ABSTRACT
Background
The goal of this study was to compare the analgesic efficacy of dexmedetomidine and levobupivacaine in adductor canal block (ACB) in total knee arthroplasty (TKA) patients, as well as the ambulation ability and adverse effects.
Methods
Sixty patients, ranging in age from 18 to 60 years old and with an ASA status of I to II, had unilateral TKA under spinal anesthesia. They were randomized into two groups; Group L received 20 mL of 0.25% levobupivacaine and Group LD received 20 mL of 0.25% levobupivacaine plus 0.5 µg/kg dexmedetomidine for ACB. The time it took for the first analgesic to be requested, the amount of morphine used in a 24-hour period, the postoperative pain score, and the range of motion (ROM), a 100-foot walking test data, sedation, patient satisfaction, and adverse outcomes were measured.
Results
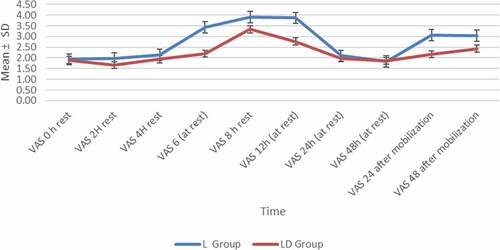
LD group had lower scores of VAS either at rest or on movement at nearly all-time intervals. The mean time to first analgesic request in group L (406.77 ± 10.64 min) and group LD (515.10 ± 27.98 min, P-value <0.001). The mean total dose of morphine consumed in first 24 h postoperative was significantly lower in LD group (6.47 ± 2.01 mg) when compared to L group (10.93 ± 2.35 mg, P value <0.001). There were significant differences in ROM test, 100 foot test, and patient satisfaction between groups but no major adverse effects in both groups.
Conclusion
The addition of 0.5 µg/kg dexmedetomidine to 20 mL of 0.25% levobupivacaine in single-shot ACB is better than 20 mL of 0.25% levobupivacaine alone regarding postoperative analgesia, patient satisfaction and ambulation ability following TKA but, with low rate of adverse events in both groups.
1. Introduction
Total knee arthroplasty (TKA) surgery is accompanied with considerable postoperative pain. Early postoperative mobilization and rehabilitation require adequate pain management. Despite the fact that femoral nerve block (FNB) or continuous epidural anesthesia (CEA) can provide adequate postoperative pain control, both treatments have negative side effects such as muscle weakness, which can delay postoperative mobilization [Citation1].
The adductor canal block (ACB) is a relatively novel analgesic block for knee surgery that not only blocks the femoral nerve’s largest sensory branch, but also causes a smaller decrease in quadriceps muscle strength in adult patients than the femoral nerve block (FNB) [Citation2,Citation3].
ACB gives at least equal analgesia to FNB, preserves quadriceps muscular strength better than FNB, and so allows for functional recovery within the first day after TKA, according to randomized controlled trials [Citation4–6]. The brief duration of analgesia provided by single-shot peripheral nerve block is a significant disadvantage. Because severe pain usually lasts 2–3 days after TKA, a continuous ACB via catheter appears to be a suitable option. Perineural catheters, on the other hand, can be difficult to insert, are prone to early dislodgement, and can raise the risk of infection. After continuous ACB, certain cases of local anesthetic-induced myotoxicity have been reported [Citation7].
Levobupivacaine is a new long-acting amide-type local anaesthetic that is less toxic to the heart and nervous system [Citation8].
Dexmedetomidine, a highly selective alpha 2 agonist [Citation9], has been utilized to increase the duration of analgesia induced by local anesthetics (LA). Perineural dexmedetomidine has a primarily peripheral impact, and it can develop its analgesic effect by maintaining nerve fiber hyper-polarization and inhibiting synaptic transmission [Citation10].
As a result, this study was designed to look at the benefits of dexmedetomidine as an adjuvant to LA for extending the duration of postoperative analgesia produced by adductor canal block in TKA patients.
