ABSTRACT
Background
The erector spinae plane block and quadratus lumborum block can provide analgesia for laparotomy surgeries. This study was conducted to compare their analgesic effects on patients posted for open colorectal cancer resection surgeries. We hypothesized that the erector spinae plane block is superior to the quadratus lumborum block at reducing postoperative pain scores. Therefore, we conducted this study to compare their analgesic efficacy and examine their validity for this type of surgeries.
Patients and methods
76 patients scheduled for open colorectal cancer surgery, aged 40–60 years, either sex, and BMI 18.5–35 Kg/m2 of ASA physical status I or II were included. All patients were randomized into two groups of 38 patients each. Every patient received 20 ml bupivacaine 0.25% and 4 mg dexamethasone for each side. The numerical rating score for pain, morphine consumption, intensity of postoperative nausea and vomiting, serum cortisol and C- reactive protein, and duration of analgesia were recorded.
Results
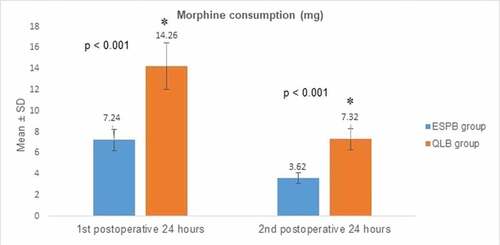
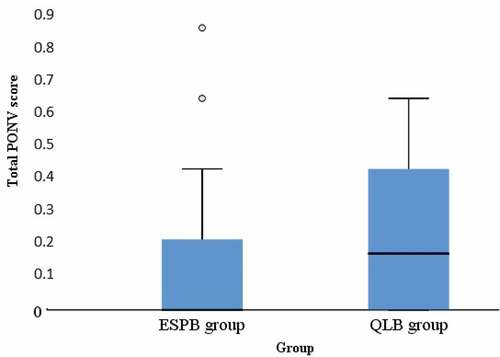
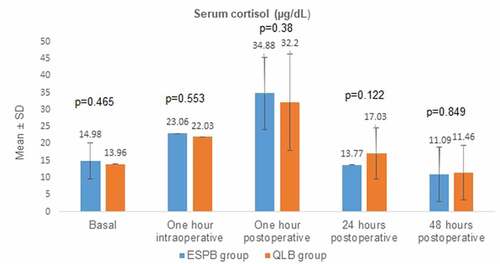
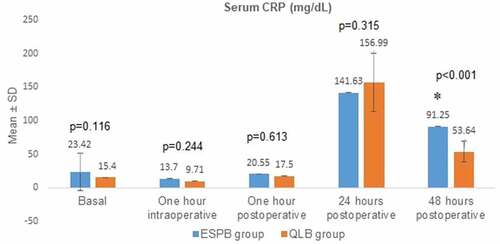
The erector spinae plane block provided lower mean pain scores assessed by NRS with statistically significant differences (p < 0.001) during rest and movement, less frequent and easily controlled breakthrough pain than the quadratus lumborum block. There was no difference between the two groups at the time of the first postoperative morphine dose. The mean ± SD values of cumulative morphine consumption after the first and second postoperative 24 hours were 7.24 ± 0.987 and 3.62 ± 0.493, respectively, in the ESPB group, while they were 14.26 ± 2.206 and 7.32 ± 1.007, respectively, in the QLB group. The mean total postoperative nausea and vomiting intensity score was lower in the ESPB group withoutstatistically significant difference. There were no statistically significant differences between the two groups in the mean postoperative serum levels of cortisol and CRP except for CRP after 48 hours, which was 91.25 ± 46.172 in the ESPB group and 53.64 ± 15.324 in the QLB group (p < 0.001).
Conclusion
The erector spinae plane block is an easy and effective opioid sparing analgesic technique. It is recommended to be a part of multimodal analgesia for open colorectal surgeries.
