ABSTRACT
Background
Formerly management of malignant tumors of lower limb was mainly through amputation. After advancement in neoadjuvant chemo-radiotherapy, saving the limb through lower limb-sparing surgery became the main line for management. Different regional techniques are used for perioperative pain control in limb-sparing surgeries. One of these techniques is lumbar paravertebral block. It is a regional technique that provides ipsilateral analgesia resulting in somatic and sympathetic blockade in a continuous dermatomal manner.
Methods
The study included 60 cancer patients scheduled for lower limb sparing surgeries. Patients were randomly allocated into two groups to receive either lumbar paravertebral block Group P with 25 ml of Bupivacaine 0.25%, with adrenaline 1:200,000 or general anesthesia Group C.
Results
There was a statistically significant decrease in hemodynamics values for Group P compared to Group C at most of the study times. Intraoperative fentanyl consumption was lower in Group P compared to Group C (107.1 ± 22.89 ug versus 233.43 ± 49.29 ug), respectively. VAS scores were lower for Group P compared to Group C with lower postoperative morphine consumption in Group P compared to Group C (8.65 ± 3.57 mg versus 16 ± 3.15 mg) respectively.
Conclusion
Ultrasound guided paravertebral block can be used as an effective perioperative analgesic modality for cancer patients undergoing lower limb sparing surgeries.
1. Introduction
Malignant tumors of bone and soft tissue of lower extremities was previously managed mainly by amputation. With advancement of chemotherapeutic agents and radiotherapy, saving the limb through lower limb-sparing surgery (LLSS) is currently the first line for management [Citation1]. Lower limb surgeries carry high risk of perioperative pain secondary to skeletal tissue injury and reconstruction, that results in pain with nociceptive and neuropathic elements [Citation2]. Early proper control of perioperative pain helps in early patient mobilization with shorter length of hospitalization and increase in patient satisfaction [Citation3]. Opioids are considered the gold standard analgesic for postoperative pain control, however using opioids is associated with multiple side effects that may include nausea, vomiting, constipation, and hypoventilation up to respiratory depression [Citation4].
Using pre-emptive multimodal analgesic modalities would provide better pain control with reduced opioid consumption [Citation5]. Preemptive analgesia is achieved through administrating analgesic drugs or techniques before initiation of the noxious stimuli; it modifies processing of the peripheral and central nervous system response to noxious stimuli, thus reducing postoperative opioid consumption [Citation6]. Multimodal analgesia is achieved through combining different analgesic drugs or techniques with different mechanism of actions, leading to augmented analgesic effect with lesser side effects [Citation7].
Regional blocks are commonly used as part of multimodal analgesia; they exert their action through inhibiting conduction of neural impulses from surgical site to the spinal cord thus decreasing spinal cord sensitization [Citation7,Citation8]. Using regional anesthesia provides better perioperative pain control with attenuation of stress response and reduction of opioids consumption [Citation9]. Various regional anesthetic techniques are commonly used for perioperative pain management in limb-sparing surgeries [Citation10]. One of these techniques is ultrasound guided lumbar paravertebral block (LBVP). The lumbar paravertebral space is bounded medially by the vertebrae, intervertebral disc and intervertebral foramina which connect the space with the epidural space; anterolaterally by psoas major muscle and posteriorly by the transverse process. LPVB is a regional anesthetic technique that involves more precise injection of local anesthetics in close proximity to spinal nerve roots in the paravertebral space, thus increase the efficacy and safety of performed nerve block [Citation11]. This study aims to evaluate the efficacy of unilateral ultrasound guided paravertebral block for perioperative analgesia of lower limb-sparing surgery in adult cancer patients and its effect on decreasing perioperative opioids consumption.
2. Materials and methods
This parallel prospective double blinded randomize controlled study was conducted at National Cancer Institute – Cairo University from January 2020 to May 2020. The study protocol was approved by the Anesthesia department scientific and ethical committees at Al Kasr Al Ainy, Cairo University (MS-270-2019) and registered at Clinical Trials.gov (NCT04396561). Consolidated Standards of Reporting Trials (CONSORT) guidelines were followed during preparation of this study [Citation12].
Eligibility criteria included adult cancer patients aged 18–65, ASA II and III, with BMI > 20 kg/m2 and < 40 kg/m2 scheduled for lower limb sparing surgeries involving the anterolateral thigh under general anesthesia. Exclusion criteria included patient refusal, allergy to local anesthesia, coagulation defects, abnormal kidney and liver functions and history of psychological disorders and/or chronic pain. Patients meeting eligibility criteria were consecutively recruited from preoperative anesthesia assessment clinic. All patients were informed about the study design and objectives as well as tools and technique but were blinded to which group, they will be assigned. Informed written consent had been signed by every patient prior to the study. Patients were randomly allocated in 1:1 ratio with a computer-generated list (www.Random.org) done by statistician, then allocated by an anesthetist in the holding area using sealed opaque envelope method into one of the two studied groups 30 patient in each group to receive either unilateral paravertebral block (Group P) or general anesthesia (Group C).
