ABSTRACT
Background
Both intraoperative esmolol and transversus abdominis plane (TAP) block facilitate postoperative analgesia after laparoscopic cholecystectomy as part of multimodal analgesia. Both strategies can minimize the use of postoperative opioids. In current study, our goal was to assess if intra-operative esmolol infusion in association with TAP block can overcome the deficits of TAP block alone after laparoscopic cholecystectomy.
Methods
This prospective, randomized and double-blinded clinical trial included 60 patients of either sex who scheduled for elective laparoscopic cholecystectomy; received either ultrasound-guided TAP block alone or in association with intravenous esmolol bolus (0.5 mg/kg) before induction followed by a maintenance infusion (0.05 mg/kg/min) till the end of operation. Intra-operative hemodynamic parameters were followed up. Postoperatively, in order to maintain visual analogue scale (VAS) scores ≤3, patients received IV morphine. The primary outcome was amount of opioid consumption during the first 24 hours postoperative. Pain scores, mean arterial pressure (MAP), heart rate (HR) and occurrence of nausea/vomiting were secondary outcomes.
Results
The mean morphine consumption after surgery in patients receiving esmolol was (5.83) mg compared to (7.5) mg in TAP only group (p = 0.204). The mean pain scores at early postoperative hours were significantly lower in esmolol group (p < 0.05). MAP and HR were significantly lower in esmolol group intraoperative; however, no variance was detected later.
Conclusion
In the first 24 hours following surgery, esmolol infusion increased the analgesic impact of TAP block in terms of opioid demand and pain severity.
1. Introduction
Minimal access keyhole entry makes pain associated with laparoscopic cholecystectomy has been generally underestimated, despite of its association with significantly high postoperative pain scores especially in early period [Citation1]. Three origins of pain can be related to this type of surgery: parietal pain due to the surgical cut in the abdominal wall that is required for entrance of the surgical tools; deep visceral pain which is hard to localize and it is related to the trauma caused by surgical separation of the gall bladder; finally scapular pain, a referred pain due to irritation of the diaphragm by CO2-pneumoperitoneum [Citation2].
Using the traditional analgesics like opioids increases the risk of adverse effects such as nausea, vomiting and sedation which may irritate the patient and delay discharge from hospital. In past years, several approaches such as port site infiltration or intraperitoneal lavage with local anaesthetics have been successfully employed to reduce pain scores and opiate need. The transversus abdominis plane (TAP) block plays an important role in postoperative analgesia after abdominal surgery, Because of the sensory block over the anterior abdominal wall from T7 to L1 that can be created by deposition of local anaesthetics in the transversus abdominis fascial plane. TAP was found to have beneficial effects in a number of studies; however, the majority of the findings were connected to lower abdominal procedures [Citation3].
Several studies showed that β adrenergic receptor antagonists withhold the upsurge of catecholamines circulating in blood which induced by surgery, as well as having analgesic sparing effect itself [Citation4]. Esmolol is an ultrashort acting β1 blocking drug that has been uncovered to own opioid-sparing effects likely due to resemblances in its structure with local anesthetic agents. Esmolol’s short course of action and titrability offer it as an attractive drug to use, although the mechanism of action of its analgesic effect has yet to be established [Citation5].
Current study aimed to assess the effect of intraoperative esmolol infusion in addition to ultrasound guided TAP block to reduce pain and analgesic requirements postoperatively, and enhance patient recovery after laparoscopic cholecystectomy.
2. Material and methods
The study was designed as a prospective randomised controlled double-blind trial. The study’s protocol was accepted by Benha Faculty of Medicine’s ethical committee under the number (RC/3/12/2020). The trial was prospectively registered in the clinicaltrials.gov with the number (NCT04752111). After receiving the approval, the trial was conducted at Benha university hospital from January 2021 till June 2021 on 60 patients with ASA Grade I and II of both sex and the age range between 18 and 60 years undergoing laparoscopic cholecystectomy under general anaesthesia. At the same time, patients who rejected to join the study, ASA grade III or IV patients, presence of bleeding disorders,patients known to be allergic to one of the used drugs, body mass index (BMI) >35,patients with pulmonary, cardiac, renal or hepatic disorders,pregnancy or chronic drug abusers were excluded from the study. During the pre-anaesthetic clinic visit, eligible participants were identified. Then, an informed written consent was taken from the enrolled participants in the evening before the procedure. Patients were taught how to use the visual analogue scale (VAS), which ranges from 0 to 10, with 0 representing no pain and 10 being the most intense pain possible.
