?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.
?Mathematical formulae have been encoded as MathML and are displayed in this HTML version using MathJax in order to improve their display. Uncheck the box to turn MathJax off. This feature requires Javascript. Click on a formula to zoom.ABSTRACT
Background
Femoral nerve block (FNB) is a prevalent technique for analgesia following knee surgeries, but it also results in quadriceps weakness and greater chances of falling. Adductor canal block (ACB) is advertised as a motor nervesparing alternative to FNB.
Objectives
The aim of the study was to compare adductor canal block with femoral nerve block as regard different surgical procedures of the knee.
Study design
Meta-analysis was used to address this concern.
Sittings
Meta-analysis-based study following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.
Methods
The database MEDLINE, EMBASE, PubMed, and Cochrane were systemically searched to detect all published randomized and prospective clinical trials comparing adductor canal block with femoral nerve block as regard different surgical procedures of the knee in the last five years.
Results
Eighteen studies were identified for inclusion in this study, involving a total of 1457 patients. The risk of bias was low. Meta-analysis revealed that groups receiving femoral nerve blocks experience a significant decrease in pain scores and analgesic medication usage. However, adductor canal block groups have a significantly lower rate of quadriceps muscle weakness than FNB groups.
Conclusion
Femoral nerve block provides more analgesia and reduces analgesic consumption. On the other hand, adductor canal block, in the early postoperative period, preserves quadriceps function.
The diversity of surgical procedures available for the knee results in postoperative pain ranging from mild to severe. Numerous techniques for determining the best analgesics for these procedures have been used. The type and duration of surgical intervention, as well as the patient’s age, all influence the postoperative pain response. Thus, the anesthesiologist can select the most appropriate analgesic regimen for each patient during and after surgery [Citation1]. Postoperative pain can impair early ambulation and length of stay in the hospital following knee surgeries. Postoperative pain that is not relieved can result in psychological and clinical changes that impair one’s quality of life [Citation2]. Adequate analgesia with preservation of motor function became the primary goal following knee surgery. Numerous options, including regional analgesics (i.e., neuraxial and peripheral) and systemic analgesics (i.e., opioid and non-opioid), are present for postoperative pain management. Multimodal analgesia is achieved through the combination of several painkillers acting at various sites in the nervous system and via distinct mechanisms [Citation3]. Numerous regional analgesic techniques were used to provide analgesia during and following knee surgery, particularly femoral nerve blockade (FNB). As regards postoperative pain management, FNB is a good choice [Citation4,Citation5]. However, FNB frequently results in quadriceps muscle motor blockade, which may postpone postoperative mobilization and increases the chances of falling [Citation6]. The addition of an adductor canal block (ACB) is a relatively recent procedure. When compared to FNB, it causes a lesser reduction in quadriceps muscle strength [Citation7,Citation8]. ACB has been shown to be effective in clinical trials investigating its effectiveness in knee operations [Citation9,Citation10]. Additionally, several meta-analyses on the use of ACB in knee surgeries have been published [Citation11–13]. Taking into account the anatomical evidence, we can suggest that ACB might be more advantageous than FNB. However, the results of previous studies that compared FNB and ACB did not entirely verify the previously mentioned evidence. Thus, the present study aimed to compare the clinical efficacy of ACB and FNB for analgesia following knee surgeries and comparing quadriceps muscular strength between two groups from the perspective of a systematic review with meta-analysis, which pooled outcomes with a small sample size into a larger sample size.
1. Methods
This study followed the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [Citation14].
2. Search strategy and selection criteria
MEDLINE, EMBASE, PubMed, and Cochrane were used to identify all published randomized and prospective clinical studies (between 2015 and 2020) comparing femoral nerve block and adductor canal block as regard various surgical procedures of the knee. The following search terms were used to identify relevant articles: “Femoral nerve block” and “Adductor canal block.” Studies were limited to human and English language studies. Reference lists of related articles were also reviewed. Institutional Review Board approval was not necessary for this study.
3. Exclusion criteria
Studies were excluded when their data were missing or inadequate, or if their authors were unavailable or did not respond when more data from their trials were requested, or if their results were considered unnecessary.
4. Data extraction
The first author, the year of publication, the study design, sample size, and setting of each included randomized trial, as well as any outcomes of interest, were extracted from the included trials. Pain score at 6, 12, 24, and 48 hours was the primary outcome of this research. Secondary outcomes included analgesia consumption and quadriceps muscle strength.