1. Introduction
Colorectal cancer (CRC) is one of the most common cancers worldwide [Citation1]. Open surgery is one of the treatment modalities of it. It is well known that surgery activates stress response that can be monitored by biomarkers such as as cortisol and C-reactive protein (CRP) [Citation2,Citation3]. Neural blockade, glucocorticoids, opioid analgesia and nonsteroidal anti-inflammatory drugs (NSAIDs) can provide opioid sparing multimodal analgesia and modulate stress response in CRC patients [Citation4–6]. Epidural analgesia is the gold standard perioperative analgesic technique for major abdominal surgeries [Citation7]. However, technical difficulties and complications related to the use of epidural catheters and its contradiction with the aspects of enhanced recovery after surgery (ERAS) protocols make seeking alternatives an important issue [Citation8–10]. The anterior trans-muscular quadratus lumborum block (QLB) is a truncal block (ventral rami of T7- L2) that produces its analgesic effect by blocking the thoracic sympathetic trunk, the ventral rami of lower spinal nerves, the sympathetic fibers and mechanoreceptors within the thoracolumbar fascia, and the celiac ganglion by spread via the splanchnic nerves [Citation11–13]. The erector spinae plane block (ESPB) targets the fascial plane between this muscle and the vertebral transverse processes. It has analgesic actions similar to the paravertebral block without the risks of pleural, neural or vascular injury [Citation14]. Dexamethasone combined with local anesthetics can prolong the duration of postoperative analgesia [Citation15]. Intravenous (IV) morphine titration provides the analgesic requirement of the patient rapidly while limiting the risk of over-dosage and side effects [Citation16]. Ketorolac is a Food and Drug Administration (FDA) approved NSAID with ideal opioid-sparing and antineoplastic properties in CRC patients [Citation5,Citation17]. Therefore, this study was conducted to find out the better regional block to be a part of multimodal analgesia for CRC surgical patients.
2. Patients and methods
This randomized, single blinded, prospective study was registered at clinical trial registry with code number (NCT03803267). The sample size was calculated using Power Analysis and Sample Size software program (PASS) version 15.0.5 for Windows (2017) using the results published by J. Lee and his colleagues [Citation18] with the post-operative pain score at rest after 24 hours as the primary outcome. A sample size of 34 patients in each group was needed to achieve 80% power to detect a mean difference of 0.7 between the two groups with estimated standard deviation of one for both groups using a two-sided two-sample equal-variance t-test with a significance level of 0.05.
After obtaining approval of the Institutional Review Board with code number (MD. 18.11.106), we started recruitment in May 1st, 2019 and completed the study in January 1st, 2020. Eighty patients who met the inclusion criteria and scheduled for CRC resection surgeries in Gastrointestinal Surgery Center, Mansoura, were enrolled in the study. Inclusion criteria included age between 40 and 60 years, either sex, ASA physical status Ι or ΙΙ, and BMI between 18.5 and 35 kg/m2. Exclusion criteria included age < 40 or > 60 years, BMI > 35 or <18.5 Kg/m2, ASA ≥ III, pregnancy, postpartum or lactating females, allergy to one of the agents used, local infection, coagulopathy, chronic use of opioids or corticosteroids, mental illness, or refusal to participate in the study. Four patients refused to participate in the study. The study subjects were randomly assigned to 2 equal groups using a computer generated table of random numbers. The patients were assessed for eligibility and written informed consents were obtained by one investigator during the preanesthetic interview on the day before surgery. Group allocation was contained in sequentially numbered, sealed opaque envelopes, which were opened by the primary investigator. The study subjects and outcome assessors were blinded about the study group. The CONSORT flow diagram is shown in ().
Group QLB (n = 38): bilateral ultrasound-guided anterior trans-muscular quadratus lumborum block.
Group ESPB (n = 38): bilateral ultrasound-guided erector spinae plane block.
Every patient in both groups received 20 ml of bupivacaine 0.25% with 4 mg dexamethasone for each side.
All patients were subjected to standard preoperative assessment. At 8 AM, on patient arrival at the pre-operative holding area, the standard monitoring was applied, the pain score was assessed by the numeric rating scale (NRS) and basal values were recorded. A 20 gauge IV cannula was inserted and IV drip of crystalloid solution was started. All patients received IV antibiotic prophylaxis and pre-medicated with IV 0.03 mg/kg midazolam as preoperative anxiolytic.
