ABSTRACT
Background
Ultrasonography is the first diagnostic tool used to diagnose lower extremities deep venous thrombosis, which represents a significant healthcare burden worldwide. In this study, we assess the sensitivity and specificity of the three-point compression ultrasonography performed by emergency physicians for diagnosis of deep vein thrombosis (DVT) were assessed.
Methods
One hundred patients were enrolled in a prospective cross-sectional study that was performed at the emergency department (ED) at Alexandria Main University Hospital after application of predefined criteria of Wells score. Every patient was examined twice, first by the emergency resident, and the second by radiology resident. Time to scan and duration of scan were calculated for both scans.
Results
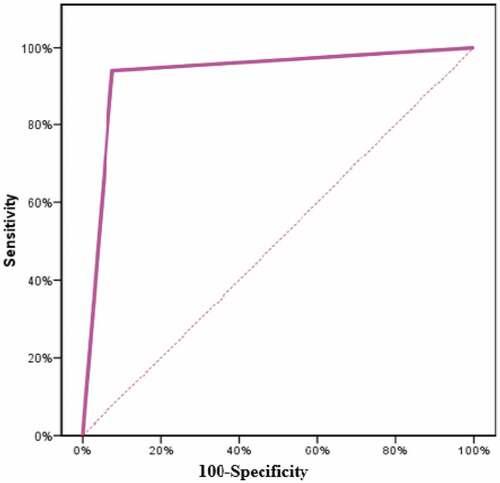
There was a statistically significant relation between the duration to emergency department ultrasound and formal radiology Doppler (p = 0.001). Also, there was no statistically significant difference between the positivity of ED ultrasound and the results of formal Doppler with p = 0.453. In the analysis of the receiver operating characteristics (ROC) area under the ROC curve of 0.933* (95% CI: 0.874–0.992, p < 0.001) (sensitivity was 94.12%, specificity was 92.42%, and accuracy was 93.0%).
Conclusion
The ED Doppler ultrasound is a highly sensitive, highly specific, and accurate diagnostic tool, which can be conducted after shorter duration of admission to the ED. It can be used for faster clinical decision-making to decrease overcrowding at both the emergency and radiology departments to save time and allow early diagnosis and management.
1. Introduction
Lower extremities deep vein thrombosis (LEDVT) is one of the major preventable causes of morbidity and mortality worldwide. The incidence of venous thromboembolism (VTE) is estimated to be 1 per 1,000 people annually. [Citation1,Citation2]
Recent European population studies reported a deep vein thrombosis (DVT) incidence of 70–140 cases /100,000 person-year. [Citation3]
Emergency department ultrasound (EDUS) is now widely used by emergency physicians for the detection and evaluation of different pathologies. [Citation4] It is listed as one of the core emergency skills in the most recent American College of Emergency Physicians (ACEP) emergency ultrasonographic guidelines. [Citation5,Citation6]
Sending a patient for formal Doppler ultrasound interpreted by radiology residents takes at least 3 hfrom triage. [Citation7]
Availability of bedside DVT ultrasound can decrease the length of patient stay in the emergency department (ED) and decrease the time to diagnosis of DVT. [Citation8–10]
1.1. Aim of the work
The primary aim of this study was to evaluate the sensitivity and specificity of three-point compression ultrasonography test performed by emergency medicine residents for detection of LEDVT.
The secondary aim of this study was to compare the time lapsed from triage till the patient is seated for the scan whether in the ED or radiology department, and the duration of the scan itself between both the emergency and radiology residents.
In addition to observing the learning curve of emergency physicians who were trained on EDUS, we compared the results of their scans with those of the radiology residents.
2. Patients and methods
2.1. Study population
This prospective cross-sectional study included 100 patients presented to the ED at Alexandria Main University Hospital (AMUH) who were suspected to have LEDVT.
Inclusion criteria:
Age > 18 years.
Acute unilateral or bilateral limb swelling.
Wells score, more than one point. [Citation11]
Exclusion criteria:
Long bone fracture at the affected limb.
Chronic lower limb swelling.
Patients with chronic peripheral vascular diseases.
Patients who have an inserted femoral catheter.
Severe lower limb pain, agitation.
