ABSTRACT
Background
Acute respiratory failure (ARF) in immunocompromised patients is associated with increased incidence of mortality when endotracheal intubation is used. Early use of high flow nasal cannula (HFNC) or non-invasive ventilation (NIV) may prevent intubation. This prospective randomized controlled study was designed to evaluate the use of HFNC versus NIV in prevention of intubation in immunocompromised patients suffering from ARF.
Methods
After ethical committee’s approval and written informed consent, 76 patients were enrolled in the study, 38 in each group. Patients were randomized into High Flow Nasal Cannula (HFNC) group as they connected to HFNC to keep SpO2 92% or more alternating with simple face mask 10–15 L/min, or non-invasive ventilation (NIV) group as they connected to ICU ventilator pressure support 8 cmH2O and PEEP 5 cmH2O or more to keep SpO2 92% or more alternating with simple face mask 10–15 L/min. Tolerance to HFNC or NIV, need for intubation, ICU stay, hospital stay and 28-day mortality rate were documented and compared between the two groups.
Results
Seventy six patients were enrolled, 38 in each group, VAS tolerance was statistically significant higher in HFNC than NIV group 7(6–7) vs 6(5–7), respectively, p value < 0.001. Incidence of intubation was statistically significant lower in HFNC than NIV (31.6% vs 55.3%), respectively, (p value 0.037), however both groups had similar 28-day mortality rate, (p value 0.195).
Conclusion
Use of high flow nasal cannula in immunocompromised patients suffering from ARF has less incidence of endotracheal intubation but same 28-day mortality rate when compared to non-invasive ventilation.
1. Introduction
Over the last decades, the number of immunocompromised patients have increased due to advances in chemotherapy, bone marrow transplantation and other organ transplantation [Citation1]. Indeed these types of patient have risk of serious complications especially acute hypoxemic respiratory failure [Citation2]. Acute respiratory distress syndrome (ARDS) mortality is high, it ranges from 35% to 46% according to the severity of ARDS and remains high despite recent modalities of treatment [Citation3]. Non-invasive ventilation (NIV) becomes a reliable method in treatment of acute respiratory failure but its role in ARDS is not certain [Citation4]. Acute respiratory failure (ARF) type 1 is considered one of the major indications for ICU admission in immunocompromised patients. Early non-invasive ventilation is considered as a practical, simple and inexpensive technique to prevent deterioration of respiratory functions and complications in this type of patients [Citation5]. A large center study showed that there is no difference between NIV and standard oxygen therapy in ARF [Citation6].
High flow nasal cannula (HFNC) which has been in clinical development for the past two decades, initially in neonatal medicine, started to be a good alternative to NIV in clinical practice in intensive care unit (ICU) [Citation7]. In recent studies, HFNC was used to treat ARF to prevent intubation and to study its effect on mortality rate [Citation8–10]. However, these studies did not compare HFNC use to NIV in immunocompromised patients suffering from ARF in ICU.
The aim of this study is to evaluate the effect of HFNC alternating with simple face mask and NIV alternating with simple face mask in immunocompromised patients admitted to ICU with ARF, primary outcome was the need for endotracheal intubation within 48 hours of admission, secondary outcome was the length of stay in ICU and mortality rate after 28 days of admission.
2. Methods
This study was conducted in the general intensive care unit after ethical committee approval and clinical trial registration in the period between March and July 2020. It is a prospective randomized controlled study. A total of 90 eligible patients were randomized by computer system, after written informed consent, to one of the two groups either high flow nasal cannula (HFNC) group or non-invasive ventilation (NIV) group. Inclusion criteria included admitted immunocompromised patients to general ICU with acute hypoxemic respiratory failure (ARF).
ARF is characterized by respiratory rate more than 25/min, PaO2 /FiO2 less than 300 under standard O2 10 L/min, or findings of persistent pulmonary infiltrates in radiographs.
Immunocompromised patients have one or more of the following criteria hematological: malignancy (either active or remitting in the last 5 years), bone marrow transplantation (in the last 5 years), severe leucopenia less than 1000 white blood cells in cubic millimeter, solid organ transplantation, steroid therapy more than 0.5 mg/kg/day for at least 3 weeks, or cytotoxic therapy for non-malignant disease.
