ABSTRACT
Background
Endotracheal intubation with the Macintosh has been associated with difficult visualization of the glottis, difficult intubation, high force,extensive manipulation with significant hemodynamic changes, which may be life threatening in vulnerable patients. We assume that Glidescope has less hemodynamic effects and less postoperative complication.
Methods
Ninety eligible patients with controlled hypertension were randomly allocated into two groups with 45 patient in each group, G group for the Glidescope and M group for the Macintosh. Both groups were compared for hemodynamic changes including systolic, diastolic, mean blood pressure, heart rate as primary outcome while first attempt success rate, number of attempts, Cormack Lehane score, postoperative sore throat, hoarseness of voice and airway injury as secondary outcome.
Results
Analysis of hemodynamic changes showed that the Glidescope decreased hemodynamic response to endotracheal intubation in controlled hypertensive patients with better intubation condition using Cormack Lehane score, first attempts success rate and number of needed trials compared to Macintosh laryngoscope. Also, Glidescope showed less post operative complications as sore throat and hoarseness of the voice; meanwhile, no airway injury happened in both groups. However, Glidescope needed more time for completion of intubation.
Conclusions
It could be concluded that using the Glidescope for endotracheal intubation in controlled hypertensive patients in comparison to Macintosh was associated with significant decrease in hemodynamic stress responses, decreased incidence of postoperative sore throat and hoarseness of voice and it improved the endotracheal intubation process.
1. Introduction
Endotracheal intubation is one of the commonest essential skill for many anesthesiologists [Citation1]. The traditional endotracheal intubation technique using the direct laryngoscopy Macintosh has significant impact on the patient hemodynamic system that results from stimulation of nociceptors in the pharynx, larynx and trachea during airway manipulation which send afferent impulses along the glossopharyngeal nerve and vagus nerve, respectively, leading to stimulation of the superior cervical sympathetic plexus resulting in exaggerated sympathetic neuro-hormonal changes [Citation2]; this hemodynamic stress response could be life threatening in patients with cardiovascular diseases [Citation3]. The magnitude of hemodynamic response is directly related to the force and duration of laryngoscopy [Citation4].
Postoperative sore throat and hoarseness of voice is an important issue following endotracheal intubation which results from soft tissue edema and mucosal erosions and may be significant enough to cause nerve injury [Citation5]. So, many techniques have been trialed to increase the success rate of endotracheal intubation, improving the quality of intubation condition and decreasing the needed force and manipulation and thus decreasing associated complications [Citation6].
The Glidoscope video laryngoscope is a device consisting of a blade with a 60° curvature and a handle in one piece; it has a camera under its surface for direct visualization of the glottis, and so it does not require alignment of the oropharyngeal axis to visualize the vocal cords [Citation7]. According to its design, less upward lifting force during laryngoscopy and intubation is required and this result in less hemodynamic effect and post operative complication [Citation8].
Hypertension is considered as a modified risk factor for the cardiovascular and cerebrovascular events; its long-term complications may be a cause of perioperative concern regardless of the hypertensive control. These complications affect variety of body systems from coronary heart disease, cerebrovascular accidents, cerebral infarctions up to hypertensive retinopathy and end stage kidney disease [Citation9].
It was reported that Glidescope had no significant advantage over Macintosh in attenuating circulatory response to endotracheal intubation in normotensive patients [Citation10]. Till now, few clinical trials investigated hemodynamic effects of Glidescope in hypertensive patients. We hypothesized that the Glidescope could induce less hemodynamic changes among hypertensive patients during endotracheal intubation and so the current study was designed to compare hemodynamic effects of Glidescope in comparison to Macintosh laryngoscope in controlled hypertensive patients as primary outcome. While the first attempt success rate, intubation time and postoperative airway complications were recorded as secondary outcome.