The primary outcome was the assessment of duration of analgesia detected by the first analgesia rescue call and total analgesic consumption. Secondary outcomes included the impact of single-shot adductor canal block using levobupivacaine and dexmedetomidine on postoperative recovery, like VAS pain scores, sedation, maximal ranges of flexion and extension and a 100-foot walking test and patient satisfaction and the side effects that could occur in the 24-hour study period in patients undertaking total knee arthroplasty.
2. Methods
2.1. Patients
The Medical Research Ethics Committee, Faculty of Medicine, Assiut University, Assiut, Egypt, approved this prospective randomized clinical double-blind trial (approval number: 17,300,626). ClinicalTrials.gov was used to register it (NCT04968392), and the Helsinki Declaration was followed. From March 2019 to May 2020, this study was conducted in the orthopedic surgical sector.
We registered a total of sixty patients aged 18–60 years old with ASA physical status I or II who had elective primary total knee arthroplasty surgery under spinal anesthesia after receiving informed written consent from all patients.
Patients with a history of significant kidney, liver, or cardiac disease, as well as any known convulsive disorder, autoimmune diseases, psychiatric illness, chronic pain, pregnant women, fixed use of analgesics, antidepressants, or opioids in the previous 2 months, morbid obesity, revision operations and allergies to local anesthetics or morphine, were excluded from the study.
Randomization and blinding: The patients were randomly divided into two groups using a computer-generated randomized table of numbers (30 patients each).
2.1.1. Group L (levobupivacaine)
Thirty patients received total volume of 20 mL of 0.25% levobupivacaine (0.5% levobupivacaine 10 ml diluted with sterile normal saline 10 ml) plus 1 mL normal saline.
2.1.2. Group LD (levobupivacaine + dexmedetomidine)
Thirty patients received total volume 20 mL of 0.25% levobupivacaine plus 0.5 µg/kg dexmedetomidine and completed it to 1 ml by adding normal saline.
Well-trained investigators who were not involved in data collecting prepared syringes with drugs. The surgeon, anesthesiologist, patient, and examiner who collected and interpreted the data were unaware of the intervention assignments. The anesthetist prepared the study drugs based on the patient’s preoperative weight and a random drug selection. Syringes were kept in opaque envelopes with numbers ranging from 1 to 60. The envelope codes were only accessible to the anesthesiologist who filled the envelopes.
3. Anesthesia and monitoring
3.1. Preoperative care
Preoperative assessment and evaluation of patients participating in the study was done. The study procedure was described to the participants. Participants were told that they could withdraw out of the study at any time without losing their medical coverage. Before performing elective anesthesia, standard preoperative fasting techniques were tracked.
Patients were trained to use the PCA device preoperatively and explained to rate pain score with the Visual Analogue Score from 0 to 10; (0 representing no pain and 10 for the worst pain) both at rest and during movement.
All patients did not receive any pre-emptive analgesic medication. Intravenous antibiotic and tranexamic acid (750 mg) were administered 30 minutes prior to surgery.
3.1.1. Anesthesia
Peripheral venous access was established, and standard ASA monitors (pulse oximeter, electrocardiogram and NIBP) were applied to all patients on their arrival in the anesthesia room. Pre-hydration with 500 mL intravenous crystalloid was given. Spinal anesthesia was performed with the patient in a lateral recumbent position. A 27-gauge needle was inserted at the L3-4 intervertebral space, and after ensuring that clear cerebrospinal fluid was in free flow, 15 mg bupivacaine (3.0 mL of a 0.5% hyperbaric solution) was given to achieve sensory blockade at or above the T10 dermatome. All patients did not receive any sedative medication.
The total knee replacements were achieved in the standard method to all patients. A pneumatic tourniquet used and a suction drain was used.
