ABSTRACT
Background
The efficacy of pain control is a crucial element of improved recovery following thoracic surgery. Inadequate analgesia may extend the interval of hospitalization, besides raising medical costs. Fascial plane blocks are quickly becoming a feasible as well as a safe alternative to epidural analgesia for abdominal and thoracic pain. Rhomboid intercostal block (RIB) is a novel, simple block utilized in a region that is described as a triangle of auscultation on the scapula’s medial edge. This study attempted to determine the impact of RIB on postoperative pain following thoracoscopic surgery compared to local anesthetic (LA) infiltration.
Methods
The current research is a randomized, controlled trial on 60 subjects undergoing video-assisted thoracic surgery. Participants were randomly divided into two groups. All subjects received standard general anesthesia protocol, which included the insertion of a double-lumen endotracheal tube as well as mechanical ventilation. At the end of the operation in the RIB group, an injection of 20 ml bupivacaine (0.25%) was administered below the rhomboid major muscle guided by ultrasound. In the LA group, patients received local wound infiltration. Visual analog scores for pain during coughing and at rest, total postoperative analgesic consumption, adverse effects, and hospital stay were recorded.
Results
The study group demonstrated diminished visual analog scores during coughing as well as at rest with less overall consumption of analgesia compared to the local infiltration group.
Conclusion
Our study showed that ultrasound guided RIB provides better pain relief and less postoperative opioid consumption after thoracoscopic surgeries compared to local anesthetic infiltration.
1. Introduction
The efficacy of pain control is a fundamental aspect of improved recovery following thoracic surgery. Inadequate analgesia can induce unfavorable outcomes, including prolonged hospitalization, in addition to rising medical costs [Citation1]. Significant benefits featured new surgical procedures like video-assisted thoracic surgery (VATS) compared to traditional thoracotomy. However, 29% of cases still have postoperative pain, making postoperative analgesia difficult to perform [Citation2].
Thoracic epidural analgesia is considered the gold standard for thoracic analgesia; nevertheless, it has a failure rate. In addition, it is linked to some complications such as elevated in-hospital mortality as well as spinal hematoma [Citation3].
Facial plane blocks have quickly emerged in order to sustain a safe and simple alternative to epidural analgesia for abdominal and thoracic pain [Citation4].
Anesthesiologists have long utilized plane blocks. They have lately been employed in a variety of surgeries. Plane blocks like the erector spinae plane block, the pectoral nerve block, and the serratus anterior plane block can be utilized in a broad spectrum of surgical procedures, including the thoracic wall [Citation5].
Rhomboid intercostal block (RIB) is a novel easy block that is less dangerous than the thoracic epidural. RIB is used in a region known as the triangle of auscultation on the scapula’s medial edge. This region is defined by the latissimus dorsi, scapula’s medial margin, and trapezius muscle’s lower border. RIB is carried out by injecting the upper intercostal muscle plane as well as below the rhomboid muscles. Elsharkawy et al. utilized it in the case of suffering from numerous rib fractures for pain relief [Citation6].
The present study attempted to investigate the impact of the rhomboid intercostal block on postoperative pain following thoracoscopic surgery as compared to local anesthetic (LA) infiltration.
2. Methods
2.1. Ethical considerations
The study protocol was authorized by the Ethics Committee of Ain Shams Faculty of Medicine, Ain Shams University, Egypt (FMASU R 34/2021). All participants signed informed written consents. Data confidentiality was protected by assigning code numbers to each participant. The study has been registered at ClinicalTrials.gov (NCT04821947; 30 March 2021).
Anonymized individual participant data will be available by directly contacting the corresponding author, between 12 months to 36 months following the publication of the article.
2.2. Design, settings, and timing of the study
From April 2021 through September 2021, this blinded, parallel-group (1:1), randomized, controlled study was carried out at Ain Shams University Hospitals (Cardiovascular Surgery Hospital – Thoracic Surgery Unit), Cairo, Egypt, from April 2021 to September 2021.
2.3. Sample size calculation
Calculation of sample size was performed utilizing STATA program, where the type-1 error (α) was set at 0.05. The result from a study by Öksüz et al. [Citation7] showed that the overall tramadol usage postoperatively during the first 24 hours was substantially diminished in the serratus anterior plane block (SAPB) group as 238.5 ± 39.5 mg compared to 306 ± 25.2 mg in the intercostals block (IB) group. Based on these values, a sample size of 30 cases in each group (60 total) provides 100% power in order to detect the observed difference.
2.4. Masking and randomization
Randomization was carried out via a computer-generated random sequence, as well as allocation concealment to be ensured during the procedure by utilizing numbered, opaque, and sealed envelopes.
