ABSTRACT
Background: Severe zoster-associated pain limits patient’s daily activity and may significantly lower the patient’s quality of life. The current study aimed to improve the patient’s quality of life by adding ESPB to the current medical therapy. The primary outcome was to improve pain control in acute stage, while the secondary outcome was to reduce the incidence of PHN.
Settings and Design: This study was a prospective randomized controlled trial.
Methods: This study was carried out on 40 patients between 20 and 60 years old suffering from acute thoracic HZ. Patients were randomly classified into two groups: one group received ESPB, using 0.25% bupivacaine 20 ml and 40 mg methylprednisolone single shot in the thoracic dermatome corresponding to the rash, together with the conventional medical treatment for herpes zoster, and the second group only received medical treatment. Once the pain started to decrease, Pregabalin dose was reduced. Acetaminophen was used as a rescue analgesic. Pain scores,PGIC, and the average doses of Pregabalin and Acetaminophen were calculated at each visit. The time to complete resolution of pain and incidence of PHN were recorded. Follow-up was done for 3 months after the first visit.
Results: Pain intensity was significantly lower in the group receiving the block at the second and fourth weeks after the block was performed. The time to complete resolution of pain was significantly longer in the medical group. Two patients progressed to PHN in the block group (10%) versus six patients in the medical group (30%). The average Pregabalin and Acetaminophen doses in the second 14 days, and the following 56 days was statistically significantly lower in the block group. Patient satisfaction was significantly higher in patients in the block group at the second and fourth weeks after the receiving the block.
Conclusion: ESPB in conjunction with medical treatment can be beneficial in decreasing pain intensity in patients with acute thoracic herpes zoster more rapidly than conventional medical treatment.
1. Introduction
Varicella Zoster Virus (VZV) belongs to the α-herpesvirus family. Its primary infection causes chicken pox, which is transmitted by droplet infection or by direct contact with a skin lesion. The reactivation of this virus, which is dormant in the nerve root ganglia after its primary infection, causes herpes zoster [Citation1,Citation2].
The rash is usually distributed along the course of one or two dermatomes. It is unilateral in distribution, maculopapular at first then vesicular, lasting 7–10 days, after which scabs are formed. The adherent scabs may last up to 3 weeks. After that, the rash is no longer infective [Citation3].
Herpes zoster can be classified as either acute or chronic according to the duration of the persistence of pain (<4 weeks or >4 weeks) [Citation4]. Postherpetic neuralgia (PHN) can be defined as pain persisting from 1 month after the onset of rash, pain persisting after rash resolution, or pain 3–6 months after the acute attack [Citation5].
Pain caused by herpes zoster often limits a patient’s daily activity and may significantly affect the quality of life [Citation6]. It is therefore necessary to effectively treat the herpes-associated pain.
Treatment of herpes zoster aims at decreasing the duration and severity of pain, avoiding secondary infection, and decreasing the incidence of PHN [Citation7]. The treatment consists of pharmacological treatment, such as antivirals, strong analgesics (ranging from paracetamol and NSAIDs up to opioids), anticonvulsants, and antidepressants [Citation8,Citation9].
Recently, interventional treatments have been used to decrease the pain severity in the acute phase of herpes zoster and to help prevent progression to PHN. Many techniques have been used, such as single-shot epidurals, epidural catheter, paravertebral block for single dermatomal distribution, and most recently erector spinae plane block (ESPB) [Citation10–12].
The aim of this study was to assess the effectiveness of ultrasound-guided ESPB in management of herpes zoster pain and incidence of PHN. The primary outcome of this study was to assess the efficacy of pain relief, and the secondary outcomes were to assess the progression to PHN, the average doses of Pregabalin and Acetaminophen consumed, and the patient global impression of change scale.
2. Patients and methods
After approval by the Ethics Committee of the Faculty of Medicine, written informed consent was taken from all the patients. This study was carried out in Alexandria Main University Hospital on 40 patients between the ages of 20 and 60 years old, ASA physical status I and II, admitted to Dermatology and Pain clinics, complaining of thoracic herpes zoster.
Inclusion criteria included patients with moderate pain (VAS ≥4), less than five dermatomes affected, and patients coming less than 3 months of rash eruption.
Patients with ASA status III, IV, and V; patients with coagulation abnormalities, or with known allergy to methylprednisolone or bupivacaine; patients with serum creatinine ≥5 mg/dl; patients coming ≥3 months after rash healing; and those with chronic pain requiring analgesia were excluded from the study.