3.1.2. Experimental protocol
A nurse who was not included in the study released an opaque sealed envelope that informed whether the patient should receive 20 mL of 0.25% levobupivacaine + 0.5 µg/kg dexmedetomidine or 20 mL of 0.25% levobupivacaine + 1 mL normal saline. The total drug volume was kept constant in both groups to avoid bias during drug administration.
The ACB was performed postoperatively at the post-anesthesia care unit (PACU) by an experienced anesthesiologist who was blinded to the addition of a perineural adjuvant. After sterile preparation and draping, the 8-cm, 22-gauge needle was inserted in-plane from the lateral side at the mid-thigh level in the supine position [Citation11] and advanced through the sartorius muscle and fascia. ACB was achieved under real-time ultrasound guidance, via an ultrasound machine with a high-frequency linear ultrasound probe and the adductor canal, with the superficial femoral artery and vein within, was recognized. Once the needle tip was placed in the adductor canal, 1–2 mL of normal saline was injected to confirm the position of the needle, then the perineural medication was injected anterior to the artery and deep under the sartorius muscle.
4. Assessment parameters
Patient’s clinical and demographic characteristics; include; age, sex, ASA class, weight and duration of the operation.
Preoperatively, intraoperatively, and then continuously for the first hour after the ACB, then 6-hourly for rest of the first 24 hours, heart rate (HR), non-invasive arterial blood pressure (NIBP), and SpO2 were measured.
The degree of sedation was assessed by Ramsay sedation scale [Citation12]: at 2,4,6,8,12 and 24 hours after the operation.
The preoperative VAS pain score was also assessed immediately after the ACB and then 2-hourly for the next 8 hours, then at 12 h, 24 h till 48 h at rest and the score was recorded on movement at 24 h and 48 h.
The time to first rescue dose and total morphine consumption in 24 hours were recorded.
Range of movement (ROM): maximal ranges of flexion and extension were also assessed and recorded by a blinded physiotherapist preoperatively, 1st day and 1 month postoperatively [Citation13].
In addition, a 100-foot walking test data throughout the preoperative time, at 24 and 48 hours after the surgery.
Satisfaction score also assessed and recorded at 24 hours after the ACB by Likert score: 5 = strongly satisfied, 4 = moderate satisfied, 3 = neutral, 2 = moderate dissatisfied, 1 = strongly dissatisfied.
5. Postoperative protocol
5.1. Postoperative pain management
The patient was observed at least 60 minutes in the PACU, and then they were discharged from PACU to the ward. At PACU, the patients were connected with the PCA devices, allowing them to control pain. The PCA device contained 100 mL of morphine 1 mg/mL with the setting of morphine bolus dose 1 mL, no background infusion, and lockout interval 15 minutes.
5.2. Physical therapy
Between 12 and 24 hours after surgery, all subjects were given a knee immobilizer until quadriceps muscle function was recovered. Physiotherapy was started 24 hours after surgery. With a primary setting of 45 degrees, the use of a Continuous Passive Motion Machine in an orthopedic room began. On the second postoperative day, CPM was given to the patient for 2 hours.
6. Statistical analysis
6.1. Power of the study
The duration of postoperative analgesia, as evaluated by the time to the first call for rescue analgesics, was the study’s primary goal. A target sample size was calculated based on the results of a pilot study. According to a power analysis, a sample size of 27 patients in each group would have 95% power at the 0.05 level of significance to detect a difference of 0.8 effect size between the two groups in the time to the first request for rescue analgesics. A total of 60 individuals were included to adjust for patient dropout.
6.2. Data analysis
The distribution of baseline variables was calculated using the Shapiro–Wilk test. Continuous variables were described using mean (SD) and evaluated using Student’s t-test and one-way test of variance (ANOVA) with many comparisons. The median (range) was utilized to show nonparametric data, and the Mann–Whitney U-test was employed to compare the two groups. Categorical data was reported using numbers and percentages, which were analyzed via chi-square test or Fisher’s exact test. Statistical significance was defined as a P value <0.05. IBM SPSS Statistics version 20 (SPSS Inc, Chicago, IL, USA) was used for all statistical analyses.
