ABSTRACT
Background
This study aimed to evaluate safety and efficacy of magnesium sulphate as an adjuvant to peribulbar block at two different doses (75 and 100 mg) in reducing intraocular pressure (IOP) in obese patients undergoing glaucoma surgery.
Methods
Forty-six adult patients, American Society of Anesthesiologists status I–III, with body mass index of 30–55 kg/m2 undergoing glaucoma surgery under peribulbar block were enrolled during February, 2021. Patients were randomly assigned into two groups (1:1). Both groups received 4 ml of lidocaine 2%, 4 ml of bupivacaine 0.5%, and 1 ml of hyaluronidase (10IU of hyaluronidase/ml of lidocaine). Magnesium sulphate was added to this mixture either in a dose of 75 mg (group I) or 100 mg (group II). Primary outcomes included onset of globe and lid akinesia and IOP. Secondary outcomes included durations of analgesia and motor block, patients’ and surgeons’ satisfaction, and vital data.
Results
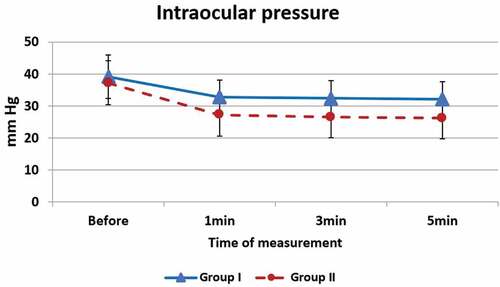
The mean onsets to globe and lid akinesia were significantly lower in group II compared to group I (2.7 vs. 4.2 min, p < 0.001 and 3.1 vs. 4.2 min, p = 0.001, respectively). After the block, the mean IOP was significantly lower in group II at 1 min (27.2 vs. 32.7 mmHg, p = 0.0034), 3 min (26.5 vs. 32.4 mmHg, p = 0.002) and 5 min (26.2 vs. 32.1 mmHg, p = 0.001). Group II had a significantly longer mean durations of analgesia (3.5 vs. 2 hours, p < 0.001) and recovery of motor block than group I (3.3 vs. 2.3 hours, p < 0.001). No complications were encountered during the surgery.
Conclusion
Magnesium sulphate at a dose of 100 mg demonstrated higher efficacy while maintaining safety compared to the dose of 75 mg.
1. Introduction
Magnesium sulphate (MS) is one of the adjuvant medications that are used along with anesthetic drugs to perform peribulbar block in ophthalmic surgeries [Citation1].
Although MS does not possess a direct analgesic effect, its use in regional blocks and spinal anesthesia has been associated with reduced pain and analgesic requirement [Citation2–5]. Several mechanisms have been proposed to explain this antinociceptive effect of MS. One mechanism is that magnesium blocks N-methyl-D-aspartate (NMDA) receptors non-competitively; thereby MS prevents central sensitization, which results from peripheral tissue injury [Citation6]. Another proposed mechanism is that magnesium is a competitive antagonist of calcium, thus it blocks calcium influx into the nerve cells and consequently reduces the release of acetylcholine from presynaptic nerve endings [Citation7]. Furthermore, MS can enhance peripheral nerve blockade. The negative charge on the surface of the outer membrane of nerve cells attracts the positively charged magnesium ions, resulting in an increased concentration of magnesium around the nerve bundle. This in turn affects Na+ channel gating, causing hyperpolarization and nerve conduction block [Citation8].
Most studies that evaluated the use of MS in peribulbar block utilized it in a dose of 50 mg [Citation1,Citation9–14]. The administration of MS at doses higher than 50 mg in patients undergoing ophthalmic procedures was reported only by two studies [Citation15,Citation16]. Moreover, previous studies were either conducted on block performed for various ophthalmic procedures [Citation1,Citation10,Citation17] or in certain procedures such as cataract [Citation9,Citation11–15] and strabismus [Citation16].
Up to the authors’ knowledge, this is the first study to include only patients undergoing glaucoma surgery. The present clinical trial aimed to evaluate the safety and efficacy of MS as an adjuvant to peribulbar block at two different doses – 75 and 100 mg – in reducing the intraocular pressure (IOP) in obese patients undergoing glaucoma surgery.