2. Patients and methods
This prospective randomized study was carried out over one year that started in November 2017 in Urology and Nephrology Centre, Mansoura University. After approval from Institutional Research Board, of faculty of medicine, Mansoura University with number Ms/17.10.93, it was registered at clinical trial with registrations number NCT03316443. Written informed consent was obtained from the patients aged more than 20 years old with American Society of Anesthesiologist score (ASA) II or ASA III and with controlled hypertension (Controlled hypertension was defined as a blood pressure around 140/90 mm Hg in hypertensive patient and if the patient is diabetic or has chronic renal disease it should be around 130/80 mm Hg) [Citation11]. Patients with body mass index less than 35, Mallampati score 1 or 2, thyromental distance more than 5 cm and central interincisor distance more than 3 cm were included. Patient’s refusal, uncontrolled hypertension, major cardiac diseases, cerebrovascular accident, with history of difficult intubation, facial deformity, cervical spine injury and patients who have any allergy from any drug used in this study were excluded.
2.1. Anesthetic management
On the day before surgery, pre-anesthetic checkup of all patients was done and the study protocol was explained to all patients and all patients fasted for 6 hours before the surgery. All patients received their regular antihypertensive medications till the morning of surgery.
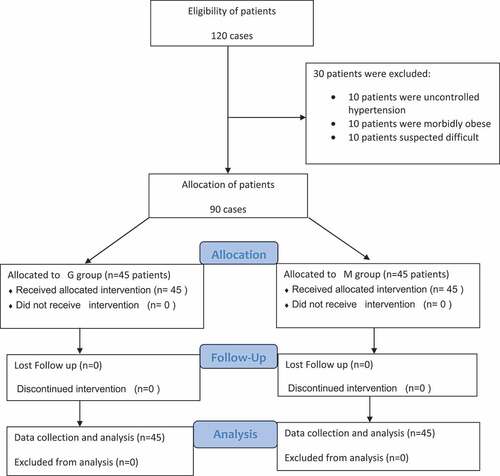
On arrival to the operation room, the routine monitoring including electrocardiogram, non-invasive blood pressure and pulse oximetry were set. Peripheral intravenous cannula was inserted and acetated Ringer was started at rate of 4–6 ml/kg/h. Induction of anesthesia was similar in all patients in both groups with pre-oxygenation for 5 min and then they received midazolam 0.02 mg/kg, fentanyl 1 μg/kg and Propofol 2 mg/kg slowly intravenously until loss of verbal contact, and then rocuronium 0.6 mg/kg with establishment of adequate neuromuscular block, controlled ventilation was carried out using a face mask with 100% oxygen. After 3 min of establishment of adequate neuromuscular block, the trachea was intubated randomly using either Glidescope or Macintosh laryngoscope according to group randomization. Eligible 90 adult patients were randomly allocated by a computer-generated randomization sequence into two equal groups with 45 patients in each group. Macintosh group (Group M) with 45 patients were intubated by Macintosh laryngoscope and Glidescope group (Group G) with 45 patients were intubated by Glidescope ().
All patients were intubated by a suitable sized tube (in males 8 mm and in females 7.5 mm internal diameter). In Macintosh group, we used a blade size 3 at first and if failed then blade size 4 was used. The laryngoscope was advanced in patient`s mouth displacing the tongue laterally, till the Macintosh blade’s tip positioned in the vallecula, and then the base of the tongue was displaced upward and forward till exposure of the glottis, then the endotracheal tube was advanced into the trachea. In Glidescope group, size 3 blade was used and if failed then blade size 4 was used. Glidescope was introduced gently throw the mouth and was slid down along the midline of the tongue, till Glidescope blade’s tip was positioned in the vallecula, and then gentle lifting force was applied for exposure of the glottis. The endotracheal tube was loaded on the 60 degree bent stylet of the Glidescope and when the glottis was exposed it was inserted into the trachea by the same operator.
