ABSTRACT
Objectives
To evaluate the ability of at-admission (Day 1) estimated serum levels of inflammatory biomarkers and clinical scorings for prediction of survival outcome of sepsis patients admitted to surgical ICU.
Patients & Methods
One hundred and seventy-eight patients were clinically evaluated and gave blood samples for estimation of serum biomarkers’ levels (Day 1 data) and re-evaluated on Days 2–3 for the National Early Warning-2 (NEWS-2) score and Day 3 for the Sequential organ failure assessment (SOFA) score and serum level of presepsin (PSP). During 28-day, patients were grouped according to survival outcome as Survivors and Non-survivors.
Results
Day1 clinical scorings and biomarkers’ levels were significantly higher in non-survivors (n = 41) than survivors (n = 137). Day 3 SOFA scores of all patients were significantly higher than Day1 scores with significantly higher scores for non-survivors. Through Day1-3, the number of patients with high-grade risk on NEWS2 was significantly higher among non-survivors. Day-3 serum PSP levels were significantly decreased in survivors, while increased in non-survivors. The statistical analyses defined high NEWS2, SOFA, PSP, and procalcitonin serum levels as the significant predictors of mortality. Diagnostic performance characteristics of combined NEWS score and PSP showed high sensitivity, specificity, and accuracy rates with a 99% negative predictive value for survival outcomes.
Conclusion
Sequential estimation of NEWS2 score and serum PSP can discriminate between high-risk patients and those prone to die. Coupling of NEWS-2 scoring and estimation of serum PSP allowed more accurate early identification of patients vulnerable to deterioration with high sensitivity and accuracy rates.
1. Introduction
Sepsis management is still one of the most important challenges in modern clinical practice because the rapid progression of sepsis to septic shock is practically unpredictable [Citation1]. Septic shock patients are prone to altered fibrinolysis, which contributes to microthrombus formation, organ failure, and mortality [Citation2].
The low positivity of traditional diagnostic methods of sepsis and septic shock may be secondary to the influence of the quality and quantity of specimens, the severity of infection, and laboratory sufficiency [Citation3]. This necessitated the search for biomarkers that can help clinicians in the management of sepsis patients to reduce the probability of a fatal outcome [Citation4].
Presepsin (PSP) is a 13 kDa, a small soluble peptide that consists of 64 amino acids [Citation5] and is truncated from a soluble cluster of differentiation 14 (CD14) by circulating plasma proteases [Citation6]. The CD14 is one of the leukocyte differentiation antigens that is present in macrophages, monocytes, granulocytes, and their cell membranes [Citation7].
Failure to recognize a deteriorating patient is a common cause of serious adverse events [Citation8]. Physiological track and trigger systems are designed to help to identify and respond to patients at risk of clinical deterioration [Citation9]. The National Early Warning Score (NEWS) was developed by the Royal College of Physicians in England to standardize early warning scores and is probably the best-validated EWS for recognition of sepsis [Citation10].
2. Objectives
This study targets to evaluate the ability of at-admission estimated serum levels of inflammatory biomarkers and clinical scorings for prediction of survival outcome of sepsis patients admitted to ICU.
2.1. Design
Prospective comparative study
2.2. Setting
Departments of Anesthesia and ICU, and Medical Biochemistry, Faculty of Medicine, Benha University
3. Patients & methods
All patients admitted to the Surgical ICU at Benha University Hospital with manifestations suggestive of sepsis were eligible for evaluation of inclusion and exclusion criteria.
3.1. Exclusion criteria
Patients who had immunosuppressive, cardiac, hepatic diseases, acute kidney injury, hemorrhagic shock, or maintained on immunosuppressant therapy, or renal supplemental therapy were excluded from the study. Also, patients with definite or fulminant infection anywhere in the body who underwent major surgical procedures, especially cancer surgeries, or were suspected to die during their ICU stay were excluded from the study.