2. Methods
2.1. Ethical considerations
This study adheres to the uniform requirements for manuscripts submitted to biomedical journals and has been conducted in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans. The study obtained approval from the Ethics Committee of the Research Institute of Ophthalmology, Egypt (8–11-2020). A written, informed consent was taken from each patient. Confidentiality of data was maintained by making code numbers for each patient. The trial was registered at the Iranian Registry of Clinical Trials (IRCT20210118050069N1; 27 January 2021).
We intend to share the individual de-identified participants’ data. Data will be accessible through direct contact with the corresponding author, beginning 12 months and ending 24 months following article publication.
2.2. Study design, settings and date
This triple-blinded, parallel-group (1:1), randomized, clinical trial was conducted at the Research Institute of Ophthalmology, Egypt during February 2021.
2.3. Sample size calculation
The sample size was calculated using G* power 3.1.9.2 software. The effect size was calculated based on the difference of the means of IOP and globe akinesia between the two study groups. We postulated that adding MS to the peribulbar block at a dose of 100 mg will enhance the onset of globe akinesia and reduce IOP by around 25% compared to adding it at a dose of 75 mg. The sample size for the globe akinesia was 16 subjects per group, while based on IOP, it was 19 subjects per group. As both were primary outcomes for the present study, we adopted the larger sample size. We then added 20% to account for loss to follow up, thus the final sample size was 23 subjects per group (a total of 46).
2.4. Randomization and masking
The sealed, opaque, sequentially numbered envelopes method was used for randomization and allocation concealment. We prepared two sets of 23 identical, opaque, letter-sized envelopes. Each envelope contained a white allocation paper, marked as “Treatment A” (n = 23) or “Treatment B” (n = 23) and a sheet of single-sided carbon paper closest to the front of the envelope (with the carbon side facing the white paper). Finally, we sealed the envelopes and signed across the seal. We combined the two sets (46 envelopes) and shuffled them thoroughly. Then, we marked a number on the front of each envelope sequentially from 1 to 46 and placed them into a plastic container in numerical order.
An investigator (not involved in sequence generation and allocation concealment) assessed participants for eligibility and assigned eligible patients to receive peribulbar anesthesia to which either 75 mg of MS (group I) or 100 mg of MS (group II) was added.
Participants, care providers (carrying out the peribulbar block), health assessors, and data analyst were blinded to treatment allocation.
2.5. Eligibility criteria
We enrolled adult male and female patients; aged 18 to 70 years; for whom glaucoma surgery was indicated; and had American Society of Anesthesiologists status I, II, or III; body mass index of 30–55 kg/m2; and axial length of 20–28 mm.
We excluded patients who refused to participate, were high myopic with an axial length exceeding 29 mm, and those who had an eye infection, history of allergy to the study medications, or severe coagulation disorders as well as those suffering from conditions preventing them from lying flat or staying still during the operation, such as skeletal problems, orthopneic patients, and patients with uncontrolled tremors as Parkinsonism.
2.6. Intervention
In the first intervention group (group I), participants were given peribulbar anesthesia with a local anesthetic mixture composed of 4 ml of lidocaine 2% (Sunny Pharmaceutical, Egypt), 4 ml of bupivacaine 0.5% (Sunny Pharmaceutical, Egypt), and 1 ml of hyaluronidase (Shreya Life Sciences Pvt. Ltd., India) (at a concentration of 10 IU of hyaluronidase/ml of lidocaine) to which 75 mg of MS (EIPICO Pharmaceutical, Egypt) was added. Group II patients received peribulbar anesthesia with the same doses and concentrations of lidocaine, bupivacaine, and hyaluronidase (as group I) to which 100 mg of MS was added.
All patients were subjected to history taking (including sociodemographics, medical illnesses, and prior surgery or anesthetic experiences), examination (including assessment of vital data, level of consciousness, and respiratory and abdominal examination), and laboratory investigations (complete blood picture, fasting and 2-hours postprandial blood glucose level, kidney function, liver function, and coagulation profile).
Supplemental analgesia (in the form of 30 µg of IV fentanyl) was planned to be given in case of block failure.
