ABSTRACT
Background
Modified radical mastectomy (MRM) with axillary clearance of lymph nodes was routinely performed under general anaesthesia with intra- and postoperative opioid analgesia. Recently, there has been a move toward opioid-free anesthesia (OFA) to appreciate the goals of hypnosis with amnesia and sympathetic stability without the adverse effects of opioids.
The aim of this study was to evaluate the effect of OFA versus opioid-based anaesthesia (OBA) in patients with breast cancer, who had undergone unilateral MRM.
The primary aims
• Pain intensity using the visual analogue scale in the first 24 h post-operatively.
• Screening for post mastectomy neuropathic pain.
The secondary aims
• Effect of opioid and surgical stress on the immune system.
• Patient outcome including haemodynamic stability, patient satisfaction and occurrence of post-operative complications.
Methods
Forty adult female patients scheduled for elective unilateral MRM were randomly divided into two groups (20 patients in each group): OFA and OBA.
Results
There was statistically significant decrease in pain score at rest and on movement in the OFA group. Postoperative nausea and vomiting was significantly decreased in the OFA group (P = 0.04). Patients in the OFA group were more satisfied than those in the OBA group using verbal rating scale for satisfaction (P < 0.001). There was significant low incidence of neuropathic pain in the OFA group; also, we found significant changes in interleukin 10, tumour necrosis factor alpha and caspase 3 between the two groups.
Conclusion
OFA is safe and effective in mastectomy as it decreases the pain score and the incidence of post mastectomy neuropathic pain; moreover, it also shows better immune response postoperatively.
1. Introduction
Breast cancer is a widespread health problem, with more than 2 million new cases worldwide [Citation1]. The neuroendocrine stress response associated with surgery, anaesthetics and opioid analgesics are factors that adversely affect the immune defense against tumors. Perioperative intervention can affect the recurrence of the tumor or metastasis by affecting tumor cell signals, immune response and neuroendocrine stress response [Citation2].
The intraoperative administration of opioids was considered the cornerstone of anaesthesia. Synthetic opioids were given to stabilize the haemodynamics during anaesthesia. They can inhibit the sympathetic nervous system without causing cardiovascular depression and histamine release [Citation3]. Despite their benefits, opioids are experiencing more and more adverse side effects, which can cause significant morbidity and mortality, as respiratory depression, nausea/vomiting, constipation, tolerance and hyperalgesia [Citation4]
Opioid-free multimodal analgesia has become an alternative to postoperative pain relief [Citation5]. The use of multimodal non-opioid analgesics during the perioperative period can preventively block receptors in complex pain pathways. It has been shown that preoperative use of Cox inhibitors, GABA agonist and paracetamol can reduce postoperative opioid consumption. Sodium channel block, G protein–related receptor block, NMDA receptor antagonist, central alpha-2 agonist and nonsteroidal anti-inflammatory drugs may lead to opioid-free anaesthesia (OFA) [Citation6]. Thoracic paravertebral block (TPVB) combined with general anaesthesia (GA) can provide excellent analgesia for cancer surgery and reduce the severity of chronic pain after mastectomy [Citation7].
The immune system has a major role in preventing cancer development and prevent its metastasis. The acute and chronic administration of exogenous opioids appear to affect the body’s cell mediated and humoral immune response. Exogenous opioids have a significant effect on several components of the immune system including lymphocyte proliferation., phagocytic activity, natural killer cell activity, cytokine expression and antibody production [Citation8,Citation9].
Interleukin 10 (IL-10) is an anti-inflammatory cytokine and it has the ability to inhibit the production of pro-inflammatory cytokines [Citation10]. TNF-α (tumour necrosis factor alpha) is a pro-inflammatory cytokine [Citation11]. Apoptosis is a non-inflammatory form of programmed cell death that is mediated by the activation of apoptotic caspases and can occur via an intrinsic or an extrinsic pathway. Activated caspase-3 is found at the end of caspase cascades and is activated by both endogenous and exogenous apoptotic pathways, making it a key protein in apoptosis [Citation12].
The purpose of this study was to evaluate the effect of OFA versus opioid-based anesthesia (OBA) for patients with breast cancer on perioperative pain score, the presence of neuropathic pain after mastectomy and the impact of opioids on the immune system.
