ABSTRACT
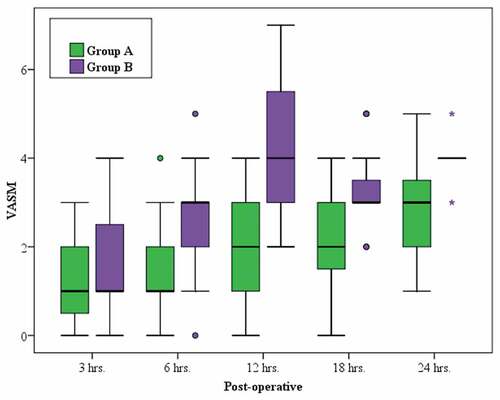
Background: Anaesthesia for patients with peripheral vascular disorders carries special challenges for the anaesthetist. The current study assessed the efficacy of pain management with bilateral quadratus lumborum block versus epidural morphine in patients undergoing aortobifemoral bypass under general anaesthesia.Settings and Design: Prospective randomized controlled trial.Methods: This work enrolled 30 patients undergoing aortobifemoral bypass under general anaesthesia. Patients were randomized into two groups. Group A received bilateral quadratus lumborum block using 20 ml 0.25% bupivacaine on each side and group B were given 4 mg morphine in 20 ml saline solution in an epidural catheter before induction of anaesthesia. Vital signs were recorded. Both rest and movement visual analogue scale (VASR and VASM respectively) were recorded postoperatively at 3, 6, 12, 18 and 24 hours. Postoperative total dose of rescue analgesic Nalbuphine and timing of first analgesic request were recorded. NO and IL-6 were assessed preoperatively and 6 hours postoperatively. Patient satisfaction was recorded at the end of study.Results: No significant difference in pain intensity through the initial six postoperative hours. VASR was significantly lesser in group A at 6th, 12th and 18th hours postoperatively (p = 0.015, <0.001 and <0.001 respectively), and 6th, 12th, 18th and 24th postoperative hours with VASM (p = 0.029, <0.001, 0.015 and 0.010 respectively). In group A the total dose of rescue analgesic was significantly less (p = 0.015) and time of first analgesic request was significantly earlier in group B (p = 0.042). NO and IL-6 levels were significantly lesser in group A at 6 hours postoperative (p = 0.014 and 0.021 respectively). Patient satisfaction was statistically better in group A (p = 0.028).Conclusion: Bilateral quadratus lumborum block may be more beneficial than epidural morphine for postoperative analgesia in patients undergoing aortobifemoral bypass surgery.
1. Introduction
Aorto-bifemoral surgery is conducted to bypass the blocked segment of the iliac arteries employing a synthetic graft [Citation1]. For many years, anaesthesiologists have debated whether regional is better than general anaesthesia for patients undergoing peripheral vascular operations. Though regional anaesthesia is not a panacea saving all our patients, it seems to offer some advantages over general anaesthesia. The decrease in the incidence of peripheral vascular graft thrombosis was demonstrated to be related to regional anaesthesia usage. The likely underlying mechanism involves fibrinolysis [Citation2].
Anaesthetic techniques for aorto-bifemoral bypass focus on reducing overall mortality and morbidity in a patient population with a great probability of comorbidities. Post-operative thrombotic events and cardiac morbidity can be minimized by regional anaesthesia. Also, effective postoperative analgesia can be maintained. Nevertheless, general anaesthesia sometimes may be essential in case of contraindications to regional anaesthesia as a substitute of similar morbidity and mortality. Moreover, peripheral nerve blocks can be relied upon cases with minimal cardiovascular function interference [Citation3,Citation4].
The use of epidural opioids such as morphine has gained greater popularity within the last years. Factors such as intense analgesic effect both with prolonged action along with great haemodynamic stability, contributed to their wide use for both intra and postoperative analgesia [Citation4].
Postoperative pain management depends on conventional drugs or a combination of peripheral nerve block and pain-escape medication (comprising: Paracetamol maximal dosing, non-steroidal anti-inflammatory drugs and oral or IV opioids). Yet, adverse effects, such as hypotension, nausea, decreased lung capacity, increased cardiac load and sedation are associated. All these hinder rehabilitation and timely discharge [Citation5]. This highlights the role of peripheral nerve block as a control of postoperative pain.