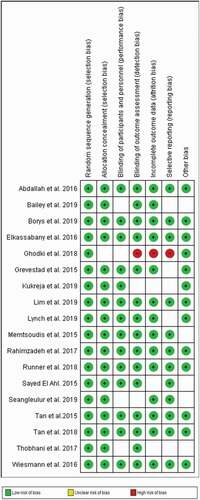
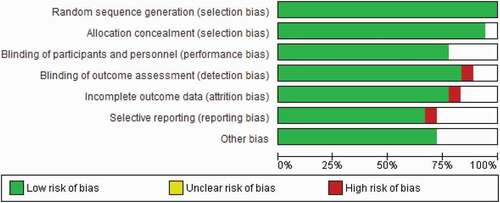
5. Quality assessment and bias risk
Using the Cochrane Collaboration’s approved risk of bias method, the quality of trials was assessed [Citation15]. We estimated the following elements as high, unclear, or low: inadequate outcome data, selective reporting, random sequence generation, blinding, allocation concealment, and other bias. Disagreements were identified and handled by discussion.
6. Statistical analysis
We used Review Manager (RevMan), Version 5.3, Copenhagen (The Nordic Cochrane Centre, The Cochrane Collaboration, 2014) to aggregate the findings of studies comparing adductor canal block versus femoral nerve block for various knee surgery procedures. Pain scores at 6, 12, 24, and 48-hours postoperative were the primary comparison themes. Secondary comparison themes included analgesia consumption and quadriceps muscle strength. We assumed that the mean and median were equal in studies that reported only the interquartile range (IQR) for continuous measure outcomes. By dividing the IQR by 1.35, we obtained the standard deviation (SD) [Citation16].
For studies reporting only the mean and the confidence interval (CI) to measure outcomes, we calculated the standard deviation from CI and sample size (N) according to the following equation described in Cochrane Handbook for Systematic Reviews of Interventions:
Using the I2 statistic, heterogeneity was determined. Pooling findings were accomplished using random-effects models. For continuous outcomes, the mean difference (MD) and associated 95% confidence intervals were computed (CIs). Statistical significance was defined as a two-sided value α of 0.05, while clinical significance was interpreted with an emphasis on confidence intervals (CIs).
7. Results
7.1. Search results
Our search identified 153 studies through database searching and other sources. Of these articles, 57 were excluded after duplicates removal. There were 96 articles screened. After screening, 72 articles were eliminated, and 24 were judged for eligibility. Finally, 18 randomized controlled trials were included in the analysis, with the remaining being eliminated according to the PRISMA flow diagram ().
8. Quality and characteristics of clinical studies included in the meta-analysis
summarizes the studies involved in the analysis. Eighteen studies were identified for inclusion in this study, involving a total of 1457 patients. Of which 11 were RCTs [Citation17–27]. All papers were published between 2015 and 2019 – the data extraction process was agreed upon by all reviewers.
Table 1. Characteristics of included studies
Bias risk in the eighteen trials was assessed to be generally low (, b))
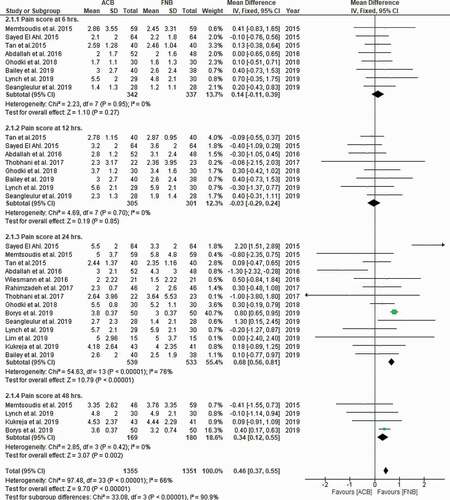
.9. Pain scores at 6, 12, 24, and 48 hours
The forest plot diagrams () showed that the FNB result in a significant decrease in pain scores. (Mean difference = −0.46 [0.37, 0.55]; 95% CI; I2 = 90.9%; P = 0.00001)
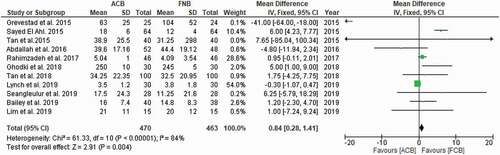
10. Analgesia consumption
The forest plot demonstrates the significant decrease in consumption of analgesic drugs in FNB group ((Mean difference = 0.84 [0.28, 1.41]; 95% CI; I2 = 84%; P = 0.004) ()
11. Quadriceps muscle strength
Although most of the included studies favor significantly less quadriceps muscle weakness in ACB groups than those in FNB groups, the meta-analysis was unable to be conducted since the majority of these research employed different techniques for comparing muscular strength between groups. This heterogeneity of data impedes the analysis of this outcome.
