ABSTRACT
Background
Reflex tachycardia that occurs during nitroglycerin-induced hypotensive anesthesia in functional endoscopic sinus surgery (FESS) increases both the risk of intraoperative bleeding and the duration of surgery. Our clinical trial aimed to compare the effect of oral ivabradine versus oral propranolol as a premedication before nitroglycerin-induced hypotensive anesthesia on the reduction of reflex tachycardia in FESS.
Methods
In this clinical, comparative, prospective, randomized, controlled, double-blinded study, 40 patients were divided into two equal groups (20 each); group P received oral propranolol (10 mg tablet) and group I received oral ivabradine (5 mg tablet) in the evening before the surgery and 1 hour before the induction of anesthesia.
Results
The reduction in heart rate (HR) was statistically significantly higher in group I than in group P. Conversely, the reduction in mean blood pressure (MAP) was statistically significantly higher in group P than in group I at baseline (pre-induction). However, after that, MAP reduction was statistically non-significant between both groups. Meanwhile, there was no statistically significant difference between both groups as regards duration of surgery, duration of deliberate hypotension, intraoperative NTG infusion doses, and the amount of bleeding.
Conclusion
Premedication with oral propranolol 10 mg or oral ivabradine 5 mg before FESS proved to be safe and effective in the reduction of reflex tachycardia that occurs during controlled nitroglycerin induced hypotensive anesthesia in FESS. However, ivabradine was more effective with higher safety profile than propranolol.
1. Introduction
Functional endoscopic sinus surgery (FESS) is well accepted and the most popular minimally invasive surgery for treating chronic refractory sinusitis. Its goal is to drain the paranasal sinuses and restore normal mucociliary clearance function of them [Citation1].
FESS is considered a safe operation, but minor and major complications may still occur including cerebrospinal fluid leakage, orbital or intracranial injury, meningitis, synechiae formation, and bleeding. Intraoperative bleeding is considered a significant problem that is associated with this technique. It decreases surgical field visibility, lengthening surgery and increases the possibility of occurrence of complications [Citation2].
Controlled (deliberate) hypotensive anesthesia is a method for reducing surgical bleeding, improving the visibility of the operative field, and finally reducing the overall surgery and anesthesia time by lowering the mean arterial pressure in a deliberate (but controlled) manner. Various agents have been used either alone or in combination with each other for attaining deliberate hypotension, such as nitroglycerin (NTG), a higher dose of inhaled anesthetics, sodium nitroprusside, and β blockers. The optimal agent used to induce hypotensive anesthesia must have certain features such as a rapid onset and offset without production of toxic metabolites, and easy to administer with fewer occurrence of side effects. However, this optimum agent cannot be assured [Citation3].
Nitroglycerin (NTG), a directly acting arterial and venous vasodilator, has been used to produce deliberate hypotension. It has a short onset and offset and is cheap and easy to use with easy titrability. However, its use is associated with tachycardia and venous congestion in the surgical site, which increases the risk of intraoperative bleeding, decreases the operative field visibility, and increases the time of both surgery and anesthesia [Citation4].
Propranolol is a non-selective beta-blocker that causes a reduction in heart rate, cardiac output, and cardiac contractility. It is absorbed entirely and rapidly from the gastrointestinal tract when taken orally. It reaches its maximal plasma level within 1–1.5 hours of dosing, and its elimination half-life is 2–3 hours [Citation5].
Ivabradine inhibits specific ionic current (If) channels (pacemaker current) in the sinoatrial node. It is used in patients with heart failure and ischemic heart disease. Compared to beta-blockers, ivabradine causes a reduction in heart rate without significantly affecting the hemodynamics in unwell, compromised patients. It is absorbed entirely and rapidly from the gastrointestinal tract when taken orally. It reaches its maximal plasma level within 1 hour of dosing [Citation6].