Ensuring the ideal dispersal of local anaesthetic around nerve structures is essential for successful regional anaesthetic blocks. This aim is attained effectively under direct sonographic visualization which generally ameliorates the result of most peripheral regional anaesthesia techniques. High resolution sonography allows anaesthetists to precisely visualize significant nerve structures at all levels for lower and upper limb nerve blocks. This improves nerve block quality and circumvents complications. Moreover, direct visualization of target nerve structures and tracking the spread of local anaesthetic permit the reposition of the needle in case of faulty distribution [Citation6].
Blanco was the first to present the quadratus lumborum (QL) block [Citation7]. Presently, it is used for perioperative pain management in different generations (paediatrics, pregnant, and adult) undergoing abdominal surgeries. Four techniques were described for QL block; anterior, lateral, posterior and intramuscular [Citation8].
Patients commonly show signs of acute phase response due to surgical stress such as anorexia, increased metabolic rate, nitrogen loss and hyperglycaemia. These changes are associated with cytokines induction such as IL-1, IL-6 and TNF. Systemic cytokine response is linked to the extent of the surgical stress. Cytokines and endotoxins were shown to have both a stimulatory and an inhibitory effect on Nitric Oxide (NO) release. NO is closely bound to infection, stress and immune system activities. Therefore, it was hypothesized that it is under regulation of surgical stress [Citation9,Citation10].
The primary aim of the current study was to assess the efficacy of pain management with bilateral quadratus lumborum block versus epidural morphine in patients undergoing aortobifemoral bypass under general anaesthesia, and the secondary aim was to assess the incidence of side effects.
2. Patients and methods
Agreement of the Ethics Committee of the Faculty of Medicine (IRB-NO: 00012098 -FWA-NO: 00018699) and a written informed consent from all the patients were obtained. Our study was carried out in vascular unit at Main University Hospital, Alexandria, on 30 adult male and female patients with ages between 40 and 80 years, American Society of Anaesthesiologists (ASA) physical status II–III, undergoing aortobifemoral bypass utilizing a synthetic graft. The study was carried out between February 2020 and July 2021.
The sample size was determined using (PASS program version 20) [Citation11].
Patients were randomized into 2 groups, (15 each), using sealed envelope in a single blinded manner where patients did not know in which group they were enrolled. Group A patients received general anaesthesia after bilateral quadratus lumborum block while Group B patients were given general anaesthesia after epidural analgesia.
The exclusion criteria in this study were: patient refusal, BMI > 40 kg/m2, severe renal impairment (Chronic kidney disease stage III or IV) or severe hepatic impairment, chronic pain or preoperative long-term opioid treatment, cognitive defect that may interfere with informed consent or data collection as decided by the investigator, severe abnormality of haemostasis (platelets < 80,000/ml) and/or of coagulation (Prothrombin activity PA <50%), diabetic neuropathy and allergy to one of the following drugs; Bupivacaine – Nalbuphine – Ketorolac – Fentanyl – Morphine.
Patient evaluation covering history taking, clinical examination, routine and required laboratory investigations, thorough cardiac and pulmonary medicine assessment was carried out on the day before surgery.
All patients were trained to use the visual analogue scale (VAS) consisting of a 10 cm measure, 0 cm denoting no pain and 10 cm denoting the worst sensation imaginable [Citation12].
On arrival to the operative theatre a peripheral venous catheter was inserted in all patients, Multichannel CARESCAPE™ Monitor B650 was attached to the patient to display ECG (lead II), mean arterial pressure (mmHg), heart rate (beats/min) using invasive left radial artery catheter after performing modified Allen’s test and peripheral oxygen saturation (SpO2). All patients received premedication with Midazolam (0.02 mg/kg) intravenously and 10 ml/kg of physiological solution was administered intravenously to all patients before the performance of the blocks.
In the 15 patients randomized to group A; before induction of general anaesthesia patients were turned to lateral decubitus with the side upwards for the block. After skin disinfection and covering of the puncture site with sterile drapes, a curved array transducer (2–6 MHz Mindray DP-50) was installed immediately in the transverse plane on the abdominal flank cranial to the iliac crest [Citation13].