In the holding area, patients were monitored for pulse, blood pressure, oxygen saturation (baseline values). Patients received Midazolam 0.02 mg/kg after insertion of intravenous (IV) 18-gauge cannula. General anesthesia was induced for both groups using a regimen of IV propofol 2 mg /kg, fentanyl 1 μg/kg and rocuronium 0.5 mg/kg. Patients were mechanically ventilated using volume-controlled ventilation mode. Tidal volume and respiratory rate were adjusted to maintain end-tidal CO2 between 35 and 40 mmHg. Anesthesia was maintained with inhaled sevoflurane with MAC 2–2.5% in oxygen-enriched air (FiO2 = 50%) and rocuronium. All patients received 1 gm of IV paracetamol, ketorolac 30 mg IV infusion. Patients were continuously monitored using pulse oximeter (SpO2), electrocardiogram (ECG), noninvasive blood pressure (NIBP), and end-tidal CO2 (ETCO2).
Group C: received only general anesthesia
Group P: after induction of general anesthesia patients were positioned in lateral decubitus position with the operating side up. After sterilization and draping, ultrasound scanning was done using SonoSite M-Turbo ultrasound machine (FUGIFILM Sonosite, Inc.Bothel, WA 98021, USA) with a low frequency curved 2–5 MHz transducer. Lumbar paravertebral region was obtained after positioning the probe 3–4 cm lateral and parallel to the lumbar spinous process. The probe was then moved downward, till reaching the L5 hyperechoic transverse process and the sacrum. After identifying of the L5 transverse process, L4,3,2 transverse processes were identified by counting from downward to upward. The “trident sign” was identified by the ultrasound. It presents the acoustic shadow of the transverse processes. The psoas muscle was localized by being in the space between the transverse processes‟ shadow. Nerves of the lumbar plexus were identified as the longitudinal hyperechoic structures seen on the posterior aspect of the psoas major muscle. Then Insulated nerve block needle 21-gauge, 10 cm (Stimuplex, B. Braun, Melsungen AG, Germany) was inserted using an in-plane technique from the caudal end of the ultrasound probe. The needle was advanced through the acoustic shadow between the transverse process of L3 and L4 to reach the posterior aspect of the psoas major muscle. Nerve stimulator, initially delivering a current of 1.5 mA at a frequency of 2 Hz was connected to the needle to confirm position and exclude intraneural injection. Upon entry of the needle to the posterior aspect of the psoas major, confirmation of proper needle position was indicated by ipsilateral contraction of the quadriceps muscle at 0.5−1 mA current denoting close proximity of the needle tip to the lumbar plexus. After negative aspiration, the local anesthetic (25 mL of bupivacaine 0.25% in addition to 1:200,000 adrenaline) was injected slowly and patients were closely monitored for any signs of inadvertent intravenous injection ().
In both groups, one reading of mean arterial pressure and heart rate were taken before induction of general anesthesia and were defined as baseline readings and then were recorded intraoperatively at 15-min intervals. Additional bolus doses of fentanyl 0.5 μg/kg were given when the mean arterial blood pressure or heart rate rose above 20% of baseline levels. Hypotension, which was diagnosed with drop of blood pressure more than 20% of baseline reading, was treated with 0.9% normal saline and/or 5 mg ephedrine in incremental doses in order to maintain mean blood pressure above 70 mmHg. Ringer acetate was infused in order to replace their fluid deficit, maintenance, and losses. Extubation was performed at the end of surgery after reversing of residual neuromuscular block and complete recovery of airway reflexes. Patients were transferred to the post anesthesia care unit (PACU) room then to the ward. Heart rate, mean arterial blood pressure and VAS scores were recorded on arrival to PACU and at 2, 4, 6, 12, 18, and 24 h postoperatively. In the first 24 hours postoperatively, all patients received multimodal analgesia using paracetamol 1 gm IV every 8 hours, ketorolac 30 mg was given, in addition to a bolus of 3 mg morphine if VAS ≥ 4. The total amount of morphine given in 24 h was recorded in the two groups. Patients in Group P were observed for any complications as hematoma, accidental nerve injury, inadvertent epidural injection and paravertebral muscle spasm. Side effects such as nausea, vomiting, hypotension, or bradycardia were recorded.