2. AIM of the work
This work aimed to compare the use of oral propranolol versus oral ivabradine as a premedication in patients undergoing FESS under general anesthesia to determine the effect and safety of both drugs in reducing reflex tachycardia that occurs during nitroglycerin induced hypotensive anesthesia.
3. Patients and methods
A clinically, prospective, randomized, controlled, and double-blinded study was conducted from January 2021 to December 2021 at Ain Shams University Hospitals. It was approved by the research ethics committee at the faculty of medicine, Ain Shams University, Cairo, Egypt (FMASU M D 235/2020) and registered with Pan African Clinical Trial Registry, identifier: PACTRPACTR202111574906850. Written informed consent was obtained from all patients.
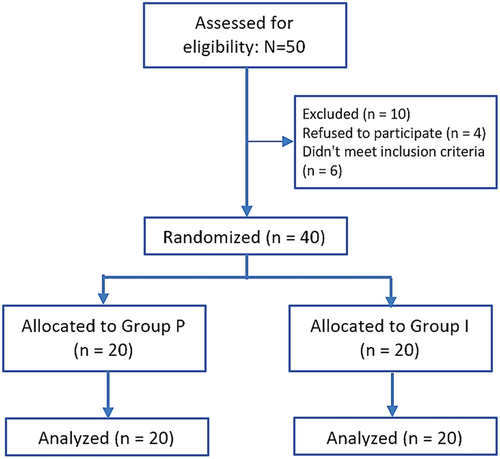
Forty patients of both sexes aged between 21 and 40 years old, American Society of Anesthesiologists (ASA) status I and II, were diagnosed with chronic sinusitis and were admitted and scheduled for FESS procedure under general anesthesia. Patients were divided into two equal groups using the closed-envelope technique (each group included 20 patients) by using a simple randomized procedure utilizing a computer program, as described in the flow diagram ():
● Group P (Propranolol): Twenty patients received one tablet (10 mg) of oral propranolol hydrochloride (InderalR) at 8:00 pm the night before surgery, and another one tablet (10 mg) with a small sip of water one hour before induction of anesthesia.
● Group I (Ivabradine): Twenty patients received one tablet (5 mg) of oral ivabradine (ProcoralanR) at 8:00 pm the night before surgery and another one tablet (5 mg) tablet with a small sip of water one hour before induction of anesthesia.
Both groups were compared regarding their demographic data, ASA, duration of surgery, hemodynamic variables (heart rate (HR) and mean arterial pressure (MAP)) at pre-induction (baseline), before nitroglycerine (NTG) infusion just after induction, every 5 minutes till termination of NTG infusion, 5 minutes after the end of deliberate hypotension, immediately after extubation, and finally 60 minutes after extubation.
Furthermore, the amount of blood loss, duration of deliberate hypotension, duration of surgery, intraoperative NTG doses used during deliberating hypotension, and occurrence of significant bradycardia or hypotension were also collected and recorded.
3.1. Exclusion criteria
Patients’ refusal.
Patients with cardiovascular diseases (atrial fibrillation, congestive heart failure, hypertension, coronary artery disease).
Patients who are already on beta-blockers, heart block, or have a heart rate of fewer than 60 beats per minute.
Patients with uncontrolled diabetes mellitus (DM).
Patients with cerebrovascular insufficiency.
Patients who have a coagulation problem.
History of severe hepatic or renal insufficiency.
Patients with a history of bronchial asthma.
Hypersensitivity or contraindication to any of the study drugs.
4. Study tools
4.1. Preoperative settings
A history, clinical examination, and investigations tailored to the patient’s condition were performed for each patient.
4.2. Monitoring
All patients were continuously monitored with standard ASA monitors: non-invasive automated blood pressure measurement (NIBP), electrocardiogram (ECG), pulse oximetry (Spao2), and capnography.
4.3. Anesthesia technique
All patients were fasting for at least 6 hours the night before surgery and pre-medicated with intravenous (IV) midazolam 0.05 mg/kg.
A peripheral venous cannula (18 G) was used to gain intravenous access.