For anterior trans-muscular QLB, in prone position, the ultrasound machine (General Electric, LOGIQ e, China) was placed opposite to the operator in a position suitable for his ergonomics. Under strict aseptic precautions, a curved array US transducer (4C-RS 5–2 MHz) was placed transversely at the abdominal flank between the costal margin and iliac crest, immediately proximal to the iliac crest. The transducer was moved medially until the quadratus lumborum (QL) muscle was identified with its attachment to the lateral edge of the transverse process of the 4th lumbar vertebra. The psoas major muscle was identified anteriorly and the erector spinae muscle posteriorly with their attachments to the transverse process. After skin infiltration with 2 ml of lidocaine 2%, a 22-gauge, Quincke spinal needle was inserted in plane to the transducer (lateral edge) and was advanced through the quadratus lumborum muscle until piercing the ventral fascia propria of the QL muscle. The needle position was confirmed by injecting 5 ml normal saline 0.9% and visualizing the hydro-dissection. After aspiration, the local anesthetic solution was injected with visualization of psoas muscle compression. The same process was repeated for the other side [Citation19]. For ESPB, in prone position, the ultrasound machine (General Electric, LOGIQ e, China) was placed opposite to the operator in a position suitable for his ergonomics. Under strict aseptic precautions, the 8th thoracic spinous process was identified by counting down from the 7th cervical spinous process by palpation. Once located, a linear US transducer (12L-RS 12–4 MHz) was placed in the longitudinal plane over the spinous process and slipped laterally approximately 3 cm until the transverse process was identified with erector spinae and trapezius muscles overlying it. The skin was infiltrated by 2 ml of lidocaine 2% subcutaneously and a 22-gauge, Quincke spinal needle was advanced in plane in the cranio-caudal direction. When the needle contacted the transverse process, 5 ml saline 0.9% was injected to confirm correct needle placement by visualizing the linear pattern of hydrodissection. After aspiration, the local anesthetic solution was injected. The same process was repeated for the other side [Citation20].
After 30 minutes, the degree of sensory block was assessed by pinprick test for the anterior abdominal wall. When the pinprick was recognized as a touch by a blunt object or not recognized at all, this was considered a successful block; otherwise, the patient was excluded from the study. Any undesired motor weakness was recorded as a side effect.
After transferring the patient to the operation room, the standard monitoring was applied and the values were recorded. After pre-oxygenation, general anesthesia was slowly induced by IV 1.5 mg/kg propofol, 0.5 mg/kg atracurium and 1 µg/kg fentanyl. After endotracheal intubation, anesthesia was maintained by 1–1.5% isoflurane in an oxygen: air mixture ratio of 40:60 to keep hemodynamics within ±20% of basal values. Muscle relaxation was maintained by IV 0.2 mg/kg atracurium boluses for every half-life of 20 minutes. Mechanical ventilation parameters were adjusted to maintain the end-tidal CO2 (ETCO2) between 33 and 36 mm Hg. The surgery was started by lower para-median incision with supra-umbilical extension, then exploration, mobilization of the colon, resection, anastomosis, hemostasis, and, finally, abdominal wall closure. Hypotension was defined as mean blood pressure (MBP) < 60 mmHg and bradycardia as heart rate (HR) < 50 beats per minute. Hypotension was treated by IV boluses of 0.1 mg/kg ephedrine, and bradycardia was treated by IV 0.01 mg/kg atropine. At the end of surgery, isoflurane was discontinued, muscle relaxation was reversed by IV 50 μg/kg neostigmine and 10 μg/kg atropine, and the patient was extubated and transferred to the post-anesthesia care unit (PACU).
