ABSTRACT
Background
To compare the analgesic effects of thoracic paravertebral block versus lidocaine infusion for management of post-thoracotomy pain.
Methods
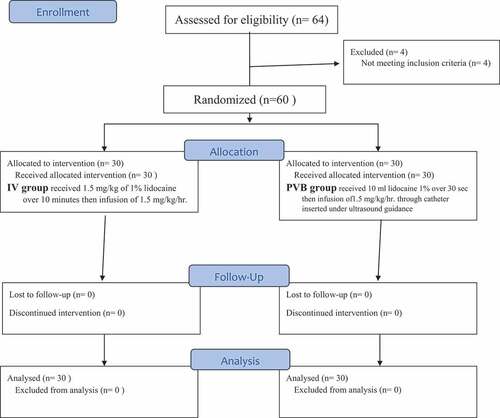
60 patients who were scheduled for thoracotomy were randomly divided into two equal groups: IV group received 1.5 mg/kg of 1% lidocaine over 10 min then infusion of 1.5 mg/kg/h, and thoracic paravertebral group (PVB) received 10 ml lidocaine 1% over 30 s then infusion of 1.5 mg/kg/h through catheter was inserted under ultrasound guidance. Hemodynamic and respiratory variables, frequency and duration of postoperative mechanical ventilation, duration of ICU stay, time till start of respiratory exercise and till chest tube removal, analgesia was assessed using 100-point visual analogue scale and defined as VAS <30 mm at rest, and in case of inadequate analgesia, IV morphine 2 mg bolus was given. Frequencies of complications and postoperative hospital stay were also recorded.
Results
17 patients of both groups were maintained on MV for mean duration of 1.5 ± 0.5 days. PVB group was successfully weaned from MV and extubated after significantly shorter duration. Mean duration of ICU stay, time till start of respiratory exercise, and till removal of chest tube were significantly shorter in PVB group. All patients requested analgesia, but the frequency of consumption and mean number of requests were significantly higher in IV group. VAS scores determined at 1, 2, 12, 36 and cumulative 48 hours were significantly lower in PVB group compared to IV group.
Conclusion
Ultrasound guidance allowed safe paravertebral space catheterization. PVB using continuous lidocaine infusion provided adequate analgesia for post-thoracotomy pain with significant reduction of rescue analgesia, shorter time till respiratory exercises start, minimal complications and shorter hospital stay.
1. Background
Acute post-thoracotomy pain (PTP) is a well-known potential problem. PTP is multi-factorial; the type of thoracotomy, muscle retraction, costal fractures and pleural irritation are the most responsible mechanisms. Intercostal incision by its virtue is associated with pain during respiration leading to pulmonary complications, delayed mobilization in the initial postoperative (PO) period and ineffective respiratory rehabilitation. Additionally, thoracotomy potentially leads to chronic PTP [Citation1–3]. Thus, pain relief after thoracic surgery is of significance for reduction of PO pulmonary and cardiac complications [Citation4].
Thoracic paravertebral blockade (TPVB) is the technique of injecting local anesthetic adjacent to the thoracic vertebra close to where the spinal nerves emerge from the inter-vertebral foramina resulting in ipsilateral somatic and sympathetic nerve blockade in multiple dermatomes above and below the site of injection. A catheter may be inserted to extend the benefit of the block beyond the pharmacologic properties of the local anesthetic used [Citation5–7].