Lactated ringer solution was given to all patients at a rate of 4–6 ml/kg/hr.
Preoxygenation for 3 minutes, then fentanyl 1–2 μg/kg IV, propofol 1–2 mg/kg IV titrated till loss of consciousness, then atracurium 0.5 mg/kg IV to induce general anesthesia.
The patient was intubated and ventilated using an orotracheal tube. End-tidal CO2 (ETCO2) was kept between 30 and 35 mmHg by adjusting the ventilator settings.
A saline-soaked oropharyngeal pack was employed.
All patients were placed in a 30° head-up position to decrease bleeding.
Anesthesia was maintained using oxygen in air, 1.5 Mac isoflurane, and atracurium top-up dosages of 0.1 mg/kg/30 min.
Controlled hypotensive anesthesia was induced by nitroglycerin infusion in a concentration of (1 mg/ml) with a dose range of 0.5–2 μg/kg/min until completion of the surgery to achieve a MAP approximately at 60 mmHg.
At the end of the procedure, Isoflurane was stopped, the oropharyngeal pack was withdrawn, and the oropharynx was suctioned. Neostigmine 0.05 mg/kg IV and atropine 0.02 mg/kg IV were used to reverse the remaining atracurium. The trachea was extubated once the patient’s hemodynamic stability was confirmed using standard extubation criteria such as spontaneous eye-opening and obeying commands.
Patients were moved to the PACU and continuously monitored with NIBP, Spao2, and ECG monitors until discharge. Oxygen supplementation was provided via a face mask flow at6L/min. Standard discharge criteria from PACU were applied, and the patient was discharged when he was fully conscious and alert and able to protect his airway, had stable vital signs, normal oxygen saturation, and respiratory rate.
The surgeon, who was blinded to the given medication, rated surgical bleeding and the operative field visibility using a 6-point bleeding scale that was adapted by Boezaart [Citation7] ():
Table 1. Boezaart surgical field grading scale [Citation7].
Furthermore, the volume of aspirated blood and fluids from the operative field was measured by milliliters (mls) using a graded suction container used to further assess bleeding.
5. Measured outcomes
● Primary outcome: Comparison between oral propranolol and oral ivabradine regarding their effect as premedication on the reduction of reflex tachycardia caused by nitroglycerin during controlled hypotensive anesthesia in FESS.
● Secondary outcomes: Comparison between two groups regarding mean arterial pressure, duration of surgery, duration of deliberate hypotension, intraoperative NTG dose, blood loss, and the occurrence of significant bradycardia or hypotension as a safety profile.
6. Statistical analysis
The sample size was calculated using the PASS 11 program and according to a previous study done by Ibrahim and Atallah [Citation8]. A sample size of 20 patients per group (total 40 patients) can detect the difference between the two groups with power >99% setting the alpha error at 0.05.
6.1. Sample size
This study enlisted the participation of 40 patients.
They were divided into two equal groups (each with 20 patients):
Group P: (Propranolol group, n = 20)
Group I: (Ivabradine group, n = 20)
The obtained data were edited, tabulated, coded using the PASS 11 program, and uploaded to a computer. For quantitative parametric data, mean and standard deviation (±SD) was used. For quantitative non-parametric data, median and interquartile range (QR) was used. Finally, for qualitative data; numbers and percentages were used. The Student's t-test and the Chi-square (X2) test were used in this study. The appropriate analysis was carried out based on the type of data gathered.
The following P-value was considered significant:
Non-significant (NS): if a P-value is greater than 0.05.
Significant (S): if a P-value is less than 0.05.
Highly significant (HS): with a P-value of less than 0.01.
7. Results
7.1. Demographic data
In terms of age, sex, and ASA status, there was no statistically significant difference between the two groups ().
Table 2. Comparison between both groups regarding demographic data and duration of surgery.