2.7. Outcome measures
The primary outcomes included the onset of globe akinesia (using 3-point scale; at 1, 3, and 5 min after the block), the onset of lid akinesia (using 3-point scale; at 1, 3, and 5 min after the block), and the intraocular pressure (using Schiotz tonometer; at baseline, 1, 3, and 5 minutes after the local anesthesia). The secondary outcomes included the duration of analgesia (using the Visual Analog Scale; at 1, 2, and 4 h postoperatively), the duration of motor block (clinical assessment of regaining full movement; at 1, 2, and 4 h postoperatively), patient and surgeon satisfaction (immediately after the block), and vital data including the heart rate, oxygen saturation, and blood pressure (using electronic vital signs monitor; every 5 minutes during the operation).
Safety was assessed looking for complications, such as lid hematoma or subconjunctival hemorrhage.
2.8. Statistical analysis
Statistical analysis was performed using the Statistical Package for Social Sciences (IBM SPSS Statistics) for Windows, version 26 (IBM Corp., Armonk, N.Y., USA). All numerical variables followed normal distribution and values were expressed as mean ± standard deviation. The two groups were compared using the Independent Samples T-test. For categorical data, the variables were summarized as frequencies (count and percentage). Pearson’s Chi-square test for independence, Fisher’s exact test or Fisher-Freeman-Halton exact test were used to examine the association between two categorical variables as appropriate. A p-value <0.05 was adopted for interpreting the significance of statistical tests.
3. Results
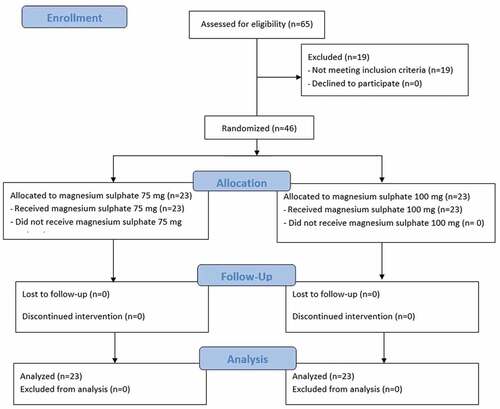
Sixty-five adult patients scheduled for glaucoma surgery were assessed, and 46 met eligibility criteria and were randomly allocated to receive either 75 mg of MS (group I) or 100 mg of MS (group II) added to the local anesthetic mixture of the peribulbar block during February 2021. There was no loss to follow up or exclusions after randomization (). Both groups were comparable regarding sociodemographic characteristics with no significant difference.
The two intervention groups were compared regarding the primary outcomes, including onset to globe akinesia and lid akinesia as well as IOP (). The mean onset to globe akinesia was significantly lower in group II compared to group I (2.7 vs. 4.2 min, p < 0.001), as a significantly higher percentage of patients in group II scored zero three minutes after the block (82.6% vs. 39.1%, p < 0.001). Similarly, the mean onset to lid akinesia was significantly lower in group II than that of group I (3.1 vs. 4.2 min, p = 0.001), as a significantly higher percentage of group II patients reached zero score three minutes after the block (78.3% vs. 39.1%, p = 0.002). Comparison of IOP revealed that baseline measurements before the block were similar in the two groups (p = 0.351). After the block, the mean IOP was significantly lower in group II than in group I when measured at 1 minute (27.2 vs. 32.7 mmHg, p = 0.004), 3 minutes (26.5 vs. 32.4 mmHg, p = 0.002) and 5 minutes (26.2 vs. 32.1 mmHg, p = 0.001) ().
Table 1. Comparison of the onset to global akinesia and lid akinesia as well as intraocular pressure between the two intervention groups
The two groups were also assessed for secondary outcomes, including the duration of both analgesia and motor block, patients’ and surgeons’ satisfaction, heart rate, blood pressure as well as oxygen saturation.
Group II had a significantly longer mean duration of analgesia than group I (3.5 vs. 2 hours, p < 0.001), as analgesia lasted for 4 hours in a significantly higher percentage of group II patients (73.9% vs. 0%, p < 0.001). The mean duration of recovery of motor block was likewise significantly longer in group II compared to group I (3.3 vs. 2.3 hours, p < 0.001), as motor block lasted for 4 hours in 65.2% of group II patients while none of group I patients exceeded 3-hour duration (p < 0.001). No significant difference was observed in patients’ satisfaction between the two groups, though the mean score was slightly higher in group II than in group I (2.7 vs. 2.4, p = 0.077). On the other hand, the mean score of surgeons’ satisfaction was significantly higher in group II (2.9 vs. 2.5, p = 0.010, ).