On the day of surgery, patients were randomly assigned to two groups (30 patients each) using a computer-generated random digit table. A set of closed opaque envelopes were used to hide the details of the group allocation and case number. Drugs were prepared by the anaesthesia staff that opened the envelope accordingly. The patient group assignments were known neither to the patient nor to the investigator who was responsible for collection of the required data. The first group was the Esmolol (E) group in which a loading and maintenance dose of esmolol was given to patients throughout the surgery in association with TAP block. The second group was TAP only (T) group in which patients received a loading and maintenance dose of isotonic saline throughout the surgery in association with the TAP block.
When patient arrived to the operating room, an intravenous (IV) line was established, and standard monitoring equipment including pulse oximetry, non-invasive blood pressure cuff, and electrocardiography electrodes were used. Before induction of anaesthesia by ten minutes, patients in group E received a loading dose of esmolol 0.5 mg/kg in 30 mL isotonic saline in the IV line, followed by an IV infusion of esmolol 0.05 mg/kg/min until the completion of surgery. Group T, on the other hand, got a loading dose of 30 mL isotonic saline in the IV line, followed by a 0.05 mg/kg/min IV infusion of saline until the completion of surgery. General anaesthesia was induced with fentanyl 1–2 mcg/kg and propofol 2–3 mg/kg followed by rocuronium 0.5–0.8 mg/kg for intubation. After general anaesthesia induction and before beginning the surgery, patients in both groups had a bilateral in-plane TAP block with 40 mL of bupivacaine 0.25%, 20 mL on each side guided by ultrasound.
2.1. Description of the technique
Following skin disinfection and covering of the ultrasound probe and cable with a sterile sheath, a broad linear array probe was placed transverse to the abdomen (horizontal plane) between the iliac crest and the costal margin in the mid-axillary line. Three muscle layers can be visualized in the image. A 20 Gauge 90 or 120 mm sharp ended spinal needle was used. The needle was introduced in a sagittal plane nearly 3–4 cm medial to the probe of ultrasound (in-plane technique). To follow the needle superficial course after skin puncture; the probe was moved slightly anterior, then gradually posteriorly to the mid-axillary line position until the needle settled in its right position in the TAP. A small volume of local anaesthetic (1 mL) was initially injected to open the plane then 20 mL of 0.25% bupivacaine was injected in each side. The local anaesthetic injectant appeared hypoechoic on ultrasound imaging. The surgery was started after completion of the block.
Maintenance of anaesthesia was accomplished with Isoflurane and rocuronium 0.15 mg/kg until the end of surgery. Ventilation parameters were adjusted to keep the tidal volume of 6–8 mL/kg and the end-tidal CO2 between 30 and 35 mmHg. Carbon dioxide is used to produce pneumoperitoneum and the intraabdominal pressure was maintained below 15 mmHg. Vital signs (HR and MAP) were recorded by the observer (at induction, at intubation and every 15 minutes till the end of surgery. Intra-operative hypotension (MAP < 60 mmHg) and bradycardia (HR < 50 beats/min) were treated with intravenous ephedrine 5 mg and 0.4 mg atropine, respectively. During the procedure, no additional opioid doses were administered.
Expelling the remained CO2 in the peritoneal cavity was done by decompression of abdomen slowly at the end of surgery. Discontinuation of isoflurane and the tested drug infusion was done after the last skin suture. Residual muscle relaxant was reversed with IV neostigmine (0.05 mg/kg) and atropine (0.01 mg/kg) followed by tracheal extubation once criteria of extubation were achieved. After emerging safely from anaesthesia, patients were moved to the post-anaesthesia care unit (PACU) for 2 hours observation period then moved to the ward with frequent follow up.