One of the investigators (who did not participate in generating sequence or allocation concealment) evaluated the recruited subjects whether they were eligible or not. In addition, they assigned those who were found eligible to receive either rhomboid intercostal block (RIB group) or local anesthetic infiltration (LA group).
Participants, care providers, investigators, and health assessors were blinded the procedure allocation.
2.5. Eligibility criteria
We recruited male and female subjects (18–65 years old) referred for thoracoscopic surgery and were of the American Society of Anesthesiologists (ASA) physical status I or II.
Exclusion criteria included allergic constitution, severe cardiovascular or hepato-renal insufficiency, coagulation system disease, injection site infection, and morbid obesity (body mass index >40 kg/m2).
2.6. Intervention
Visual analogue scale (VAS-100) of post-operative pain and pain control methods (PCA) were explained to each patient. The VAS score ranged from 0 to 100 (100 = most severe pain, whereas 0 = no pain).
Standard monitoring of subjects included heart rate, peripheral oxygen saturation, invasive systolic, diastolic and median blood pressure, as well as timing of operations.
All participants were subjected to standard general anesthesia procedure, which included induction with rocuronium (0.6–0.8 mg/kg), propofol (2–3 mg/kg), and intravenous midazolam (0.05 mg/kg). Sevoflurane (2–2.5%) was used to maintain anesthesia while aiming for a 40–50 bispectral index.
With the patient in the supine position, a double-lumen endotracheal tube of adequate size (35–39 French) was inserted. Patients were positioned on either the left or right side, depending on which side was to be operated.
Mechanical ventilation was set up to maintain end-tidal CO2 around 30–35 mmHg. Additionally, the dosages of fentanyl and sevoflurane were modulated to keep the mean arterial blood pressure (MAP) as well as heart rate (HR) in the range between 80% and120% of the preoperative outcomes. All subjects were administered paracetamol (1 g) and ondansetron (0.1 mg/kg). By the end of the procedure, the RIB was carried out by the anesthesiologist, or local anesthetic infiltration of the wound was conducted by the operating surgeon.
RIB was carried out, while the participant was in a lateral position. A linear ultrasound transducer with an orientation marker directed cranially was inserted in the sagittal plane, medial to the medial edge of the scapula. The transducer was rated such that the cranial end was slightly medially directed and the caudal somewhat laterally directed.
From superficial to deep, the following structures were detected: rhomboid major muscle, trapezius muscle, intercostal muscles between ribs, pleura, as well as lung. The tissue plane that connects the intercostal muscles as well as the rhomboid major was determined. An 18-gauge Tuohy needle was advanced in plan from a superomedial to an inferolateral direction, through trapezius and rhomboid major muscles. The initial injection was administered via the skin at the T5-T6 level immediately medial to the scapula.
After confirming the position with a 3-ml hydrodissection on the upper intercostal muscles under the rhomboid major muscle, injection of 20 ml of bupivacaine (0.25%) was done below the rhomboid major muscle.
The LA group received local wound infiltration. The video assisted thoracoscopic surgery (VATS) incision was determined by the position of the pulmonary nodules and was either a single-incision (about 4 cm) with 10 mL of 0.25% bupivacaine or a double-incision (roughly 3 cm + 5 mL) with 15 mL (10 mL + 5 mL) of 0.25% bupivacaine. If double-incision thoracoscopic surgery was cumbersome, we utilized a three-port technique (about 3 cm + 1 cm + 0.5 cm) with 17 mL (10 mL + 5 mL + 2 mL) of 0.25% bupivacaine for camera and instrument placement.
Ephedrine was utilized for treating hypotension (MAP < 80% of the baseline), whereas 0.5 atropine mg was used for the treatment of Bradycardia (HR < 45 beats/min).
After meeting the extubation criteria, all patients were extubated and referred to the ICU.
All patients received patient-controlled analgesia (PCA) (TURen-Germany-PRC). The PCA was set to inject 10 mg of tramadol into each bolus, up to three times per hour, with a locked period reaching 20 minutes. If the participant still has pain (VAS score >40), he received 1 mg of morphine.
A trained team member blinded to the allocation of groups and was not present or engaged in surgery evaluated and managed the postoperative pain.
Examination of data included weight, sex, age, ASA, the proportion of postoperative analgesic consumption, operating time, operation type, VAS at 1st, 2nd, 4th, 6th, 12th, 24th hours during coughing and at rest, in addition to complications like vomiting, nausea, atelectasis, bradycardia, and hypotension, as well as the interval of hospitalization.