Our primary outcome was to calculate total intraoperative fentanyl consumption for both groups. Secondary outcomes were to measure total postoperative morphine consumption in first 24 h, assessing VAS score in first 24 hour postoperatively in addition to comparing hemodynamic values between the two groups.
3. Sample size and statistical methods
Based on previous study by Borle and colleagues in 2014 [Citation13], intraoperative fentanyl consumption mean value (SD) was 2.07 (0.26) for PVB group versus 2.74 (0.75) for control group with an effect size of approximately 0.8 was expected. A total sample size of 52 (26 per group) will be sufficient, a power of 80%, and a significance level of 5%. This was the minimum sample size to be required. Sample size was calculated using G*Power program (University of Düsseldorf, Düsseldorf, Germany). Number of patients were increased to 30 per group to replace dropouts.
The statistical analysis was done by standard SPSS software package version 22 (SPSS, Chicago, IL, USA). Analysis of variance was used to test the difference between the two groups for quantitative parametric data. Post-hoc Tukey’s test was used when there was a significant difference between the 2 groups. Kruskal-Wallis test was performed for studying quantitative nonparametric data. Qualitative data was compared by using Chi square test. Data were presented in the form of mean± SD for continuous parametric data, median (IQR) for parametric data and number of patients for categorical data. P values were considered significant if < 0.05 and were considered highly significant if < 0.001.
4. Results
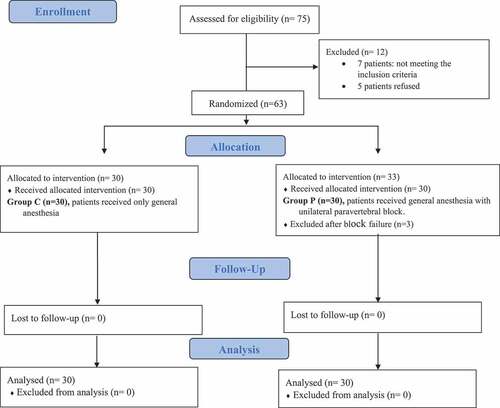
Seventy-five cancer patients scheduled for lower limb-sparing surgery under general anesthesia were consecutively recruited to the study. Five patients were excluded, 7 of them were not meeting the eligibility criteria and 5 patients refused to participate. Sixty-three patients were randomly allocated into one the 2 studied groups (). Both groups were comparable for their demographic data and procedure duration ().
Table 1. Demographic data in the two studied groups
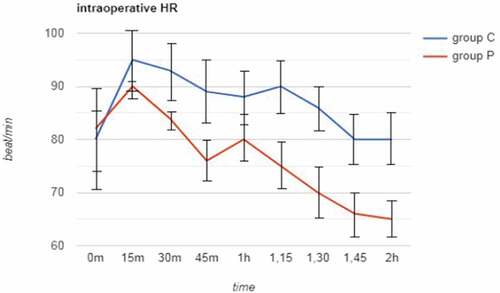
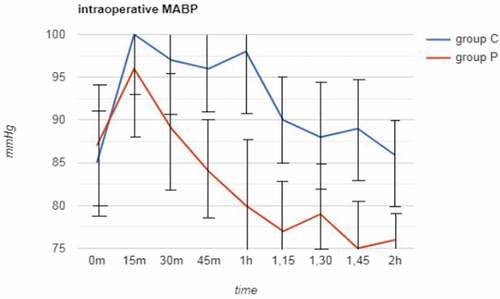
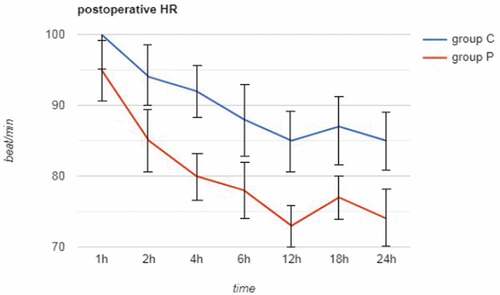
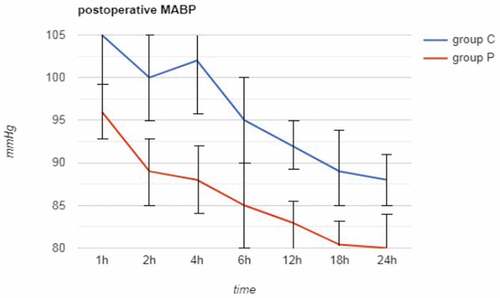
Total intraoperative fentanyl consumption was significantly lower in group P (107.1 ± 22.89 ug) compared to group C (233.43 ± 49.29 ug) (p < 0.05) (). There was a statistically significant decrease in intraoperative hemodynamics (HR and MAP) for (group P) compared to (group C) at all the predetermined study measurement points except for heart rate values at 0, 15 and 60 minutes and mean arterial blood pressure values at 0, 15, and 30 min (). Group P showed statistically significant lower heart rate and mean arterial blood pressure values though out the postoperative period except for heart rate values at 1 h and mean arterial blood pressure values at 1 and 6 h ().