Postoperative pain management included oral acetaminophen 500 mg\6 h as a fixed-dose. Assessing VAS score for pain at rest and during movement was done by the blinded investigator in the PACU (on arrival, 1 h, 2 h) and in surgical ward (at 6 h, 12 h and 24 h). IV 5 mg morphine was given if VAS score exceeded 3. Furthermore, postoperative vital signs (HR and MAP) were observed every (0, 1, 2, 4 and 6 h) by a resident who was ignorant of the intraoperative anaesthesia plan.
Occurrence of any side effects like postoperative nausea and vomiting (PONV) were observed, Ondansetron 4 mg was available when required. Patient’s satisfaction was also evaluated depending on a 5-point Likert scale as follow: (1-very unsatisfied, 2-unsatisfied, 3-unsure, 4-satisfied, and 5-very satisfied).
The primary outcome in this trial was opioid (morphine) consumption during the first 24 hs following surgery. Measures of Secondary outcome included patient-reported VAS scores for pain at rest and during movement, intraoperative and postoperative vital signs (HR and MAP) changes, postoperative nausea and vomiting (PONV) and patient’s satisfaction.
2.2. Statistical analysis
Analysis of data was done by using SPSS version 25 (IBM, Armonk, New York, United states). Quantitative parametric data were presented as mean ± SD and were analyzed by unpaired t-test. Qualitative data were presented as percentage and numbers and were analyzed by Chi-square test. Statistical significance was defined as a p-value of less than 0.05.
2.3. Sample size
The sample size was estimated according to a study done by Bharti et al. 2011 [Citation3], based on the primary outcome (24-h morphine consumption). Assuming that there is a reduction in analgesic consumption 30% in group E using of a power of at least 80%, the two-sided α error of 5% level and the calculated effect size was 0.807. A sample size of 26 patients per group was obtained by G*Power software version 3.1.9.4 (Universitat Keil, Germany). Thirty patients were enrolled per group to minimize the effect of drop out.
3. Results
This study enlisted the participation of 60 patients (51 females and 9 males). There were no significant variations in the distribution of age, sex, BMI, ASA physical status, or duration of surgery (). There were no serious complications happened to any patient, and none of them were rolled out from the study ().
Table 1. Comparison of demographic and baseline characteristics of patients
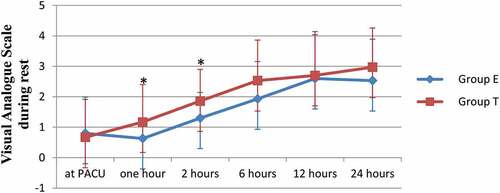
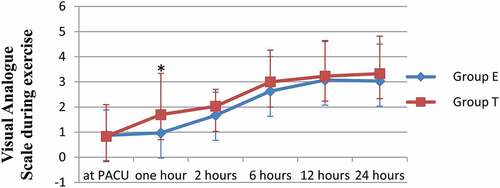
According to statistical analysis using t-test, there was a significant decrease in pain status during rest based on VAS criteria reported in group E during the early recovery phase exactly at the first and second hours following surgery (P = 0.038, P = 0.023, respectively, ; ). However, only VAS score at first hour during exercise was significantly lower in group E (P = 0.034, ; ). The VAS score at the remaining monitoring time points was generally lower in group E but not statistically significant. The amount of analgesic (morphine) given to the patients after surgery was lower in group E (5.83 ± 2.87 mg) than group T (7.5 ± 3.65 mg), but these values didn’t achieve the significant difference (P = 0.204). Furthermore, the average time to provide the first analgesic dose was longer in group E (12.91 ± 6.16) hours when compared to group T (9.13 ± 6.69) but they showed no significant difference (P = 0.148) ().