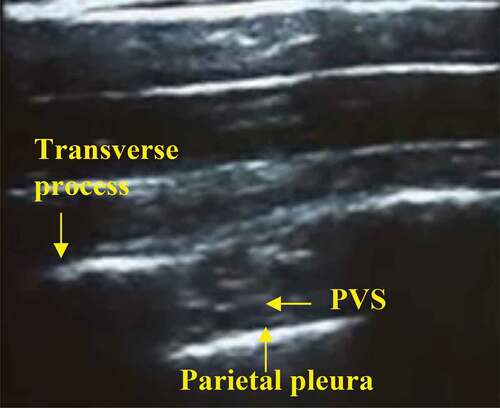
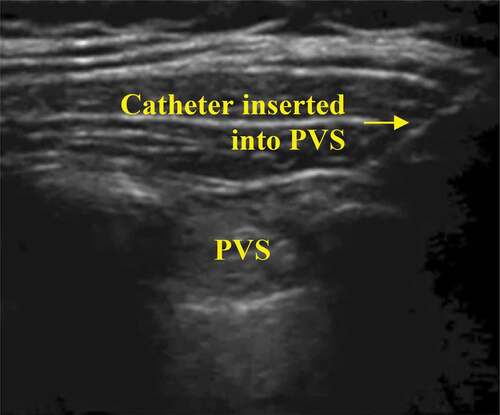
However, locating the thoracic paravertebral space (TPVS) can be technically difficult because it requires location of the transverse process and blind needle placement gives a failure rate of 6.8–10%. Also, failure to identify the transverse process results in several needle reorientations causing pain and increases the potential risk of complications. On contrary, the use of ultrasound offers several advantages including visualizing boundaries of the TPVS and sometimes its structures, the capability to visualize the needle, the spread of local anesthetic solution and the placement of a catheter in the PVS under direct vision, thus allowing depositing the local anesthetic solution and placing the catheter tip between the superior costo-transverse ligament and the parietal pleura [Citation8,Citation9].
The local anesthetic lidocaine has analgesic and anti-inflammatory properties due to the blockage of sodium channels and N-methyl-D-aspartate and G protein-coupled receptors [Citation10]. Systemic lidocaine was reported to decrease PO pain, analgesic consumption nausea and vomiting, and the length of hospital stay. In addition to be easy to administer, it has low price, accessibility and safety [Citation11].
This study aimed to compare the analgesic effects of paravertebral block versus lidocaine infusion for the management of post-thoracotomy pain.
2. Methods
The current prospective comparative study was conducted at Departments of
Anesthesia, National cancer institute, Cairo University from Jan 2018 till April
2018. The study protocol was approved by the Hospital Local Ethical Committee
and was registered in Pan African Clinical Trials Registry (PACTR201805003410305) aimed to include 60 patients (Consort flow diagram) who were scheduled for open thoracotomy after written informed consent was obtained from each patient.
2.1. Inclusion criteria
American Society of Anesthesiologists (ASA) status I to III adults,
Age of patients from 36 to 66 years,
Sex all genders,
Patients scheduled for open thoracotomy.
2.2. Exclusion criteria
Patients with systemic diseases, such as diabetes mellitus, hypertension,
Renal or hepatic dysfunction,
Bleeding diathesis,
Neurological diseases,
Hypersensitivity to the used drugs.
For equalization of comparisons, all the procedures were performed by the same team of anesthetists and surgeons.
Demographic and preoperative ASA grading and hemodynamic data were collected. Then, patients were randomly, using sealed envelopes chosen by the patient, allocated into two equal groups: IV Lidocaine Group included patients assigned to receive postoperative (PO) analgesia in the form of intravenous lidocaine 1%, in a dose of 1.5 mg/kg as initial dose over 10 min then as continuous infusion of 1.5 mg/kg/h for 48 h, which equals half of the dose that was previously used by Kuo et al. [Citation12]. PVB group included patients assigned to receive post-operative analgesia in the form of 10 ml of 1% lidocaine over 30 s then continuous PVB using lidocaine 1% infusion at the rate of 1.5 mg/kg/h through catheter inserted in the thoracic paravertebral space (PVS) under ultrasound guidance. In both groups, infusions were started immediately postoperatively and were stopped once complications occurred including nausea and vomiting, urinary retention, respiratory depression and resumed after stabilization.
2.3. Procedure of thoracic PVB
An open venous access on the contralateral side was prepared and patients were non-invasively monitored for pulse rate, blood pressure and pulse oximetry during the procedure. Patients were pre-medicated by intravenous midazolam 2 mg and with the patient in the sitting position, both cervical–thoracic paravertebral areas were disinfected.