7.2. Duration of surgery
Although the mean duration of surgery was a little longer in the propranolol group (89.65 ± 8.86 min) compared with the ivabradine group (84.65 ± 13.95 min), yet this difference was statistically non-significant ().
7.3. Heart rate
The reduction in heart rate (HR) was statistically significantly higher (P-value < 0.001) in group I than in group P at pre-induction (baseline), before nitroglycerin (NTG) infusion just after induction, every 5 minutes till termination of NTG, with significant statistic reduction (P-value < 0.025) 5 minutes after the end of anesthesia to be again highly significant statistic reduction (P-value < 0.001) immediately after extubation and finally 60 minutes after extubation () ().
Figure 2. Bar chart comparing between two groups as regard HR, mean ± SD were used for data expression, t = Student’s t-test.
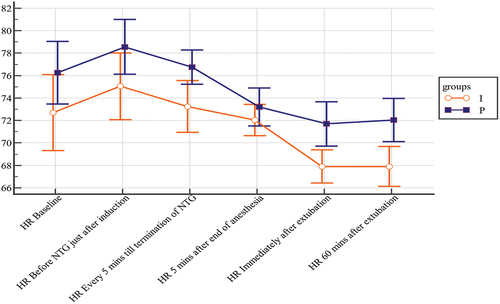
Table 3. Comparison between both groups regarding heart rate (HR).
Intraoperative episodes of significant bradycardia (HR≤ 50 beats/min) were more common in group I than in group P, with a statistically significant difference ().
Table 4. Comparison between both groups regarding bradycardia and significant persistent hypotension episodes.
It was recorded in eight patients (one patient in group P and seven patients in group I). It was managed by atropine 0.6 mg IV with decreasing the dose of isoflurane to 1 Mac in this patient in group P, and only in one patient (of the seven patients) in group I when it was associated with a decrease in MAP of less than 60 mmHg.
7.4. Mean arterial pressure
The reduction in MAP was statistically significantly higher in group P than in group I at pre-induction (baseline) (P-value < 0.001). However, after that, till 60 minutes after extubation, MAP reduction was statistically non-significant (P-value > 0.05) between both groups ( and ).
Figure 3. Bar chart comparing between two groups as regard MAP, mean ± SD were used for data expression, t = Student’s t-test.
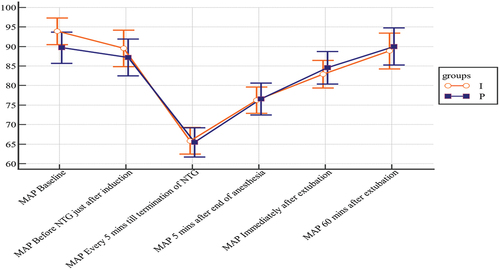
Table 5. Comparison between both groups regarding mean arterial blood pressure (MAP).
Intraoperative episodes of persistent, significant hypotension (MAP ≤ 60 mmHg for 5 minutes or more) occurred more frequently in group P than in group I, yet without statistically significant difference ().
It was recorded in five patients (four patients in group P and one patient in group I). It was managed by decreasing the infusion rate of nitroglycerin in this patient in group I and by the stoppage of NTG, giving fluid boluses of ringer acetate, and decreasing the dose of isoflurane to 1 Mac in three patients in group P. Only one patient in group P did not respond to the previous measures and was managed by giving 10 mg ephedrine IV.
7.5. Duration of deliberate hypotension
The mean duration of deliberate hypotension (presented in minutes) was longer in group P (73.5 ± 9.47 Min) compared with group I (69.75 ± 14.46 Min). However, this difference was statistically non-significant ().
Table 6. Comparison between both groups regarding duration of deliberate hypotension, intraoperative NTG dose used during deliberate hypotension, and intraoperative bleeding amount.
7.6. Intraoperative NTG dose (μg/kg/min) used during deliberating hypotension
Both groups were comparable without significant statistical difference between them ().
7.7. Intraoperative bleeding amount in milliliters (MLs)
There was less bleeding in group I than in group P. This difference was statistically non-significant ().