3.2. Clinical assessment tools
Sepsis and septic shock were defined according to the 3rd International consensus definitions; sepsis was defined as life-threatening organ dysfunction secondary to the deregulated host response to infection [Citation11]. Septic shock was defined as sepsis with profound circulatory, cellular, and metabolic abnormalities and was clinically identified by serum lactate level of >18 mg/dl, concurrent hypotension requiring vasopressor therapy to maintain a mean arterial pressure (MAP) of ≥65 mmHg in absence of hypovolemia [Citation12] and is associated with an in-hospital mortality rate (MR) of 30–50% [Citation13].
(2) The Sequential [Sepsis-related] Organ Failure Assessment (SOFA) score
SOFA score allows for the calculation of both the number and the severity of organ dysfunction in six organ systems (respiratory, coagulation, liver, cardiovascular, renal, and neurologic) and the score can measure individual or aggregate organ dysfunction that was defined as individual SOFA score of ≥2 points [Citation14], which is the predetermined cutoff point for in-hospital mortality rate (MR) of >10% [Citation15].
(3) Acute Physiology and Chronic Health Evaluation II (APACHE II) Score
APACHE II score is the severity of disease classification system using point scores for initial values of 12 routine physiological measures, age, and previous health status to provide a score ranging from 0 to 71 with the higher is the score, the higher the mortality risk [Citation16].
(4) The National Early Warning Score (NEWS2)
NEWS2 is based on six vital signs including respiratory rate, oxygen saturation, systolic blood pressure, heart rate, consciousness, and temperature. A NEWS2 score categorizes patients as low, medium, or high-risk patients and guides the frequency of monitoring with a score of zero indicating the need for 12-hr monitoring, a score of 1–4 indicating the need for monitoring every 4–6 h and a score of 5–6 indicates medium risk and potential serious acute clinical deterioration that necessitates hourly monitoring [Citation17], while a NEWS2 score of ≥7 indicates high risk and severe clinical deterioration with the need for continuous monitoring [Citation18].
3.3. Laboratory investigations
At the time of ICU admission, peripheral venous blood samples were obtained by venipuncture under complete aseptic conditions and without the use of a tourniquet by a lab assistant who was blinded about the diagnosis. Blood samples were collected in plain tubes, allowed to clot in a warm water bath at a temp of 37°C for 5 minutes, and then centrifuged at 5000 rpm for 2 minutes to separate serum, which is divided into two parts:
The first part was used for photocolorimeteric estimation of serum lactate levels according to the manufacturer’s instructions [Citation19].
The 2nd part was collected in Eppendorf tubes for estimation of serum procalcitonin (PCT), C-reactive protein (CRP), and presepsin (P-SEP) using enzyme-linked immunosorbent assay (ELISA) kits according to the manufacturer’s instructions and were read using a 96 well microplate ELISA reader (Dynatech. MR 7000):
Human serum PCT level was estimated using an ELISA kit (catalog no. ab221828, Abcam Inc., San Francisco, USA) by quantitative sandwich enzyme immunoassay technique [Citation20].
Human CRP level using ELISA kit (catalog no. ab99995, Abcam Inc., San Francisco, USA) by quantitative sandwich enzyme immunoassay technique [Citation21].
Human prespesin (PSP) level using ELISA kit (catalog no. MBS766136, MyBioSource Inc., San Diego, California, USA) by quantitative sandwich enzyme immunoassay technique [Citation22].
3.4. Study outcomes
The primary outcome is the ability of clinical scorings alone or in conjunction with biomarkers for the prediction of the 28-day ICU mortality rate
Secondary outcomes
The extent of change in NEWS-2 and SOFA scores and serum presepsin levels on the 3rd day after ICU admission was calculated as ∆ = Day3- Day1
Evaluation of the significance of the change concerning mortality.
3.5. Statistical analysis
Obtained data were presented as mean, standard deviation, numbers, percentages, and median and interquartile ranges. Results were analyzed using one-way ANOVA for analysis of variance between groups, paired t-test for analysis within each group, Chi-square test (X2 test) for analysis of non-numeric data, and Mann–Whitney test for median values. Predictability of studied parameters for discrimination of sepsis patients vulnerable to death was evaluated using the receiver operating characteristic (ROC) curve analysis judged by the area under the curve (AUC) compared versus the null hypothesis that AUC = 0.05. Regression analysis (Stepwise method) was used for the stratification of studied parameters as specific predictors. Statistical analysis was conducted using IBM® SPSS® Statistics (Version 22, 2015; Armonk, USA) for Windows statistical package. P-value <0.05 was considered statistically significant.