The ultrasound (8–14 MHz curved array probe in Siemens ACUSON X300 Ultrasound System) was used and initial U/S examination of the T3 and T6 paravertebral region at the surgical side was performed using transportable U/S equipment and a 50-mm linear 6 MHz probe. The sequence of U/S examination is as follows: identification of T3 and T6 spinous processes by positioning of the U/S probe at the spinous process of T3, lateral movement until the transverse process is visible, and oblique movement until the transverse process and the parietal pleura are visualized in one image with PVS in-between as shown in . After skin infiltration with 1 ml of lidocaine 1%, an out-of-plane needle guidance technique with the needle positioned 1 cm caudal to the US probe, a 22 G Touhy needle 8 cm length (Perifix Epidural Needle) was advanced and PVB was performed according to the method described by Marhofe et al., [Citation13]. Then, the catheter was tunneled away from the surgical field ().
2.4. Anesthetic procedure
Anesthetic procedure was standardized for all patients including the use of double-lumen endobronchial tubes to allow single lung ventilation. Anesthesia was induced by a bolus of fentanyl (1–2 μg/kg) followed by Propofol (1–2 mg/kg) and vecuronium was given in dose of 0.1 mg/kg to facilitate tracheal intubation and was continued throughout duration of surgery. All patients received sevoflurane 1–2% and 0.05 mg/kg morphine for maintenance of anesthesia. After the induction of anesthesia, an arterial catheter was placed in the radial artery, and a central venous line (two lumens 20 cm long) was applied. After clinical confirmation of correct double-lumen tube placement (by inspection and auscultation) with the patient in both the supine and lateral decubitus positions, ventilation was controlled by using 100% oxygen and a tidal volume starting by 8–10 ml/kg then turned to 4–5 ml/kg. The rate is adjusted to maintain the PaCO2 between 35 and 40 mmHg. Effective lung isolation was determined by the absence of a leak from the non-ventilated lumen of the endobronchial tube. When the pleura was opened, the isolation was confirmed by direct observation of the collapsed non-ventilated lung and the absence of leak from this lung.
2.5. Outcome measures
2.5.1. Primary outcomes
Adequacy of analgesia was assessed using a 100-mm pain VAS with 0 means no pain and 100 mean the worst pain imaginable, patients were asked to rate their pain at rest every hour for 3 h and then at 12-, 24-, 36- and 48-h PO. Adequate analgesia was defined as a VAS <30 mm at rest and inadequate analgesia was defined as VAS at rest >30 mm despite the adjusted rate of infusions. In case of inadequate analgesia, IV morphine bolus (2 mg) was given and repeated on request.
2.5.2. Secondary outcomes
Hemodynamic and respiratory measures including heart rate (HR), mean arterial blood pressure (MAP), respiratory rate and peripheral arterial oxygen saturation were determined every hour for 3 h and 3 hourly till the end of the first 24-h PO and expressed collectively at end of 24 h.
Immediate PO data including the frequency of need for mechanical ventilation (MV) and its duration, duration of ICU stay, time till start of respiratory exercise and time till removal of chest drainage tube.
Expected complications of lidocaine is bradycardia hypotension, seizer, convulsion, complications of PVB: infection, pneumothorax.
2.5.3. Sample size calculation
Mistry et al. [Citation14] studied 26 patients divided into two groups including 16 and 10 patients to evaluate the effectiveness of PVB for immediate postoperative pain control in living liver donors and reported markedly reduced PO pain trajectory in catheter group than in non-catheter group. The current study supposed to get significant difference in VAS pain scoring in favor of PVB with a study power of 90% at α value of 0.05 and β value of 0.1 when patients’ number is >19 patient per group. Considering the possibility of dropout of patients during immediate postoperative course, number of enrolled patients was 30 patients per group and the allowable minimum number was 20 patients per group.