In the PACU, oxygen was administered, standard monitoring was applied, and readings were recorded. Pain intensity was monitored using the NRS for pain during rest and movement every 30 minutes for 2 hours as 0 for no pain and 100 for the worst pain, recovering from general anesthesia from the zeroth point of time. When NRS at rest became ≥ 40, the duration of analgesia was recorded and IV morphine titration was administered in a dose of 0.05 mg/kg to 4 mg maximally at 15-minute intervals until NRS became <40 or side effects as over-sedation or respiratory depression occurred. Over-sedation was defined as Ramsey sedation score (RSS) > 3, and respiratory depression was defined as respiratory rate < 10 breathes per minute. IV naloxone was ready for reversal of respiratory depression associated with the disturbed conscious level. After discharge from PACU, IV 30 mg Ketorolac was given every 12 hours, while IV morphine in a dose of 0.05 mg/kg to a maximum of 4 mg was given as rescue analgesic when NRS at rest persists to be ≥40. Postoperative nausea and vomiting (PONV) were assessed by the PONV intensity scale [Citation21]. It equals severity of nausea (1 = mild, 2 = moderate, 3 = severe) x pattern of nausea (1 = varying, 2 = constant) x duration of nausea in hours (whole or fraction). PONV was defined as clinically important when the score became ≥ 50 at any point of time. Scores were summated for the total score throughout the study period. IV 10 mg metoclopramide was given as rescue antiemetic if vomiting or persistent nausea occurred. Then, the patient was transferred to the intermediate care unit for monitoring and management throughout the study period. Peripheral venous blood samples of 5 ml were collected in the following time points: at 8 AM before injection of the anxiolytic, 1 hour after induction of general anesthesia, 1 hour after recovery from general anesthesia, and 24 hours and 48 hours, postoperatively. Blood samples were left to coagulate at room temperature for 30 minutes and centrifuged at 2500 rpm for 10 minutes, and then, serum was separated and frozen until assay. The serum cortisol level was estimated by the electro-chemiluminescence technique (Cobas e411, Roche, China), and the serum CRP level was estimated by particle enhanced turbidimetric immunoassay (Cobas integra 400 plus, Roche, China). The primary outcome was pain scores assessed by NRS during rest at 0, 30 minutes, 60 minutes, 90 minutes, 120 minutes, 2 hours, 6 hours, 10 hours, 14 hours, 18 hours, 24 hours, 32 hours, 40 hours and 48 hours postoperatively. The secondary outcomes included pain scores during movement, cumulative postoperative morphine consumption (mg), intensity of PONV, changes of stress response assessed by follow-up of serum cortisol (µg/dl) and CRP (mg/L), and duration of analgesia (hours). After that, the data were tabulated and statistically analyzed.
3. Statistical analysis
Statistical analysis of the collected data was done by IBM’s Statistical Package for the Social Science (SPSS) statistics for Windows (version 25). Microsoft Excel for Windows 2019 and SPSS’ chart builder were used for generation of charts. The normality of the data distribution was checked by the Shapiro–Wilk test. Mean ± standard deviation (SD) was used for the expression of normally distributed continuous variables, while abnormally distributed continuous variables and categorical ones were expressed in number and percentage or median and inter-quartile range (as appropriate). Normally and abnormally distributed continuous data were analyzed by the Student t-test and Mann–Whitney test, respectively. Categorical data were analyzed by the chi-square test using the crosstabs function. 95% confidence interval (95% CI) was used with conduction of all tests. Difference was considered statistically significant when the P (probability) value was < 0.05.
4. Results
Eight patients were excluded; three in the QLB group and one in the ESPB group due to failure of the block, which may be due to poor ultrasonic anatomical delineation caused by fatty flanks and low muscle mass, one in the QLB group and two in the ESPB group due to aborting of the surgery for advanced unresectable tumor, and one in the ESPB group due to inconsistent pathology with malignancy. Finally, 68 patients were statistically analyzed; the ESPB group (n = 34) and QLB group (n = 34). No case was lost to follow-up.
The demographic data are shown in . There were no statistically significant difference between the two groups with respect to age, gender, BMI, existence, and severity of comorbid diseases assessed by ASA physical status classification or duration of surgery.
Table 1. Demographic data of the patients in the studied groups
Postoperative NRS at rest is shown in . ESPB had statistically significant lower pain scores at nearly all time points except at basal and 14-hour time points.
Table 2. Post-operative numerical rating score during rest
Postoperative NRS during movement is shown in . ESPB had statistically significant lower pain scores at all-time points except at the basal time point.
Table 3. Post-operative numerical rating score during movement
Postoperative morphine consumption (mg) is shown in . ESPB had statistically significant lower cumulative consumption at both 24-hour and 48-hour time points.