12. Discussion
Almost all knee surgeries result in moderate-to-severe postoperative pain, making sufficient analgesia critical for postoperative analgesia and early mobility while preserving motor function, which is required for fast recovery. FNB offers adequate postoperative analgesia but decreases the quadriceps muscle strength and raises the chances of falling following surgery. ACB is better due to its ability to preserve motor function while providing sufficient analgesia. So, this research was conducted to determine if ACB was superior to FNB in terms of muscular strength, pain management, and side effects. ACB is an excellent alternative to FNB in postknee surgeries, as demonstrated by the meta-analysis of RCTs. This meta-analysis assessed pain VAS scores throughout a broader range of follow-up times (e.g., post-anesthesia, 2, 4, 6–8, 12, 24, 48, and 72 h). Comparisons of pain scores between ACB and FNB indicate that ACB has a substantially same analgesic effect as FNB. In this analysis, we included RCTs that assessed pain scores at various time periods. Based on the results of 18 trials, ACB and FNB showed no significant difference in pain scores at 6 hours and 12 hours. At 24 and 48 hours, the FNB resulted in a significant decrease in pain scores. In this study, we found that five studies showed that FNB is better than ACB in pain control as there is a decrease in VAS at 8,24,48 h in FNB than ACB [Citation18,Citation22,Citation23,Citation28,Citation29]. Other studies included in this metanalysis suggest that no significant difference in analgesic effect between FNB&ACB in postoperative 24,48 h or at knee flexion [Citation20,Citation24,Citation25,Citation30]. The two groups showed no significant difference in pain scores in a meta-analysis done by Min et al. [Citation31].
On the other hand, a trial done by Lynch et al. [Citation26] showed that the ACB had less VAS at 4 hours postoperative and less opioid consumption than FNB. We found in our meta-analysis that there is a decrease in consumption of analgesic drugs in the FNB group than ACB group. Still, there is no significant difference in opioid associated adverse effects, but [Citation26,Citation31] found that, between the two groups, no significant differences in opioid consumption or side effect was found. The present debate over quadriceps strength recovery focuses on whether ACB may generate results that are superior to or comparable to those obtained with FNB. After evaluating the included research, we concluded that this disagreement most likely arises from the fact that separate studies used different scales or assessment systems. We just reported the outcomes due to the fact that the data were not accessible for meta-analysis.
Mobilization ability is an indicator for muscular strength recovery, and the majority of the trials included in this meta-analysis found that patients who received ACB showed superior results in terms of mobilization abilities. Additionally, there is greater conservation of quadriceps muscular strength than with FNB. Early ambulation has been found to reduce deep venous thrombosis (DVT), improve muscular strength, and shorten hospital stays. The length of hospital stay has a direct correlation with postoperative problems. However, our meta-analysis revealed no statistically significant difference between the two groups regarding the length of hospital stay because multiple variables, including body mass index, age, and physiological state, might influence the length of stay in the hospital.
Regarding ACB &FNB, no significant difference in the Quadriceps strength or functional recovery was found by Lim et al. [Citation25], Wiesmann et al. [Citation32], and Xin et al. [Citation33].
Edwards et al. [Citation34] meta-analysis which done by eight randomized controlled trials on and gets data from 655 patient suggest that ACB preserve the quadriceps muscle function only in the early postoperative period.
13. Limitations
There are several limitations of this study due to limited long-term follow-up and using different functional measures. We reasoned that this disagreement might have been triggered by the use of various time points for evaluation. The number of trials included and the sample size of these trials were limited, which may have introduced bias. Also, heterogeneity among studies in reporting Quadriceps muscle strength variable made uniform comparison difficult. To decide whether ACB provides superior functional recovery compared with FNB, further studies are required.
14. Conclusion
FNB results in better analgesia and less analgesic consumption than
Disclosure statement
The authors declare that they have no conflicts of interest. This work was not subject to ethical review. The findings provided in this paper have not been previously published in their entirety or in part.
Correction Statement
This article has been republished with minor changes. These changes do not impact the academic content of the article.