Exclusion criteria included need of emergency intubation as in cases of cardiopulmonary resuscitation or as result of respiratory arrest, patients with deterioration of conscious level with hypoxemia with SpO2 less than 90% in spite of maximum O2 support, haemodynamic instability with need of vasoconstrictor support to maintain systolic blood pressure more than 90 mmHg, and postoperative patients.
Patients included in the study were randomized after admission to ICU to one of the two groups, HFNC group or NIV group. Patients enrolled in the HFNC group immediately connected to HFNC (Optiflow Fisher and Paykel, Auckland, New Zealand) with a flow of 60 L/min, and FIO2 adjusted to have SpO2 of 92% or more, through a heated humidifier and an oxygen blender of the same machine (). In case of patient intolerance to high flow, flow was diminished to the highest tolerated by the patient. Patients were encouraged to have their mouth closed during HFNC to augment positive end expiratory pressure (PEEP) created by high flow. The constant flow rate of HFNC offers variable pressures in airways according to the breath effort of the patient and dynamic thoracic compliance. Patient was connected to it to most tolerated period alternating with simple face mask 10–15 L/min.
NIV group, patients were connected to ICU ventilator (Evita, Drager, Lubeck, Germany) on NIV mode for at least 4 hours, through a NIV continuous positive airway pressure (CPAP) mask with ventilator settings; pressure support (PS) level of 8 cmH2O and PEEP level of 5 cmH2O, which can be increased to 10 cmH2O to maintain tidal volume between 6 and 8 ml/kg and FiO2 adjusted to keep SpO2 equal or more than 92%. At least patient was on NIV for 12 hours during the day, alternating with simple face mask 10–15 L/min to keep SpO2 equal or more than 92%.
In all patients, the head of the bed was elevated till 45-degree angle, monitoring was continuous for heart rate, blood pressure, respiratory rate (RR) and oxygen saturation. Frequent arterial blood gas (ABG) monitoring was done/12 hours and if needed in case of desaturation. Medications included antimicrobial agents, bronchodilators, diuretics, immunosuppressive agents and subcutaneous heparin to be continued during patient stay in ICU. Parenteral nutrition, correction of electrolyte disturbances, and fluid resuscitation was kept for all patients during the study.
Oxygen support for patients of both groups was continued for at least 48 hours, then according to the respiratory state of the patient, could be weaned from oxygen support or need mechanical ventilation. Patients of both groups could be weaned from HFNC and NIV and switched to conventional oxygen therapy in the form of simple face mask or nasal cannula with oxygen flow from 4 to 10 L/min, when RR is less than 25 breaths/min and SpO2 equal or more than 92% with FiO2 equal or less than 0.5 and flow less than 50 L/min in HFNC or stopped NIV with maintenance of the same respiratory parameters. In case of respiratory distress or desaturation after weaning of oxygen support in the form of HFNC or NIV, patient was shifted again to oxygen support according to his randomization group.
There was no hesitation of intubation for patients included in the study to avoid harms of delayed intubation. Intubation was performed for patients of either HFNC or NIV in case of occurrence of one of the following criteria; disturbed conscious level in the form of agitation or Glasgow Coma Scale less than 8, severe hemodynamic instability defined as need of more than 300 ng/kg/min norepinephrine support to maintain systolic blood pressure more than 90 mmHg, severe respiratory distress with RR more than 40 breaths/min, severe hypoxemia with PaO2 /FiO2 less than 100 or presence of significant acidosis with pH less than 7.35.
2.1. Data collection
Data of each patient were collected by a research assistant for each patient after written informed consent and computer randomization. Age, sex, and weight of patient were documented. Comorbidities of patients as regards hypertension, diabetes, coronary artery disease, renal impairment or hepatic impairment were documented. Group of patient either HFNC or NIV group, state of oxygenation in the form of PaO2, FiO2 and oxygen saturation. Tolerance of patient to oxygen support either HFNC or NIV was monitored via visual analogue scale of 10 cm ranges from 0: means very uncomfortable to 10: means very comfortable, frequent ABG every 12 hours, and daily chest X-ray, with documentation of percent of chest affection by infiltration or consolidation which was done by intensivist who was blinded to treatment modality. Daily clinical examination of patient in the morning round in ICU for follow up of patient improvement or deterioration on oxygen support. If patient of either groups need intubation and mechanical ventilation, cause and time of intubation were evaluated. Length of ICU stay and total duration of hospital stay were documented, mortality rate after 28 days of ICU admission and cause of death were recorded.