The transducer was dorsally directed to keep transverse orientation until the QL muscle was recognized with its attachment to the lateral edge of the L4 vertebral body’s transverse process. A well identifiable pattern of a “shamrock with three leaves” could be seen with the psoas major muscle (PM), the erector spinae muscle (ESM) anteriorly and posteriorly and the QL muscle adhering to the transverse process [Citation14,Citation15].
The needle was inserted in an anteromedial direction in the plane from the posterior edge of the convex probe traversing the QL muscle [Citation15]. The needle tip was placed between the PM muscle and the QL muscle then the local anaesthetic was injected into the fascial plane between the QL muscle and the PM muscle (20 ml bupivacaine 0.25% for each side) [Citation16].
In the 15 patients randomized to group B; an epidural catheter was placed at T12-L1 interspace and morphine 4 mg in 20 ml saline solution was given before general anaesthesia. Anaesthesia was induced, in the two groups, using Fentanyl (1 µg/kg), Propofol (2 mg/kg), and Rocuronium (0.6 mg/kg). A suitable endotracheal tube (ETT) was placed. Anaesthesia was maintained with Isoflurane (1–2% in 100% oxygen) [Citation17]. Controlled ventilation was kept at a rate of 10 breath/min, and a tidal volume to maintain the end-tidal carbon dioxide at 35–40 mmH).
Conventional fluid management protocol was used for all patients. Intraoperative blood volume was replaced using ringer acetate solution, plasma substitutes and blood products as required [Citation17].
Reversal of residual muscle relaxation was done at the end of the operation with Atropine and Neostigmine (0.015 mg/kg and 0.04 mg/kg respectively).
Postoperative analgesia with 30 mg intravenous Ketorolac every 6 hours was given for both groups. Nalbuphine (4 mg) aliquots was given in case of a VAS ≥ 4 as rescue analgesia.
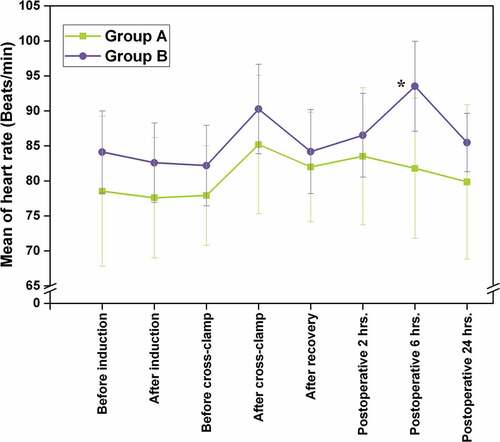
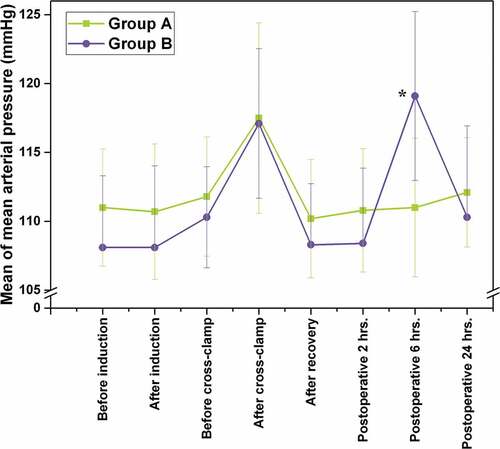
Vital signs including; HR and MABP were recorded at the following timings: before and after induction of GA, before and after aortic cross clamp, before and after declamping the aorta, after recovery and 2,6,24 hours postoperatively.
All patients peripheral blood samples (3 ml) were collected preoperatively and 6 hours postoperatively in EDTA tubes on ice and plasma was isolated for measuring [Citation18]; Plasma Nitric oxide (NO) in “μmol/l”, Interleukin-6 (IL-6) in “pg/ml”.