Figure 2. Comparison of post-operative morphine consumption between the studied groups
The PONV intensity score is shown in . ESPB had a lower total PONV intensity score without statistical significance.
Figure 3. Comparison of total postoperative nausea and vomiting intensity score between the studied groups
The serum cortisol level (µg/dL) is shown in . There was no statistically significant difference between both groups at any time point.
Figure 4. Comparison of the serum cortisol level between the studied groups
Serum CRP (mg/L) is shown in . QLB had a statistically significant lower level at the 48-hour time point.
Figure 5. Comparison of the serum CRP level between the studied groups
All patients were given rescue analgesia upon recovery from general anesthesia. So, the duration of analgesia was related to the duration of surgery, whose difference was statistically insignificant (p = 0.372). No case had reported local anesthetic systemic toxicity, local hematoma or infection, lower limb weakness, hypotension, bradycardia, desaturation, respiratory depression or over-sedation.
5. Discussion
In this prospective, randomized study, the bilateral ESPB was a simple and effective analgesic technique for open CRC resection. The patients in this group had lower pain scores during rest and movement, and less opioid consumption and looked much more comfortable than patients in the group received bilateral anterior trans-muscular QLB. Dexamethasone is a commonly used local anesthetic adjuvant to prolong the duration of analgesia of regional anesthetic techniques with subsequent reduction of postoperative opioid consumption and its side effects [Citation22].
Although both groups had a satisfactory sensory block for anterior abdominal wall assessed by the pinprick test preoperatively, the patients in the QLB group had higher pain scores at almost all timepoints during rest and movement. They did not complain of incisional pain, but they usually recovered with severe colicky pain in the upper abdominal compartment. After administration of IV morphine, pain intensity decreased, but breakthrough pain was more frequent.
This agreed to some extent with what Rao and his colleagues found in their study, which included laparotomy surgeries. They observed a deficient sympathetic blockade and visceral analgesia in the QLB group despite continuous catheter infusion of the local anesthetic and fentanyl patient controlled analgesia (PCA) [Citation23]. However, this contradicted with many studies that gave the advantage of visceral and somatic analgesia to QLB. Lee and his colleagues found that QLB had equal analgesic effect on the paravertebral block during the first 24 hours in patients who underwent radical cystectomy. This can be explained by using higher local anesthetic concentration (ropivacaine 0.5%) with dexmedetomidine adjuvant and postoperative hydromorphone PCA. In addition, radical cystectomy is confined to the lowermost part of the abdomen and does not imply extensive visceral manipulation compared to colectomy surgeries [Citation18]. Zhu and his colleagues found that the QLB group had better analgesia than the control group in patients who underwent laparoscopic nephrectomy. They used intraoperative remifentanil IV infusion and postoperative sufentanil PCA [Citation24].
On the other hand, the patients in the ESPB group usually recovered with a heaviness or burning pain in the lower abdominal compartment. They more frequently expressed their pain as a desire to evacuate bowel or bladder despite urinary catheterization. They experienced their first colicky pain after postoperative 14 hours. This explains the absence of statistically significant difference in NRS during rest between both groups at this time point. However, their pain was easily controlled by either intravenous morphine or ketorolac with less frequent breakthrough pain. This agreed with many studies that proved adequate analgesic and opioid sparing efficacy of ESPB that was comparable to the paravertebral block and excelled many other blocks in different types of surgeries such laparotomy, laparoscopy, thoracotomy, thoracoscopy, nephrectomy, hepatectomy, distal esophagectomy, cesarean section and spine surgeries [Citation25]. Therefore, cumulative morphine consumption during first and second postoperative 24 hours was lower in the ESPB group than in the QLB group. Subsequently, the total PONV intensity score was lower in the ESPB group without statistically significant difference.
Pain observed in both groups can be explained by deficient coverage of the whole abdominal cavity, which requires blocking of the splanchnic and sacral pelvic nerves whose cell bodies are located in the thoracolumbar and lumbosacral dorsal root ganglia [Citation26].