End point of the study was need of intubation and mechanical ventilation in HFNC or NIV groups, or cardiac arrest and declared death.
Sample size calculation was done based on previous study Gilles et al. [Citation11], using PASS 11 program and assuming incidence of intubation in NIV group 46%, sample size of 38 patients in each group can detect the difference between two groups with power 80% and α − error 0.05. Data were collected, revised, coded and entered to the statistical package for social science (IBM SPSS) version 23 (released 2015.IBM SPSS statistics for Windows, Armonk, NY: IBM Corp.). The comparison between the quantitative data was done as mean, standard deviation and range, when parametric and presented as median with inter-quartile range (IQR) when non-parametric. Qualitative variables were presented as number and percentages. The comparison between the groups as regards to qualitative data was done by using Chi-square test. The comparison between groups as regards qualitative data was done by using Chi-square test. The comparison between two independent groups with quantitative data and parametric distribution was done by using Independent t-test while with non-parametric distribution was done by using Mann-Whitney test. Repeated Measures ANOVA was used to compare between more than two paired measurements in the same group.
The confidence interval was set to 95% and the margin of error accepted was set to 5%. So, the P value was considered statistically significant at the level of <0.05.
3. Results
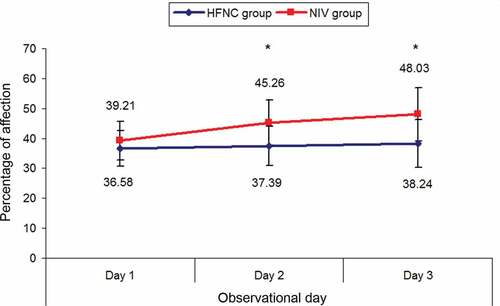
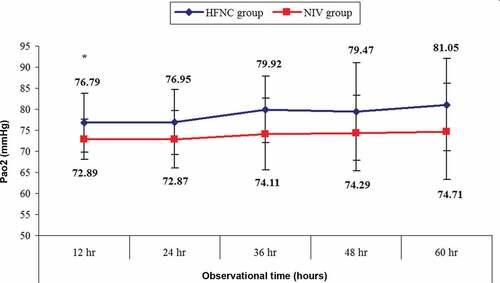
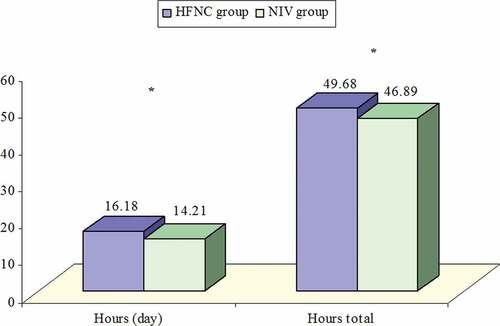
Patients assessed for eligibility were 90, 10 patients were excluded for different reasons, 80 patients were followed up, 76 patients continued for analysis (Consort flow diagram, ); follow up in ICU for all patients was done by the same ICU team. There were no statistically significant differences between the two groups as regards age, sex, and diagnosis, while there were statistically significant higher VAS tolerance in HFNC than NIV 7 [Citation6,Citation7] vs 6 [Citation5–7], respectively, p value < 0.001 (). There were no statistical differences as regards admission parameters to ICU (). Chest X-ray affection showed statistically significant differences between the two groups as more affection in NIV group than HFNC group at second and third day of ICU stay (p value < 0.001), while more affection and deterioration of NIV group in second and third day in comparison to first day (p value < 0.001) (, ). Changes in PaO2 showed statistically significant higher PaO2 in HFNC group than NIV group at 12, 24, 36, 48, and 60 hours from admission to ICU (p value < 0.05) (). Application of HFNC or NIV to patients in ICU showed statistically significant longer hours of application in HFNC than NIV as regards hours/day and total hours during ICU stay (p value< 0.05) (, ). Incidence of intubation was statistically significant lower in HFNC than NIV (12 patients 31.6% versus 21 patients 55.3% respectively) (p value 0.037)().There was no statistically significant difference between HFNC and NIV as regards 28 day mortality (p value 0.159) (). Duration of ICU stay and hospital stay were statistically significant lower in HFNC than NIV (p values 0.044 and 0.042), respectively. Duration of intubation was statistically significant lower in HFNC than NIV. (p value 0.001) ().