2. Patients and methods
After obtaining an approval from the local ethics committee and informed consent from each patient, the research was carried out on 40 adult female patients (admitted to the Medical Research Institute, University of Alexandria) and scheduled for elective unilateral modified radical mastectomy.
2.1. Inclusion criteria
American Society of Anesthesiology (ASA) physical status class I and II, age group from 40 to 65 years.
2.2. Exclusion criteria
Coagulopthies, body mass index (BMI) >35 kg/m2, immunosuppressive therapy or immune disorders, radiotherapy or chemotherapy before surgery, history of allergy to local anaesthetics, patients suffering from neuropathy, patients with chronic pain on opioid therapy, patients with cognitive dysfunction or with psychiatric disordered and patients with previous ipisilateral breast surgery.
2.3. Anaesthetic technique
All patients were attached to multichannel monitor displaying heart rate (HR) (beats/minute) non-invasive mean arterial blood pressure (MABP) in mmHg and peripheral oxygen saturation (SpO2) (%)
In the OFA group, all patients received midazolam (0.05 mg/kg) prior to ultrasound guided TPVB [Citation13,Citation14] using a 2–5 MHz low-frequency curved array transducer (Sonosite S-Nerve, Sonosite Inc,USA) placed longitudinally (out-of-plane approach) at T3-T4 to obtain a parasagittal view to visualize the transverse process as a hyperechoic structure, with acoustic shadowing below it. An 18-gauge Tuohy tip needle was inserted at the cephalic end of the transducer and the needle was advanced into the paravertebral space. After negative aspiration of air, blood and CSF, 30 ml of levobupivacaine 0.25% was slowly injected into the paravertebral space. Proper spread of the drug in the paravertebral space was confirmed by anterior displacement of the pleura, A catheter was introduced through the Tuohy needle and placed 4–5 cm beyond the tip of the needle.
GA was induced by propofol (2 mg/kg) and atracurium (0.5 mg/kg), then Laryngeal mask airway (LMA) was inserted.
Anaesthesia was maintained with isoflurane (MAC 1.2) and incremental doses of atracurium guided by nerve stimulator (TOF-Watch SX, Organon, Ireland) train of four (TOF). Then, 5 ml of levobupivacaine 0.25% was injected through the paravertebral catheter as incremental doses if HR or MABP are more than 20% of baseline after exclusion of other causes than pain. At the end of surgery, residual neuromuscular block was reversed by atropine and neostigmine.
Postoperatively, all patients were on continuous paravertebral catheter infusion 0.125% levobupivacaine at a rate 7 ml/h on syring pump. Paracetamol 1 g IV and 5 ml of levobupivacaine 0.25% through the paravertebral catheter were given if the VAS was 3 or more (at rest or on arm movement).
In the opioid-based anaesthesia (OBA) group, standard GA was induced by IV nalbuphine (0.2 mg/kg), propofol (2 mg/kg) and atracurium (0.5 mg/kg), then LMA was inserted.
Anaesthesia was maintained with isoflurane (MAC 1.2) and incremental doses of atracurium guided by nerve stimulator (TOF-Watch SX). Nalbuphine (0.1 mg/kg) was given as an increment if HR or MABP were more than 20% of baseline after exclusion of other causes than pain.
Postoperatively, all patients received paracetamol IV 1 g/6 h and nalbuphine (0.1 mg/kg) IV given if the VAS was 3 or more (at rest or on arm movement).
3. Measurements
3.1. The following parameters were measured
3.1.1. Vital signs
HR: (beats/minute).
MABP in mmHg.
SpO2 (%)
3.1.2. Pain score postoperatively (at rest and on arm movement)
Pain level was assessed in the post anaesthesia care unit (PACU) upon arrival from the operating room and after 30 min, every hour in the first 4 h and every 4 h postoperatively for 24 h using the visual analogue scale (VAS) at rest and on arm movement (0–10), where 0 = no pain and 10 = severe pain [Citation15].
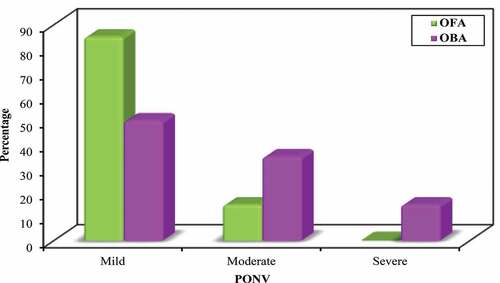
3.1.3. Postoperative nausea and vomiting (PONV)
Nausea was defined as subjective unpleasant sensation with concomitant awareness of the urge to vomit. Postoperative nausea was evaluated during the first 24 h by means of VAS where 1–3 (mild nausea), 4–6 (moderate nausea) and 7–10 (severe nausea) [Citation16]. Ondansetron 4 mg was given in moderate to severe nausea.