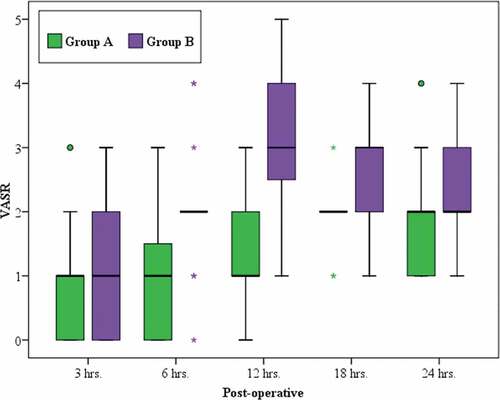
For pain assessment, VASR and VASM were recorded at 3, 6, 12, 18 and 24 hours postoperatively [Citation12].
Total dose of postoperative rescue analgesia (mg) consumed by the end of the 24 hours of study as well as time of first analgesic request (hours) were also determined.
No attempt was made to wake patients during sleep, and this was considered a period of pain relief. When a patient’s severe pain and refusal hindered recording VAS, it was scored 10.
Assessment of patient satisfaction was done using a four-point scale as [Citation19]: 1. Excellent, 2. Good, 3. Fair and 4. Poor, recorded once at the end of the 24 postoperative hours constituting the study period.
3. Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp). The Kolmogorov- Smirnov was used to verify the normality of distribution of variables; Comparisons between groups for categorical variables were assessed using Chi-square test (Fisher or Monte Carlo). Student t-test was used to compare two groups for normally distributed quantitative variables. Mann Whitney test was used to compare between two groups for not normally distributed quantitative variables. Paired t-test was assessed for comparison between two periods for normally distributed quantitative variables, Wilcoxon signed ranks test was assessed for comparison between two periods for abnormally distributed quantitative variables. Significance of the obtained results was judged at the 5% level.
4. Results
Thirty-five subjects were assessed for eligibility to participate in this study, 30 patients were enrolled in the study, with 5 patients excluded for not meeting the inclusion criteria and no dropouts along the course of the study. A total of 30 participants completed the 24 hours of study period ().
The studied groups were perfectly matched regarding; age, sex, BMI and surgery duration ().
Table 1. Comparison between the two studied groups according to demographic data
There was a significant increase in both mean heart rate value (p = 0.001) and MAP mean value (p < 0.001) at 6 hrs. Postoperative in group B in comparison to group A ().
There was no significant difference in pain intensity through the first 6 postoperative hours. VASR was significantly lesser in the group A at the 6th, 12th and 18th hours postoperative (p = 0.015, <0.001 and <0.001 respectively) (), and at 6th, 12th, 18th and 24th hours postoperative with VASM (p = 0.029, <0.001, 0.015 and 0.010 respectively) ().
Total dose of rescue analgesic was significantly lower in group A (p = 0.015) and the time of first analgesic request was statistically earlier in group B (p = 0.042). Also, the number of patients who needed rescue analgesic in group A is only 4 which is significantly lower than group B (n = 12) ().
Table 2. The total dose of nalbuphine rescue analgesia (mg) and the time of first analgesic request (hours) in the two groups
NO and IL-6 levels were significantly lower in group A at 6 hours postoperative (p = 0.014 and 0.021 respectively) ().
Table 3. Nitric oxide level (μmol/l) in the two studied groups
Table 4. IL-6 (pg/ml) in the two studied groups
Regarding side effects, only postoperative nausea and vomiting (PONV) was significantly higher in group B than group A (p = 0.035), all cases responded to conventional management of PONV. All other side effects were not significant ().
Table 5. Comparison between the two studied groups according to postoperative complications
Patient satisfaction scoring was significantly better in group A (p = 0.028) ().
Table 6. Comparison between the two groups according to patient’s satisfaction
5. Discussion
Our results show a greater decrease in pain intensity in patients who received ultrasound guided bilateral QL block, than in patients who were given epidural morphine before induction of GA, with more patient satisfaction and less analgesic intake.
Administration of QL block resulted in lower pain scores starting from 6 hours postoperatively compared to the other group and lasting for the 24 hours of the study period.
Since Blanco first described the QL block in 2007 [Citation7] there is scanty of randomized controlled trials applying the block for different surgical procedures. Krohg A et al. [Citation20] and Mieszkowski MM et al. [Citation21] described the use of QL block for pain management after caesarean section and stated that it resulted in lower 24- and 48-hours opioid consumption by patients respectively. Two other randomized controlled trials by Blanco et al. [Citation22,Citation23] demonstrated an opioid sparing effect after application of QL block for patients undergoing caesarean section. Ishio J et al. [Citation24] described the beneficial effect and lower analgesic requirements after posterior QL block for patients undergoing laparoscopic gynaecological procedures.