Patients were randomly classified into two equal groups by closed-envelope technique. Group I received ultrasound-guided ESPB using 0.25% bupivacaine 20 ml and 40 mg methylprednisolone single shot. They were then prescribed 800 mg acyclovir five times a day for 7 days, 150 mg Pregabalin twice daily for 7 days, and Acetaminophen 1000 mg was used as a rescue analgesic when VAS ≥4.
The patient was placed in a sitting position, and a high frequency linear ultrasound transducer was placed in a longitudinal orientation 3 cm lateral to the thoracic spinous process corresponding to the affected dermatome. Three muscles were identified superficial to the hyperechoic transverse process shadow as follows: trapezius, rhomboid major, and erector spinae. An 8 cm 22 gauge block needle was inserted in a cephalad to caudad direction until the tip lies in the plane between the erector spinae muscle and the transverse process. This was seen as visible linear spread of the fluid upon injection.
The dose of Pregabalin was increased or decreased according to pain severity and patient’s ability to tolerate its side effects. The duration of analgesia was considered the analgesia starting from the performance of the block until the first analgesic requirement or reporting a pain score of 4/10. The block was repeated after a 2-week interval if the VAS was found to be >6. Group II received medical treatment without the block. Patients were followed up for a 3-month period, with visits after 2 weeks, 1 month, and 3 months from the initial visit. PGIC was assessed upon each visit [Citation13].
3. Statistical analysis
Data were collected and entered to the computer using SPSS (Statistical Package for Social Science) program for statistical analysis (ver. 21) [Citation14].
Data were entered as numerical or categorical as appropriate.
The Kolmogorov–Smirnov test of normality revealed significance in the distribution of the variables, so the non-parametric statistics was adopted [Citation15].
Data were described using minimum, maximum, median, and interquartile range.
Categorical variables are described using frequency and percentage.
Comparisons were carried out between the two studied independent non-normally distributed subgroups using the Mann–Whitney U-test [Citation16].
Comparisons were carried out among related samples by Friedman’s test “alternative to the one-way ANOVA with repeated measures” [Citation17].
Pairwise comparison when Friedman’s test was significant was carried out using Dunn–Sidak method [Citation18].
Box and whiskers plots were used accordingly.
The alpha level was set to 5% with a significance level of 95%.
When calculating the sample size, a beta error was accepted up to 20% with a power of study of 80%.
4. Results
Fifty-five patients were screened for eligibility to participate in this study. Forty-five patients were enrolled in the study, with 10 patients excluded for not meeting the inclusion criteria and 5 dropouts along the course of treatment. A total of 40 participants continued the trial until the end of the 12 weeks ().
There was no statistically significant difference between the two groups in regard to age, sex, and BMI. There was no significant difference in the VAS between the two groups at the baseline (p = 0.294).
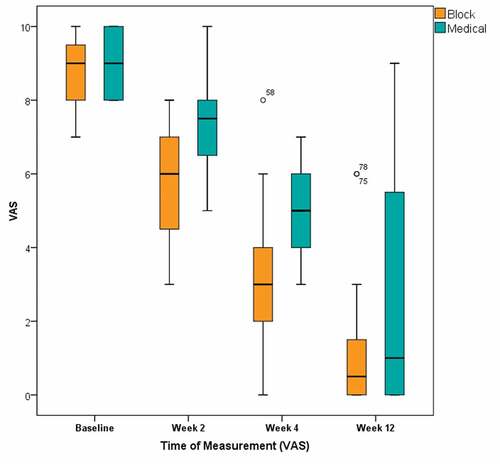
Pain intensity was statistically significantly higher in the medical group at week 2 and week 4 (p = 0.001 and 0.000, respectively). At week 12, there was no statistical significance in VAS scores between the two groups ().
Figure 2. Box and whisker graph of VAS in the studied groups. The thick line in the middle of the box represents the median, the box represents the interquartile range (from 25th to 75th percentiles), and the whiskers represent the minimum and maximum after excluding outliers (black-filled circles)
At week 12, two patients (10%) in the block group progressed to PHN (had a VAS score greater than 3), while in the medical group, six patients (30%) progressed to PHN. There was no statistically significant difference between the two groups ().
Table 1. Progression to PHN
There was no statistically significant difference between the two groups in the average Pregabalin dose in the first 14 days (p = 0.094). The average Pregabalin dose in the second 14 days and the following 56 days was statistically significantly lower in the block group compared with the medical group (p = 0.002, and p = 0.000, respectively) ().
Table 2. Average Pregabalin consumption (per day in mg)
Average Acetaminophen dose was statistically significantly lower in the block group compared with the medical group, in the first 14 days (p = 0.000), the second 14 days (p = 0.000), and the following 56 days (p = 0.000) ().