Vomiting was defined as forceful expulsion of stomach contents through the mouth. Postoperative vomiting was evaluated as present or absent during the first 24 h.
3.1.4. Patient satisfaction score
Patient satisfaction score was recorded before discharge using verbal rating scale for satisfaction [Citation17]:
Very dissatisfied.
Dissatisfied.
Neutral.
Satisfied.
Very satisfied.
3.1.5. Screening for neuropathic pain
Screening for neuropathic pain was assessed after 1 week postoperatively by Douleur Neuropathique 4 (DN 4) Questionnaire [Citation18] ()
Scoring: Yes = 1 point … …. No = 0 points
Score ≥4/10 has > 90% specificity for neuropathic pain diagnosis
Figure 1. Douleur Neuropathique 4 (DN 4) Questionnaire [Citation18]
![Figure 1. Douleur Neuropathique 4 (DN 4) Questionnaire [Citation18]](/cms/asset/a46c6133-80ed-475d-9c73-d5b018a8377c/teja_a_1983366_f0001_oc.jpg)
3.1.6. Immunological assay
Peripheral blood samples were withdrawn from all patients preoperatively, 24 h post operatively and after 7 days from the operation for the following [Citation19,Citation20]:
Detection of IL-10 and TNFα in serum, which were monitored as a charactarestic pro and anti-inflammatory cytokines respectively, this was done by enzyme-linked immunosorbent assay (ELISA) using eBioscience kits and according to the manufacturer’s instructions.
Detection of programmed cell death:
Apoptosis was monitored in culture supernatant collected following a short-term culture of peripheral blood mononuclear cells. Caspase 3 as an irreversible marker for apoptosis was done by ELISA using cloud-clone kits and according to the manufacturer’s instructions.
3.2. Statistical analysis of the data
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (Armonk, NY: IBM Corp) Qualitative data were described using number and per cent. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation and median. Significance of the obtained results was judged at the 5% level.
3.3. The used tests were
1 Chi-square test
For categorical variables, to compare between different groups
2 Fisher’s exact or Monte Carlo correction
Correction for chi-square when more than 20% of the cells have expected count less than 5
3 Student t-test
For normally distributed quantitative variables, to compare between two studied groups
4 Mann–Whitney test
For abnormally distributed quantitative variables, to compare between two studied groups
4. Results
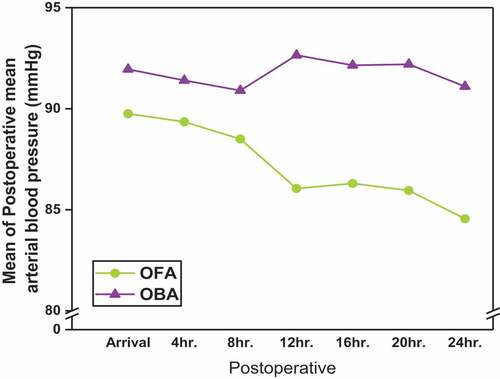
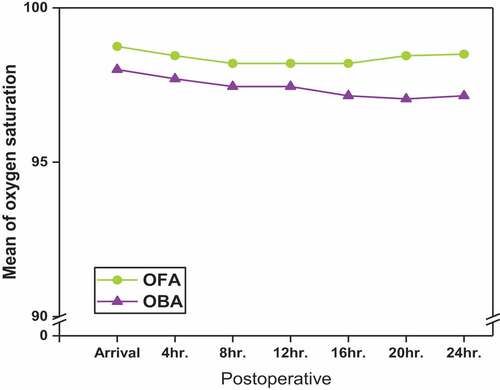
