ABSTRACT
Background: Deliberate hypotensive anesthesia (DHA) is performed to achieve a bloodless operative field, allowing better visualization and decreasing the intraoperative blood loss amount. The present trial evaluated the efficacy of intravenous infusion (IVI) of remifentanil versus labetalol in inducing DHA in children undergoing cochlear implantation surgery.
Methods: Fifty children aged from 2 to 4 years undergoing cochlear implantation surgery under general anesthesia at Al Manaa General Hospital were included in this double-blind, randomized study. Patients were randomly assigned into two equal groups. Group R: received 0.0125–0.05 µg/kg/h remifentanil IVI after anesthesia induction. Group L: received 0.1–0.25 mg/kg/h labetalol IVI after anesthesia induction. Assessment of the quality of operative field and surgeon satisfaction were recorded. Heart rate (HR) and mean arterial blood pressure (MABP) were recorded at baseline, after intubation, then 5 minutes after the start of infusion of study drugs then every 15 minutes until the end of procedure, and for 30 minutes after recovery).
Results: Quality of surgical field and surgeon satisfaction were significantly better in group R compared to group L. Good visual field was significantly better in group R compared to group L (96% vs. 72%, P = 0.049). MABP was insignificantly different between both groups at all times of measurement. HR was significantly decreased in group R compared to group L intraoperatively from 15 min till the end.
Conclusion: Both remifentanil and labetalol were effective for DHA. However, remifentanil was superior to labetalol by allowing better surgical field quality and surgeon satisfaction with significant intraoperative HR reduction.
1. Introduction
In cochlear implantation as microsurgery, a bloodless field is needed as minimal bleeding will obscure the view in front of the surgeon [Citation1,Citation2]. Deliberate hypotensive anesthesia (DHA) is one of the most common techniques used for this purpose [Citation3].
DHA in children has been begun with Dr. Shiela Anderson in July 1955 by using a ganglion blocker; arfonad [Citation4].
Indicators of DHA in pediatrics aged 1–6 years are decreasing mean arterial blood pressure (MABP) less than baseline values by at least 20% and heart rate (HR) to 70–80 beats per minute. The characteristics of ideal hypotensive drugs include easy administration, rapid onset, rapid offset with discontinuing the drug, a rapid elimination, no toxic metabolites, minimal effect on the vital organs with dose-dependent action [Citation5].
To provide DHA in pediatrics, many drugs are used such as direct acting vasodilators, but they have many side effects such as reflex tachycardia [Citation6].
Remifentanil is a μ-opioid receptor agonist with an ultra-short action. It has been used in DHA safely in pediatrics as it can induce DHA effectively to achieve a dry surgical field without other hypotensive drugs [Citation7]. Remifentanil leads to both hypotension and bradycardia [Citation8].
Labetalol has been used in DHA due to its effect on both α and β receptors. Blocking α receptors of blood vessels results in vasodilatation, and blocking β receptors prevents reflex increase in HR and cardiac output [Citation9].
There is a lack of literature about comparing remifentanil and labetalol in DHA in pediatrics. Therefore, the present trial was designed to determine the efficacy of intravenous infusion (IVI) of remifentanil compared to labetalol in DHA in cochlear implantation in pediatrics.
2. Materials and methods
Fifty children aged 2–4 years, both genders, American Society of Anesthesiologists (ASA) physical status I and II undergoing cochlear implantation surgery were enrolled in this double-blind prospective randomized trial. The study was done from February 2017 to August 2017 in the otorhinolaryngology department, Al Manaa General Hospital, Kingdom of Saudi Arabia, following the ethical committee approval and informed signed consent from guardians of each child.
Exclusion criteria were known allergy to any of the drugs used in the trial (from guardians of the children and medical records), congenital heart disease, and patients with disorders of coagulation, renal and hepatic disorders.
2.1. Randomization and blinding
The randomization was performed using computer‐generated randomization numbers put in sealed numbered envelopes indicating the group of each patient. Study drugs were prepared by an independent anesthesiologist. All anesthesiologists, surgeons, and nurses in the operating room were blinded to randomization and preparations. The same surgeon performed all operations to ensure consistency in estimating the surgical field.