External pressure to the front of the neck was applied on request of the operator by another anesthetist. All intubation processes were performed by a single expert anesthetist. After placement of the endotracheal tube, the cuff of the tube was inflated gradually and controlled ventilation was started. When carbon dioxide trace was displayed, chest was auscultated to ensure proper tracheal positioning and to exclude bronchial intubation and then the tube was fixed. All patients were mechanically ventilated with tidal volumes of 6–8 ml/kg, with respiratory rate 12 breath per min and positive end expiratory pressure 5–8 cmH2O to keep end tidal carbon dioxide around 30–35 mmHg. Anesthesia was maintained in all patients using (1–1.5%) minimum alveolar concentration of sevoflurane in oxygen/air mixture with Fio2 about 35–40%.
2.2. Monitoring
Systolic blood pressure, diastolic blood pressure, mean arterial blood pressure and heart rate were recorded at the basal, after induction and immediately before intubation, immediately after completion of intubation, after 1 min of intubation, after 2 min of intubation, after 3 min of intubation, after 5 min of intubation and after 10 min of intubation. The intubation attempt failure was defined when the intubation times exceed 120 seconds, esophageal intubation occurrence or desaturation with arterial oxygen saturation drop below 90%. Only three attempts were allowed, and then anesthesia was carried out according to decision of the attending anesthetist with exclusion of the case from the study. Face-mask intermittent positive pressure ventilation with 100% oxygen was carried out in between the intubation attempts. The intubation process was assessed using first attempt success rate, number of attempts, intubation time and Cormack Lehane score. The intubation time was defined as the period from termination of face mask oxygenation and insertion of the blade into the patient mouth till the appearance of carbon dioxide trace after positive pressure ventilation [Citation12]. Cormack Lehane score is based on the laryngoscopic view as following: grade 1: full view of the glottis, grade 2: partial view of the glottis, grade 3: only the epiglottis appear and grade 4: neither the glottis nor the epiglottis appear [Citation13].
2.3. Postoperative follow up
All patients were assessed postoperatively for the sore throat and hoarseness of voice according to the 4-point score [Citation14].
Sore throat was graded as none = 0, mild = 1 (less severe than with common cold), moderate = 2 (similar to common cold), severe = 3 (more severe than with common cold). Hoarseness of voice was graded as none = 0, mild = 1 (noted only by the patient), moderate = 2 (obvious to the observer), sever = 3 (like aphonia).
2.4. Statistical analysis
Sample size was calculated using G*power analysis program, by using a prior power analysis with accuracy mode calculation. The power analysis was based on a previous pilot study of 20 patients. The sample size was selected to detect the incidence of 25% increase in mean arterial blood pressure above the basal values as a difference in between the studied groups. A sample of 45 patients for each group will be required to achieve a power of 80% (two tailed) with α-error of 0.05.
The collected data were coded, processed and analyzed using the SPSS (Statistical Package for Social Sciences) version 22 for Windows® (SPSS Inc, Chicago, IL, USA). Qualitative data were presented as number percentage. The two groups were compared for qualitative data by Chi-Square test (χ2). Quantitative data was tested for normality by Kolmogorov-Smirnov test. Normally distributed data were presented as mean ± SD. Independent Student t-test was used for comparison between the two groups. Paired samples t-test was used to compare patients in the same groups at different time points. P-value <0.05 was considered to be statistically significant.
3. Results
Ninety adult patients of both sex aged above 20 years were randomly allocated into two groups (45 patients in each) and they completed this randomized clinical trial. The demographic data were comparable in both groups (). Associated comorbidities, antihypertensive medications used, preoperative assessment of Mallampati score, mean central inter-incisor distance and mean thyromental distance in both studied groups values are recorded in with no statistical significant differences between both studied groups.
Table 1. Demographic data in both studied groups
Table 2. Associated comorbidities, antihypertensive medication and preoperative airway assessment in both studied groups
Systolic blood pressure changes in response to intubation showed significant decrease in both studied groups in comparison to basal value at induction of anesthesia up to 10 min of intubation except at immediate after intubation in which G group showed significant decrease (134.64 ± 11.70) compared to basal value but M group showed no significant difference in the systolic blood pressure compared to its basal value (.