4. Results
During the study duration from June 2019 to Nov 2021, 231 sepsis patients were admitted to the surgical ICU at Benha University Hospital, 53 patients were excluded for not fulfilling the inclusion criteria, and 178 patients were enrolled in the study. Throughout the 28-day follow-up at ICU, 41 patients (23%) died, non-survivors were significantly older (p = 0.048) and showed a significantly (p = 0.037) higher frequency of the need for mechanical ventilation than survivors. At-admission data of all patients categorized according to 28-day survival outcome is shown in .
Table 1. At-admission data of studied patients categorized according to 28-day survival.
During the duration since ICU admission (Day-1) till D-3, all the clinical scorings of non-survivors were significantly higher in comparison to the scorings of survivors. Day-3 SOFA score was significantly higher compared to the Day-1 score of all patients, but the ∆SOFA was significantly higher in non-survivors than in survivors. As regards the NEWS-2, from Day1 to Day3, patients’ distribution according to the risk grades of NEW-2 score showed a significant (p < 0.0001) difference between survivors and non-survivors with a significantly higher frequency of patients of high-risk grade among non-survivors. The median values of NEWS-2 scores were significantly higher among non-survivors than the survivors during days 1-3 with significantly higher ∆NEWS2 for non-survivors ().
Table 2. Clinical scorings of studied patients categorized according to 28-day survival.
Estimated levels of sepsis-associated laboratory variables were significantly higher in non-survivors compared to the levels estimated in survivors. On Day-3 serum, presepsin levels were significantly decreased in survivors (p < 0.0001), while were significantly (p = 0.0001) increased in non-survivors with significantly (p < 0.0001) higher levels in sera of non-survivors compared to survivors. Moreover, the median value of ∆PSP of non-survivors was significantly higher in comparison to that of survivors ().
Table 3. Laboratory findings of studied patients categorized according to 28-day survival.
Correlation analysis showed a negative significant correlation between survival rate and patients’ age and at-admission APACHE II, SOFA, and NEWS-2 clinical scorings and total leukocytic count, plasma lactate levels, and serum levels of CRP, PCT, and PSP. At-admission, the NEWS-2 score showed a positive significant correlation with the APACHE II score, plasma lactate levels, and serum PSP levels. Serum PSP levels estimated at ICU admission showed a positive significant correlation with APACHE II, SOFA, and NEWS-2 clinical scores and with plasma lactate levels and serum CRP levels ().
Table 4. Spearman’s correlation between survival rate, NEWS-2 clinical scores, serum P-SEP levels, and other studied variables studied in patients admitted to surgical ICU.
Regression analysis of variables correlated with mortality defined high at-admission NEWS-2 score, serum PSP, SOFA score, and serum PCT as the significant independent variables for the prediction of mortality. ROC curve analysis defined high at-admission NEWS-2 score and serum PSP as positive independent predictors for mortality with moderate accuracy, while high at-admission SOFA score and serum PCT levels as positive predictors for mortality with weak accuracy as judged by the area under the curve (, ).
Figure 1. ROC curve analysis of at-admission clinical scorings and lab parameters of studied patients for prediction of upcoming 28-day ICU mortality of sepsis patients.