Table 2. Comparison of the duration of analgesia and recovery of the motor block as well as patients and surgeons satisfaction between the two intervention groups
Monitoring and assessment of heart rate, blood pressure and oxygen saturation after the block at 5, 10 and 15 minutes showed the lack of significant differences between the two intervention groups (p > 0.05, ).
Table 3. Comparison of heart rate, blood pressure, and oxygen saturation between the two intervention groups
No adverse events were encountered in any patient during the block performance or surgery.
4. Discussion
Magnesium sulphate is one of the adjuvant medications that are used along with anesthetic drugs to perform peribulbar block in ophthalmic surgeries [Citation1]. Most studies that evaluated the use of MS in peribulbar block utilized it in a dose of 50 mg [Citation1,Citation9–14,Citation17]. The administration of MS at doses higher than 50 mg in patients undergoing ophthalmic procedures was reported only by two studies [Citation15,Citation16]. Moreover, previous studies were either conducted on block performed for various ophthalmic procedures [Citation1,Citation10,Citation17] or in certain procedures such as cataract [Citation9,Citation11–15] and strabismus [Citation16].
Up to the authors’ knowledge, this is the first study to include only patients undergoing glaucoma surgery. The present clinical trial aimed to evaluate the safety and efficacy of MS as an adjuvant to peribulbar block at two different doses – 75 and 100 mg – in reducing IOP in obese patients undergoing glaucoma surgery. Forty-six patients were randomly assigned into group I (MS-75) and group II (MS-100).
The results of this clinical trial showed the efficacy of MS, particularly the 100 mg dose, in hastening the onset to globe and lid akinesia. The mean onset to globe akinesia was significantly lower in group II compared to group I (2.7 vs. 4.2 min, p < 0.001), and also was the mean onset to lid akinesia (3.1 vs. 4.2 min, p = 0.001).
The ability of MS to hasten the onset of globe akinesia compared to control (the standard block without adjuvants) was reported by previous studies at a dose of 50 mg in patients undergoing various ophthalmic procedures [Citation1,Citation9–12,Citation17]. However, the study by Hamawy and Bestarous [Citation13] showed the lack of significant difference in the median akinesia score between the control and MS (administered as 50 mg) groups. Another study by Abu Elyazed and Mostafa [Citation14] showed non-significant differences in onset to globe or lid akinesia between control and MS (50 mg dose) groups.
As regards the effect of higher doses of MS, Sherif et al. [Citation16] assessed a dose of 100 mg against the standard technique in adult patients undergoing strabismus surgery. They reported a hastened onset of globe akinesia compared to the standard technique (2.3 vs. 4.4 min, respectively, p < 0.001). In partial agreement with our results, Mogahed et al. [Citation15] compared 50 mg and 100 mg of MS in patients undergoing cataract surgery. They found that the mean score of globe akinesia was significantly lower in the 100 mg-MS group compared to the control and 50 mg-MS groups at 3 min (p < 0.001). However, the difference in the score at 5 min between the two MS groups was non-significant. They observed no significant differences in the mean lid squeezing scores between the two doses of MS at 3, 5, or 10 min.
Obese patients show a tendency to have elevated IOP [Citation18–20]. In the present clinical trial, the mean IOP was significantly lower in group II than in group I at 1 minute (27.2 vs. 32.7 mmHg, p = 0.004), 3 minutes (26.5 vs. 32.4 mmHg, p = 0.002) and 5 minutes (26.2 vs. 32.1 mmHg, p = 0.001) after the block. The decrease of IOP with the higher dose of MS provides a great advantage in glaucoma surgery, particularly with obese patients. On the contrary, Mogahed et al. [Citation15] found that IOP first increased in the control and the two MS groups at 1 minute then decreased at 5 and 10 minutes and the amount and pattern of decrease was nearly similar in the three groups.
The duration of analgesia and motor block represent important considerations to the surgical team as inadequate analgesia or short duration of a motor block will require the administration of analgesics and additional doses of anesthetics. The mean durations of analgesia and motor block in this clinical trial were significantly longer in group II compared to group I (3.5 vs. 2 hours, p < 0.001 and 3.3 vs. 2.3 hours, p < 0.001, respectively). None of the patients in either group received supplemental analgesia or additional doses of the local anesthetic mixture.