Table 3. Systolic blood pressure (mmhg) changes in both studied groups
Regarding diastolic blood pressure changes in response to intubation immediately before intubation up to 10 min of intubation process, the diastolic blood pressure in both studied groups significantly dropped with both groups with nearly equal values compared to their basal value (P ≤ 0.0001) except that immediately after intubation, diastolic blood pressure in M group showed significant increase (97.04 ± 9.29) from the basal value in comparison to G group (82.58 ± 13.32) (p < 0.0001) (.
Table 4. Diastolic blood pressure (mmhg) changes in both studied groups
shows that the mean arterial blood pressure significantly increased immediately after intubation in M group (106.22 ± 10.88) compared to its basal, while G group showed significant drop (93.62 ± 9.53) from its basal value and as well after 1 min of intubation mean arterial blood significantly higher in M group (95.78 ± 9.96) compared to G group (85.51 ± 8.12) (p < 0.0001).
Table 5. Mean arterial blood pressure (mmhg) changes in both studied groups
shows that the heart rate changes in response to intubation process immediately after intubation in M group increased (92 ± 17.1) in comparison to its basal value and it is also significantly higher in comparison to G group (84 ± 14.56); however, after 1 min of intubation process, G group showed significant decrease in mean heart rate (79 ± 13.95) in comparison to its basal value, which was also significantly decreased more than the decrease in M group (82 ± 14.27) (p < 0.0001).
Table 6. Heart rate data (beat/min) in both studied groups
demonstrates the characteristics of the process of intubation in which external cricoid pressure was applied in 1 case only in G group while it was applied in 12 cases in M group with (p < 0.0001) and there was no need to change the blade from 3 to 4 in G group while it was needed in four patients in M group with no significant difference between both groups. Stylet was used in all patients in G group (100%) while it was applied only in eight cases in M group. The mean intubation time in G group was prolonged (26.44 ± 4.07 s) than in M group (19.18 ± 5.90 s). on the other hand, all cases in G group underwent successful intubation in the first trial while in M group, 40 cases showed first attempt success and the other 5 cases which showed no successful attempt in the first trial were intubated successfully after the second trial with significant difference between both studied groups.
Table 7. Characteristic of the intubation process and examination of patients by Cormack lehane score in both studied groups
Mean arterial oxygen saturation changes in both studied groups showed that the mean basal oxygen saturation in both groups was above 99%, and that continues till the end of the 10 min post intubation interval without significant changes in both groups.
In , regarding analysis of post-operative complications in both groups, all cases in G group had no sore throat after intubation while in M group 40 cases (88.9%) had no sore throat after intubation and 5 cases (11.1%) had post-operative sore throat of grade 1. Regarding post-operative hoarseness of voice, all cases in G group had no hoarseness of voice after intubation while in M group, 40 cases (88.9%) had no hoarseness of voice after intubation and 5 cases (11.1%) had post-operative hoarseness of voice of grade 1. No cases complained from post-operative airway injury in both groups.
Table 8. Post intubation complications in both studied group
4. Discussion
Hemodynamic response to laryngoscope and tracheal intubation remains of utmost concern in anesthesia practice. Sympathetic stimulation and adverse physiologic events could be tolerated by healthy individuals, but it may be detrimental in hypertensive patients. Macintosh laryngoscopy to view the glottic opening requires alignment of oral, pharyngeal and tracheal axes in one line, causing tissue stretch painful stimulus with subsequent stress response .while with the use of videolaryngoscopic devices for tracheal intubation the lifting forces needed to visualize the glottis may be reduced leading to attenuation of hemodynamic stress responses to endotracheal intubation [Citation15].
The current study demonstrated that both blood pressure and heart rate increased significantly immediately after endotracheal intubation in the Macintosh group. On the other hand, the Glidescope group showed decreased both blood pressure and heart rate immediately after endotracheal intubation process.