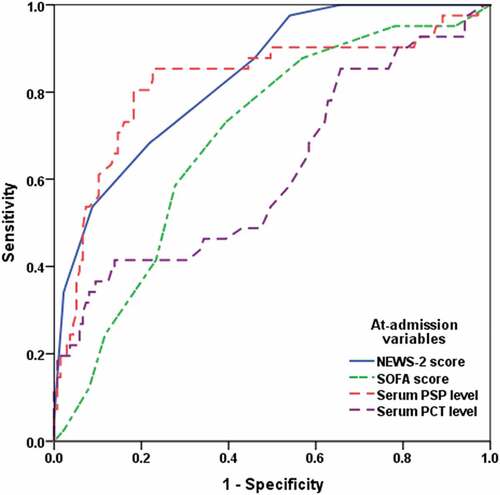
Table 5. Statistical analyses of at-admission clinical and lab variables of studied patients for prediction of the upcoming 28-day mortality of sepsis patients.
The diagnostic performance characters of NEWS-2 score and serum PSP estimated at-admission using the median value for each (5 for NEWS-2 and 432 for PSP) separately and in combination were improved on the application of both variables as a diagnostic tool with sensitivity and negative predictive value for mortality of 97.6 and 99%, respectively, and specificity of 73.7% and accuracy rate for prediction of mortality by 79.2% ().
Table 6. The diagnostic performance characters of at-admission NEWS-2 score and serum PSP levels as predictors for mortality of sepsis patients admitted to surgical ICU.
5. Discussion
The application of the National Early Warning score-2 (NEWS-2) for daily evaluation of sepsis patients at ICU allowed discrimination of patients improving and those deteriorating using a cutoff point of ≥5 on the at-admission NEWS-2 score. The selected cutoff point for differentiation coincided with the recently documented that NEWS2 is an effective predictor of mortality for emergency department patients and suggested a maximum NEWS2 score of ≥4 as the best trigger point for escalation of treatment [Citation23].
At-admission, the NEWS-2 score showed higher specificity and negative predictive value than at-admission APACHE II and SOFA scores. Moreover, sequential NEWS-2 evaluation for 3 days allowed identification of 34 patients of the 41 patients who died at the end of 28-ICU stay, thus it provided a correct prediction of mortality by a rate of 82.9%. This high predictive ability of NEWS-2 score for deterioration and mortality was assured statistically by ROC curve analysis (AUC = 0.834) and by regression analysis.
In line with these findings, a recent study found NEWS-2 could predict admission to ICU and mortality of a high percentage of those admitted to ICU for their disease severity with an AUC = 0.9 [Citation24]. Another study documented that NEWS2 at a cutoff point of ≥7 had significantly greater AUC than other screening tools at Emergency Triage for the prediction of sepsis among ambulance patients with clinically suspected infection [Citation25]. In a similar comparison of NEWS2 and SOFA scores, a recent study reported that the 3-day NEWS2 had good discrimination for predicting 7-, 14-, 21-, and 28-day mortalities and was not inferior to the SOFA [Citation26].
The ability of at-admission serum presepsin to discriminate ICU sepsis patients vulnerable to die was superior to the ability of TLC, CRP, and PCT, with an AUC = 0.822. In line with these findings, multiple studies assured the superiority of estimated serum presepsin over other biomarkers as an early marker for discrimination of septic patients who are vulnerable to progression to septic shock or deterioration and death [Citation27–29]. Moreover, two recent studies documented that PSP has a reliable early diagnostic ability for sepsis comparable to that of PCT [Citation30] and could be a useful marker for prognosis of sepsis severity and mortality risk [Citation31].
Estimation of diagnostic performance characters assured the sensitivity and negative predictive value of high day-1 presepsin levels as an early predictor of mortality of sepsis patients admitted to surgical ICU with high accuracy rate than the NEWS-2 score. Similarly, a recent study assured the higher accuracy of early presepsin measurement in ICU patients for the diagnosis of sepsis and the prediction of mortality in comparison to quick SOFA or systemic inflammatory response syndrome scores [Citation32]. Moreover, the performance characteristics of NEWS-2 as a predictor for mortality were increased when combined with presepsin and both could predict mortality with a sensitivity rate of 97% and negative predictive value of 99%, and specificity and accuracy rates of 73.7% and 79.2%, respectively. In line with these findings, one recent study found that combined estimation of serum presepsin levels with the Glasgow Prognostic Score increased the specificity of clinical scoring for predicting septic acute respiratory distress syndrome [Citation33]. Another recent study suggested that NEWS2 score and laboratory illness severity as calculated by a frailty index were independently associated with post-discharge survival of older adults admitted to ICU with acute clinical conditions [Citation34].