This effect of the higher dose of MS in prolonging the duration of analgesia and motor block is supported by the findings of Sherif et al. [Citation16] who reported a mean duration of anesthesia of 180 min with 100 mg MS.
The anesthetic and analgesic effects of MS could be explained by the fact that magnesium blocks calcium channel and NMDA receptors. Meanwhile, magnesium may not possess analgesic or anesthetic effects on its own [Citation21].
The oculocardiac reflex (OCR) is a complication that may occur during any ophthalmic surgery involving the orbit due to pressure on the eye globe, conjunctiva, or other orbital structures and traction on the extraocular muscles. The reflex causes bradycardia and hypotension, with potentially serious, life-threatening consequences. Monitoring and assessment of heart rate and blood pressure are mandatory to manage OCR [Citation22]. The stability of heart rate and blood pressure indicates the non-occurrence of OCR in either group. This protective effect of MS against OCR was also stated by Sherif et al. [Citation16] who found that none of the patients suffered this reflex in the 100 mg-MS group compared to 33.3% of patients in the standard technique group (p = 0.002). Such an effect of MS may be the result of deep anesthesia and analgesia [Citation23].
The oxygen saturation after the block at 5, 10 and 15 minutes was also stable, with no differences between the two groups. Respiratory complications are among the serious challenges that may be encountered during surgery in obese patients. Routine oxygen supplementation via nasal cannula (3 L/min) was considered for all, but no major respiratory problems were encountered.
No significant difference was observed in patients’ satisfaction between the two groups, though the mean score was slightly higher in group II than in group I (2.7 vs. 2.4, p = 0.080). On the other hand, the mean score of surgeons’ satisfaction was significantly higher in group II (2.9 vs. 2.5, p = 0.010). Higher surgeon’s satisfaction with the higher dose of MS could be attributed to the more favorable conditions induced by this dose, in terms of faster onset of akinesia besides prolonged duration of motor block. On the contrary of these findings, Sinha et al. [Citation1] found that surgeons’ satisfaction score was similar between the MS group and control. Sherif et al. [Citation16] reported a higher percentage of patient’s satisfaction with the use of 100 mg MS compared to the standard technique (100% vs. 25.9%, p < 0.001). These variations in the reported patients’ and surgeons’ satisfaction among the studies could be attributed to differences in the method of assessing satisfaction or to the different nature of ophthalmic procedures performed.
No adverse events were observed in the present trial in either group, which is in line with previous studies using 100 mg of MS with peribulbar block [Citation15,Citation16].
The present research work showed some points of strength, being the first study to assess MS as an adjuvant to peribulbar block in glaucoma surgery in a high-risk category of patients (the obese). However, our results are limited by being a single-center trial and the satisfaction of patients and surgeons was assessed subjectively without using a structured questionnaire form.
5. Conclusions
The addition of MS to the peribulbar block anesthetic mixture in a dose of 100 mg shortened the onset of akinesia, prolonged the duration of analgesia, decreased IOP, and protected against OCR without obvious adverse effects. At this dose, MS demonstrated higher efficacy compared to the dose of 75 mg, while maintaining safety. Besides these inferences, the cost-effectiveness of MS is an added advantage, which favors its use as an adjuvant to peribulbar block in glaucoma surgery.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Sinha R, Sharma A, Ray BR, et al. Effect of addition of magnesium to local anesthetics for peribulbar block: a prospective randomized double-blind study. Saudi J Anaesth. 2016;10:64–67.
- Bilir A, Gulec S, Erkan A, et al. Epidural magnesium reduces postoperative analgesic requirement. Br J Anaesth. 2007;98:519–523.
- Arcioni R, Palmisani S, Tigano S, et al. Combined intrathecal and epidural magnesium sulfate supplementation of spinal anesthesia to reduce post-operative analgesic requirements: a prospective, randomized, double-blind, controlled trial in patients undergoing major orthopedic surgery. Acta Anaesthesiol Scand. 2007;51:482–489.