Table 1. Demographic data and tolerance to HFNC or NIV
Table 2. Admission parameters to ICU
Table 3. Chest X-ray changes (percent of affection) during ICU stay
Table 4. Application of HFNC or NIV to patients in ICU hours/day and total hours
Table 5. Incidence of intubation, ICU stay and hospital stay
4. Discussion
The present study was designed to compare the effect of using HFNC versus NIV in immunocompromised patients admitted to intensive care unit suffering from acute hypoxemic respiratory failure for prevention of intubation and assessment of 28 day mortality. The main finding of the study is that incidence of intubation was lower in patients assigned to HFNC than those patients treated with NIV. As regards 28-day mortality, there was no significant difference noted between patients treated with HFNC and NIV.
Invasive ventilation is associated with high mortality rates in immunocompromised patients, so seek of other treatment modality like NIV is recommended as means of avoiding intubation [Citation12]. However, NIV was associated with failure rate from 60% to 70% in immunocompromised patients with acute hypoxemic respiratory failure [Citation13,Citation14]. This failure rate of NIV required obligation of endotracheal intubation is near the result of the present study as need of intubation in NIV was 55.3%. In the present study tolerance to HFNC was significantly higher than NIV by patients, this may explain the lower incidence of intubation in HFNC than NIV group, the present result coincides with Frat et al. [Citation15] who found that NIV was not the best treatment for acute hypoxemic respiratory failure in immunocompromised patients and had increased risk of intubation when compared to HFNC. On the other hand, in the present study duration before intubation was not statistically significant different between two groups although duration of tolerance was much higher in HFNC than NIV this might be due to difference of incidence of intubation between two groups. The results of the present study as regards need for intubation in NIV were different from Huang et al. [Citation16]. who emphasized that NIV would reduce intubation rate and length of stay in ICU, the cause of this difference is mostly the large scale of patient in their study and different groups of immunocompromised patients with acute respiratory failure.
Chest X-ray differences between NIV and HFNC groups were statistically insignificant at admission (day 1), while were statistically significant worse in NIV than HFNC group after admission by second and third day, this might be due to better tolerance of patients in HFNC than NIV group to the oxygen support technique or might be also due to other causes like chest infection, aspiration, deterioration of primary pathology. The result is coincident with finding of Tan et al. [Citation17] who found that patients in HFNC were more tolerant to treatment than of NIV, however in a different group of patients as they compared HFNC to NIV for chronic obstructive pulmonary disease patients after extubation. Improvement of PO2 in HFNC group more than NIV was statistically significant this might be due to longer time of patient treatment on HFNC than NIV, this result was similar to findings of Sim et al. [Citation18] in a physiological study between simple face mask, non-rebreathing mask and HFNC found that FIO2 by HFNC was higher due to the high flow 40 L/min so higher PO2 of patients among the three groups. Twenty-eight day mortality rate was similar between patients in HFNC group and NIV group, this finding was different from Frat et al. [Citation15] who found that HFNC treatment in immunocompromised patients suffering from acute hypoxemic respiratory failure was associated with lower incidence of 28 day mortality than NIV patients, this may be due to difference in sample size as it was a multicenter study, whereas the present study is a single center study. Mortality rate in the present study was 47 % which was near to the result of Bellani et al. [Citation19] who emphasized that in a large scale international lung safe study, severe hypoxemic patients who failed NIV had a higher mortality rate (approximately 43%) than invasively ventilated patients, in the present study we compared HFNC to NIV with result of 28 days mortality 31% to 47%, respectively. In a systematic review and meta analysis was done by Sklar et al. [Citation20], HFNC was found that it decreased mortality compared to alternative non-invasive oxygen control, the cause of difference of result of the present study might be due to difference of sample size as it was a meta analysis study.
ICU stay and hospital stay were statistically significant shorter in HFNC group than NIV group. These findings were different from findings of Huang et al. [Citation16] that early use of NIV is associated with shorter ICU stay in comparison to oxygen therapy alone.
5. Conclusion
In conclusion, the results of the present study found that, high flow nasal cannula could prevent endotracheal intubation and is associated with shorter ICU stay and hospital stay when used in immunocompromised patients suffering from acute hypoxemic respiratory failure when compared to non-invasive ventilation, but both methods have similar 28-day mortality rate.