In the current study, there was no significant differences between OFA and OBA groups regarding the demographic data and patient characteristics (). There were no significant differences in the intraoperative HR, MABP and SpO2 between OFA and OBA (); however, there was significant decrease in HR, MABP and increase in SpO2 postoperatively inthe OFA group (). As regard VAS, there was significant decrease in VAS at rest and on arm movement at all times in the OFA group ()
Figure 5. Comparison between OFA and OBA according to VAS for pain assesement during rest and on arm movement
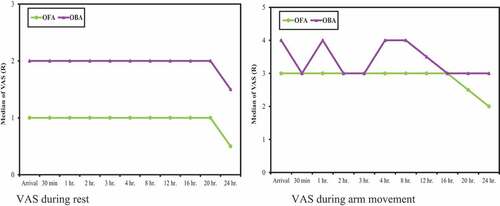
Table 1. Demographic data in OFA and OBA groups
Table 2. Correlation between caspase3, IL-10 and TNF in OFA and OBA groups
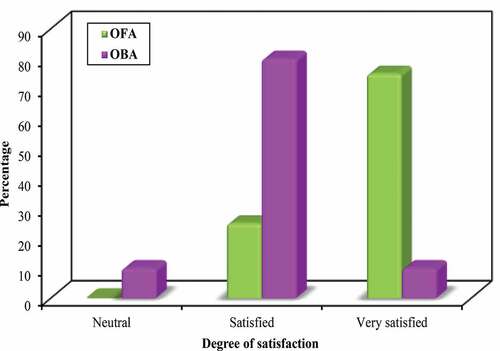
PONV was significantly decreased in the OFA group (P = 0.04) (). Patients in the OFA group were more satisfied than those in the OBA group (P < 0.001) ().
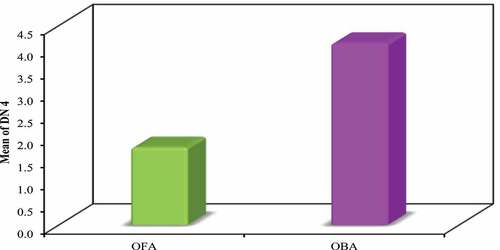
As regard screeing for neuropathic pain by DN4, all patients in the OFA group were scored less than 4; however, 14 patients (70%) in the OBA group scored more than 4. There was significant lower score of DN4 in the OFA group (P < 0.001) ().
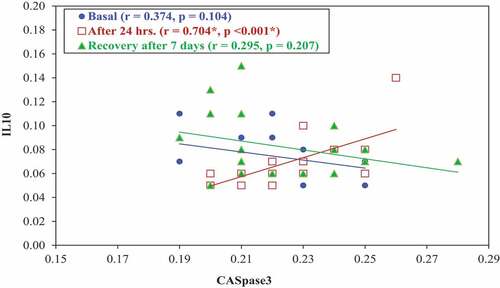
As regard IL-10 in the OFA group, statistical analysis of the data revealed significant increase after 24 h and after 7 days postoperative in comparison to basal level of IL-10 (P < 0.001), but there was no significant change in IL-10 after 24 h and after 7 days postoperatively (P = 0.635). In the OBA group, there was no significant change between the basal IL-10, 24 h and 7 days postoperatively. The comparison between the two groups showed that there was significant increase of IL-10 after 24 h and after 7 days postoperatively in the OFA group (P values were < 0.001, 0.04, respectively) ().
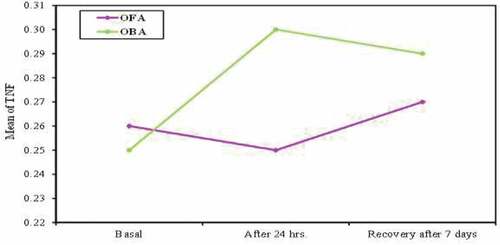
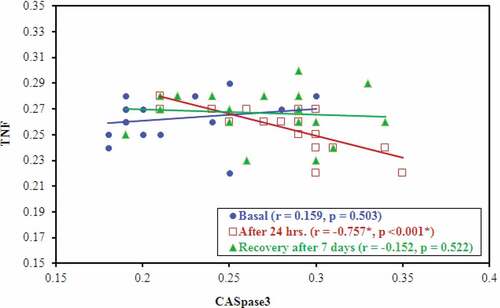
In the OFA group, there was no significant change between the basal TNFα, 24 h and 7 days postoperatively. In the OBA group, statistical analysis of the data revealed significant increase in the level of TNFα after 24 h and after 7 days postoperatively in comparison to basal level (P < 0.001), but there was no significant change between TNFα after 24 h and 7 days postoperatively (P = 1.00). The comparison between the two groups showed that there was no significant statistical difference of basal TNFα (P = 0.081), but there was significant decrease of TNFα after 24 h and after 7 days postoperatively in the OFA group (P < 0.001 and 0.002, respectively) ().