These results of our study could be explained by the fact that the unique design of Glidescope provided advantages make it superior to the Macintosh laryngoscope and other videoassisted devices regardless of the Mallampati class or difficult intubation as Glidescope does not require alignment of oropharyngeal axis to visualize the glottis and so less upward lifting force with less manipulation of pharyngeal structures is needed during intubation, producing less stimulation of the pharyngeal and laryngo-tracheal noci-ceptors with subsequent attenuation of the sympathetic neuro-hormonal changes.
In agreement with the current study, Amini and Shakib, when they designed study on patients undergoing caesarean section, claimed that the Glidescope has significant hemodynamic changes in comparison to the Macintosh in first 3 min after intubation. Later on, they were similar in both groups [Citation16]. Also, in another study by Bankar on comparing the hemodynamic response associated with using both i-scope videolaryngoscope and Macintosh laryngoscope in controlled hypertensive patients, they founded that heart rate and blood pressure in Macintosh laryngoscope were significantly higher than with the i-scope video laryngoscope [Citation17]. There were fewer studies on hypertensive patients [Citation18]; however, there were several studies on normal patients that found that hemodynamic stress responses to intubation was similar in both videolaryngoscope and Macintosh. A study by İnangil, comparing the hemodynamic response associated with endotracheal intubation by using both Glidescope and Macintosh in normotensive patients, found that the Glidescope does not have any advantage in comparison to Macintosh laryngoscope as regard hemodynamic response and they claimed that the long time needed by the Glidescope resulted in equal hemodynamic response in both groups [Citation10]. Also, in a meta-analysis by Hoshijima et al., who performed a comprehensive database search from 13 articles comparing hemodynamic response (including heart rate and mean blood pressure) to tracheal intubation with the Glidescope and Macintosh laryngoscope, found that Glidescope did not lower the hemodynamic response after tracheal intubation when compared with the Macintosh laryngoscope [Citation19] and this could be explained and supported by Abdelgawad et al.’s study that comparing cardiac output and hemodynamic response of intubation among different video laryngoscopies in normotensive and hypertensive patients, they founded that both video laryngoscopies and video intubation stylet devices attenuated only the hemodynamic response to intubation compared to the Macintosh laryngoscope only in hypertensive patients but not in normotensive patients which may be due to the fact that in hypertensive patients the hemodynamic stress response exaggerated in comparison to normotensive patients which could be probably due to increased catecholamine levels with marked peripheral vessels sensitivity to this circulating catecholamines [Citation20].
The Glidescope has antifog mechanism that prevents clouding of the image on the video display, allowing for clear magnified view and recognition of different anatomical structures and anomalies in the airway, but longer intubation time was required as the stylet loaded with endotracheal tube was inserted by the side of the blade till the tip of tube faces the trachea and then the stylet should be withdrawn and tube involved into trachea and so it considered as disadvantage of Glidescope compared to Macintosh laryngoscopes [Citation21]. On the analysis of the characteristics of the intubation process, the current study founded that the Glidescope group showed better intubation conditions as regard the need for external cricoid pressure, need for changing the blade size, first attempt success, number of attempts and Cormack Lehane score but with prolonged intubation time in comparison to M group. The same operator (with a reasonable level of experience) performed the intubation in all cases which minimizes the risk of bias of different level of experience when multiple operators were involved.
In parallel with the current study, a study by Jafra on 200 patients of suspected easy intubation to assess the intubation process criteria by the Glidescope in comparison to the Macintosh found that the mean intubation time was significantly shorter in the Macintosh group and he claimed that it was statistically significant but clinically not relevant as it does not affect the arterial oxygen saturation [Citation22].
While in contrast to current study, Choi and his colleague designed a multicentric study, where the first attempt success rates were not significantly different (85.7% in the Glidescope group and 82.3% in the Macintosh group); they explained that it is due to presence of operators with different level of skills and experience [Citation23]. On the other hand, Nandakumar investigated the quality of intubation process in 45 morbidly obese patients using Glidescope, Macintosh and McCoy and reported that the intubation time was significantly longer in Glidescope group but the Cormack Lehane score and intubation difficulty scale had no significant difference between the three devices which may be due to the high level of skill of the investigator who performed intubation process [Citation24].