All patients were subjected to
Initial evaluation, including medical, surgical and family history, physical examination, Wells score, and coagulation profile.
Local examination of the lower limb suspected for DVT.
2.2. Imaging technique
All enrolled patients were examined twice; the first was on admission to the ED, which was done by third-year emergency medicine residents, who were trained through having 10 h point of care ultrasound (POCUS) course 3 months before starting the study through which they applied what they learned in the course on a variety of patients including focused assessment sonography for trauma (FAST) and extended Focused assessment sonography for trauma (e FAST), chest ultrasound, and finally compression sonography in patients with suspected DVT.
The second by the radiology department residents, who performed the formal Doppler examination and were blinded from the results of EDUS.
Results obtained from emergency physicians in different shifts and at different times during the day including weekends and vacations were compared to those obtained by radiology physicians.
Moreover, all scans obtained from both the emergency and radiology physicians were either supervised with senior attendees from both departments or saved on the machines and further revised by the senior attendees in both departments on the following day. Both attendees were also blinded to their results.
Three-point compression test was performed using a portable ultrasound machine using portable DC-30 (MINDRAY, Biomedical Electronics, Hamburg, Germany) diagnostic ultrasound machine equipped with a 7.5–10 MHz linear-array transducer. And for obese patients, a 3.5 MHz curvilinear transducer will be used.
Suspected lower limb was examined at three points: common femoral vein (CFV), sapheno-femoral junction, and popliteal vein.
After taking patient consent and assurance of privacy, patient was laid supine and entire leg was exposed till the inguinal ligament and the hip slightly rotated externally. The probe was maintained perpendicular and adherent to the skin.
Examination of common femoral and Sapheno-femoral junction: Starting with the probe transverse and the pointer to the patient’s right, the inguinal ligament was identified, the common femoral artery and cCFV just below it. Pressure was applied until CFV was completely compressed or until the visualization of an echogenic structure within the lumen of the vein. Then, the transducer was rotated longitudinally, 2–3 cm distally along the sapheno-femoral junction, compression was done until completely compressed or until visualization of a thrombus.
Examination of popliteal vein: The patient was still supine and entire leg still exposed. Then, the knee was semi-flexed with the heel of the patient just touching the bed. For identification of popliteal artery and popliteal vein in popliteal fossa, the probe was placed in transverse plane, the pointer to the patient’s right, compression was applied until the vein was fully compressed or until visualization of a thrombus. The popliteal vein was more superficial than the artery, so less pressure was required to visualize it than that needed for the CFV.
Complete venous compressibility excludes the presence of DVT. Partial compressibility, total non-compressibility, or presence of hyper-echoic lesion inside the examined vein indicated the presence of DVT.
The time to scan and duration of scan were calculated and recorded starting from the patient triaging until both EDUS and radiology department Doppler were done.
2.3. Statistical analysis
Data were fed to the computer and analyzed using IBM SPSS software package version 20.0. (IBM Corp, Armonk, NY). Qualitative data were described using number and percent. The Kolmogorov–Smirnov test was used to verify the normality of distribution. Quantitative data were described using range (minimum and maximum), mean, standard deviation, median, and interquartile range (IQR). Significance of the obtained results was judged at the 5% level.
McNemar test was used to analyze the significance between the different stages. Wilcoxon signed-rank test was used for abnormally distributed quantitative variables to compare between two periods. Differences with p-values < 0.05 were considered statistically significant.
3. Results
The overall sensitivity of the three-point compression test done by emergency resident at the ED was (94.12%), specificity was (92.42%), and accuracy was (93.0%) with positive predictive value (PPV) (86.49%) and negative predictive value (NPV) (96.83%).
This study included 100 patients. The results of the three-point compression test at the ED were positive in 37% and negative in 63%. While during formal radiological examination only 34% of the patients were confirmed positive for LEDVT.
The 3% false-positive cases were in the popliteal vein, which is a deep vein difficult to clearly visualize in obese patients. Moreover, there is a difference in the machines used in both departments. Machines in the radiology department are technically advanced and higher resolution than those in the ED.