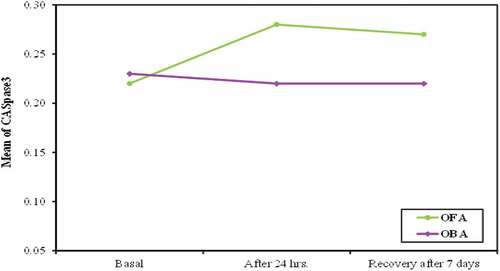
Statistical analysis of the data in the OFA group revealed significant increase in the level of caspase 3 after 24 h and 7 days postoperatively in comparison to basal level (P < 0.001, < 0.002 respectively), but there was no significant change between caspase 3 after 24 h and after 7 days postoperatively (P = 0.071). In the OBA group, there was no significant change in caspase 3 throughout time of measurement (P = 1.00). The comparison between the two groups showed that there was significant increase in caspase 3 after 24 h and after 7 days postoperatively in the OFA group (P value < 0.001) ().
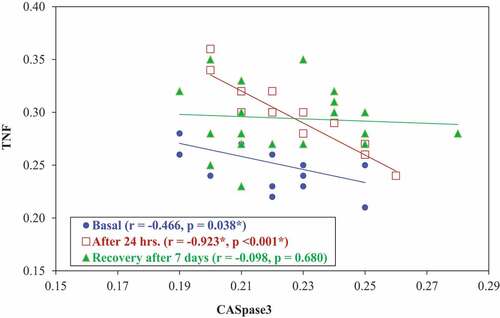
A correlation study was done between caspase 3 and IL-10 in the OFA group, and it showed significant positive correlation after 24 h postoperatively (P = 0.001) ().
A correlation study was done between caspase 3 and IL-10 in the OBA group, and it showed significant positive correlation after 24 h postoperatively (P < 0.001) ().
A correlation study was done between caspase 3 and TNFα in the OFA group, and it showed significant negative correlation after 24 h postoperatively (P < 0.001) ().
A correlation study was done between caspase 3 and TNFα in the OBA group, and it showed significant negative correlation at basal and after 24 h postoperatively (P = 0.038 and <0.001, respectively) ().
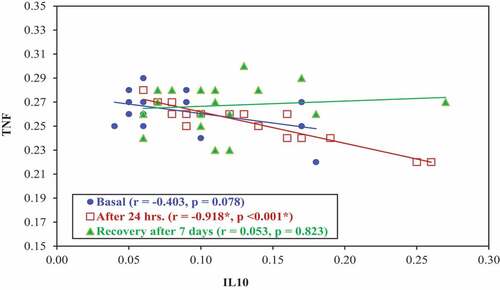
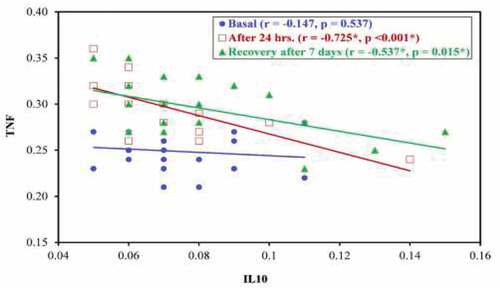
A correlation study was done between IL-10 and TNFα in the OFA group, and it showed significant negative correlation 24 h postoperatively (P < 0.001) ().
A correlation study was done between IL-10 and TNFα in the OBA group, and it showed significant negative correlation after 24 h and after 7 days postoperatively (P <0.001 and 0.015 respectively) ().
5. Discussion
The main target of anaesthesia is to make the patients pain free postoperatively with less side effects of analgesics. Opioid anaesthesia has many side effects as nausea and vomiting, respiratory depression, urine retention, intestinal obstruction, hyperalgesia, tolerance, chronic pain and increase the incidence of cancer metastasis [Citation21]. So, OFA can be used as an alternative to opioid anaesthesia to abolish the side effects of opioids. Regional anaesthesia, dexmedetomidine, ketamine and other drugs are used to rule out the use of opioids [Citation22,Citation23].