But when Akbarzadeh compared the intubation condition in 102 obese patients using Glidescope, Macintosh and McCoy, he found that the Glidescope group shows significant improvement of the glottic view and less intubation time than the other groups [Citation25].
Because of less manipulation and less force applied with the Glidoscope compared to the Macintosh, it is suspected to be associated with less postoperative complications and airway injury; Thus, in the current study, regarding the postoperative complications like sore throat, hoarseness of voice and airway injury, the Glidescope is considered very superior as no complications were reported. While five patients developed mild sore throat and developed mild hoarseness of voice in the Macintosh group, no airway injury occurred in both groups. Similarly, in different studies by Aqil and Najafi, they founded that the incidence and severity of postoperative sore throat and hoarseness of voice was significantly lower in the Glidescope group than in the Macintosh laryngoscope group [Citation5,Citation26].
4.1. The limitations of the study include
First, there was a lack of the blindness. Second, monitoring of the stress response better to be done by the estimation of the stress hormones like cortisol and catecholamines, which was not available at the time of the study. Finally, the study was not applied for patients with possible difficult airway.
5. Conclusions
From the results of the current study, it could be concluded that using the Glidescope for endotracheal intubation in controlled hypertensive patients in comparison to Macintosh laryngoscope was associated with significant decrease in hemodynamic changes including heart rate, blood pressure immediately after intubation and for 1 min after intubation with decreased incidence of postoperative complications regarding sore throat and hoarseness of voice and improved conditions of endotracheal intubation process, while it required more time for completion of intubation.
Authors’ contributions
Study design: Mahmoud M Othman, Salwa MS Hayes,
Ibrahim A Elbaser, Ahmed M A Bobo.
Patient recruitment: Mahmoud M Othman, MDˡ, Ahmed M A Bobo
Data collection and analysis: Mahmoud M Othman, Salwa MS Hayes,
Ibrahim A Elbaser, Ahmed M A Bobo.
Disclosure statement
No potential conflict of interest was reported by the authors.
References.
- Panda N, Donahue DM. Acute airway management. Ann Cardiothorac Surg. 2018;7(2):266–272.
- Yoo KY, Jeong CW, Kim SJ, et al. Altered cardiovascular responses to tracheal intubation in patients with complete spinal cord injury: relation to time course and affected level. Br J Anaesth. 2010;105:753–759.
- Shyam R, Chaudhary AK, Sachan P, et al. Evaluation of fastrach laryngeal mask airway as an alternative to fiberoptic bronchoscope to manage difficult airway: a comparative study. J Clin Diagn Res. 2017;11(1):UC09–UC12.
- Ahmed SM, Doley K, Athar M, et al. Comparison of endotracheal intubation time in neutral position between C-Mac and airtraq laryngoscopes: a prospective randomized study. Indian J Anaesth. 2017;61(4):338–343.
- Aqil M, Khan MU, Mansoor S, et al. Incidence and severity of postoperative sore throat: a randomized comparison of Glidoscope with Macintosh laryngoscope. BMC Anesthesiol. 2017;17:127.
- Nakanishi T, Shiga T, Homma Y, et al. Comparison of the force applied on oral structures during intubation attempts by novice physicians between the Macintosh direct laryngoscope, airway scope and C-MAC PM: a high-fidelity simulator-based study. BMJ Open. 2016;6(5):e011039.
- Vargas M, Pastore A, Aloj F, et al. A comparison of video laryngoscopes for tracheal intubation in predicted difficult airway: a feasibility study. BMC Anesthesiol. 2017;17:25.
- Mahjoubifar M, Borjian Boroojeny S. Hemodynamic changes during orotracheal intubation with the Glidescope and direct laryngoscope. Iran Red Crescent Med J. 2010;12(4):406–408.
- Sim JJ, Bhandari SK, Shi J, et al. Comparative risk of renal, cardiovascular, and mortality outcomes in controlled, uncontrolled resistant, and non-resistant hypertension. Kidney Int. 2015;88(3):622–632.