Table 3. Average Acetaminophen consumption (per day in grams)
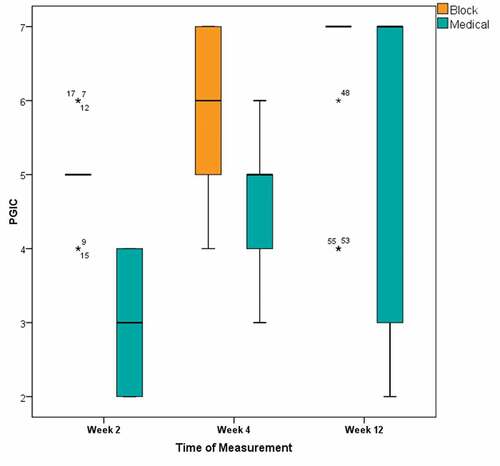
The block group were statistically significantly more satisfied according to the PGIC score with the treatment than the medical group in week 2 and week 4 (p = 0.000 and 0.000, respectively). There was no statistically significant difference between the two groups in week 12 (p = 0.254) ().
Figure 3. Box and whisker graph of PGIC in the studied groups. The thick line in the middle of the box represents the median, the box represents the interquartile range (from 25th to 75th percentiles), and the whiskers represent the minimum and maximum after excluding outliers (black-filled circles) extremes (asterisks) (numbers indicate the serial number of the patient in the original master table).
5. Discussion
The results of the current study reported a greater decrease in pain intensity in patients who received ultrasound-guided ESPB than in patients who received medical treatment alone, with more patient satisfaction and less drug intake, earlier in the course of treatment.
The administration of ESPB in the acute phase of the disease resulted in lower pain scores 2 weeks after the block administration and 1 month after the onset of the disease. This is consistent with the findings of Aydin et al. [Citation19] and Balban et al. [Citation20] who found a decrease in pain scores after administration of ESPB.
One advantage of this technique is that it provided analgesia that lasted 24–48 hours after the block and decreased the pain intensity after that. Fourteen patients (70%) required a second block 2 weeks after the first block was administered.
Another advantage of ESPB is that it is a relatively safe technique with a lower risk of complications such as nerve damage or pleural puncture.
In the current study, 3 months after the initial visit, only two patients (10%) in the block group versus six patients (30%) in the medical group progressed to PHN (VAS > 3). This, however, was not statistically significant.
Many previous studies were done on nerve blocks to decrease the progression of PHN. Similar to our study, Lipton et al. [Citation21] reported that there was no statistically significant difference between patients who received single stellate ganglion block and those who received IV acyclovir and prednisolone for 8 days along with the standard medical treatment.
Opstelten et al. [Citation22] reported that there was no statistically significant difference in PHN incidence between the patients who received single-shot epidural and those who were given standard medical treatment.
Makharita et al. [11] also found that patients who received continuous paravertebral block had a lower incidence of PHN than patients who received a single-shot paravertebral block.
In another study, Makharita et al. [Citation23] reported a decrease in PHN incidence in patients who received stellate ganglion block twice, 2 weeks apart, after 6 months from injection, but there was no statistically significant difference at 3 months.
The decrease in incidence of PHN with repeated blocks may be attributed to the early reduction in pain and inflammation, with the blocking of continuous noxious stimulation, decreasing peripheral and central sensitization and hyperexcitability. Also, the period of follow-up of the patients may have made a difference in the results given, as various papers reported the improvement after 6 months from the intervention, while this study was only conducted for 3 months from the initial visit.
There was a significant decrease in the average consumption of Pregabalin and Acetaminophen in the patients who received erector spinae block compared to those with conventional medical treatment. In concordance with our study, Makharita et al. [11] found that patients who received paravertebral injections for acute herpes zoster had less consumption in analgesics than prior to receiving the block.
Cui et al. [Citation24] also found a significant decrease in analgesic consumption per week compared with the values of the first week.
6. Conclusion
Ultrasound-guided ESPB using local anaesthetic and steroids combined with conventional medical treatment can be a useful technique for early control of pain in the acute phase of herpes zoster. However, further studies can be conducted to assess its efficacy in preventing PHN with multiple blocks.
7. Limitations
There are several limitations of this study, starting from the small sample size, the short duration of follow-up period, difficulty in follow-up with the patients, and frequent dropouts.