6. Conclusion
At-admission high NEWS-2 clinical score and serum PSP could discriminate sepsis patients who were prone to death with high sensitivity and negative predictive value. Coupling of NEWS-2 scoring and serum PSP allowed more accurate early identification of patients vulnerable to deterioration with high-performance characters. Sequential estimation of both variables can discriminate high-risk patients and thus allows early modification of management plans.
6.1. Limitation
The study was a single-center study and results need multicenter comparative studies to be established.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Beltrán-García J, Manclús J, García-López E, et al. Comparative analysis of chromatin-delivered biomarkers in the monitoring of sepsis and septic shock: a pilot study. Int J Mol Sci. 2021 Sep 14;22(18):9935.
- Larsen J, Aggerbeck M, Larsen K, et al. Fibrin network formation and lysis in septic shock patients. Int J Mol Sci. 2021 Sep 2;22(17):9540.
- Memar MY, Baghi HB. Presepsin: a promising biomarker for the detection of bacterial infections. Biomed Pharmacother. 2019;111:649–656.
- Piccioni A, Saviano A, Cicchinelli S, et al. Proadrenomedullin in sepsis and septic shock: a role in the emergency department. Medicina (Kaunas). 2021 Sep 1;57(9):920.
- Malíčková K, Koucký M, Pařízek A, et al. Diagnostic and prognostic value of presepsin in preterm deliveries. J Matern Fetal Neonatal Med. 2015;28(9):1032–1037.
- Ishii M, Hoshina T, Ichikawa S, et al. The physiological variation in plasma presepsin levels during the early neonatal period. Tohoku J Exp Med. 2018 Nov;246(3):199–203.
- Liu B, Yin Q, Chen YX, et al. Role of Presepsin (sCD14-ST) and the CURB65 scoring system in predicting severity and outcome of community-acquired pneumonia in an emergency department. Respir Med. 2014;108(8):1204–1213.
- Donaldson LJ, Panesar SS, Darzi A. Patient-safety-related hospital deaths in England: thematic analysis of incidents reported to a national database, 2010–2012. PLoS Med. 2014;11(6):e1001667.
- Williams T, Tohira H, Finn J, et al. The ability of early warning scores (EWS) to detect critical illness in the prehospital setting: a systematic review. Resuscitation. 2016 May;102:35–43.
- Goulden R, Hoyle M, Monis J, et al. qSOFA, SIRS and NEWS for predicting inhospital mortality and ICU admission in emergency admissions treated as sepsis. Emerg Med J. 2018 Jun;35(6):345–349.
- Wiersinga WJ, van Zanten ARH, Kaasjager KA, et al. Sepsis: new insights, new definition. Ned Tijdschr Geneeskd. 2017;161:D1551.
- Bösch F, Schallhorn S, Miksch R, et al. The prognostic value of presepsin for sepsis in abdominal surgery: a prospective study. Shock. 2020 Jul;54(1):56–61.
- Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). Jama. 2016;315(8):801–810.
- Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related organ failure assessment) score to describe organ dysfunction/failure. On behalf of the working group on sepsis-related problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996 Jul;22(7):707–710.
- McDonald GB, Tabellini L, Storer BE, et al. Predictive value of clinical findings and plasma biomarkers after fourteen days of prednisone treatment for acute graft-versus-host disease. Biol Blood Marrow Transplant. 2017 Aug;23(8):1257–1263.
- Knaus WA, Draper EA, Wagner DP, et al. APACHE II: a severity of disease classification system. Crit Care Med. 1985;13:818–829.
- Physicians RCo. National Early Warning Score (NEWS) 2-Standardising the assessment of acute-illness severity in the NHS, Updated report of a working party December 2017. 2017 Dec 19. Available from: www.rcplondo.ac.uk:RoyalCollegeofPhysicians.