In the current study, there was no significant difference between the two groups in haemodynamics intraoperatively; however, the HR and MABP in the OFA group were significantly lower postoperatively, SpO2 was higher as compared to the OBA group. These reults referred to the marvelous effect of OFA on perioperative pain, which is the major factor influencing the patient’s haemodynamic status, and the OFA group showed lower VAS for pain assesement than the OBA group.
The results of this study were consistent with the views of Mulier et al. [Citation24], who evaluated the effects of OFA and OBA on postoperative pain and discomfort in lap bariatric surgery, and found no difference in intraoperative haemodynamics between the two groups; however, six patients in the OA group developed severe hypertention in the PACU required antihypertensive treatment, and two of them had postoperative bleeding (P = 0.007). The lowest saturation lower than 94% (P = 0.002), the highest systolic arterial blood pressure (P < 0.001) and the highest HR (P = 0.004) were in the OBA group.
On the other hand, a study conducted by Hatipoglu et al. [Citation25] compared ultrasound-guided paravertebral block (PVB) versus intravenous tramadol for postoperative pain control in percutaneous nephrolithotomy, and they found that the systolic, diastolic blood pressure, HR and SpO2 values in the postoperative period were similar between the two groups. They explained these findings by the less significant sympathetic blockade and unilateral segmental nature of the block.
In our study, the OFA group had significantly lower VAS scores during rest and on arm movement when compared to the OBA group due to effective TPVB, which result in significant reduction of pain score in the OFA group. Tripathi et al. [Citation22] compared the OFA group with the OBA group for breast cancer surgery, and found significant reduction in the VAS scores in the OFA group (P < 0.05).
In contrast to the present study, King et al. [Citation23] conducted a comparative study between OFA and conventional anaesthesia (CA) in patients undergoing mastectomy, they found that the mean pain scores in PACU, postoperative day 0 and throughout entire hospitalization were similar in OFA and CA groups (P = 0.29, 0.90 and 0.16), respectively. They referred these results to complete elimination of opioids.
The current study showed that the OFA group had a significantly lower PONV than the OBA group; this result referred to absence of opioids and their side effects in the OFA group. Ziemann et al. [Citation26] reported that the severity of PONV was significantly higher in GA with opioids group (37.3%) than the OFA group (20.0%) underwent bariatric surgery (P = 0.04).
On the other side, King et al. [Citation23] conducted a comparative study between OFA and CA in patients undergoing mastectomy, and no significant difference was found in PACU antiemetic use between OFA and CA (P = 1.00). They referred these findings to the liberal use of antiemetic drugs intraoperatively, with more than 90% of both groups receiving intraoperative dexamethasone and ondansetron
In this study, patients in the OFA group were significantly more satisfied compared with those in the OBA group due to lower pain scores and lower PONV in the OFA group. Similar to to this study, Hontoir et al. [Citation27] evaluated the influence of opioid-free methods on postoperative comfort of breast cancer patients, measured by quality of recovery (QoR40) performed 24 h after surgery, and found that there was statistically significant more satisfaction in the OFA group than the OBA group (P = 0.04).
Regarding the detection of neuropathic pain, the DN4 questionnaire of the OFA group has a statistically significant low value than OBA group, this may be due to lower pain score and good management of acute pain in the OFA group. In coherence to this study, Kairaluoma et al. [Citation28] found that the PVB group was lower at 12 months after surgery (P = 0.029 and 0.003, respectively), and the intensity of exercise-related pain and other pain levels were lower in the PVB group (P = 0.011, 0.003.), respectively).
On the other side, Heesen et al. [Citation29] examined the effect of PVB on the prevalence of persistent postsurgical pain after breast surgery and found that there was no statistically significant risk reduction for persistent postoperative pain at 3 , 6 or 12 months. The risk ratio were 0.75, 0.57 and 0.42, respectively. They recommended a large, adequately powered trial to test the efficacy of PVB in preventing the development of chronic postoperative pain in patients undergoing breast surgery .