Children were randomly assigned into two equal groups (25 children in each) according to drugs used to induce DHA:
Group R (Remifentanil group): patients received remifentanil continuous IVI 0.0125–0.05 µg/kg/hour after anesthesia induction [Citation10].
Group L (Labetalol group): patients received labetalol by continuous IVI 0.1–0.25 mg/kg/hour after anesthesia induction [Citation11].
2.2. Preoperative
Preoperative preparation included history taking, physical examination, and laboratory investigations (complete blood count, prothrombin time, liver function tests, and kidney function tests).
2.3. Intraoperative
During anesthesia, the standard monitoring (temperature probe, pulse oximetry, electrocardiogram, non-invasive blood pressure, and capnography) was performed. Invasive blood pressure monitoring was done after induction of general anesthesia (GA).
Sevoflurane (6–8%) was used for induction of GA. Then, two IV lines were inserted after deep anesthesia; one line was used for IVI of remifentanil and labetalol, and the other one for IV fluid maintenance and other drugs needed. Then, fentanyl 1 μg/kg was given. Cisatracurium 0.15 mg/Kg was used to facilitate orotracheal tube insertion. Sevoflurane 2–3% in 50% O2 was used for maintaining GA. Cisatracurium 0.03 mg/kg every 20–30 minutes was done to maintain muscle relaxation. End-tidal CO2 between 32 and 35 mmHg was maintained by adjusting the tidal volume and respiratory rate of the mechanical ventilator. Lactated ringer solution 5 ml/kg/h IVI was administered.
In both groups, the rate of IVI was adjusted to make MABP 20% below the baseline of the patients.
Fentanyl 0.5 µg/kg IV was administered if inadequate GA manifestations appeared (increase in HR or MABP more than 15% of the baseline values (after excluding other causes). Significant hypotension was defined as a reduction of MABP by 30% or more below the baseline value and was managed by ephedrine 0.2 mg/kg IV. Significant bradycardia was defined as HR less than 60 beats/min and was managed by atropine 0.01 mg/kg IV.
Before the expected surgery end by 10 minutes, the IVI of remifentanil or labetalol was ceased.
For prevention of postoperative nausea and vomiting (PONV), dexamethasone 0.15 mg/kg IV was given before the surgery end. If PONV occurred, ondansetron 0.1 mg/kg IV was administered.
The inhalation anesthesia was discontinued after the surgery end. Atropine 0.02 mg/kg and neostigmine 0.05 mg/kg IV were used in the reversal of muscle relaxation. Spontaneous breathing was allowed then removal of the endotracheal tube was done in a deep anesthesia plane in the recovery position. Transferring to the postanesthesia care unit (PACU) was done.
2.4. Measurements
Assessment of the quality of operative field was performed by the operating surgeon by using a scale used by Fromme et al. [Citation12] (0-no bleeding, 1-slight bleeding, no suctioning of blood required, 2-slight bleeding occasional suctioning required, surgical field not threatened, 3-slight bleeding – frequent suctioning required. Bleeding threatens surgical field as few seconds after suction was removed, 4-moderate bleeding – frequent suctioning required, bleeding threatens surgical field directly after suction was removed, 5-severe bleeding – constant suctioning required, bleeding appeared faster than removed by suction. The surgical field severely threatened, and surgery not possible). The ideal category scale value was determined to be ≤3.
The surgeon satisfaction was assessed using a 5 – point scale [Citation13]; 1 – very satisfied, 2-somewhat satisfied, 3 – neither satisfied nor dissatisfied, 4 – somewhat dissatisfied, and 5 – very dissatisfied.