- Hwang JY, Na HS, Jeon YT, et al. I.V. infusion of magnesium sulphate during spinal anaesthesia improves postoperative analgesia. Br J Anaesth. 2010;104:89–93.
- Gunduz A, Bilir A, Gulec S. Magnesium added to prilocaine prolongs the duration of axillary plexus block. Reg Anesth Pain Med. 2006;31:233–236.
- Lee AR, Yi H-W, Chung IS, et al. Magnesium added to bupivacaine prolongs the duration of analgesia after interscalene nerve block. Can J Anaesth. 2012;59:21–27.
- Woolf CJ, Thompson SWN. The induction and maintenance of central sensitization is dependent on N-methyl-d-aspartic acid receptor activation; implications for the treatment of post-injury pain hypersensitivity states. Pain. 1991;44:293–299.
- Akutagawa T, Kitahata LM, Saito H, et al. Magnesium enhances local anesthetic nerve block of frog sciatic nerve. Anesth Analg. 1984;63:111–116.
- Helal DAA, Refkee MA, Farid DM, et al. Effect of adding magnesium sulphate to lidocaine, bupivacaine and hyaluronidase in extraconal block for cataract surgeries. J Anest Inten Care Med. 2018;7:1–8.
- AbdAlali SA, Mohamed GF, AbdAlmagid AS, et al. Clinical comparative study between magnesium sulphate versus rocuronium versus dexmedetomidine as adjuvants for local anesthetic in peribulbar block for eye surgeries. Egypt J Hosp Med. 2018;73:7204–7210.
- Kassem OAH, ELgarhy AMM, Salim MG. Magnesium sulphate versus Dexmedetomidine as adjuvants for local anasthetics in peribulbar block for eye surgeries: clinical comparative study. Egypt J Hosp Med. 2018;72:4308–4312.
- Mohamed AZE, Genidy MM. Magnesium sulphate versus dexmedetomidine as an adjuvant to local anesthetic mixture in peribulbar anesthesia. Egypt J Anaesth. 2017;33:375–380.
- Hamawy TY, Bestarous JN. Rocuronium versus magnesium as an adjuvant to local anesthetics in peribulbar block. Ain-Shams J Anesthesiol. 2013;6:317–321.
- Abu Elyazed MM, Mostafa SF. Fentanyl versus magnesium sulphate as adjuvant to peribulbar anesthesia in cataract surgery. Egypt J Anaesth. 2017;33:159–163.
- Mogahed MM, Anwar AG, Abo-elazm WN. The effect of adding two different doses of magnesium sulphate as adjuvant to ropivacaine in peribulbar block for cataract surgery. J Anesth Clin Res. 2017;8:1–7.
- Sherif NA, Mohamad MK, Taher SG, et al. Effectiveness and safety of single percutaneous peribulbar block using magnesium sulphate as an adjuvant to local anesthetics versus the standard peribulbar block for strabismus surgery in adults. Open Anesthesia J. 2019;13:100–105.
- Shoukry A, Kawy A. Efficacy and safety of magnesium versus dexmedetomidine as additives to local anesthetic mixture using single injection percutaneous peribulbar anesthesia in vitreoretinal surgeries. Open Anesthesia J. 2018;12:94–100.
- Klein BE, Klein R, Linton KL. Intraocular pressure in an American community. The Beaver Dam eye study. Invest Ophthalmol Vis Sci. 1992;33:2224–2228.
- Wu SY, Leske MC. Associations with intraocular pressure in the Barbados eye study. Arch Ophthalmol. 1997;115:1572–1576.
- Mori K, Ando F, Nomura H, et al. Relationship between intraocular pressure and obesity in Japan. Int J Epidemiol. 2000;29:661–666.
- Do SH. Magnesium: a versatile drug for anesthesiologists. Korean J Anesthesiol. 2013;65:4–8.
- Bharati SJ, Chowdhury T. Chapter 7 - the oculocardiac reflex. In: Chowdhury T, Schaller BJ, editors. Trigeminocardiac reflex. Boston: Academic Press; 2015. p. 89–99.
- Shin SY, Kim MJ, Joo J. Oculocardiac reflex and oculorespiratory reflex during strabismus surgery under general anesthesia using the laryngeal mask airway with maintenance of spontaneous respiration: a retrospective study. J Int Med Res. 2020;48:0300060520945158.