There was no statistically significant difference in the serum cortisol level between both groups at any time point, reflecting the capability of surgical cortisol response to overcome the circadian rhythm and any inhibitory effect of analgesic techniques [Citation27]. The serum CRP level did not have a statistically significant difference between both groups except at the postoperative 48-hour time point. This can be explained by the absence of the important effect of neural blockade on inflammatory responses as they are independent of neural stimulation and pain [Citation4]. However, the significant difference observed at the postoperative 48-hour time point can be explained by the immunosuppressive properties of morphine whose cumulative consumption was higher in the QLB group [Citation28].
This study has some limitations. Firstly, NRS is a subjective indicator, but it is quick and easy [Citation29]. Secondly, the sample size is not large enough to determine small differences between the two blocks in terms of effects and complications. Thirdly, regional use of dexamethasone as a local anesthetic adjuvant is off-label, but we wanted to be sure about its delivery to the site of action as long as we did not exceed the ceiling dose, 4 mg [Citation30].
Despite these limitations, this study is important as it compares the QLB, whose body of literature is limited, with ESPB, which is a relatively novel analgesic technique in abdominal surgeries like colectomy. This study evaluates their analgesic efficacy alone without any adjuvant analgesics that could mislead the results. Additionally, it spots light on stress response and two of its biomarkers in an attempt for more objective evaluation and monitoring of immune competence and outcome in cancer surgical patients.
6. Conclusion
ESPB provides adequate analgesic coverage with lower pain scores, less frequent and easily controlled breakthrough pain, less cumulative morphine consumption, and lower intensity of postoperative nausea and vomiting than trans-muscular QLB. Therefore, ESPB is recommended to be a part of multimodal analgesia for open colorectal surgeries. Further studies are required for further monitoring of stress response, immune markers and long term outcome and implementation of multimodal analgesia as a part of ERAS protocols.
Data availability
The data used are available upon request
Ethics approval and informed consent
Approval was obtained by the Institutional Review Board with code number (MD. 18.11.106), Mansoura university, Egypt, and registered at ClinicalTrials.gov (ID: NCT03803267).
Consent for publication
Written informed consent was taken from all patients.
Acknowledgments
Thanks to my colleague, Ahmed El-shamy, for participation in statistical analysis of the data.
Disclosure statement
The authors report no financial or non-financial conflicts of interest in this work.
Supplementary material
Supplemental data for this article can be accessed here.
Additional information
Funding
References
- Mahfouz EM, Sadek RR, Abdel-Latief WM, et al. The role of dietary and lifestyle factors in the development of colorectal cancer: case control study in Minia, Egypt. Cent Eur J Public Health. 2014;22(4):215–222.
- Heaney A, Buggy D. Can anaesthetic and analgesic techniques affect cancer recurrence or metastasis? Br J Anaesth. 2012;109(suppl_1):i17–i28.
- Piazza JR, Almeida DM, Dmitrieva NO, et al. Frontiers in the use of biomarkers of health in research on stress and aging. J Gerontol B Psychol Sci Soc Sci. 2010;65(5):513–525.
- Kehlet H. Manipulation of the metabolic response in clinical practice. World J Surg. 2000;24(6):690–695.
- Schack A, Fransgaard T, Klein MF, et al. Use of nonsteroidal anti-inflammatory drugs decreases the risk of recurrence of cancer after colorectal resection: a cohort study based on prospective data. Ann Surg Oncol. 2019;26(12):3826–3837.
- Simpson JC, Bao X, Agarwala A. Pain management in Enhanced Recovery after Surgery (ERAS) protocols. Clin Colon Rectal Surg. 2019;32(2):121–128.
- Moraca RJ, Sheldon DG, Thirlby RC. The role of epidural anesthesia and analgesia in surgical practice. Ann Surg. 2003;238(5):663–673.
- Altinpulluk EY, Ozdilek A, Colakoglu N, et al. Bilateral postoperative ultrasound-guided erector spinae plane block in open abdominal hysterectomy: a case series and cadaveric investigation. Rom Anaesth Int Care. 2019;26(1):83–88.
- Lassen K, Soop M, Nygren J, et al. Consensus review of optimal perioperative care in colorectal surgery: Enhanced Recovery After Surgery (ERAS) group recommendations. Arch Surg. 2009;144(10):961–969.