QL block was believed to cause prolonged analgesia only for superficial surgeries till the year 2013 when two case studies were published; one by Kadam VR [Citation14] for post-operative analgesia for a laparotomy case, and another case for closure colostomy published by Visoiu M et al. [Citation25]. Two further case reports were published in 2015 by Shaaban M et al. [Citation26] for proctosigmoidectomy and in 2016 by Elsharkawy H et al. [Citation27] for a case of colectomy.
Results demonstrated a statistically significant increase in IL-6 and NO levels in group B compared to group A at the 6th postoperative hour which indicates the efficacy of QL block over epidural morphine in late postoperative times. These results are consistent with the study conducted by Yun SH et al [Citation28] who tested postoperative serum levels of IL-6 in patients underwent total knee replacement, they demonstrated significantly lower levels in patients who received dexmedetomidine in comparison to the control group.
All previous studies and case reports demonstrated the superiority of QL block for post-operative analgesia and lower opioid usage with all its side effects, on contrary; Irwin R. et al [Citation29] in there 2020 published study concluded that parturient receiving bilateral QL block after caesarean section did not show any reduction in 24 hour morphine consumption by PCA versus those who received sham block.
Although epidural morphine shows marvellous results for post-operative analgesia in plenty of published studies and an effect lasting 24 to 48 hours in some literature like Duale C et al. [Citation30] and Meng ZT et al. [Citation31], this was not the condition in our study in which the analgesic effect lasted only for 6 hours postoperatively. This can be explained by the nature of the surgery which includes three incisions; one midline and two groin incisions, also the ischaemic component of pain which is frequently encountered in patients with peripheral vascular disease.
6. Conclusion
Bilateral quadratus lumborum block may be more beneficial than epidural morphine for postoperative analgesia in patients undergoing aortobifemoral bypass surgery.
7. Limitations
This study was limited by its short duration, difficulty in follow-up of patients and small sample size.
Acknowledgments
The authors are thankful to the Anaesthesia and Surgical Intensive Care Department and Vascular Surgery Unit, Faculty of Medicine, Alexandria University.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Aboyans V, Lacroix P, Criqui MH. Large and small vessels atherosclerosis: similarities and differences. Prog Cardiovasc Dis. 2007;50(2):112–125.
- Gelman S. General versus regional anaesthesia for peripheral vascular surgery. Is the problem solved? Anesthesiology. 1993;79(3):415–418.
- Duncan A, Pichel A. Anaesthesia for elective open abdominal aortic surgery. Anaesth & Int Care Med. 2016;17(5):238–242.
- Agarwal K, Sharma M, Agarwal N, et al. Comparative study of single dose epidural morphine and intermittent dose morphine with bupivacaine in post cesarean Analgesia. NJOG. 2012;7(3):41–44.
- Simonsen OH, Gorst-Rasmussen A, Simonsen AB, et al. Blood reinfusion combined with femoral nerve block in total knee replacement for patients with increased risk of bleeding. Hong Kong, J Orthop Surg. 2011;19(1):64–68.
- Marhofer P, Greher M, Kapral S. Ultrasound guidance in regional anaesthesia. Br J Anaesth. 2005;94(1):7–17.
- Blanco R. Tap block under ultrasound guidance: the description of a “no pops” technique: 271. Reg Anesth Pain Med. 2007;32(5):130.
- Ueshima H, Otake H, Lin JA. Ultrasound-Guided Quadratus Lumborum block: an updated review of anatomy and techniques. BioMed Res Int. 2017;2017:2752876.
- Satoi S, Kamiyama Y, Kitade H, et al. Prolonged decreases in plasma nitrate levels at early postoperative phase after hepato-pancreato-biliary surgery. J Lab Clin Med. 1998;131(3):236–242.
- Claudia S. Serotonin in pain and analgesia. Mol Neurobiol. 2004;30(2):117–125.