References
- Espelund M, Grevstad U, Jaeger P, et al. Adductor canal blockade for moderate to severe pain after arthroscopic knee surgery: a randomised controlled trial. Acta Anaesthesiol Scand. 2014;58:1220–1227. 12407.
- Carr DB, Goudas LC. Acute pain. Lancet. 1999;353(9169):2051–2058. 13-9.
- Slover J, Riesgo A, Payne A, and Umeh U. Modern anesthesia for total joint arthroplasty. Ann. Orthop. Rheumatol. 2014;2: 1026.
- Chelly JE, Greger J, Gebhard R, et al. Continuous femoral blocks improve recovery and outcome of patients undergoing total knee arthroplasty. J Arthroplasty. 2001;16(4):436–445.
- Paul JE, Arya A, Hurlburt L, et al. Femoral nerve block improves analgesia outcomes after total knee arthroplasty: a metaanalysis of randomised controlled trials. Anesthesiology. 2010;113(5):1144–1162.
- Sharma S, Iorio R, Specht LM, et al. Complications of femoral nerve block for total knee arthroplasty. Clinical Orthopaedics & Related Research. 2010;468(1):135–140.
- Jæger P, Nielsen ZJK, Henningsen MH, et al. Adductor Canal Block versus Femoral Nerve Block and Quadriceps Strength. Anesthesiology118. 2013;118(2):409–415.
- Kwofie MK, Shastri UD, Gadsden JC, et al. The effects of ultrasound-guided adductor canal block versus femoral nerve block on quadriceps strength and fall risk: a blinded, randomised trial of volunteers. Regional Anesthesia and Pain Medicine. 2013;38(4):321–325.
- Jaeger P, Grevstad U, Henningsen MH, et al. Effect of adductor-canal-blockade on established, severe post-operative pain after total knee arthroplasty: a randomised study. Acta Anaesthesiologica Scandinavica. 2012;56(8):1013–1019.
- Jenstrup MT, Jæger P, Lund J, et al. Effects of adductor-canal-blockade on pain and ambulation after total knee arthroplasty: a randomised study. Acta Anaesthesiol Scand. 2012;56(3):357–364.
- Kuang M-J, Ma J-X, Fu L, et al. Is adductor canal block better than femoral nerve block in primary total knee arthroplasty? A GRADE analysis of the evidence through a systematic review and meta-analysis. J Arthroplasty. 2017;32(10):3238–3248.
- Kuang M-J, Xu L-Y, Ma J-X, et al. Adductor canal block versus continuous femoral nerve block in primary total knee arthroplasty: a meta-analysis. International Journal of Surgery. 2016;31:17–24.
- Li D, Yang Z, Xie X, et al. Adductor canal block provides better performance after total knee arthroplasty compared with femoral nerve block: a systematic review and meta-analysis. International Orthopaedics. 2016;40(5):925–933.
- Moher D, Liberati A, Tetzlaff J, et al. The PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6(7):e1000097.
- Higgins JPT, Altman DG, Gøtzsche PC, et al. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011;343(oct18 2):d5928.
- Wan X, Wang W, Liu J, et al. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14(1):135.
- Grevstad U, Mathiesen O, Valentiner LS, et al. Effect of Adductor Canal Block Versus Femoral Nerve Block on Quadriceps Strength, Mobilization, and Pain After Total Knee Arthroplasty. Regional Anesthesia and Pain Medicine. 2015;40(1):3–10.
- El Ahl MS. Femoral nerve block versus adductor canal block for postoperative pain control after anterior cruciate ligament reconstruction: a randomized controlled double blind study. Saudi J Anaesth. 2015;9(3):279–282.
- Memtsoudis SG, Yoo D, Stundner O, et al. Subsartorial adductor canal vs femoral nerve block for analgesia after total knee replacement. Int Orthop. 2015;39(4):673–680.
- Abdallah FW, Whelan DB, Chan VW, et al. Adductor canal block provides noninferior analgesia and superior quadriceps strength compared with femoral nerve block in anterior cruciate ligament reconstruction. Anesthesiology. 2016;124(5):1053–1064.
- Runner RP, Boden SA, Godfrey WS, et al. Quadriceps Strength Deficits After a Femoral Nerve Block Versus Adductor Canal Block for Anterior Cruciate Ligament Reconstruction: a Prospective, Single-Blinded, Randomized Trial. Orthopaedic Journal of Sports Medicine. 2018;6(9):2325967118797990.