2.6. Statistical analysis
Obtained data were presented as mean±SD, numbers and percentages. Results were analyzed using Wilcoxon ranked test for unrelated data (Z-test) for intergroup comparisons; paired t-test for intragroup comparisons; and chi-square test (X2 test) for non-parametric analysis of numbers and ratios using Friedman test. Statistical analysis was conducted using the SPSS (Version 15, 2006; SPSS Inc., Chicago, IL, USA) for Windows statistical package. P-value <0.05 was considered statistically significant [Citation15].
3. Results
The study included 60 patients: 47 males and 13 females with mean age of 51.4 ± 8.5, range: 36–66 years. Twenty-nine patients (48.3%) were ASA physical status grade I, 17 patients (28.3%) were ASA grade II and 14 patients (23.4%) were ASA grade III. Thirty-seven patients were ex-smokers, 11 patients were current smokers and 12 patients were never smokers. Thirty-four patients (56.7%) were obese, 20 patients (33.3%) were overweight and only six patients (10%) were of average weight with a mean body mass index of 30.4 ± 2.6, range: 24.4–34.2 Kg/m2. There was a non-significant (p > 0.05) difference between studied patients about the age, sex, ASA grade, weight, height and body mass index. Patients’ details are shown in .
Table 1. Patients’ enrolment data
Twenty-three patients (38.3%) had lobectomy, 11 patients (18.3%) bi-lobectomy, 10 patients (16.7%) had pneumonectomy, nine patients (15%) had sleeve lobectomy and seven patients (11.7%) had segmentectomy. Mean duration of surgery was 142.3 ± 30.4, range: 110–180 minutes; mean duration of one-lung ventilation was 132.6 ± 16.6, range: 100–160 min and mean amount of intraoperative blood loss was 398.4 ± 104.1, range: 225–640 ml. About the type of tumor, 35 patients (58.3%) had adenocarcinoma, 13 patients (21.7%) had large cell carcinoma and another 12 patients (20%) had squamous cell carcinoma. There was non-significant (p > 0.05) difference between both groups about operative data and type of tumor ().
Table 2. Operative data
The procedure of paravertebral block was performed successfully without procedure-related complications. Both groups showed significantly decreased heart rate and MAP measures determined immediately after the end of surgery (prior to start of infusion) compared to preoperative measures with non-significant (p > 0.05) difference between PO measures of both groups. Throughout the first 24 h after surgery, HR and MAP measures were significantly lower compared to preoperative measures in both groups with non-significant difference between both groups at all estimates. However, respiratory rate and percentage of arterial oxygen saturation were non-significantly (p > 0.05) decreased on all PO estimations compared to preoperative measures with non-significant (p > 0.05) difference between both groups despite being in favor of PVB group ().
Table 3. Hemodynamic and respiratory data of studied groups throughout 24-h PO
All patients were transferred immediately to ICU; 17 patients could not be extubated and were maintained on mechanical ventilation for a mean duration of 1.5 ± 0.5, range: 1–2 days. Despite of the non-significantly (p > 0.05) higher frequency of patients who could not be extubated in PVB group, they were successfully weaned of mechanical ventilation and extubated after a significantly (p = 0.046) shorter duration compared to those of IV group. Concerning the remaining 43 patients, the mean duration of ICU stay for patients of PVB group was significantly (p = 0.025) shorter compared to those of IV group. Total ICU stay duration was significantly (p = 0.023) shorter in PVB group compared to IV group. Administration of PVB allowed earlier start of respiratory exercise with significantly (p = 0.001) shorter duration till start of respiratory exercise compared to those received IV lidocaine. Duration till removal of chest drainage was significantly (p = 0.01) shorter in PVB group compared to IV group ()
Table 4. Immediate post-operative data
Pain VAS scores could not be determined for patients maintained on mechanical ventilation, so pain VAS scores were determined for only 43 patients: 23 in IV group and 20 in PVB group. Both analgesic modalities alleviated post-thoracotomy pain; however, PVB provided more perfect analgesia manifested as significantly lower pain VAS scores determined at 1- (p = 0.021), 2- (p = 0.017), 12- (p = 0.042) and 36-h PO (p = 0.017). At 3- and 24-h PO, pain VAS scores were non-significantly (p > 0.05) higher in PVB group compared to IV group, while at 48-h PO pain VAS scores were non-significantly (p > 0.05) lower in PVB group compared to IV group (). Cumulative 48-h pain VAS score of patients of both groups was significantly (p = 0.005) lower in PVB group compared to IV group (, ).
