré-operatório. Rev Bras Anestesiol. 2007;57:52–62.
- Zigmond AS. Snaith RP: the hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370.
- Torres-González MI, Manzano-Moreno FJ, Vallecillo-Capilla MF, et al. Preoperative oral pregabalin for anxiety control: a systemic review. Clin Oral Invest. 2020;24:2219–2228.
- Li Z, Taylor CP, Weber M, et al. Pregabalin is a potent and selective ligand for α(2)δ-1 and α(2)δ-2 calcium channel subunits. Eur J Pharmacol. 2011;667(1–3):80–90.
- Kent JM, Mathew SJ, Gorman JM. Molecular targets in the treatment of anxiety. Biol Psychiatry. 2002;52:1008–1030.
- Doddaiah DB, Singh NR, Fatima N, et al. A comparative study of oral pregabalin and oral gabapentin in the attenuation of hemodynamic response to laryngoscopy and intubation. J Med Soc. 2017;31:14–18.
- Meena R, Meena K, Prakash S. Study of attenuation of cardiovascular response during laryngoscopy and intubation using two different doses of pregabalin as premedication in controlled hypertensive patients-A RCT. J Anesth Clin Res. 2016;7:607.
- Memis D, Turan A, Karamanlioglu B, et al. Gapapentin reduce cardiovascular response to laryngoscopy and tracheal intubation. Eur J Anaesthesiol. 2006;23:686–690.
- El Kanany S, El Tahan MR. Effects of preoperative pregabalin on post-caesarean delivery analgesia: a dose- response study. Int J Obstet Anesth. 2016;26:24–31.