- Tan Z, Kang AP, Pei F, et al. A comparison of adductor canal block and femoral nerve block after total-knee arthroplasty regarding analgesic effect, effectiveness of early rehabilitation, and lateral knee pain relief in the early stage. Medicine (Baltimore). 2018 Nov;97(48):e13391.
- Borys M, Domagała M, Wencław K, et al. Continuous femoral nerve block is more effective than continuous adductor canal block for treating pain after total knee arthroplasty. A randomized, double-blind, controlled trial. Medicine (Baltimore). 2019Sep;98(39):e17358. PMCID: PMC6775428. PMID: 31574881.
- Kukreja P, Bevinetto C, Brooks B, et al. Comparison of Adductor Canal Block and Femoral Nerve Block for Early Ambulation After Primary Total Knee Arthroplasty: a Randomized Controlled Trial. Cureus. 2019Dec;11(12):e6331. PMCID: PMC6948094. PMID: 31938621.
- Lim YC, Quek H, Phoo W. How Yow Kelvin Quek, Wai Heng Jimmy Phoo, Chou Liang Mah, and Shumei Tan, BPhysio (Hons). A randomised controlled trial comparing adductor canal block and femoral nerve block for knee arthroplasty. Singapore Medical Journal. 2019Mar;60(3):145–149. PMCID: PMC6441689. PMID: 30009316.
- Lynch JR, Okoroha KR, Lizzio V, et al. Adductor canal block versus femoral nerve block for pain control after anterior cruciate ligament reconstruction: a prospective randomized trial. Am J Sports Med. 2019;47(2):355–363.
- Bailey L, Griffin J, Elliott M, et al. Adductor canal nerve versus femoral nerve blockade for pain control and quadriceps function following anterior cruciate ligament reconstruction with patellar tendon autograft: a prospective randomized trial. Arthroscopy. 2019;35(3):921–929.
- Tan Z, et al. The effect of adductor canal block and femoral nerve block under multimodal analgesia for early analgesic effect and re-habilitation after total knee replacement (Chinese). Chin J Orthop. 2015;35.
- Poupak Rahimzadeh P, Faiz HR, Imani F, et al. Relieving pain after arthroscopic knee surgery: ultrasound-guided femoral nerve block or adductor canal block? Turkish Journal of Anesthesia and Reanimation. 2017Aug;45(4):218–224. PMCID: PMC5579215. PMID: 28868169.
- Ghodki PS, Shalu PS, Sardesai SP. Ultrasound-guided adductor canal block versus femoral nerve block for arthroscopic anterior cruciate ligament repair under general anesthesia. J Anaesthesiol Clin Pharmacol. 2018;34(2):242–246.
- Min H, Ouyang Y, Chen G. Anterior cruciate ligament reconstruction with the use of adductor canal block can achieve similar pain control as femoral nerve block. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-020-05933-6
- Wiesmann T, Piechowiak K, Duderstadt S, et al. Continuous adductor canal block versus continuous femoral nerve block after total knee arthroplasty for mobilisation capability and pain treatment: a randomised and blinded clinical trial. Arch Orthop Trauma Surg. 2016;136(3):397–406.
- Xin J, Yabing Z, Li Q, et al. Adductor canal block is similar to femoral nerve block for the quality of rehabilitation after arthroscopic partial meniscectomy. Knee Surg Sports Traumatol Arthrosc. 10.1007/s00167-019-05796-6
- Edwards MD, Bethea JP, Hunnicutt JL, et al. Effect of Adductor Canal Block Versus Femoral Nerve Block on Quadriceps Strength, Function, and Post-operative Pain After Anterior Cruciate Ligament Reconstruction. A Systematic Review of Level 1 Studies. Am J Sports Med. 2019;1–9. 10.1177/0363546519883589
- Elkassabany NM, Antosh S, Ahmed M, et al. The Risk of Falls After Total Knee Arthroplasty with the Use of a Femoral Nerve Block Versus an Adductor Canal Block: a Double-Blinded Randomized Controlled Study. Anesth Analg. 2016May;122(5):1696–1703. PMID: 27007076.
- Thobhani S, Scalercio L, Ce E, et al. Novel regional techniques for total knee arthroplasty promote reduced hospital length of stay: an analysis of 106 patients. Ochsner J. 2017;2017(17):233–238.
- Seangleulur A, Manuwong S, Chernchujit B, et al. Comparison of post-operative analgesia between adductor canal block and femoral nerve block after arthroscopic anterior cruciate ligament reconstruction: a randomised controlled trial. J Med Assoc Thai. 2019;102(3):335–342.