7. Results
Sixty individuals were chosen for the study from a total of 68 who were evaluated for eligibility; each group included 30 patients ().
A single surgeon performed all of the surgeries. Anaesthetists with extensive experience in ultrasound-guided peripheral nerve block performed all ACBs. There were no significant variations in age, height, weight, sex or duration of operation between the groups of individuals ().
Table 1. Demographic data, patient’s characteristics and patient satisfaction score
Vital signs: There were no significant differences between groups in mean MAP at other time points, mean heart rate, or SPO2 at any of the time points analyzed (data not presented). NIBP and HR were stable throughout the procedure.
In the postoperative period, to determine the need for rescue analgesia, the pain was assessed using the VAS score. The VAS scores in the LD group were significantly lower. We found that it was statistically insignificant over the first 4 hours, i.e., from baseline to 4 hours, with a P value of >0.05. At 6 th, 8th, and 12th hours postoperatively.
The difference in VAS scores (at rest) between the two groups becomes statistically significant (P < 0.05). At 24 hours following surgery, the difference in VAS scores (after mobilization) between the two groups becomes statistically significant. At almost all time periods, the LD group had lower VAS scores ().
7.1. The analgesic consumption and rescue analgesia
The (L group) had a higher VAS score, requiring rescue analgesia at 406.77 ± 10.64 min, but the (LD group) had a higher VAS score, requiring rescue analgesia at 515.10 ± 27.98 min.
Not only was the time required for the first rescue analgesia significantly longer in the LD group (P value <0.001), but also the mean total dose of rescue analgesia taken in first 24 h postoperative was significantly lower in LD group (6.47 ± 2.01 mg) when compared to L group (10.93 ± 2.35 mg, P value <0.001). The postoperative rescue analgesia was given with PCA as needed or at any time the VAS score was ≥4 over a period of 24 hours ().
Table 2. The rescue analgesia and analgesic consumption
7.2. Postoperative sedation
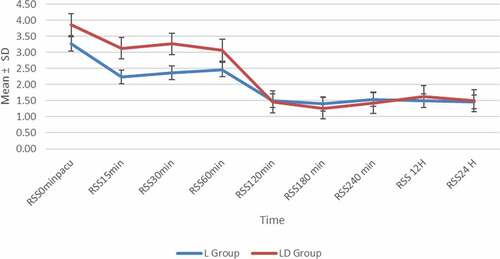
In the first 24 hours after surgery, the Ramsay sedation score was used to assess sedation. In both groups, it decreased over time. Until nearly 1 hour after surgery, the LD group’s mean sedation values were significantly higher than the L group’s ().
7.3. Range of movement (ROM) and 100-foot walking tests
The L group had poorer range of extension and flexion than the LD group on the first day and first month after surgery when the preoperative and postoperative scores were excluded. On the first day, the groups had significant differences in range of extension and flexion (P < 0.05) ().
Table 3. Range of movement (ROM) and 100-foot walking tests
In contrast to the preoperative measurements, the time for performing the 100-foot walk test in the L group was significantly longer than in the LD group 24 and 48 hours after the operation (214.8 ± 19.2 versus 192.1 ± 15.6 s and 138.5 ± 10.3 versus 113.3 ± 9.6 s, correspondingly; P < 0.001) ()
7.4. Side effects
Finally, during the course of the trial, neither group of patients experienced any serious complications. During the follow-up period, there were no cases of neurologic deficit.
One month after surgery, there was no postoperative bleeding or infection, either primary or secondary. The patient has no major complaints.
7.5. Patients’ satisfaction
Patients’ satisfaction measured using “Likert scale” was acceptable (very satisfied, satisfied, neutral) in nearly 72.5% of LD group as compared with 57.5% in L group, P < 0.05 ().