Table 2. Intraoperative fentanyl consumption and postoperative morphine consumption in the two studied groups
There was a statistically significant decrease in VAS score values at all the predetermined measurement points for group P compared to group C (p < 0.05) (). Total postoperative morphine consumption was significantly lower in group P (8.65 ± 3.57 mg) compared to group C (16 ± 3.15 mg) (p < 0.05) (). The incidence of PONV showed statistically significant higher values for Group C 23% (seven patients) compared to group P 6.5% (two patients) (p < 0.05) ().
Table 3. VAS scores in the two studied groups in the first 24 h
Table 4. Number of patients (%) subjected to postoperative nausea and vomiting
5. Discussion
We demonstrated that ultrasound-guided lumbar paravertebral block in patients undergoing lower limb-sparing surgeries for cancer when used as a part of multimodal analgesia is associated with improved perioperative analgesia with reduced both intraoperative fentanyl consumption and total postoperative morphine consumption over 24 h period. Furthermore, VAS score values in the first 24 h postoperatively were significantly lower in paravertebral group compared to the control group.
The current study results came in accordance with the results of Stevens and colleagues who studied the efficacy of lumbar plexus block in reducing pain associated with total hip arthroplasty. They reported that lumbar paravertebral block reduces perioperative pain and both intra- and postoperative opioid consumption with significantly lower pain scores in the lumbar plexus block group patients undergoing total hip arthroplasty [Citation14]. These results are consistent with the results of Abdelhamid and colleagues who documented that ultrasound guided paravertebral block reduces perioperative opioid requirements with maintaining hemodynamic stability and can be used as a safe technique for efficient analgesia in patients undergoing hip surgeries [Citation15]. Furthermore, this was supported with the results of Ardon and colleagues who studied the efficacy of paravertebral blockade for analgesia in total hip arthroplasty surgeries, they reported that adding paravertebral block as a part of multimodal analgesia results in reduced VAS scores with less opioid consumption [Citation16]. In the same context, Utebey and colleagues compared lumbar plexus block to epidural block and general anesthesia and their effect on postoperative analgesia and total blood loss during total hip arthroplasty [Citation17]. They found that total morphine consumption in the first 24 h postoperatively was lower in patients who received lumbar paravertebral block than patients received epidural block and those who received only general anesthesia. They also documented that postoperative first VAS values were significantly higher in general anesthesia group compared to the lumbar paravertebral group and the epidural group. Similarly, in a study done by Hatipoglu and colleagues who compared ultrasound-guided paravertebral block to intravenous tramadol effect on postoperative pain management in percutaneous nephrolithotomy, they reported that the paravertebral group showed lower VAS scores with lower values of total postoperative opioid consumption and lower need for supplemental analgesia compared to the tramadol group [Citation18].
There was significant difference between both groups in hemodynamic values being lower in the lumbar paravertebral block group compared to the control group throughout most of measurement points during intra- and postoperative period. This can be explained by the analgesic effect of the block. These results were consistent with those found by Stevens and colleagues who reported that intraoperative MAP was lower in the lumbar plexus group during most of the procedure time [Citation14].
Concerning postoperative nausea and vomiting (PONV), we reported significantly less incidence of PONV in the lumbar paravertebral block group compared to the control group. This can be explained by the fewer doses of opioids needed with patients of paravertebral group. These results are coinciding with studies illustrating higher incidence of postoperative nausea and vomiting associated with opioid administration [Citation19,Citation20].
5.1. Conclusion
Unilateral paravertebral block as a part of multimodal analgesia effectively reduces perioperative pain and opioid consumption in cancer patients undergoing lower limb sparing surgeries.
Ethics approval and consent to participate
The study was conducted after approval of the Anesthesia department scientific and ethical committees at Al Kasr Al Ainy, Cairo University (MS-270-2019) and registered at Clinical Trials .gov (NCT04396561). The study was done after a written informed consent was taken from patients enrolled in the study.
Competing of interests
The authors declare that they have no competing interests.