Table 2. Comparison between both groups as regard visual analogue scale at rest during 24 hours postoperative
Table 3. Comparison between both groups as regard visual analogue scale on movement during 24 hours postoperative
Table 4. Comparison between both groups regarding total pain rescue-analgesia consumption during 24 hours (mg/24 h) and time of first dose
At various time points, both groups were compared in terms of heart rate and mean blood pressure. When compared to group T, there was a statistically significant decrease in heart rate in group E after the bolus dose was administered. This decline continued throughout the operative period at all the measured time points (p < 0.001). However, in the postoperative period, both groups’ mean heart rate values were comparable (p > 0.05) (). Similar results were noted regarding MAP which was significantly lower in group E at various time-points during the surgery (p < 0.05) but, it didn’t accomplish significant changes between both groups postoperatively ().
Table 5. Comparison between both groups regarding Intraoperative and postoperative heart rate values (Beats/min)
Table 6. Comparison between both groups regarding intraoperative and postoperative mean arterial blood pressure values (mm Hg)
Finally, as regards postoperative nausea and vomiting, it was less in group E (2 patients) when compared to (seven patients) in group T with an insignificant difference (p = 0.072). Finally, both groups of the patients were satisfied with their mode of analgesia and were discharged home within 24 h postoperatively ().
Table 7. Comparison between both groups as regards postoperative nausea and vomiting and patient satisfaction
4. Discussion
One of the major issues in perioperative care is analgesia. Traditionally, this is accomplished by the use of opioids, which are effective broad-spectrum analgesics. However, these drugs can cause many unwanted side effects such as depression of respiration, nausea, vomiting, sedation, constipation and increased hospital stay length [Citation6]. Therefore, using opioid-sparing techniques has become trend in anaesthesia in order to enhance recovery following surgery and decrease postoperative use of opioids.
In current study, among patients undergoing abdominal laparoscopic cholecystectomy; using intraoperative esmolol infusion in association with TAP block had showed a significant reduction in early postoperative pain scores along with an observed degree of variation in hemodynamics when compared with using TAP block alone, implying the effectiveness of esmolol in postoperative pain management.
Although esmolol role in modulating postoperative pain is still unestablished, yet a few studies have helped to explain the mechanism of its analgesic effect. Beta-adrenergic antagonists act by activation of G proteins in the isolated cell membranes; this feature is similar to the mechanism of clonidine which produces central analgesia [Citation7].
Ekstein et al. study on Laparoscopic patients in the PACU reported that pain in post-laparoscopy individuals required 33% more analgesic doses, and their pain was more severe than the post-laparotomy individuals for the first 4 hours postoperatively; however, laparoscopy patients show a relative decrease in pain scores after 24 hours and were discharged from hospital earlier with more satisfaction from the technique. The study assumed that the increase in pain scores in the immediate postoperative period could be explained by the generation of “central sensitization,” which further prolongs and enhances pain, this could occurs due to carbon dioxide insufflation itself [Citation8].
Other studies have assessed the effectiveness of TAP block alone for postoperative analgesia after laparoscopic cholecystectomy. Controversial outcomes have been declared. Many reasons can explain these controversies; at first, the approach of TAP block used, lateral versus subcostal, which appears to be more appropriate for laparoscopic cholecystectomy. Besides, multimodal analgesia which is a recommended medical practice was not always applied in such studies; this strategy has the potential to reduce postoperative pain as well as reducing the clinical utility of TAP block. Finally, the efficacy of TAP block would be more obvious if the parietal pain was more predominant than visceral pain. On the contrary, if visceral pain was predominant TAP block effectiveness would be less [Citation9].
In current study, the mean static and dynamic VAS scores in group E were significantly lower in the first two hours postoperatively (p < 0.05). As well as, postoperative opioid consumption was lesser among patients in group E than group T (5.83 vs 7.5). Though this decrease was insignificant, but it confirms our finding of low pain scores in group E. These results are similar to the findings of previous studies, such as that of Lahiri et al. who studied the influence of intraoperative esmolol infusion on postoperative pain following laparoscopic cholecystectomy and they found that postoperative requirements of fentanyl were significantly lower in patients of esmolol group [Citation5].