8. Discussion
The adductor canal block (ACB), a type of peripheral nerve block (PNB), is a sensory nerve block that was recently introduced as a way to provide analgesia while maintaining quadriceps muscle strength following TKA [Citation14,Citation15]. Various perineural adjuvants have been tested in single-shot ACB to improve the duration and quality of local anesthetic [Citation16].
The ultrasound-guided ACB is being investigated as a potential alternative to the FNB, which has side effects such as quadriceps weakness, delayed movement, and limitations in physiotherapy. Instead of a motor blockage on the knee, ACB achieves a more pure sensory blockage while maintaining pain control [Citation17].
According to the current study findings, a single-shot adductor canal block with a combination of levobupivacaine and dexmedetomidine (LD group) improved postoperative analgesia, increased the time to the first analgesic demand, decreased pain scores, and reduced the need for postoperative analgesia.
Levobupivacaine is the S (-) enantiomer of bupivacaine, which has less cardiac toxicity and motor blockage than bupivacaine but has a longer duration of action [Citation18]. The effects of levobupivacaine for FNB and PAI on postoperative VAS values were reported to be equivalent in a study by Wall et al. In the first 48 hours after surgery, the authors found that ACB resulted in better VAS values at rest and during activity than FNB [Citation19].
The current study agrees with the study of Kampitak et al. reported that combining local infiltrate analgesia (LIA) to single-dose ACB with 0.5% levobupivacaine 20 mL had a significantly longer time for 1st rescue dose [Citation20].
We discovered that the VAS scores at rest and on movement and the total amount of morphine consumed were lower in both groups, but it was better in the LD group than in the L group. Like our study, Goyal et al. demonstrated that addition of dexmedetomidine to ropivacaine can provide longer duration of analgesia, lesser tramadol consumption and lesser pain on movement than ropivacaine alone in dose-dependent manner in ACB after simultaneous bilateral TKA [Citation21].
Locally, perineural dexmedetomidine produces vasoconstriction, suppression of C-fiber discharge, and a reduction in inflammatory mediator release [Citation22]. Kang et al. discovered that dexmedetomidine causes neurotoxicity in neonate rats in a dose-dependent manner, and that low dosage dexmedetomidine is neuroprotective and reduces both inflammatory response and neuronal death [Citation23]. Because we were concerned that the majority of our participants were elderly patients, we used a low dose of dexmedetomidine (0.5 µg/kg), the lowest dose of therapeutic use, to add to 20 mL 0.25% levobupivacaine.
In contrast to our study, Oritz-Gomez et al. found no significant change in pain scores in the ACB group with and without Dexmedetomidine [Citation24].
This analgesic method is specifically developed to avoid sedation and allow for early movement and discharge following lower limb arthroplasty. Until one hour following admission to the PACU post-operatively, the LD group had considerable sedation levels. There were no incidents in which the patient was heavily sedated. Sedation progressed from full consciousness to calmness.
We discovered that the LD group had greater extension and flexion knee motions throughout the first week. Furthermore, the LD group performed better in the walking test than the L group. The LD group’s ROM and walking records were shown to be superior. The blocking of the saphenous nerve in the adductor canal with levobupivacaine in the first 48 hours after surgery demonstrates these outcomes.
The range of motion preoperatively is the main sign of the range of motion postoperatively. Several factors determine the range of motion postoperative. After a total knee replacement, rehabilitation programs should be continued until a knee flexion of at least 90 degrees is obtained, allowing patients to resume normal social life [Citation25].
According to Ritter et al., preoperative range of motion, intraoperative range of motion, posterior capsule relaxation, and the patient’s age are all factors to consider during surgery. They claimed that beyond the first year, there was no difference in the degree of flexion over time, and that the range of motion achieved in the first 6 months was important [Citation26].
The etiology of the osteoarthritis, the preoperative range of motion, the patient’s age, and the degree of posterior capsule relaxation during the procedure are all crucial factors to consider during knee prosthesis surgery. The ability of a patient to do functional tasks including walking, climbing stairs, and rising from a chair is dependent on proper postoperative knee ROM [Citation27].