Regarding immunoassays, in the OFA group, IL-10 and caspase 3 were significantly increase after 24 h and 7 days postoperatively, but TNFα decreased. In the OBA group, the level of IL-10 and caspase 3 were statistically significantly reduced, but the level of TNFα increased. Theses results because TPVB protects cell-mediated immunity and reduces surgical neuroendocrine stress responses that stimulate the hypothalamic-pituitary-adrenal axis and sympathetic nervous system. Jin et al. [Citation30] conducted a study in elderly patients undergoing esophagectomy, they found that the plasma TNFα levels in the PVB group were significantly reduced compared with the patient-controlled analgesia group, 24, 48, and 72 h after surgery (P < 0.05)
Consistent with our research, Buckley et al. [Citation31] compared the effect of PVB versus GA opioid anaesthesia on the immune response in patients undergoing breast cancer surgery, they found that patients received PVB maintained normal natural killer (NK) cell cytokine IL-10 function during the postoperative period (P = 0.9). However, in patients undergoing GA, IL-10 expression decreased after surgery (P = 0.001). Also, there was an increase in the level of apoptosis with patients in the PVB group (P = 0.0001), but not with the GA group.
On the other hand, Cong et al. [Citation32] compared between GA (GA group, paravertebral nerve blocks with GA (PG group) and epidural anaesthesia with GA (EG group) in oesophageal cancer surgery on perioperative cellular immunity. They found that before anaesthesia, at the end of surgery, at postoperative day 1 (POD 1) and POD 2, there was no significant difference in cytokine level of TNF-α, was noted among the three groups (P > 0.05). This was an observational cohort study with a small sample size, and subsequent studies with a larger sample size and randomised trials are needed to confirm the findings.
In conclusion, OFA technique can be used as an alternative to CA technique in mastectomy as it decreases the pain score and the incidence of post mastectomy neuropathic pain as well as shows better immune respose postoperatively.
Recommendations
•OFA technique can be used as an alternative to conventional technique in cancer surgeries.
• Further prospective studies will be needed for longer postoperative period to assess the long-term benefits of avoiding opioids as regard tumor metastasis and quality of life.
•Multicentric studies with larger number of patients are needed to be carried out to confirm the findings.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ferlay J, Colombet M, Soerjomataram I, et al. Cancer incidence and mortality patterns in Europe: estimates for 40 countries and 25 major cancers in 2018. Eur J Cancer. 2018;103:356–387.
- Byrne K, Levins KJ, Buggy DJ. Can anesthetic-analgesic technique during primary cancer surgery affect recurrence or metastasis? Can J Anaesth = Journal Canadien d’Anesthesie. 2016;63(2):184–192.
- Beloeil H, Laviolle B, Menard C, et al. POFA trial study protocol: a multicentre, double-blind, randomised, controlled clinical trial comparing opioid-free versus opioid anaesthesia on postoperative opioid-related adverse events after major or intermediate non-cardiac surgery. BMJ Open. 2018;8(6):e020873.
- Winn AN, Check DK, Farkas A, et al. Association of current opioid use with serious adverse events among older adult survivors of breast cancer. JAMA Network Open. 2020;3(9):e2016858.
- Rafiq S, Steinbrüchel DA, Wanscher MJ, et al. Multimodal analgesia versus traditional opiate based analgesia after cardiac surgery, a randomized controlled trial. J Cardiothorac Surg. 2014;9:52.
- Beloeil H. Opioid-free anesthesia. Best Pract Res Clin Anaesth. 2019;33(3):353–360.
- Simpson J, Ariyarathenam A, Dunn J, et al. Breast surgery using thoracic paravertebral blockade and sedation alone. Anesthesiol Res Pract. 2014;2014:127467.
- Zajączkowska R, Leppert W, Mika J, et al. Perioperative Immunosuppression and risk of cancer progression: the impact of opioids on pain management. Pain Res Manag. 2018;2018:9293704.
- Cho JS, Lee MH, Kim SI, et al. The effects of perioperative anesthesia and analgesia on immune function in patients undergoing breast cancer resection: a prospective randomized study. Int J Med Sci. 2017;14(10):970–976.
- Howes A, Gabryšová L, O’Garra A. Role of IL-10 and the IL-10 receptor in immune responses. reference module in biomedical sciences. Elsevier; 2014.
- Salomon BL, Leclerc M, Tosello J, et al. Tumor necrosis factor α and regulatory T cells in oncoimmunology. Front Immunol. 2018;9:444.
- Rogers C, Erkes DA, Nardone A, et al. Gasdermin pores permeabilize mitochondria to augment caspase-3 activation during apoptosis and inflammasome activation. Nat Commun. 2019;10(1):1689.
- Patnaik R, Chhabra A, Subramaniam R, et al. Comparison of paravertebral block by anatomic landmark technique to ultrasound-guided paravertebral block for breast surgery anesthesia: a randomized controlled trial. Reg Anesth Pain Med. 2018;43(4):385–390.