Figure 3. Mean Pain VAS Score of patients of both groups determined throughout first 48 hours postoperative (![]()
Table 5. Pain VAS scores of patients of both groups determined throughout the first 48-h PO
All patients requested rescue analgesia; 28 patients requested it once and 15 patients requested it twice. The frequency of higher consumption of rescue analgesia was significantly higher (X2 = 25.221, p = 0.0003) in IV group compared to PVB group with significantly (p = 0.003) higher mean number of requests in IV group compared to PVB group (). Mean calculated dose of rescue analgesia was significantly (p = 0.003) high in IV group compared to PVB group (). No PO complication related to PVB or intravenous lidocaine were detected, but were mostly related to morphine consumption as a rescue analgesia, so it was more frequent in patients received intravenous lidocaine, despite of the non-significant difference between both groups
4. Discussion
Both applied analgesic modalities provided proper postoperative analgesia for patients who underwent thoracotomy; however, PVB provided superior outcome compared to IV lidocaine manifested as significantly lower VAS pain scores with significantly lower consumption of rescue analgesia. Proper PO analgesia provided by PVB was reflected clinically as significantly shorter time on mechanical ventilation, if required, shorter time of ICU stay and time till start of respiratory exercise. Early ambulation and start of respiratory exercise indicated minimal or no pain sensation during forced actions of respiratory muscles.
The frequency of analgesia-related complications was significantly higher in IV group compared to PVB group and were mostly due to increased morphine consumption; a finding indicated safety of lidocaine given either intravenously or locally and safety of PVB which by its virtue reduced the frequency of rescue analgesia and so minimized the dose of morphine used with subsequent reduction of its complications.
The reported superior beneficial effects of PVB over IV lidocaine analgesia go in hand with Arunakul & Ruksa [Citation16] who found patients following modified radical mastectomy under PVB and general anesthesia to have lower incidence and severity of PO complications and no patients were unsatisfied with anesthetic technique compared to those received general anesthesia alone. the reported superior beneficial effect of paravertebral block over IV lidocaine analgesia supported that previously reported concerning the superiority of nerve block over intravenous analgesia irrespective of the surgical procedure as documented by Kuo et al. [Citation12]
Concerning the outcome of patients who received PVB for post-thoracotomy pain (PTP), the obtained results are in line with Joshi et al. [Citation17] who conducted systematic review of randomized trials evaluated thoracic epidural analgesia (TEA) and PVB compared to each other and to systemic opioid analgesia, in adult thoracotomy and found continuous PVB was as effective as TEA with local anesthetic but was associated with a reduced incidence of hypotension, pulmonary complications compared with systemic analgesia, whereas TEA did not. In a similar review study, Daly & Myles [Citation18] reported that PVB can provide acceptable pain relief compared with TEA, less frequent side-effects, better pulmonary function and fewer pulmonary complications and contraindications to TEA do not preclude PVB, which can also be safely performed in anesthetized patients without an apparent increased risk of neurological injury.
Moawad et al. [Citation19] found single injection PVB to result in similar analgesia but greater hemodynamic stability than epidural analgesia in patients undergoing renal surgery, so it may be recommended for patients with coexisting circulatory disease. Ding et al. [Citation20] conducted meta-analysis for articles compared TEA and PVB for pain control after thoracic surgery and concluded that PVB can provide comparable pain relief to traditional thoracic epidural block and have a better side-effect profile with lower rates of failed block.