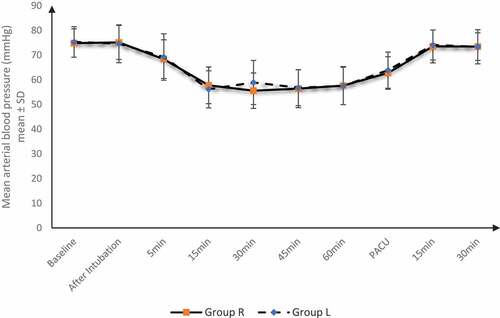
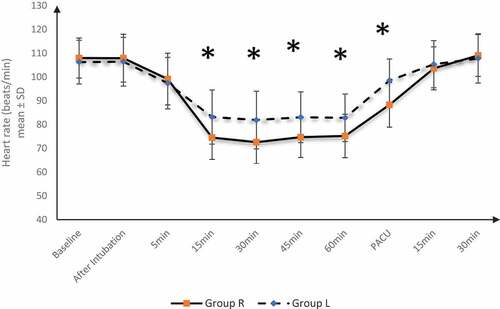
Hemodynamics (HR and MABP) were recorded at baseline, after intubation, then 5 minutes after the start of infusion of study drugs then every 15 minutes until the end of the procedure, and for 30 minutes after recovery).
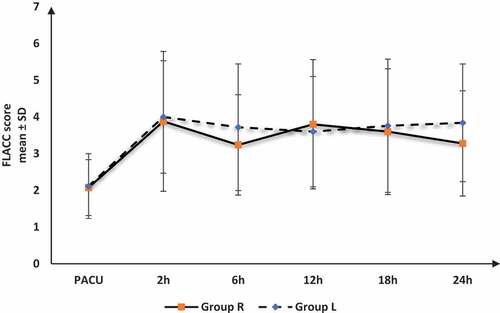
Intraoperative consumption of fentanyl, recovery time (from discontinuing anesthesia with muscle relaxant reversal till spontaneous eye opening), and postoperative pain by FLACC score (at PACU, 2, 6, 12, 18, and 24 h) were recorded. Adverse events were recorded and managed as mentioned above.
The primary outcome was the quality of surgical field. The secondary outcomes were surgeon satisfaction and a decrease in HR and MABP without adverse events.
2.5. Sample size
G.power 3.1.9.2 was used for sample size calculation. The expected good visual field (scale ≤3) was between 50% and 90%. With confidence level 95%, power 80%, and adding 5 cases (to overcome dropout), the recruited cases were 25 in each group.
2.6. Statistical analysis
Analysis of data was done using SPSS v20 (IBM©, Chicago, IL, USA). The quantitative variables were presented as mean and standard deviation (SD) and were analyzed by unpaired student t-test. Repeated measures ANOVA was used to compare multiple variables within the same group. The qualitative variables were presented as frequency and percentage and were compared by Chi-square (X2) or Fisher’s Exact test when appropriate. The cut-off of statistical significance of a two-tailed P value is ≤0.05.
3. Results
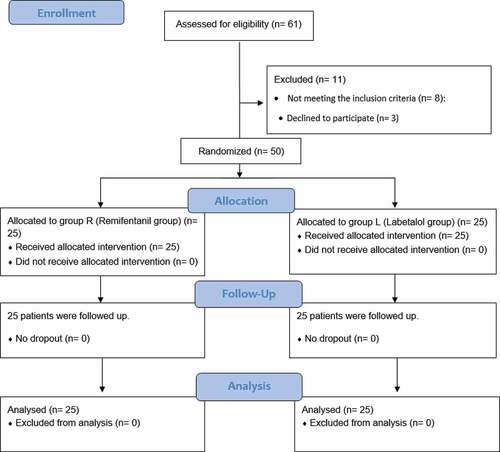
The flowchart of enrolled patients in both groups is shown in . Demographic data, ASA physical status, and duration of surgery were comparable in the two groups ().
Table 1. Demographic data in between the studied groups
Quality of surgical field was significantly better in group R compared to group L. Good visual field was significantly better in group R compared to group L (96% vs 72%, P = 0.049). Consequently, surgeon satisfaction was significantly better in group R compared to group L. ()
Table 2. Quality of surgical field and surgeon satisfaction about both techniques
MABP was insignificantly different between both groups at all times of measurement. MABP was significantly decreased in both groups from 5 min till PACU compared to baseline. The onset of bradycardia was insignificantly earlier in group R (9.64 ± 2.98 min) compared to group L (10.44 ± 3.24 min) with P value = 0.368 ().
HR was significantly lower in group R than group L at 15, 30, 45, and 60 min intraoperative and at PACU. HR was significantly decreased in both groups from 5 min till PACU compared to baseline. The onset of bradycardia was significantly earlier in group R (7.88 ± 1.36 min) compared to group L (12.12 ± 2.09 min) with P value <0.001 ().