- Pullyblank A, Tavaré A, Little H, et al. West of England Patient Safety Collaborative: implementation of the National Early Warning Score in patients with suspicion of sepsis: evaluation of a system-wide quality improvement project. Br J Gen Pract. 2020;70(695):e381–8.
- Srisawat N, Kulvichit W, Tungsanga S, et al. The role of neutrophil chemotaxis activity as an immunologic biomarker to predict mortality in critically-ill patients with severe sepsis. J Crit Care. 2020 Apr;56:215–221. Epub 2020 Jan 17.
- Kremmer E, Meyer K, Grässer FA, et al. A new strategy for the development of monoclonal antibodies for the determination of human procalcitonin in serum samples. Anal Bioanal Chem. 2012;402(2):989–995.
- Volkova E, Willis JA, Wells JE, et al. Association of angiopoietin-2, C-reactive protein and markers of obesity and insulin resistance with survival outcome in colorectal cancer. Br J Cancer. 2011;104(1):51–59.
- Arai Y, Mizugishi K, Nonomura K, et al. Phagocytosis by human monocytes is required for the secretion of presepsin. J Infect Chemother. 2015;21(8):564–569.
- Masson H, Stephenson J. Investigation into the predictive capability for mortality and the trigger points of the National Early Warning Score 2 (NEWS2) in emergency department patients. Emerg Med J. 2021 Jun 9;39:685–690. emermed-2020-210190.
- Vergara P, Forero D, Bastidas A, et al. Validation of the National Early Warning Score (NEWS)-2 for adults in the emergency department in a tertiary-level clinic in Colombia: cohort study. Medicine (Baltimore). 2021 Oct 8;100(40):e27325.
- Wallgren UM, Sjölin J, Järnbert-Pettersson H, et al. Performance of NEWS2, RETTS, clinical judgment and the predict sepsis screening tools with respect to identification of sepsis among ambulance patients with suspected infection: a prospective cohort study. Scand J Trauma Resusc Emerg Med. 2021 Sep 30;29(1):144.
- Hsu C, Tsai Y, Lin C, et al. Application of a 72 h national early warning score and incorporation with sequential organ failure assessment for predicting sepsis outcomes and risk stratification in an intensive care unit: a derivation and validation cohort study. J Pers Med. 2021 Sep 13;11(9):910.
- Kang J, Gong P, Zhang X, et al. Early differential value of plasma presepsin on infection of trauma patients. Shock. 2019;52(3):362–369.
- Venugopalan D, Pillai G, Krishnan S. Diagnostic value and prognostic use of presepsin versus procalcitonin in sepsis. Cureus. 2019;11(7):e5151.
- Ikeda T, Kamohara H, Suda S, et al. Comparative evaluation of endotoxin activity level and various biomarkers for infection and outcome of ICU-admitted patients. Biomedicines. 2019 Jun 29;7(3):47.
- Wang S, Ruan W, Yu Z, et al. Validity of presepsin for the diagnosis and prognosis of sepsis in elderly patients admitted to the intensive care unit. Minerva Anestesiol. 2020 Nov;86(11):1170–1179.
- Drăgoescu AN, Pădureanu V, Stănculescu AD, et al. Presepsin as a potential prognostic marker for sepsis according to actual practice guidelines. J Pers Med. 2020 Dec 22;11(1):2.
- Abdelshafey EE, Nasa P, Elgohary AE, et al. Role of presepsin for the diagnosis of sepsis and ICU mortality: a prospective controlled study. Indian J Crit Care Med. 2021 Feb;25(2):153–157.
- Shimoyama Y, Umegaki O, Kadono N, et al. Presepsin values predict septic acute kidney injury, acute respiratory distress syndrome, disseminated intravascular coagulation, and shock. Shock. 2021 Apr 1;55(4):501–506.
- Engvig A, Wyller T, Skovlund E, et al. Association between clinical frailty, illness severity and post-discharge survival: a prospective cohort study of older medical inpatients in Norway. Eur Geriatr Med. 2021 Aug 21:1–9. DOI:10.1007/s41999-021-00555-8.