The obtained results indicated the feasibility, efficacy and safety of PVB using continuous catheter infusion of lidocaine and go in hand with Gulbahar et al. [Citation21] who documented that PVB catheterization can be easily performed and placed in a short span perioperatively and therefore, it might be the preferred method over Thoracic epidural block which has a high incidence of adverse effects and complication rates. Pintaric et al. [Citation22] found continuous PVB to result in similar analgesia but greater hemodynamic stability than epidural analgesia in patients having thoracotomy. Pipanmekaporn & Saeteng [Citation23] documented that continuous thoracic PVB offered satisfactory pain control with less complications and could be considered as an alternative when TE block is difficult to access. Elsayed et al. [Citation24] found PVB catheter analgesia to be as effective as TE for reducing the risk of PO complications but is associated with a shorter hospital stay and better analgesia for fast-track thoracic surgery. Katayama et al. [Citation25] reported that continuous PVB is safe in patient’s ineligible for epidural block and can contribute to their pain relief following pulmonary resection procedure. Júnior Ade et al. [Citation26] documented that continuous PVB showed a lower incidence of side effects with reduced frequency of urinary retention and hypotension compared to continuous TEA.
Komatsu et al. [Citation27] reported that continuous PVB could provide adequate PTP control and allow good cough effort with the need for weak rescue analgesia. Also, Raveglia et al. [Citation28] reported statistically significant differences in favor of PVB for both cough and rest pain control and respiratory function in terms of FEV1 and ambient air saturation levels compared to continuous infusion analgesia using TE catheter and concluded that drugs administered through PVB catheter are very effective and does not present contraindications to its positioning or collateral effects.
5. Conclusion
Ultrasound guidance allowed safe and feasible PV space catheterization. PVB using continuous lidocaine infusion provided adequate analgesia for PTP with significant reduction of rescue analgesia, shorter time till start of respiratory exercises, improved pulmonary functioning with minimal complications.
(![]() significant differance)
significant differance)
(![]() significant differance)
significant differance)
(![]() significant differance)
significant differance)
Availability of data and materials
The data that support the findings of this study are available from Cairo
university hospitals but restrictions apply to the availability of these data,
which were used under license for the current study, and so are not publicly
available. Data are however available from the authors upon reasonable
request and with permission of Cairo university hospitals.
Acknowledgments
The authors provide thanks to all members of Cardiothoracic Department, Cairo University Hospital for assistance for completion of the current work.
Disclosure statement
The authors declare that they have no competing interests.
Additional information
Funding
References
- Durá Navarro R. De Andrés Ibáñez J: a review of clinical evidence supporting techniques to prevent chronic postoperative pain syndromes. Rev Esp Anestesiol Reanim. 2004 Apr;51(4):205–212.
- Lu YL, Wang XD, Lai RC. Correlation of acute pain treatment to occurrence of chronic pain in tumor patients after thoracotomy. Ai Zheng. 2008 Feb;27(2):206–209.
- Kinney MA, Hooten WM, Cassivi SD, et al. Chronic post-thoracotomy pain and health-related quality of life. Ann Thorac Surg. 2012 Apr;93(4):1242–1247.
- De Cosmo G, Aceto P, Gualtieri E, et al. Analgesia in thoracic surgery: review. Minerva Anestesiol. 2009;75(6):393–400.
- Arnal D, Garutti I, Olmedilla L. Paravertebral analgesia in thoracic surgery. Rev Esp Anestesiol Reanim. 2004;51(8):438–446.
- Sato N, Sugiura T, Takahashi K, et al. Analgesia with paravertebral block for postoperative pain after thoracic or thoracoabdominal aortic aneurysm repair. Masui. 2014;63(6):640–643.
- Karmakar MK, Samy W, Li JW, et al. Thoracic paravertebral block and its effects on chronic pain and health-related quality of life after modified radical mastectomy. Reg Anesth Pain Med. 2014;39(4):289–298.
- Hura G, Knapik P, Krakus A, et al. Anatomical basis and technique of thoracic paravertebral blockade. Wiad Lek. 2005;58(5–6):313–318.
- Bondár A, Szűcs S, Iohom G. Thoracic paravertebral blockade. Med Ultrason. 2010;12(3):223–227.
- Koppert W, Ostermeier N, Sittl R, et al. Low dose lidocaine reduce secondary hyperalgesia by a central mode of action. Pain. 2000 Mar;85(1–2):217–224.