Intraoperative consumption of fentanyl was significantly lower in group R (14.56 ± 2.24 µg) compared to group L (17.18 ± 4.65 µg) with P value = 0.014. Recovery time was insignificantly different between both groups (7.12 ± 1.90 min in group R and 6.64 ± 1.85 min in group L with P value = 0.369).
The postoperative FLACC score was insignificantly different between both groups at all times of measurements ().
Adverse events (PONV, tachycardia, significant bradycardia, and significant hypotension) were minimal and insignificantly different between both groups ().
Table 3. Adverse events among the studied groups
4. Discussion
Anesthetic aims in cochlear implantation are to keep hemodynamics stable, offer a dry surgical field, adjust anesthetic technique to enable the facial nerve and stapedius reflex monitoring and testing [Citation14]. DHA leads to decrease blood loss that can help surgical exposure, reduce tissue damage, and enhance postoperative healing. Various medications and techniques were used in the past, but none was completely effective and safe [Citation15].
In the present trial, both remifentanil and labetalol were effective for inducing DHA. However, remifentanil was superior to labetalol by allowing better surgical field quality and surgeon satisfaction and significant intraoperative reduction of HR with earlier onset of bradycardia and lower intraoperative consumption of fentanyl.
Hypotension during the administration of remifentanil may be due to its direct role on regional vascular tone, which has a role in inducing hypotension and/or sympathetic outflow decrease [Citation16]. Also, an advantage of remifentanil is being an ultrashort-acting potent opioid with rapid onset and offset [Citation17]. Therefore, group R had less opioid consumption without affecting the recovery profile.
Labetalol is one of the antihypertensive drugs that blocks α and β receptors, leading to a decrease in HR and MAP (by vasodilation). However, labetalol specifically blocks β receptors 5–10 times other receptors preventing reflex tachycardia that occurs with other antihypertensive vasodilator medications [Citation18].
Sajedi et al. [Citation19] demonstrated that a bolus dose followed by IVI of remifentanil (0.5–1 μg/kg bolus, then 0.25–0.5 μg/kg/min) or labetalol (20 mg bolus, then infusion 0.5–2.0 mg/min) induced DHA effectively during functional endoscopic sinus surgery (FESS) in adults. Bleeding during surgery and intraoperative consumption of fentanyl in remifentanil group were lower than in labetalol group. In addition, surgeons in remifentanil group were significantly more satisfied compared to labetalol group. Incidences of bradycardia and hypotension were insignificantly different between both groups.
In pediatrics undergoing middle ear microsurgery, Shirgoska et al. [Citation10] demonstrated that both remifentanil and remifentanil with sevoflurane-induced DHA effectively.
Also, Zaky and Saleh [Citation7] showed that remifentanil (1 μg/kg bolus, then 0.15 μg/kg/min IVI) efficiently reduced both HR and MABP and improved surgical feasibility during FESS in adults.
In another study, Ghodraty et al. [Citation9] evaluated labetalol induced controlled hypotension compared to nitroglycerin in septorhinoplasty in adults. Labetalol was administered as 0.25 mg/kg bolus, then 2–4 mg/minute IVI. HR and MABP were decreased significantly compared to baseline. Labetalol was not good enough in inducing controlled hypotension. Also, surgeon’s satisfaction score from the surgical field was not high. They attributed this to the delayed onset of labetalol in producing their hypotensive effect.
Consistent with the present study, Degoute et al. [Citation1] found that remifentanil (1 µg/kg bolus then 0.25 = 0.50 µg/kg IVI) decreased the blood flow of middle ear (as evaluated by doppler velocimetry) effectively and provided good surgical condition during tympanoplasty in adults by reducing MABP to the desired level.
A limitation of our study is that this trial included only children with ASA I and II. Another limitation, we did not use an objective method such as doppler to assess the decrease in blood flow. Also, we did not follow up the children for possible complications of DHA.