Isometric quadriceps workouts are started on the first postoperative day in our service. Knee ROM exercises ranging from 0 to 30 degrees of flexion for the first 3 days, with at least 90 degrees of flexion between days.
Patients, who can walk 30 metres with assistance, use the bathroom, make transfers, do basic daily activities, and complete home exercise programs on their own are in a position of being released home, according to the common signs used in relation to TKA therapies. In the current study, ACB-LD performed better than ACB-L in the first 48 postoperative hours on the 100-foot walk test.
Furthermore, compared to the levobupivacaine alone, this combination in single-shot adductor canal blocks resulted in improved satisfaction on the first day following surgery without increasing the incidence of complications.
9. Limitations
There are certain limitations to this research. First, the success of the block was not validated after the bolus injection since the ACB was administered so soon after surgery that most patients’ spinal anaesthetic had not yet worn off. Second, we did not investigate whether dexmedetomidine affected the plasma levels of levobupivacaine.
9.1. Conclusion
The addition of 0.5 µg/kg dexmedetomidine to 20 mL of 0.25% levobupivacaine in single-shot ACB is better than 20 mL of 0.25% levobupivacaine alone regarding postoperative analgesia, patient satisfaction and ambulation ability following TKA but, with low rate of adverse events in both groups.
Acknowledgments
The authors gratefully acknowledge the assistance of all orthopaedic consultants, nurses, residents, and other surgical theatre personnel.
Disclosure statement
The authors declare that they do not have any conflicts of interest.
Additional information
Funding
References
- Bauer MC, Pogatzki-Zahn EM, Zahn PK. Regional analgesia techniques for total knee replacement. Curr Opin Anesthesiol. 2014;27(5):501–506.
- Jæger P, Koscielniak-Nielsen ZJ, Schrøder HM, et al. Adductor canal block for postoperative pain treatment after revision knee arthroplasty: a blinded, randomized, placebo-controlled study. PLoS One. 2014;9(11):e111951.
- Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of adductor canal block versus femoral nerve block on quadriceps strength, mobilization, and pain after total knee arthroplasty: a randomized, blinded study. Reg Anesthesia Pain Med. 2015;40(1):3–10.
- Jiang X, Wang Q, Wu C, et al. Analgesic efficacy of adductor canal block in total knee arthroplasty: a meta‐analysis and systematic review. Orthop Surg. 2016;8(3):294–300.
- Kuang M-J, Xu L-Y, Ma J-X, et al. Adductor canal block versus continuous femoral nerve block in primary total knee arthroplasty: a meta-analysis. Int J Surg. 2016;31:17–24.
- Thacher RR, Hickernell TR, Grosso MJ, et al. Decreased risk of knee buckling with adductor canal block versus femoral nerve block in total knee arthroplasty: a retrospective cohort study. Arthroplast Today. 2017;3(4):281–285.
- Neal JM, Salinas FV, Choi DS. Local anesthetic-induced myotoxicity after continuous adductor canal block. Reg Anesthesia Pain Med. 2016;41(6):723–727.
- Tas E, Hanci V, Ugur MB, et al. Does preincisional injection of levobupivacaine with epinephrine have any benefits for children undergoing tonsillectomy? An intraindividual evaluation. Int J Pediatr Otorhinolaryngol. 2010;74(10):1171–1175.
- Venn R, Bradshaw C, Spencer R, et al. Preliminary UK experience of dexmedetomidine, a novel agent for postoperative sedation in the intensive care unit. Anaesthesia. 1999;54(12):1136–1142.
- Abdallah F, Brull R. Facilitatory effects of perineural dexmedetomidine on neuraxial and peripheral nerve block: a systematic review and meta-analysis. Br J Anaesth. 2013;110(6):915–925.
- Wong WY, Bjørn S, Strid JMC, et al. Defining the location of the adductor canal using ultrasound. Reg Anesthesia Pain Med. 2017;42(2):241–245.