- Kim TH, Kung H, Hong JH. Intraperitoneal and Intravenous lidocaine for effective pain relief after laparoscopic appendectomy: aprospective, randomized, double-blind, placebo-controlled study. Surg Endovasc. 2011;25: 3183–3190.
- Kuo CP, Jao SW, Chen KM, et al. Comparison of the effects of thoracic epidural analgesia and i.v. infusion with lidocaine on cytokine response, postoperative pain and bowel function in patients undergoing colonic surgery. Br J Anaesth. 2006;97(5):640–646.
- Marhofe P, Kettner SC, Hajbok L, et al. Lateral ultrasound-guided paravertebral blockade: an anatomical-based description of a new technique. Br J Anasth. 105(4):526–532.
- Mistry K, Hutchins J, Leiting J, et al. Continuous Paravertebral Infusions as an Effective Adjunct for Postoperative Pain Management in Living Liver Donors: a Retrospective Observational Study. Transplant Proc. 2017 Mar;49(2):309–315. .
- Day SJ, Graham DF. Sample size and power for comparing two or more treatment groups in clinical trials. BMJ. 1989;299:663–665.
- Arunakul P, Ruksa A. General anesthesia with thoracic paravertebral block for modified radical mastectomy. J Med Assoc Thai. 2010;93(Suppl 7):S149–53.
- Joshi GP, Bonnet F, Shah R, et al. A systematic review of randomized trials evaluating regional techniques for postthoracotomy analgesia. Anesth Analg. 2008;107(3):1026–1040.
- Daly DJ, Myles PS. Update on the role of paravertebral blocks for thoracic surgery: are they worth it? Curr Opin Anaesthesiol. 2009;22(1):38–43.
- Moawad HE, Mousa SA, El-Hefnawy AS. Single-dose paravertebral blockade versus epidural blockade for pain relief after open renal surgery: a prospective randomized study. Saudi J Anaesth. 2013;7(1):61–67.
- Ding X, Jin S, Niu X, et al. A comparison of the analgesia efficacy and side effects of paravertebral compared with epidural blockade for thoracotomy: an updated meta-analysis. PLoS One. 2014;9(5):e96233.
- Gulbahar G, Kocer B, Muratli SN, et al. A comparison of epidural and paravertebral catheterisation techniques in post-thoracotomy pain management. Eur J Cardiothorac Surg. 2010;37(2):467–472.
- Pintaric TS, Potocnik I, Hadzic A, et al. Comparison of continuous thoracic epidural with paravertebral block on perioperative analgesia and hemodynamic stability in patients having open lung surgery. Reg Anesth Pain Med. 2011;36(3):256–260.
- Pipanmekaporn T, Saeteng S. The use of continuous thoracic paravertebral nerve block under direct vision for postoperative pain management in thoracic surgery. J Med Assoc Thai. 2012;95(2):191–197.
- Elsayed H, McKevith J, McShane J, et al. Thoracic epidural or paravertebral catheter for analgesia after lung resection: is the outcome different? J Cardiothorac Vasc Anesth. 2012;26(1):78–82.
- Katayama T, Hirai S, Kobayashi R, et al. Safety of the paravertebral block in patients ineligible for epidural block undergoing pulmonary resection. Gen Thorac Cardiovasc Surg. 2012;60(12):811–814.
- Júnior Ade P, Erdmann TR, Santos TV, et al. Comparison between continuous thoracic epidural and paravertebral blocks for postoperative analgesia in patients undergoing thoracotomy: systematic review. Braz J Anesthesiol. 2013;63(5):433–442.
- Komatsu T, Sowa T, Takahashi K, et al. Paravertebral block as a promising analgesic modality for managing post-thoracotomy pain. Ann Thorac Cardiovasc Surg. 2014;20(2):113–116.
- Raveglia F, Rizzi A, Leporati A, et al. Analgesia in patients undergoing thoracotomy: epidural versus paravertebral technique. A randomized, double-blind, prospective study. J Thorac Cardiovasc Surg. 2014;147(1):469–473.