2.7. Study outcomes
The study outcomes included the total amount of postoperative analgesic consumption (total dose of postoperative tramadol and morphine) and the Visual Analogue Score (VAS) measured at 1st, 2nd, 4th, 6th, 12th, 24th hours postoperative (at rest and during cough).
2.8. Statistical methods
The data were coded and tabulated, and subsequently, the statistical analysis was then performed utilizing the Statistical Package for Social Sciences software, version 22.0 (IBM Corp., Chicago, USA, 2013). Quantitative data were verified for normality via the Shapiro-Wilk test. Normally distributed data were described as mean and standard deviation (SD) and were compared utilizing the independent t-test. Data that were not normally distributed were presented as median (interquartile range) and were compared using Mann Whitney test. Qualitative data, including variables with expected and small numbers, were described as number and percentage and were compared using Chi-square test, as well as Fisher’s Exact test. The significance level was determined at P-value <0.05.
3. Results
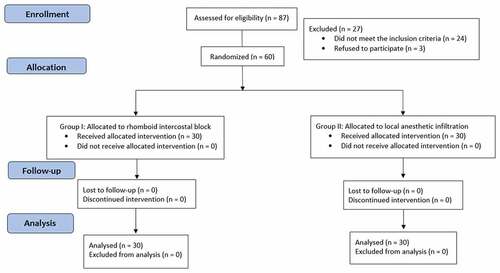
Eighty-seven adult subjects scheduled for thoracoscopic surgery were evaluated; 27 were excluded (24 subjects failed to fulfill the inclusion criteria, as well as three subjects declined participation). Sixty patients were eligible and randomly assigned to undergo either local anesthetic infiltration (LA group, n = 30) or rhomboid intercostal block (RIB group, n = 30). All subjects were followed up and after randomization, none of them has been excluded ().
shows no significant difference between the studied groups in relation to weight, sex, age, ASA, operation type, operation duration, or thoracoscopic lesions.
Table 1. Comparison regarding demographic characteristics
shows that the doses of both postoperative tramadol and morphine were significantly lower in the RIB group in the first 24 hours postoperatively.
Table 2. Comparison regarding the doses of postoperative tramadol and morphine
shows that the postoperative pain perception (VAS-100) during rest and cough was lower in the RIB group. In addition, the differences were statistically significant at 2, 4, and 6 hours.
Table 3. Comparison regarding postoperative pain perception (VAS-100) during rest and cough
Atelectasis, nausea, and vomiting were non-significantly less frequent in the RIB group. The RIB group had an insignificantly shorter time to remove the chest tube and decreased hospitalization interval ().
Table 4. Comparison regarding complications and hospital stay
4. Discussion
Our current prospective randomized clinical trial was meant to compare RIB with LA wound infiltration for postoperative pain control in thoracoscopic surgeries to prove the efficacy of RIB.
The data obtained in our study demonstrated that the analgesic requirements in the first 24 h postoperatively were significantly lower in the RIB group with a highly significant difference in the VAS scores both at rest and during cough at second, fourth and sixth hours postoperatively and less yet non-significant difference till the end of the day indicating the effectiveness of RIB over LA wound infiltration with longer duration of action.
Insertion of chest tube, operative wound muscle splitting, and visceral pain are crucial aspects of post-thoracoscopic pain. Consequently, the management of multiple pains following thoracoscopic surgery is fundamental to improving spontaneous patient ventilation, thus allowing early ambulation and preventing atelectasis. Nevertheless, the majority of patients are complaining most about the pain caused by chest tube following operations [Citation8].
VATS-wound infiltration has been demonstrated to alleviate postoperative pain and offers a simple and effective technique with few side effects, which has previously been utilized in several surgeries, particularly minimally invasive surgeries. Recently, more attention has been drawn to innovative techniques (Plane blocks), which recently substituted the thoracic epidural block, which was formerly the gold standard for post-thoracotomy pain [Citation9].
Elsharkawy et al. [Citation5] were the first to define RIB, and they attempted to investigate the diffusion of dye and the impact of local anesthetic administered between the rhomboid major muscle and the intercostal muscles in patients and cadavers.
They utilized six fresh human cadavers. They demonstrated that injection in the tissue plane that is allocated between intercostal and the rhomboid muscles in the triangle of auscultation targeting lateral cutaneous branches of ventral rami of thoracic intercostal nerves. The spread expands until reaching the erector spinae tissue plane, peripherally to thoracic transverse processes at the region in which the thoracic intercostal nerves’ dorsal rami arises between the tips of adjacent transverse processes T3 to T9 and laterally until reaching the serratus anterior muscle [Citation6].