8. Discussion
The mucosa of the nose and paranasal sinuses is highly vascular and easily bleeds during FESS, which could interfere with the operative field visibility through the endoscopic procedures. This bleeding might result in unintentional tissue injury, resulting in scarring, adhesions, and even more severe consequences such as direct brain and orbital injury and a more extended surgery and anesthesia time [Citation9].
Both venous and arterial pressures and localized capillary circulation influence bleeding from the surgical field. Decreasing the operative field bleeding improves surgical outcomes and decreases the incidence of complications [Citation10].
In our study, we compared the use of oral ivabradine versus oral propranolol as a premedication in patients undergoing FESS under general anesthesia to assess the effect and safety of both drugs in reducing the reflex tachycardia that occurs during nitroglycerin-induced hypotensive anesthesia. Furthermore, we assessed the effect of both drugs on the mean arterial pressure, duration of surgery, duration of deliberate hypotension, intraoperative NTG dose used, blood loss, and finally the occurrence of significant bradycardia and/or hypotension as a drug safety profile.
Our study’s results regarding the heart rate changes were similar to those of Apipan and Rummasak [Citation11]. They assessed the efficacy and safety of oral propranolol 10 mg as a premedication before hypotensive anesthesia induced with sodium nitroprusside (a potent vasodilator) to reduce reflex tachycardia that can occur during deliberate hypotensive anesthesia in orthognathic surgery. They discovered that using an oral propranolol 10 mg tablet as a premedication before sodium nitroprusside-induced hypotensive anesthesia was effective and safe in preventing reflex tachycardia.
In addition, our findings on reducing reflex tachycardia with ivabradine in group I were similar to those of Raghuram et al. [Citation12]. They compared the efficacy of oral ivabradine 5 mg given 1 hour before intubation versus a placebo to attenuate hemodynamic responses after intubation. They concluded that ivabradine is an excellent drug for preventing both the aberrant increase in heart rate and, to a lesser extent, blood pressure that occurs during laryngoscopy and endotracheal intubation. They advocated for its routine use during laryngoscopy and endotracheal intubation in all patients at risk for hypertension and tachycardia. Contrary to this study, we used propranolol in group P instead of a placebo for patient safety regarding the reduction of bleeding. Indeed, propranolol is a well-known, long-used, and safe drug to compare with.
Interestingly, although our study focused on a different type of surgery (FESS), our findings were similar to those of Ibrahim and Atallah [Citation8]. They compared the efficacy of oral propranolol versus oral ivabradine premedication in microlaryngoscopic surgeries to reduce the stress response. They found that oral propranolol 10 mg and oral ivabradine 5 mg given in the evening before the operation and 1 hour before the induction of anesthesia provide good hemodynamic stability. Ivabradine, on the other hand, was more effective, with the added benefit of avoiding some beta-blocker side effects and the ability to be used in patients who were intolerant to them. In contrast to our study, which reported a large statistically significant difference in pre-induction (baseline) MAP between both groups, they discovered no statistically significant baseline MAP difference between their two research groups.
As regard safety profile of our studied drugs, only one patient in group P and one patient (from a total of seven patients) in group I developed bradycardia (HR ≤ 50 beats/min) and MAP less than 60 mmHg and were properly managed. This large safety margin was supported by the fact that ivabradine causes heart rate reduction without causing hemodynamic instability [Citation6].
Additionally, in group P, four patients had episodes of persistent, significant hypotension (MAP ≤ 60 mmHg for ≥5 minutes), which was properly managed. These episodes in group P were more frequent with a longer mean duration of hypotension than in group I, which may add more safety advantages to ivabradine. However, this was not statistically significant.
In our study, the average amount of blood loss in the ivabradine group was slightly lower than in the propranolol group. However, this difference was not statistically significant with the possible need for further clinical trials with larger numbers of patients.