Watts et al. review and meta-analysis studied the influence of perioperative esmolol infusion in postoperative analgesia, showed that numeric pain scores at rest in the immediate postoperative period were reduced in esmolol group. As well, the opioid consumption in the PACU was less when compared to the placebo group [Citation10].
Dhir et al. found that both intraoperative and postoperative analgesic requirements were altered after esmolol infusion [Citation11]. Many previous studies showed also a significant reduction in opioids (fentanyl, morphine) given postoperatively to the patients who received esmolol infusion [Citation12–15].
In current study, the mean values of HR were significantly lower in group E (p < 0.001) at all-time points measured intraoperatively compared to group T. As well as, MAP was significantly lower in group E (p < 0.05). However, these significant differences were not observed in the postoperative period and both groups were comparable (p > 0.05). Similar results were noted by Dhir et al. who reported that HR, MAP, systolic and diastolic blood pressure were statistically comparable in esmolol and control groups from 0 to 8 min (time of intubation). Followed by a significant decrease of MAP in esmolol group and remained higher in control group till the end of surgery [Citation11]. Dereli et al. conducted a similar trial and reported that HR was significantly lower in esmolol groups compared to controls (p = 0.001); but, blood pressures were comparable in all groups (p = 0.594) [Citation16]. Other studies as well reported lower HR and/or MAP compared with controls [Citation17,Citation18].
the contrary, Lahiri et al. study found that patients received esmolol had better intraoperative HR and MAP control, although it failed to reach statistical significance [Citation5]. Similar studies found no changes in one or both of these parameters [Citation19,Citation20].
In current study, postoperative nausea and vomiting were less in group E in which only three patients experienced PONV in comparison to seven patients in group T but statistically insignificant. In Dereli et al. study, they found that PONV incidence was significantly lowest in groups that received esmolol [Citation16].
A random-effects meta-analysis compared the impact of esmolol and opioids on PONV and reported that among 439 patients, of whom 228 received esmolol while 211 received opioids, esmolol led to a reduction by 69% in the incidence of PONV [Citation21]. Watts et al. review and meta-analysis showed that a reduction in postoperative nausea and vomiting was also evident [Citation10].
The current study had several limitations, the first of which was that the majority of the participants were female patients. According to studies, women may experience and express more pain following surgery, requiring higher doses of analgesics [Citation22]. The second limitation was absence of a placebo group because TAP block was helpful for laparoscopic operations so we employed it as an active comparator instead of a placebo group. As well as, there were evidences suggesting that esmolol decreases opioids need following surgery when compared to placebo [Citation15]. Importantly, the ethical issue for not using opioids intraoperatively was concerned. Finally, the small sample size, so further studies with adequate sample size is needed.
5. Conclusion
The current study showed that there was an improvement of pain management after laparoscopic cholecystectomy when using intraoperative esmolol infusion in association with TAP block particularly in the early postoperative period. Otherwise, there were no statically significant differences between other variables postoperatively.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ramkiran S, Jacob M, Honwad M, et al. Ultrasound-guided combined fascial plane blocks as an intervention for pain management after laparoscopic cholecystectomy: a randomized control study. Anesth Essays Res. 2018 Jan;12(1):16.
- Siddiqui NA, Azami R, Murtaza G, et al. Postoperative port-site pain after gall bladder retrieval from epigastric vs. umbilical port in laparoscopic cholecystectomy: a randomized controlled trial. Int J Surg. 2012 Jan 1;10(4):213–216.
- Bharti N, Kumar P, Bala I, et al. The efficacy of a novel approach to transversus abdominis plane block for postoperative analgesia after colorectal surgery. Anesthesia Analg. 2011 Jun 1;112(6):1504–1508.
- Davidson EM, Szmuk P, Doursout MF, et al. Antinociceptive and cardiovascular properties of esmolol following formalin injection in rats. Can J Anaesth. 2001;48:59–64.
- Lahiri S, Das S, Basu SR. Effect of intraoperative esmolol infusion on postoperative analgesia in laparoscopic cholecystectomy patients: a randomised controlled trial. J Evol Med Dent Sci. 2015 Oct 8;4(81):14143–14152.