- İnangil G, Cansız K, Gürbüz F, et al. Comparison of hemodynamic responses to endotracheal intubation with the GlideScope video laryngoscope and Macintosh laryngoscope in patients undergoing cardiovascular surgery. J Thorac Cardiovasc Surg. 2018;26:386–393.
- Houlihan SJ, Simpson SH, Cave AJ, et al. Hypertension treatment and control rates: chart review in an academic family medicine clinic. Can Family Physician. 2009;55(7):735–741.
- Rai MR, Dering A, Verghese C. The Glidescope system: a clinical assessment of performance. Anaesthesia. 2005;60:60–64.
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39:1105–1111.
- Stout DM, Bishop MJ, Dwersteg JF, et al. Correlation of endotracheal tube size with sore throat and hoarseness following general anesthesia. Anesthesiology. 1987;67:419–421.
- Kumar D, Gombar S, Ahuja V, et al. Glidescopic versus D-blade for tracheal intubation in cervical spine patients: a randomized controlled trial. Indian J Anaesth. 2019;63(7):544–550.
- Amini S, Shakib M. Hemodynamic changes following endotracheal intubation in patients undergoing cesarean section with general anesthesia: application of glidescope videolaryngoscope versus direct laryngoscope. Anesth Pain Med. 2015;5(2):e21836.
- Bankar P, Kachru N, Yadav R. Hemodynamic stress response in controlled hypertensive patients: a randomized comparison of I-scope video laryngoscope and Macintosh laryngoscope. Arch Anesthesiol Critical Care. 2022;8(1):11–17.
- Ali QE, Amir SH, Jamil S, et al. A comparative evaluation of the Airtraq and king Vision video laryngoscope as an intubation aid in adult patients. Acta Anaesthesiol Belg. 2015;66:81–85.
- Hoshijima H, Maruyama K, Mihara T, et al. Use of the glidescope does not lower the hemodynamic response to tracheal intubation more than the Macintosh laryngoscope: a systematic review and meta-analysis. Medicine (Baltimore). 2020;99:48e23345.
- Abdelgawad AF, Shi QF, Abo Halawa M, et al. Comparison of cardiac output and hemodynamic responses of intubation among different videolaryngoscopies in normotensive and hypertensive patients. J Huazhong Univ Sci Technol Med Sci. 2015;35:432–438.
- Cordovani D, Russell T, Wee W, et al. Measurement of forces applied using a Macintosh direct laryngoscope compared with a Glidescope video laryngoscope in patients with predictors of difficult laryngoscopy: a randomised controlled trial. Eur J Anaesth. 2019;36(3):221–226.
- Jafra A, Gombar S, Kapoor D, et al. A prospective randomized controlled study to evaluate and compare GlideScope with Macintosh laryngoscope for ease of endotracheal intubation in adult patients undergoing elective surgery under general anesthesia. Saudi J Anaesth. 2018;12(2):272–278.
- Choi HJ, Kim Y-M, Oh YM. Choi HJ, Kim YM, Oh YM, Kang HG, Yim HW, Jeong SH. GlideScope video laryngoscopy versus direct laryngoscopy in the emergency department: a propensity score-matched analysis. BMJ Open. 2015;5(5):e007884.
- Nandakumar KP, Bhalla AP, Pandey RK, et al. Comparison of Macintosh, McCoy, and Glidescope video laryngoscope for intubation in morbidly obese patients: randomized controlled trial. Saudi J Anaesth. 2018;12(3):433–439.
- Akbarzadeh SR, Taghavi Gillani M, Tabari M, et al. Comparative analysis of the usefulness of the GlideScope, Macintosh, and McCoy laryngoscopes for endotracheal intubation in patients with obesity: a randomized, clinical trial. Anesth Pain Med. 2017;7(6):57913.
- Najafi A, Imani F, Makarem J, et al. Postoperative sore throat after laryngoscopy with macintosh or glide scope video laryngoscope blade in normal airway patients. Anesth Pain Med. 2014;4(1):e15136.