Ivabradine and propranolol are well tolerated and absorbed entirely and quickly from the gastrointestinal tract when taken orally. The oral forms take 20–30 min to start working [Citation8].
As a result, we preferred to use the oral forms of ivabradine and propranolol to benefit from their potential effects as pre-anesthetic medications to improve patient convenience and compliance. Furthermore, the doses provided to the patients were the lowest effective starting doses recommended by the manufacturing pharmaceutical companies and pharmacological references to ensure patient safety.
Finally, there was no statistically significant difference between the two groups regarding the hypotensive periods, the operative times, and the incidence of episodes of persistent, significant hypotension between both groups. This makes using both drugs as a premedication before hypotensive anesthesia effective, practical, and safe in FESS surgeries and allows ivabradine to be used as an alternative in patients with contraindication to propranolol or intolerant to it.
9. Study limitation
One of the major limitations of this work is that ENT surgeon was not the same in all operations with different experience and procedural skills. Furthermore, the complexity of the surgeries was different.
Additionally, the sample size was relatively small, so further future clinical trials on different population ethnicity and larger sample sizes could be conducted. Finally, we did not use different dose regimens of both drugs, propranolol, and ivabradine, which may differ from one patient to another.
10. Conclusion
Our study concluded that premedication with 10 mg of oral propranolol or 5 mg of oral ivabradine in the evening before surgery and 1 hour before anesthesia induction proved to be both safe and effective in reducing reflex tachycardia that occurs during controlled nitroglycerin induced hypotensive anesthesia in FESS. However, ivabradine was more effective with a higher safety profile, especially in patients with contraindication to propranolol or intolerant to it.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Shaban AAE, Mohammed HF, Zaher AAA. Role of gabapentin in controlled hypotension for nasal surgeries: a randomized controlled study. Sci J AlAlAzhar Med Fac Girls. 2019;3:172.
- El-Shmaa NS, Ezz HA. Younes A. JClinAnesth. 2017;39:154–158.
- Cincikas D, Ivaškevicius J, Martinkenas JL, et al. A role of anesthesiologist in reducing surgical bleeding in endoscopic sinus surgery. Medicina (Kaunas). 2010;46:730–734.
- Srivastava U, Dupargude AB, Kumar D, et al. Controlled hypotension for functional endoscopic sinus surgery; comparison of esmolol and nitroglycerin. Ind J Otolaryngol Head Neck Surg. 2013;65. S440–S444.
- Morgan GE, Mikhail MS, Mj M. Clinical Anesthesiology. 6th ed. New York: McGraw-Hill; 2018.
- Koruth JS, Lala A, Pinney S, et al. The clinical use of ivabradine. A review article. J Am Coll Cardiol. 2017; 70(14):1777–1784.
- Boezaart AP, van der Merwe J, Coetzee A. Comparison of sodium nitroprusside- and esmolol-induced controlled hypotension for functional endoscopic sinus surgery. Can J Anaesth. 1995;42(5 Pt 1):373–376.
- Ibrahim AN, RY A. Ivabradine versus propranolol given orally in microlaryngoscopic surgeries in attenuating stress response; A comparative prospective double-blind randomized study. Egyptian J Anesth. 2016;32:503–511.
- MA T, Pj W. Ten pearls for safe endoscopic sinussurgery. Otolaryngol Clin North Am. 2010;43:933–944.
- AR B, AB B. Anesthesia for endoscopic sinus surgery. Acta Anaesthesiol Scand. 2010;54:795–803.
- Apipan B, Rummasak D. Efficacy and safety of oral propranolol premedication to reduce reflex tachycardia during hypotensive anesthesia with sodium nitroprusside in orthognathic surgery: a double-blind, randomized clinical trial. J Oral Maxillofac Surg. 2010;68(1):120–124.
- Raghuram CG, Deepraj S. Attenuation of haemodynamic response to laryngoscopy and endotracheal intubation using intra-oral ivabradine: a clinical study. J Evol Med Dental Sci. 2014;3(39):9944–9955.