Ethical committee approval number is: (FMASU R 9/2020).
Clinical trial .gov number is: (NCT04293991).
Acknowledgments
We wish to thank Prof Dr Rafaat Abd El Azim Hammad. Professor of anesthesia and intensive care Ain Shams University for his continuous encouragement and revision of manuscript of this work, ICU staff for their assistance and data collection of this study.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Salvadori M, Berloni E. What’s new in clinical solid organ transplantation by 2013. World J Transplant. 2014;4(4):243–266.
- Azoulay E, Lemiale V, Mokart D, et al. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40(8):1106–1114.
- Bellani G, Laffey JP, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315(8):788–800.
- Brambilla AM, Aliberti S, Prina E, et al. Helmet CPAP vs. oxygen therapy in severe hypoxemic respiratory failure due to pneumonia. Intensive Care Med. 2014;40(7):942–949.
- Stefan MS, Nathanson BH, Lagu T, et al. Outcomes of noninvasive and invasive ventilation in patients hospitalized with asthma exacerbation. Ann Am Thorac Soc. 2016;13(7):1096–1104.
- Lemiale V, Mokart D, Resche-Rigon M, et al. Effect of noninvasive ventilation vs oxygen therapy on mortality among immunocompromised patients with acute respiratory failure: a randomized clinical trial. JAMA. 2015;314(16):1711–1719.
- Manley BJ, Dold SK, Davis PG, et al. High-flow nasal cannulae for respiratory support of preterm infants: a review of the evidence. Neonatology. 2012;102(4):300–308.
- Maggiore SM, Idone FA, Vaschetto R, et al. Nasal high-flow versus Venturi mask oxygen therapy after extubation. Effects on oxygenation, comfort, and clinical outcome. Am J Respir Crit Care Med. 2014;190(3):282–288
- Spoletini G, Alotaibi M, Blasi F, et al. Heated humidified high-flow nasal oxygen in adults: mechanisms of action and clinical implications. Chest. 2015;148(1):253–261.
- Frat JP, Thille AW, Mercat A, et al. High-flow oxygen through nasal cannula in acute hypoxemic respiratory failure. N Engl J Med. 2015;372(23):2185–2196.
- GILLES H, DIDIER G, FRDERIC V, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever, and acute respiratory failure. N Engl J Med. 2001;344(7):481–487.
- Rochwerg B, Brochard L, Elliott MW, et al. Official ERS/ATS clinical practice guidelines: noninvasive ventilation for acute respiratory failure. Eur Respir J. 2017;50:
- Azoulay E, Lemiale V, Mokart D, et al. Acute respiratory distress syndrome in patients with malignancies. Intensive Care Med. 2014;40(8):1106–1114.
- Thille AW, Contou D, Fragnoli C, et al. Non-invasive ventilation for acute hypoxemic respiratory failure: intubation rate and risk factors. Crit Care. 2013;17(6):R269.
- iFrat JP, Stéphanie R, Christophe G, et al. Effect of non-invasive oxygenation strategies in immunocompromised patients with severe acute respiratory failure: a post-hoc analysis of a randomised trial. Lancet Respir Med. 2016;4(8):646–652.
- Huang B, Guang-Y X, Jian-Dong L, et al. Use of noninvasive ventilation in immunocompromised patients with acute respiratory failure: a systematic review and meta-analysis. Crit Care. 2017;21:4.
- Tan D, Harold J, Ling B, et al. High-flow nasal cannula oxygen therapy versus non-invasive ventilation for chronic obstructive pulmonary disease patients after extubation: a multicenter, randomized controlled trial. Crit Care. 2020;24(1):489.
- Sim MA, Dean P, Kinsella, J. R R Black, R Carter, M Hughes performance of oxygen delivery devices when the breathing pattern of respiratory failure is simulated. Anaesthesia. 2008;63(9):938–940.
- Bellani G, Laffey JG, Pham T, et al. Noninvasive ventilation of patients with acute respiratory distress syndrome. Insights from the LUNG SAFE Study. Am J Respir Crit Care Med. 2017;195(1):67–77.
- Sklar MC, Mohammed A, Orchanian- Cheff A, et al. The impact of high-flow nasal oxygen in the immunocompromised critically ill: a systematic review and meta-analysis. Respir Care. 2018;63(12):1555–1566.