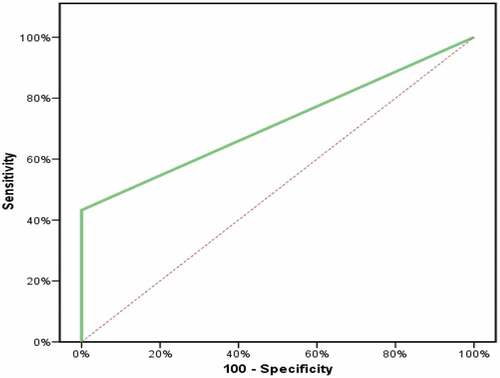
The sensitivity of D-dimer was 43.24%, while the specificity was 100.0%, with PPV (100%), NPV (75%), and accuracy (79%). The receiver operating characteristics (ROC) curve for the D-dimer () showed that it was a significant fair tool to diagnose DVT with area under the ROC curve (AUC) of 0.716* (95% CI: 0.602–0.830, p= <0.001*).
For correlation between the D-dimer and the EDUS, patients were divided as follows: 84 patients (84%) had D-dimer <500 ng/ml and 16 patients (16%) had D-dimer >500 ng/ml. There was a statistically significant relationship between D-dimer and EDUS, p-value < 0.001.
shows a statically significant difference between the clinical suspicious of LEDVT using the Wells score and the results of EDUS three-point compression as regards the presence or absence of LEDVT. 76.2% were false positive by Wells score, while 2.7% were false negative.
Table 1. Correlation between emergency department ultrasound, Wells score
shows that the mean time from patient triage until seated for the scan in the ED was 38.8 min compared to 74.4 min in the radiology department. Also, the mean time spent to perform the scan itself by emergency physicians was 6.68 min compared to 5.76 min for the radiology physicians.
Table 2. Comparison between the EDUS and formal Doppler according to duration to scan and duration of scan
demonstrates that the three-point compression test performed by emergency physicians was similarly accurate to those performed by radiology physicians.
Table 3. Comparison between positivity of the EDUS and radiology at the three sites of examination (femoral, saphenous, and popliteal vein)
EDUS is a significantly excellent tool to diagnose DVT in the lower extremities with AUC of 0.933* (95% CI: 0.874–0.992, p< 0.001) as shown in and .
Table 4. Sensitivity, specificity, and accuracy of the three-point compression test done at the emergency department
4. Discussion
LEDVT represents a significant healthcare burden. Early detection and initiation of anticoagulant therapy are important to prevent complications and reduce morbidity and mortality. [Citation12]
Compression ultrasonography is a first-line imaging tool for diagnosis of LEDVT. It is safe, non-invasive, cost-effective, and repeatable tool [Citation13,Citation14].
In the current research, the D-dimer as a clinical predictor for DVT was studied. D-dimer appeared to be a good negative, specific (100%) but low sensitive (43.24%) and moderately accurate (79%) tool for diagnosis of DVT, with NPV of 75% and PPV of 100%. On the other hand, a randomized clinical trial on the correlation between selective D-dimer testing and DVT by Linkins et al. [Citation15] on 860 patients found that selective testing reduced the proportion of patients who required D-dimer testing and reduced the proportion who required ultrasonography. Besides, Rectenwald et al. [Citation16] performed a prospective study to determine the sensitivity and specificity of plasma assays for D-dimer and found that plasma markers for DVT can be developed and achieve moderate sensitivity (73%), specificity (81%), and accuracy (77%) in diagnosing DVT.
In the present research, Wells score resulted in 76.2% false-positive and 2.7% false-negative cases when compared to EDUS.
It is in agreement with Sartori et al. [Citation17], where whole leg ultrasound identified 128 LEDVT (20%) of the studied patients. The failure rate of the low probability Wells score (< 1) to rule out DVT was 9.8%.
Also, Silveira et al. [Citation18] studied the performance of Wells score for DVT in inpatients and outpatients. They stated that it had a higher failure rate and lower efficiency in the inpatient setting compared with that reported in the outpatient. Proximal DVT incidence was low probability in 5.9%, moderate in 9.5%, and high 16.4%, in-between the inpatients (p < 0.001) compared with the much broader range for outpatients, and low probability in 3.0%, moderate probability in 16.6%, and high probability in 74.6%. This may be attributed to the use of anticoagulants in the inpatient.