- Gupta A, Björnsson A, Fredriksson M, et al. Reduction in mortality after epidural anaesthesia and analgesia in patients undergoing rectal but not colonic cancer surgery: a retrospective analysis of data from 655 patients in central Sweden. Br J Anaesth. 2011;107(2):164–170.
- Dam M, Moriggl B, Hansen CK, et al. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesth Analg. 2017;125(1):303–312.
- Kumar A, Sadeghi N, Wahal C, et al. Quadratus lumborum spares paravertebral space in fresh cadaver injection. Anesth Analg. 2017;125(2):708–709.
- Blanco R. Tap block under ultrasound guidance: the description of a “no pops” technique. Reg Anesth Pain Med. 2007;32(5):130. 271.
- Hamilton D, Manickam B. Erector spinae plane block for pain relief in rib fractures. Br J Anaesth. 2017;118(3):474–475.
- YaDeau JT, Paroli L, Fields KG, et al. Addition of dexamethasone and buprenorphine to bupivacaine sciatic nerve block: a randomized controlled trial. Reg Anesth Pain Med. 2015;40(4):321–329.
- Aubrun F, Mazoit JX, Riou B. Postoperative intravenous morphine titration. Br J Anaesth. 2012;108(2):193–201.
- Vadivelu N, Gowda AM, Urman RD, et al. Ketorolac tromethamine–routes and clinical implications. Pain Pract. 2015;15(2):175–193.
- Lee AJ, Yabes JG, Hale N, et al. The comparative effectiveness of quadratus lumborum blocks and paravertebral blocks in radical cystectomy patients. Can J Urol. 2018;25(2):9255–9261. PMID: 29680003.
- Abduallah MA, Ahmed SA, Abdelghany MS. The effect of post-operative ultrasound-guided transmuscular quadratus lumborum block on post-operative analgesia after hip arthroplasty in elderly patients: a randomised controlled double-blind study. Indian J Anaesth. 2020;64(10):887–893.
- Luis-Navarro JC, Seda-Guzmán M, Luis-Moreno C, et al. Erector spinae plane block in abdominal surgery: case series. Indian J Anaesth. 2018;62(7):549–554.
- Wengritzky R, Mettho T, Myles PS, et al. Development and validation of a postoperative nausea and vomiting intensity scale. Br J Anaesth. 2009;104(2):158–166.
- Choi S, Rodseth R, McCartney CJ. Effects of dexamethasone as a local anaesthetic adjuvant for brachial plexus block: a systematic review and meta-analysis of randomized trials. Br J Anaesth. 2014 Mar;112(3):427–439.
- Rao Kadam V, Ludbrook G, van Wijk R, et al. Comparison of ultrasound‐guided transmuscular quadratus lumborum block catheter technique with surgical pre‐peritoneal catheter for postoperative analgesia in abdominal surgery: a randomised controlled trial. Anaesthesia. 2019;74(11):1381–1388.
- Zhu M, Qi Y, He H, et al. Analgesic effect of the ultrasound-guided subcostal approach to transmuscular quadratus lumborum block in patients undergoing laparoscopic nephrectomy: a randomized controlled trial. BMC Anesthesiol. 2019;19(1):1–8.
- Tulgar S, Ahiskalioglu A, De Cassai A, et al. Efficacy of bilateral erector spinae plane block in the management of pain: current insights. J Pain Res. 2019;12:2597–2613.
- Grundy L, Erickson A, Brierley SM, et al. Visceral pain. Annu Rev Physiol. 2019;81(1):261–284.
- Prete A, Yan Q, Al‐Tarrah K, et al. The cortisol stress response induced by surgery: a systematic review and meta‐analysis. Clin Endocrinol. 2018;89(5):554–567.
- Kurosawa S, Kato M. Anesthetics, immune cells, and immune responses. J Anesth. 2008;22(3):263–277.
- Aubrun F, Paqueron X, Langeron O, et al. What pain scales do nurses use in the postanaesthesia care unit?. Eur J Anaesthesiol. 2003;20(9):745–749.
- Kirkham KR, Jacot-Guillarmod A, Albrecht E. Optimal dose of perineural dexamethasone to prolong analgesia after brachial plexus blockade: a systematic review and meta-analysis. Anesth Analg. 2018;126(1):270–279.