In the clinical part of the study, they described a case series that included 15 patients. Dermatomal cold sensory impairments were consistently obtained, with the greatest cephalad coverage reaching T2 and T12 for the most caudal coverage. The dermatomal coverage included the anterior hemithorax, laterally to the axilla, and the posterior hemithorax. The average duration of analgesia for single-shot blocks was 16 hours, whereas catheter infusion lasted 3–6 days. There were no adverse effects from the blocks [Citation6].
Case reports by Tulgar et al. [Citation10] showed that RIB carried out with 25 ml of bupivacaine at a concentration of 0.25% on cases suffering from multiple rib fractures provided sensory block as well as symptomatic relief at the T2 – T9 levels in the posterior, lateral and mid-anterior hemithorax.
Also, in a case report done by Okmen [Citation11], five patients were scheduled for posterolateral thoracotomy for lobectomy surgery because of lung cancer, and he found that RIB utilizing 30 ml LA mixture 20 ml bupivacaine + 10 ml lidocaine led to an effective sensory block at the levels of T3 to T7 in all five subjects with a VAS score mean of 2/10 [Citation11]. However, block spread levels varied according to block volume, and infusions delivered via catheter were observed to enhance block duration.
The RIB provides significant dermatomal analgesic coverage of the thorax and upper abdomen. Besides, it can be utilized as a supplement to a patchy thoracic epidural for postoperative pain following thoracotomy and thoracoscopic surgeries, pain related to chest tube, pain induced by rib fracture as well as pain due to upper abdominal incisional [Citation6].
In the present study, the occurrence of PONV showed a lower yet non-significant difference between RIB and LA groups. Patients who received RIB block had PONV decreased occurrence primarily due to lower consumption of narcotics and less pain scores.
The two groups did not demonstrate statistically significant differences in pulmonary complications, probably because of the small sample size in the present study.
The current research has some limitations that need to be taken into account; first, there is no control group since it was deemed unethical to perform sham wound infiltration or a sham RIB. Second, we failed to assess the sensory dermatomal level. Eventually, chronic pain should also be taken into consideration following thoracic surgery, whereas only early postoperative pain was recorded in the present study, and we did not follow up further.
5. Conclusions
Our study showed that ultrasound guided RIB provides better pain relief and less post-operative opioid consumption after thoracoscopic surgeries, compared to local anesthetic infiltration.
Disclosure statement
No potential conflict of interest was reported by the authors.
References
- Miralpeix E, Nick AM, Meyer LA, et al. A call for new standard of care in perioperative gynecologic oncology practice: impact of enhanced recovery after surgery (ERAS) programs. Gynecol Oncol. 2016;141(2):371–378.
- Neustein SM, McCormick PJ. Postoperative analgesia after minimally invasive thoracoscopy: what should we do? Can J Anaesthes. 2011;58(5):423–5, 5–7
- Rosero EB, Joshi GP. Nationwide incidence of serious complications of epidural analgesia in the United States. Acta Anaesthesiol Scandinavica. 2016;60(6):810–820
- Chin KJ, McDonnell JG, Carvalho B, et al. Essentials of our current understanding: abdominal wall blocks. Region Anesthes Pain Med. 2017;42(2):133–183
- Elsharkawy H, Maniker R, Bolash R, et al. Rhomboid intercostal and subserratus plane block: a cadaveric and clinical evaluation. Region Anesthes Pain Med. 2018;43(7):745–751.
- Elsharkawy H, Saifullah T, Kolli S, et al. Rhomboid intercostal block. Anaesthesia. 2016;71(7):856–857.
- Öksüz G, Sayan M, Arslan M, et al. The comparison of serratus anterior plane block versus intercostal block for postoperative analgesia following thoracotomy surgery. Anestezi Dergisi. 2018;26:223–228.
- Kwon WK, Choi JW, Kang JE, et al. Long thoracic nerve block in video-assisted thoracoscopic wedge resection for pneumothorax. Anaesthes Intensive Care. 2012;40(5):773–779.
- Sihoe AD, Manlulu AV, Lee TW, et al. Pre-emptive local anesthesia for needlescopic video-assisted thoracic surgery: a randomized controlled trial. Eur J Cardiothorac Surg. 2007;31(1):103–108.
- Tulgar S, Thomas DT, Deveci U, et al., Ultrasound guided rhomboid intercostal block provides effective analgesia for excision of elastofibroma extending to the subscapular space: the first report of use in anesthesia practice. 2019;J Clin Anesthes. 52:34–35.
- Ökmen K. Efficacy of rhomboid intercostal block for analgesia after thoracotomy. Korean J Pain. 2019;32(2):129–132.