In the present study, the mean time to both EDUS and the formal Doppler scans calculated from patient’s triage to the performance of ultrasound was 38.80 min and 74.40 min, respectively; consequently, EDUS was 50% shorter in time, which is one of the most important quality indicators in emergency management.
On the other hand, the mean duration of the scan for EDUS was 6.58 min for both lower limbs, while for the radiologist was 5.76 min.
The present research agreed with Crowhurst et al. [Citation19], who studied the sensitivity and specificity of the three-point compression ultrasonography performed by emergency physicians for the proximal DVT. They found that median duration EDUS was 10 min 34 s, with a median duration of 209 min from triage to examination. While the median delay between triage and radiology department diagnosis was 891 min, the difference was statistically significant (p < 0.05).
The current study showed that EDUS was a good diagnostic tool for diagnosis of LEDVT with sensitivity of 94.12%, specificity of 92.42%, PPV of 86.49%, and NPV of 96.83%. Moreover, there was no statistically significant difference between the results of both emergency and radiology examinations (p-value = 0.453).
As mentioned before, Crowhurst et al. [Citation19] also reported that the ensitivity of emergency resident examination was 77.8%, specificity was 91.4%, and accuracy was 89.6%. Moreover, Torres et al. [Citation20] studied the accuracy of EDUS performed by emergency physicians in patients with suspected DVT and concluded that sensitivity was 92.6%, specificity was 89%, PPV was 86.2%, and NPV was 94.2%.
Also, Burnside et al. [Citation21] reported a sensitivity of 95% and specificity of 96%, suggesting that EDUS may be accurate for the diagnosis of DVT.
Furthermore, Magazzini et al. [Citation22] conducted a study on 399 patients suspected of having DVT, presenting to the ED, to evaluate the accuracy and safety of emergency duplex ultrasound, without predefined clinical criteria to stratify the risk of the patients for DVT. The sensitivity of EDUS was 100%, specificity was 98.4%, PPV was 94.9%, NPV was 100%, and accuracy was 98.7%. [Citation22]
Abbasi et al. [Citation7] conducted a cross-sectional study on 81 patients with suspected LEDVT and reported a sensitivity of 85.9%, specificity of 41.2%, and accuracy of 84.6%.
Blaivas et al. [Citation23] stated sensitivity of EDUS 74%, specificity 93%, NPV 97%, and PPV 50%.
In conclusion, although it is well known that the three-point compression ultrasound is first-line imaging tool for DVT, but our study added the following:
It can be accurately and reliably performed with well-trained emergency physicians; in addition, it has a fast-learning curve.
EDUS can save 50% of time compared to the formal exam:
EDUS training should be reinforced in EDs in developing countries, and further research should be facilitated and encouraged.
Note: Well-trained emergency physician was considered when performing 80% successful scans for DVT. The minimum number of suspected DVT cases presenting to the Alexandria Main University Hospital ED per day is about five cases. The minimum working hours for emergency physicians is 48 h(2 days). The accepted number of successful scans to identify a well-trained emergency physician is 32 per month.
Fast learning curve, as emergency physicians were able to master the technique during a period of 3 months.
4.1. Pitfalls and limitations
The duration of the scan would be better calculated for every limb separately rather than both lower limbs together. This might improve the results of time calculations for emergency ultrasound and formal Doppler.
Technical difficulties should have been highlighted, such as weight of the patient, machine differences, and availability especially in the ED at the different working hours vacations, etc.
Morbidly obese patients were excluded but overweight were scanned as it is difficult to include only patients with ideal body weight.
Machine difference is a technical difficulty for emergency physicians because machines in the radiology department are more advanced with higher technical options.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Beckman MG, Hooper WC, Critchley SE. Venous thromboembolism: a public health concern. Am J Prev Med. 2010;38:S495–501.
- White RH. The epidemiology of venous thromboembolism. Circulation. 2003;107:I4–8.
- Raskob GE, Angchaisuksiri P, Blanco AN, et al.; and Day ISCfWT. Thrombosis: a major contributor to global disease burden. Arterioscler Thromb Vasc Biol. 2014;34:2363–2371.