- Ramsay M, Savege T, Simpson B, et al. Controlled sedation with alphaxalone-alphadolone. Br Med J. 1974;2(5920):656–659.
- Klupiński K, Krekora K, Woldańska-Okońska M. Evaluation of early physiotherapy in patients after surgical treatment of cruciate ligament injury by bone-tendon-bone method. Polski Merkuriusz Lekarski. 2014;36(211):22–27.
- Ellis TA II, Hammoud H, Merced PD, et al. Multimodal clinical pathway with adductor canal block decreases hospital length of stay, improves pain control, and reduces opioid consumption in total knee arthroplasty patients: a retrospective review. J Arthroplasty. 2018;33(8):2440–2448.
- Laurant DB-S, Peng P, Arango LG, et al. The nerves of the adductor canal and the innervation of the knee: an anatomic study. Reg Anesthesia Pain Med. 2016;41(3):321–327.
- Turner JD, Dobson SW, Henshaw DS, et al. Single-injection adductor canal block with multiple adjuvants provides equivalent analgesia when compared with continuous adductor canal blockade for primary total knee arthroplasty: a double-blinded, randomized, controlled, equivalency trial. J Arthroplasty. 2018;33(10):3160–6. e1.
- Kim DH, Lin Y, Goytizolo EA, et al. Adductor canal block versus femoral nerve block for total knee arthroplasty: a prospective, randomized, controlled trial. Anesthesiology. 2014;120(3):540–550.
- McLeod GA, Burke D. Levobupivacaine. Anaesthesia. 2001;56(4):331–341.
- Wall PDH, Sprowson AP, Parsons N, et al. Protocol for a single-centre randomised controlled trial of multimodal periarticular anaesthetic infiltration versus single-agent femoral nerve blockade as analgesia for total knee arthroplasty: perioperative Analgesia for Knee Arthroplasty (PAKA). BMJ Open. 2015;5(12):e009898.
- Kampitak W, Tanavalee A, Ngarmukos S, et al. Does adductor canal block have a synergistic effect with local infiltration analgesia for enhancing ambulation and improving analgesia after total knee arthroplasty? Knee Surg Relat Res. 2018;30(2):133.
- Goyal R, Mittal G, Yadav AK, et al. Adductor canal block for post-operative analgesia after simultaneous bilateral total knee replacement: a randomised controlled trial to study the effect of addition of dexmedetomidine to ropivacaine. Indian J Anaesth. 2017;61(11):903.
- Memary E, Mirkheshti A, Dabbagh A, et al. The effect of perineural administration of dexmedetomidine on narcotic consumption and pain intensity in patients undergoing femoral shaft fracture surgery; a randomized single-blind clinical trial. Chonnam Med J. 2017;53(2):127–132.
- Kang Z, Xie W, Xie W, et al. Comparison of neurotoxicity of dexmedetomidine as an adjuvant in brachial plexus block in rats of different age. Neurotoxicol Teratol. 2018;69:21–26.
- Ortiz-Gómez JR, Perepérez-Candel M, Vázquez-Torres JM, et al. Postoperative Analgesia for elective total knee arthroplasty under subarachnoid anesthesia with opioids: comparison between epidural, femoral block and adductor canal block techniques (with and without perineural adjuvants). A Prospective, randomized, clinical trial. Minerva Anestesiol. 2017;83(1):50–58.
- Harvey I, Barry K, Kirby S, et al. Factors affecting the range of movement of total knee arthroplasty. J Bone Joint Surg Br Volume. 1993;75(6):950–955.
- Ritter MA, Harty LD, Davis KE, et al. Predicting range of motion after total knee arthroplasty: clustering, log-linear regression, and regression tree analysis. JBJS Open Access. 2003;85(7):1278–1285.
- Mistry JB, Elmallah RD, Bhave A, et al. Rehabilitative guidelines after total knee arthroplasty: a review. J Knee Surg. 2016;29(3):201–217.