Author’s contributions
YF: Contributed to study idea, patient recruitment, interpreted and analyzed the data, shared in writing the manuscript.
SA: Contributed to study idea, interpreted and analyzed the data, shared in writing the manuscript.
TK: Shared in interpreting, analyzing the data and in writing the manuscript.
AA: Initiated the study idea, shared in interpreting and analyzing the data, supervised the writing of the manuscript.
ES: Supervised the writing of the manuscript and data analyzation.
WE: Contributed to study idea, writing the manuscript, shared in the study design and in interpreting the data.
All authors read and approved the final manuscript.
Availability of data and materials
Data generated and analyzed during the current study are available on reasonable request.
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Anghelescu DL, Oakes LL, Hankins GM. Treatment of pain in children after limb-sparing surgery: an institution’s 26-year experience. Pain Manage Nurs. 2011;12:82–94.
- Marhofer P, Willschke H, Kettner S. Current concepts and future trends in ultrasound-guided regional anesthesia. Curr Opin Anaesthesiol. 2010;23:632–636.
- Finnerup NB, Jensen TS. Mechanisms of disease: mechanism-based classification of neuropathic pain - A critical analysis. Nat Clin Pract Neurol. 2006;2:107–115.
- Stein C, Kuchler S. Non-analgesic effects of opioids: peripheral opioid effects on inflammation and wound healing. Curr Pharm Des. 2012;18:6053–6069.
- Woolf CJ, Bennett GJ, Doherty M, et al. Towards a mechanism-based classification of pain? Pain. 1998;77:227–229.
- De JV, Gae D, Harsanyi Z, et al. Efficacy and safety of controlled-release oxycodone and standard therapies for postoperative pain after knee or hip replacement. Canadian Journal of Surgery. 2005;48:277–283.
- Kehlet H, Dahl JB. The value of ???multimodal??? or ???balanced analgesia??? in postoperative pain treatment. Anesthesia Analg. 1993 Nov;77(5):1048–1056.
- Joshi GP. Multimodal analgesia techniques and postoperative rehabilitation. Anesthesiology Clinics of North America. 2005;23(1): 185-202.
- Roberts S. Ultrasonographic guidance in pediatric regional anesthesia. Part 2: techniques. Pediatr Anesthesia. 2006 Jul;19:060720072529063.
- El-Boghdadly K, Madjdpour C, Chin KJ. Thoracic paravertebral blocks in abdominal surgery - A systematic review of randomized controlled trials. Br J Anaesth. 2016;117:297–308.
- Capdevila X, Coimbra C, Choquet O. Approaches to the lumbar plexus: success, risks, and outcome. Reg Anesth Pain Med. 2005;30:150–162.
- Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. 2011;9:672–677.
- Borle AP, Chhabra A, Subramaniam R, et al. Analgesic efficacy of paravertebral bupivacaine during percutaneous nephrolithotomy: an observer blinded, randomized controlled Trial. J Endourol. Internet]. 2014 Sep;28(9):1085–1090. Available from: http://www.liebertpub.com/doi/10.1089/end.2014.0179.
- Stevens RD, Van Gessel E, Flory N, et al. Lumbar plexus block reduces pain and blood loss associated with total hip arthroplasty. Anesthesiology. 2000;93:115–121.
- Abdelhamid BM, Belita MI, Mostafa Gomaa H, et al. Effect of ultrasound-guided L1/L2 paravertebral block in decreasing drug requirements during general anesthesia in patients undergoing hip surgeries; randomized controlled trial. Egypt J Anaesth. 2020;36(1):44–49.
- Ardon AE, Greengrass RA, Bhuria U, et al. the use of paravertebral blockade for analgesia after anterior-approach total hip arthroplasty. Middle East J Anaesthesiol. 2015;23:81–89.
- Ütebey G, Akkaya T, Alptekin A, et al. The effects of lumbar plexus block and epidural block on total blood loss and postoperative analgesia in total hip arthroplasty. Agri. 2009;21:62–68.
- Hatipoglu Z, Gulec E, Turktan M, et al. Comparative study of ultrasound-guided paravertebral block versus intravenous tramadol for postoperative pain control in percutaneous nephrolithotomy. BMC Anesthesiol. 2018;18(1):1-6.
- Roberts GW, Bekker TB, Carlsen HH, et al. Postoperative nausea and vomiting are strongly influenced by postoperative opioid use in dose-related a manner. Anesth Analg. 2005;101(5):1343–1348.
- Chandrakantan A, Glass PSA. Multimodal therapies for postoperative nausea and vomiting, and pain. Br J Anaesth. 2011;107(SUPPL. 1):27–40.