- Pomero F, Dentali F, Borretta V. Accuracy of emergency physician performed ultrasonography in the diagnosis of deep vein thrombosis. A systematic review and meta-analysis. Thromb Haemost. 2013;109:137–145.
- American College of Emergency Physicians. Emergency ultrasound guidelines. Ann Emerg Med. 2009;53:550–570.
- Ashar T, Jayarama K, Yun R. Bed side ultrasound for detection of deep vein thrombosis: the two point compression method. Israeli J Emerg Med. 2006;6:36–43.
- Abbasi S, Bolverdi E, Zare MA. Comparison of diagnostic value of conventional ultrasonography by emergency physicians with Doppler ultrasonography by radiology physicians for diagnosis of deep vein thrombosis. J Pak Med Assoc. 2012;62:461–465.
- Blaivas M. Ultrasound in the detection of venous thromboembolism. Crit Care Med. 2007;35(1):224–234.
- Theodoro D, Blaivas M, Dugga LS, et al. Real-time B-mode ultraound in the ED saves time in the diagnosis of deep vein thrombosis (DVT). Am J Emerg Med. 2004;22:197–200.
- Bates SM, Ginsberg JS. Clinical practice. Treatment of deep-vein thrombosis. N Engl J Med. 2004;351:268–277.
- Hargett CW, Tapson VF. Clinical probability and D-dimer testing: how should we use them in clinical practice? Semin Respir Crit Care Med. 2008;29:15–24.
- Caldeira D, Rodrigues FB, Barra M, et al. Non-vitamin K antagonist oral anticoagulants and major bleeding-related fatality in patients with atrial fibrillation and venous thromboembolism: a systematic review and meta-analysis. Heart. 2015;101:1204–1211.
- Ho VB, Van Geertruyden PH, Yucel EK, et al. ACR appropriateness Criteria® on suspected lower extremity deep vein thrombosis. J Am College Radiol. Elsevier B.V. 2011;8:383–387.
- Min S-K, Kim YH, Joh JH, et al. Diagnosis and treatment of lower extremity deep vein thrombosis: korean practice guidelines. Vasc Spec. 2016;32(3):77–104.
- Linkins LA, Bates SM, Lang E, et al. Selective d-dimer testing for diagnosis of a first suspected episode of deep venous thrombosis: a randomized trial. Ann Intern Med. 2013;158(2):93–100.
- Rectenwald JE, Myers DD, Hawley AE, et al. D-dimer, P-selectin, and microparticles: novel markers to predict deep venous thrombosis: a pilot study. Thromb Haemost. 2005 Dec 7;94(6):1312–1317.
- Sartori M, Gabrielli F, Favaretto E, et al. Proximal and isolated distal deep vein thrombosis and Wells score accuracy in hospitalized patients. Intern Emerg Med. 2019 Sep 1;14(6):941–947.
- Silveira PC, Ip IK, Goldhaber SZ, et al. Performance of wells score for deep vein thrombosis in the inpatient setting. JAMA Intern Med. 2015 Jul 1;175(7):1112–1117.
- Crowhurst TD, Dunn RJ. Sensitivity and specificity of three-point compression ultrasonography performed by emergency physicians for proximal lower extremity deep venous thrombosis. Emerg Med Australas. 2013;25(6):588–596.
- Torres-Macho J, Antón-Santos JM, García-Gutierrez I, et al. Initial accuracy of bedside ultrasound performed by emergency physicians for multiple indications after a short training period. Am J Emerg Med. 2012;30(9):1943–1949.
- Burnside PR, Brown MD, Kline JA. Systematic review of emergency physician–performed ultrasonography for lower-extremity deep vein thrombosis. Acad Emerg Med. 2008;15(6):493–498.
- Magazzini S, Vanni S, Toccafondi S, et al. Duplex ultrasound in the emergency department for the diagnostic management of clinically suspected deep vein thrombosis. 2007;14(3):216–220.
- Blaivas M, Lambert MJ, Harwood RA, et al. Lower-extremity doppler for deep venous thrombosis-can emergency physicians be accurate and fast. Acad Emerg Med. 2000;7(2):120–126.