- Rockemann MG, Seeling W, Brinkmann A, et al. Analgesic and hemodynamic effects of epidural clonidine, clonidine/ morphine,and morphine after pancreatic surgery–a double-blind study. Anesthesia Analg. 1995 May 1;80(5):869–874.
- Breivik H, Borchgrevink PC, Allen SM, et al. Assessment of pain. Br J Anaesth. 2008;101(1):17–24.
- Elsharkawy H. Ultrasound-Guided quadratus lumborum block: how do i do it?. ASRA News. 2015;15(4):34–40.
- Kadam VR. Ultrasound-guided quadratus lumborum block as a postoperative analgesic technique for laparotomy. J Anaesthesiol Clin Pharmacol. 2013;29(4): 550–552. 10.4103/0970-9185.119148.
- Sandeep S, Suri A, Sindwani G, et al. Bilateral quadratus lumborum block for postoperative analgesia in a von Hippel-Lindau syndrome patient undergoing laparoscopic radical nephrectomy. Saudi J Anaesth. 2017;11(4):513–514.
- Putzu M, Gambaretti E, Rizzo F, et al. Postoperative analgesia for laparotomic surgery provided by bilateral single shot quadratus lumborum block. Minerva Anestesiol. 2018;84(10):1231–1232.
- Bardia A, Sood A, Mahmood F, et al. Combined Epidural-General anaesthesia vs general anaesthesia alone for elective abdominal aortic aneurysm repair. JAMA Surg. 2016;151(12):1116–1123.
- Kelm M. Nitric oxide metabolism and breakdown. Biochim et Biophy Acta. 1999;1411(1):273–289.
- Pitimana-aree S, Visalyaputra S, Komoltri C, et al. An economic evaluation of bupivacaine plus fentanyl versus ropivacaine alone for patient-controlled epidural analgesia after total-knee replacement procedure: a double-blinded randomized study. Reg Anesth Pain Med. 2005;30(5):446–451.
- Krohg A, Ullensvang K, Rosseland LA, et al. The analgesic effect of ultrasound-guided quadratus lumborum block after cesarean delivery: a randomized clinical trial. Anesth Analg. 2018;126(2):559–565.
- Mieszkowski MM, Mayzner-Zawadzka E, Tuyakov B, et al. Evaluation of the effectiveness of the quadratus lumborum block type I using ropivacaine in postoperative analgesia after a cesarean section: a controlled clinical study. Ginekol Pol. 2018;89(2):89–96.
- Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after caesarean section: a randomised controlled trial. Eur J Anaesthesiol. 2015;32(11):812–818.
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762.
- Ishio J, Komasawa N, Kido H, et al. Evaluation of ultrasound-guided posterior quadratus lumborum block for postoperative analgesia after laparoscopic gynecologic surgery. J Clin Anesth. 2017;41:1–4.
- Visoiu M, Yakovleva N. Continuous postoperative analgesia via quadratus lumborum block: an alternative to transversus abdominis plane block. Paediatr Anaesth. 2013;23:959–961.
- Shaaban M, Esa WA, Maheshwari K, et al. Bilateral continuous quadratus lumborum block for acute postoperative abdominal pain as a rescue after opioid-induced respiratory depression. A A Case Rep. 2015;5(7):107–111.
- Elsharkawy H, Salmasi V, Soliman LM, et al. Anterior quadratus lumborum block versus transversus abdominis plane block with liposomal bupivacaine: a case report. J Anesth Crit Care Open Access. 2016;6:1–5.
- Yun SH, Park JC, Kim SR, et al. Effects of dexmedetomidine on serum interleukin-6, hemodynamic stability, and postoperative pain relief in elderly patients under spinal anesthesia. Acta Med Okayama. 2016;70(1):37–43.
- Irwin R, Stanescu S, Buzaianu C, et al. Quadratus lumborum block for analgesia after caesarean section: a randomised controlled trial. Anaesthesia. 2020;75(1):89–95.
- Duale C, Frey C, Bolandard F, et al. Epidural versus intrathecal morphine for postoperative analgesia after Caesarean section. Br J Anaesth. 2003;91(5):690–694.
- Meng ZT, Cui F, Li XY, et al. Epidural morphine improves postoperative analgesia in patients after total knee arthroplasty: a randomized controlled trial. PloS One. 2019;14(7):e0219116.