Abbreviations
VZV: Varicella Zoster Virus; ESPB: Erector Spinae Plane Block; VAS: Visual Analogue Scale; PHN: Postherpetic Neuralgia; PGIC: Patient Global Impression of Change
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Gnann JW Jr., Whitley RJ. Clinical practice. Herpes zoster. N Engl J Med. 2002;347(5):340–346.
- Sawyer MH, Chamberlin CJ, Wu YN, et al. Detection of varicella-zoster virus DNA in air samples from hospital rooms. J Infect Dis. 1994;169(1):91–94.
- Mueller NH, Gilden DH, Cohrs RJ, et al. Varicella zoster virus infection: clinical features, molecular pathogenesis of disease, and latency. Neurol Clin. 2008;26(3):675–697.
- Seo YG, Kim SH, Choi SS, et al. Effectiveness of continuous epidural analgesia on acute herpes zoster and postherpetic neuralgia: a retrospective study. Medicine (Baltimore). 2018;97(5):e9837.
- Johnson RW. Consequences and management of pain in herpes zoster. J Infect Dis. 2002;186(Suppl 1):S83–S90.
- Gater A, Abetz-Webb L, Carroll S, et al. Burden of herpes zoster in the UK: findings from the zoster quality of life (ZQOL) study. BMC Infect Dis. 2014;14(1):402.
- van Wijck AJ, Wallace M, Mekhail N, et al. Evidence-based interventional pain medicine according to clinical diagnoses. 17. Herpes zoster and post-herpetic neuralgia. Pain Pract. 2011;11(1):88–97.
- Wood M. Understanding pain in herpes zoster: an essential for optimizing treatment. J Infect Dis. 2002;186(Suppl 1):S78–S82.
- Schmader KE, Dworkin RH. Natural history and treatment of herpes zoster. J Pain. 2008;9(1 Suppl 1):S3–S9.
- Kumar V, Krone K, Mathieu A. Neuraxial and sympathetic blocks in herpes zoster and postherpetic neuralgia: an appraisal of current evidence. Reg Anesth Pain Med. 2004;29(5):454–461.
- Makharita MY, Amr YM, El-Bayoumy Y. Single paravertebral injection for acute thoracic herpes zoster: a randomized controlled trial. Pain Pract. 2015;15(3):229–235.
- Ji G, Niu J, Shi Y, et al. The effectiveness of repetitive paravertebral injections with local anesthetics and steroids for the prevention of postherpetic neuralgia in patients with acute herpes zoster. Anesth Analg. 2009;109(5):1651–1655.
- Ferguson L, Scheman J. Patient global impression of change scores within the context of a chronic pain rehabilitation program. J Pain. 2009;10(4):S73.
- IBM Corp. IBM SPSS statistics for Windows, version 21.0. Armonk, NY: IBM Corp.; 2012.
- Field A. Discovering statistics using IBM SPSS statistics. 4th ed. London, California, New Delhi: SAGE Publications Ltd; 2013.
- Mann HB, Whitney DR. On a test of whether one of two random variables is stochastically larger than the other. Ann Mathem Statist. 1947;18(1):50–60.
- Friedman M. The use of ranks to avoid the assumption of normality implicit in the analysis of variance. J Am Statist Assoc. 1937;32(200):675–701.
- Dunn OJ. Multiple comparisons using rank sums. Technometrics. 1964;6(3):241–252.
- Aydin T, Balaban O, Ahiskalioglu A, et al. Ultrasound-guided erector spinae plane block for the management of herpes zoster pain: observational study. Cureus. 2019;11(10):e5891.
- Balaban O, Aydin T. Ultrasound guided bi-level erector spinae plane block for pain management in Herpes Zoster. J Clin Anesth. 2019;52:31–32.
- Harding SP, Lipton JR, Wells JC. Natural history of herpes zoster ophthalmicus: predictors of postherpetic neuralgia and ocular involvement. Br J Ophthalmol. 1987;71(5):353–358.
- Opstelten W, van Wijck AJ, Moons KG, et al. Treatment of patients with herpes zoster by epidural injection of steroids and local anaesthetics: less pain after 1 month, but no effect on long-term postherpetic neuralgia—a randomised trial. Ned Tijdschr Geneeskd. 2006;150(48):2649–2655.
- Makharita MY, Amr YM, El-Bayoumy Y. Effect of early stellate ganglion blockade for facial pain from acute herpes zoster and incidence of postherpetic neuralgia. Pain Physician. 2012;15(6):467–474.
- Cui JZ, Zhang JW, Yan F, et al. Effect of single intra-cutaneous injection for acute thoracic herpes zoster and incidence of postherpetic neuralgia. Pain Manag Nurs. 2018;19(2):186–194.