5. Conclusion
Both remifentanil and labetalol were effective for inducing DHA. However, remifentanil was superior to labetalol by allowing better surgical field quality and surgeon satisfaction with significant intraoperative HR reduction.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Degoute CS, Ray MJ, Manchon M, et al. Remifentanil and controlled hypotension; comparison with nitroprusside or esmolol during tympanoplasty. Canadian journal of anaesthesia = Journal canadien d’anesthesie. 2001 Jan;48(1):20–27.
- Amin SM, Elmawy MGE. Optimizing surgical field during cochlear implant surgery in children: dexmedetomidine versus esmolol. Egypt J Anaesth. 2016 Jul 01;32(3):255–261.
- Aydin GB. Controlled hypotension: remifentanil or esmolol during tympanoplasy. Mediterr J Otol. 2008;4:125–131.
- Anderson SM. Controlled hypotension with arfonad in paediatric surgery. Br Med J. 1955;2(4931):103–104.
- Chhabra A, Saini P, Sharma K, et al. Controlled hypotension for FESS: a randomised double-blinded comparison of magnesium sulphate and dexmedetomidine. Indian J Anaesth. 2020;64(1):24–30.
- Hassan PF, Saleh AH. Dexmedetomidine versus magnesium sulfate in anesthesia for cochlear implantation surgery in pediatric patients. Anesth Essays Res. 2017;11(4):1064–1069.
- Zaky M, Saleh A. Hypotensive anesthesia during functional endoscopic sinus surgery: a comparative study of remifentanil versus magnesium sulfate infusion [Original Article]. Ain-Shams J Anaesthesiol. 2017;10(1):124–130.
- Modir H, Modir A, Rezaei O, et al. Comparing remifentanil, magnesium sulfate, and dexmedetomidine for intraoperative hypotension and bleeding and postoperative recovery in endoscopic sinus surgery and tympanomastoidectomy. Med Gas Res. 2018;8(2):42–47.
- Ghodraty M, Khatibi A, Rokhtabnak F, et al. Comparing labetalol and nitroglycerine on inducing controlled hypotension and intraoperative blood loss in rhinoplasty: a single-blinded clinical trial. Anesth Pain Med. 2017;7(5):e13677.
- Shirgoska B, Netkovski J, Zafirova B. The influence of remifentanil and remifentanil-plus-sevoflurane-controlled hypotension on mean arterial pressure and heart rate in children. Prilozi. 2012;33(1):171–185.
- Salem AE, Hagras AM, Abo-Ragab HM. Labetalol hypotensive anesthetic protocol paves the way to safe open abdominal myomectomy. J Anest Inten Care Med. 2017;3(2):555606.
- Fromme GA, MacKenzie RA, Gould AB Jr., et al. Controlled hypotension for orthognathic surgery. Anesth Analg. 1986 Jun;65(6):683–686.
- Mira JJ, Tomás O, Virtudes-Pérez M, et al. Predictors of patient satisfaction in surgery. Surgery. 2009 May;145(5):536–541.
- Baidya DK, Dehran M. Anaesthesia for cochlear implant surgery. Trends Anaesth Crit Care. 2011 Apr 01;1(2):90–94.
- Barak M, Yoav L, Abu el-Naaj I. Hypotensive anesthesia versus normotensive anesthesia during major maxillofacial surgery: a review of the literature. ScientificWorldJournal. 2015;2015:480728.
- Noseir RK, Ficke DJ, Kundu A, et al. Sympathetic and vascular consequences from remifentanil in humans. Anesth Analg. 2003 Jun;96(6):1645–1650.
- Oriby ME, Elrashidy A. Comparative effects of total intravenous anesthesia with propofol and remifentanil versus inhalational sevoflurane with dexmedetomidine on emergence delirium in children undergoing strabismus surgery. Anesth Pain Med. 2021;11(1):e109048.
- Fahed S, Grum DF, Papadimos TJ. Labetalol infusion for refractory hypertension causing severe hypotension and bradycardia: an issue of patient safety. Patient Saf Surg. 2008 May;27(2):13.
- Sajedi P, Rahimian A, Khalili G. Comparative evaluation between two methods of induced hypotension with infusion of remifentanil and labetalol during sinus endoscopy. J Res Pharm Pract. 2016;5(4):264–271.