- El Mourad MB, Amer AF. Effects of adding dexamethasone or ketamine to bupivacaine for ultrasound-guided thoracic paravertebral block in patients undergoing modified radical mastectomy: a prospective randomized controlled study. Indian J Anaesth. 2018;62(4):285–291.
- Alghadir AH, Anwer S, Iqbal A, et al. Test-retest reliability, validity, and minimum detectable change of visual analog, numerical rating, and verbal rating scales for measurement of osteoarthritic knee pain. J Pain Res. 2018;11:851–856.
- Sameermohan A. Comparison between palonosetron and ramosetron to prevent postoperative nausea and vomiting in patients undergoing laparoscopic surgery. Indian J Clin Anaesthesia. 2020;5(3):348–353.
- Host BK, Turner AW, Muir J. Real-time teleophthalmology video consultation: an analysis of patient satisfaction in rural Western Australia. 2018;101(1):129–134.
- Beloeil H, Sion B, Rousseau C, et al. Early postoperative neuropathic pain assessed by the DN4 score predicts an increased risk of persistent postsurgical neuropathic pain. Eur J Anaesthesiol. 2017;34(10):652–657.
- Yang X, Zhong D-N, Qin H, et al. Caspase-3 over-expression is associated with poor overall survival and clinicopathological parameters in breast cancer: a meta-analysis of 3091 cases. Oncotarget. 2018;9(9):8629.
- Lim JA, Oh CS, Yoon TG, et al. The effect of propofol and sevoflurane on cancer cell, natural killer cell, and cytotoxic T lymphocyte function in patients undergoing breast cancer surgery: an in vitro analysis. BMC Cancer. 2018;18(1):159.
- Amaram-Davila J, Davis M, Reddy A. Opioids and cancer mortality. Curr Treat Options Oncol. 2020;21(3):22.
- Tripathy S, Rath S, Agrawal S, et al. Opioid-free anesthesia for breast cancer surgery: an observational study. J Anaesthesiol Clin Pharmacol. 2018;34(1):35.
- King CA, Perez-Alvarez IM, Bartholomew AJ, et al. Opioid-free anesthesia for patients undergoing mastectomy: a matched comparison. Breast J. 2020;26(9):1742–1747.
- Mulier J, Wouters R, Dillemans B, et al. A randomized controlled, double-blind trial evaluating the effect of opioid-free versus opioid general anaesthesia on postoperative pain and discomfort measured by the QoR-40. 2018;2.
- Hatipoglu Z, Gulec E, Turktan M, et al. Comparative study of ultrasound-guided paravertebral block versus intravenous tramadol for postoperative pain control in percutaneous nephrolithotomy. BMC Anesthesiol. 2018;18(1):24.
- Ziemann-Gimmel P, Goldfarb AA, Koppman J, et al. Opioid-free total intravenous anaesthesia reduces postoperative nausea and vomiting in bariatric surgery beyond triple prophylaxis. Br J Anaesth. 2014;112(5):906–911.
- Hontoir S, Saxena S, Gatto P, et al. Opioid-free anesthesia: what about patient comfort? A prospective, randomized, controlled trial. Acta anaesthesiologica Belgica. 2016;67(4):183–190.
- Kairaluoma PM, Bachmann MS, Rosenberg PH, et al. Preincisional paravertebral block reduces the prevalence of chronic pain after breast surgery. 2006;103(3):703–708.
- Heesen M, Klimek M, Rossaint R, et al. Paravertebral block and persistent postoperative pain after breast surgery: meta-analysis and trial sequential analysis. Anaesthesia. 2016;71(12):1471–1481.
- Jin L, Yao R, Heng L, et al. Ultrasound-guided continuous thoracic paravertebral block alleviates postoperative delirium in elderly patients undergoing esophagectomy: a randomized controlled trial. Medicine (Baltimore). 2020;99:17.
- Buckley A, McQuaid S, Johnson P, et al. Effect of anaesthetic technique on the natural killer cell anti-tumour activity of serum from women undergoing breast cancer surgery: a pilot study. Br J Anaesth. 2014;113(Suppl 1):i56–62.
- Cong X, Zhang W, Huang Z, et al. Effects of different anaesthesia methods on perioperative cellular immune function and long-term outcomes in patients undergoing radical resection of esophageal cancer: a prospective cohort study. 2020.