- Ricardo Buenaventura M, Rajive Adlaka M, Nalini Sehgal M. Opioid complications and side effects. Pain Physician. 2008;11:S105–20.
- Hagelüken A, Grünbaum L, Nürnberg B, et al. Lipophilic beta-adrenoceptor antagonists and local anesthetics are effective direct activators of G-proteins. Biochem Pharmacol. 1994;47:1789–1795.
- Ekstein P, Szold A, Sagie B, et al. Laparoscopic surgery may be associated with severe pain and high analgesia requirements in the immediate postoperative period. Ann Surg. 2006 Jan;243(1):41.
- Zhao X, Tong Y, Ren H, et al. Transversus abdominis plane block for postoperative analgesia after laparoscopic surgery: a systematic review and meta-analysis. Int J Clin Exp Med. 2014;7(9):2966.
- Watts R, Thiruvenkatarajan V, Calvert M, et al. The effect of perioperative esmolol on early postoperative pain: a systematic review and meta-analysis. J Anaesthesiol Clin Pharmacol. 2017;33:28–39.
- Dhir R, Singh MR, Kaul TK, et al. Effect of intravenous esmolol on analgesic requirements in laparoscopic cholecystectomy. J Anaesthesiol Clin Pharmacol. 2015 Jul;31(3):375.
- Miller RE, White PF, Eng MR. Ambulatory (outpatient) anesthesia. Anesthesia. 7th ed. Philadelphia Churchill Livingstone Elsevier; 2010. p. 2419–2459.
- Ozturk T, Kaya H, Aran G, et al. Postoperative beneficial effects of esmolol in treated hypertensive patients undergoing laparoscopic cholecystectomy. Br J Anaesth. 2008;100:211–214.
- Celebi N, Cizmeci EA, Canbay O. Intraoperative esmolol infusion reduces postoperative analgesic consumption and anaesthetic use during septorhinoplasty: a randomized trial. Rev Bras Anestesiol. 2014;64:343–349.
- Collard V, Mistraletti G, Taqi A, et al. Intraoperative esmolol infusion in the absence of opioids spares postoperative fentanyl in patients undergoing ambulatory laparoscopic cholecystectomy. Anesth Analg. 2007;105:1255–1262.
- Dereli N, Tutal ZB, Babayigit M, et al. Effect of intraoperative esmolol infusion on anesthetic, analgesic requirements and postoperative nausea-vomitting in a group of laparoscopic cholecystectomy patients. Rev Bras Anestesiol. 2015 Apr;65(2):141–146.
- Gökçe BM, Karabiyik L, Karadenizli Y. Hypotensive anesthesia with esmolol. Assessment of hemodynamics, consumption of anesthetic drugs, and recovery. Saudi Med J. 2009 Jun 1;30(6):771–777.
- Bhawna SJ, Lalitha K, Dhar P, et al. Influence of esmolol on requirement of inhalational agent using entropy and assessment of its effect on immediate postoperative pain score. Indian J Anaesth. 2012 Nov;56(6):535.
- Chia YY, Chan MH, Ko NH, et al. Role of β-blockade in anaesthesia and postoperative pain management after hysterectomy. Br J Anaesth. 2004 Dec 1;93(6):799–805.
- Coloma M, Chiu JW, White PF, et al. The use of esmolol as an alternative to remifentanil during desflurane anesthesia for fast-track outpatient gynecologic laparoscopic surgery. Anesthesia Analg. 2001 Feb 1;92(2):352–357.
- Thiruvenkatarajan V, Watts R, Calvert M, et al. The effect of esmolol compared to opioids on postoperative nausea and vomiting, postanesthesia care unit discharge time, and analgesia in noncardiac surgery: a meta-analysis. J Anaesthesiol Clin Pharmacol. 2017;33:172–180.
- Taenzer AH, Clark C, Curry CS. Gender affects report of pain and function after arthroscopic anterior cruciate ligament reconstruction. Anesthesiology. 2000;93:670–675.