ABSTRACT
Background
Airway assessment before anaesthesia in the elderly is crucial. The delay in endotracheal intubation in this age group can lead to fatal consequences. This study aimed to evaluate the validity of sternomental displacement (SMDD) as a predictor of difficult airway in the elderly and to compare it with the thyromental height test (TMHT).
Methods
This study included 150 patients aged > 65 years old, ASA i–iii, who were scheduled for elective surgeries under general anaesthesia with endotracheal intubation using conventional laryngoscopy. Cormack–lehane grades iii and iv were assigned as difficult laryngoscopy (DL). Difficult intubation (DI) was defined as insertion of endotracheal tube required more than two attempts or 10 minutes. The primary outcome was the AUROC curve for the SMDD as a predictor of difficult laryngoscopy.
Results
14% of our patients showed DL, while 4.7% had DI. SMDD was a good predictor for DL with 0.692 AUC (95% ci: 0.611 − 0.765) at a cut-off value of ≤35 mm, with 71.43% sensitivity, 59.69% specificity, 22.4% PPV and 92.8% NPV. TMHT showed good prediction for DL with 0.794 AUC (95% ci: 0.721–0.856) at a cut-off value of ≤ 49.5 mm. For predicting DI, SMDD showed AUROC (95% ci): 0.814 (0.743–0.873) at a cut-off value ≤35 mm and TMHT had AUROC (95% ci): 0.719 (0.640–0.790) at a cut-off value ≤ 49.5 mm.
Conclusion
SMDD and TMHT are good objective predictors for DL and di in elderly surgical patients.
1. Introduction
Even though serious airway management problems are becoming less prevalent, they remain the most life-threatening condition in anaesthetic practice and even medicine [Citation1]. Failure to maintain a patent airway during general anaesthetic induction relates to many consequences, from sore throat and traumatic airway injuries to brain damage and even death [Citation2]. In most circumstances, direct laryngoscopy is commonly utilised to intubate the patient. The difficult airway can be indicated by difficulty with laryngoscopy and/or intubation [Citation3].
The senior population is growing. The airway screening for difficulties before anaesthesia is critical in this age group. The delays in endotracheal intubation in the elderly might have deadly effects due to reduced organ reserve and comorbidities. Previous research has shown that aged people are more likely to have difficult airways due to age-related anatomic changes in the head and neck. These changes include, but are not limited to, tooth loss, narrow dental arch, reduced oral soft tissue flexibility, TMJ dysfunction, degenerative change of intervertebral disc ligament and tendons causing intervertebral disc compression, cervical lordosis and spondylosis, limited head and upper neck extension, and fixed cervical spine flexion deformity [Citation4,Citation5].
The thyromental height test (TMHT) measures the distance between the anterior margins of the mentum and thyroid cartilage while the patient lies supine with the mouth closed. This test was initially reported in 2013 as a substitute for three significant anthropometric measures: mandibular protrusion, submandibular space dimensions, and anterior larynx location. The test is not restricted by head extension and is not dependent on cervical spine mobility, dentition, or patient compliance [Citation6].
Another objective airway assessment is sternomental displacement (SMDD), which calculates the difference in sternomental distance (SMD) with the head in a neutral posture (SMD-neutral) and stretched on the neck (SMD-extension). The SMDD serves as a proxy for neck mobility [Citation7]. TMHT and SMDD were excellent objective predictors of difficult laryngoscopy (DL) in adult surgical patients [Citation6,Citation7].
The TMHT has been found to possess a strong predictive capacity for difficult airways in elderly patients [Citation8], but to our knowledge, the SMDD has not been investigated in this age group. So, this study aimed to compare the validity of SMDD as a predictor of difficult airways in the elderly to that of TMHT. Our primary endpoint is the AUROC curve (area under the receiver operating characteristic curve) of the SMDD as a predictor of DL in elderly surgical patients. The secondary endpoint is to compare the accuracy of SMDD with that of the TMHT for predicting difficult airway.
2. Methods
After receiving permission from the research ethics committee of the faculty of medicine at cairo university (email: [email protected] id: ms-623-2021), this prospective cohort study was conducted in the operating theatres. The study was registered on clinicaltrials.gov with identifier id: nct05414214. Informed consent was obtained from all patients. In addition, the STARD (standards for reporting diagnostic accuracy studies) guidelines were followed.
One hundred and fifty elderly patients (> 65 years) of both sexes with american society of anaesthesiologists (ASA) physical status i, ii, and iii who were scheduled for elective surgeries under general anaesthesia with endotracheal (ETT) intubation accomplished using conventional laryngoscopes were included. Patients undergoing emergency procedures, patients requiring elective awake fibreoptic, patients with neuromuscular disorders or craniofacial abnormalities, patients with cervical spine surgeries, neck scars, obviously limited neck extension, and morbid obesity (BMI >40 kg/m2) were excluded.
In the anaesthesia preparatory room, the airway assessment was performed preoperatively by two research team members who were not involved in the process of ETTintubation or the assessment of the laryngeal view. The following tests were accomplished:
When the patient was sat with the head in a neutral posture, the SMD was recorded as the SMD-neutral, which is the distance between the upper edge of the manubrium-sterni and the mentum. The SMD-extension was evaluated when the head was extended on the neck. The difference between SMD-extension and SMD-neutral was used to compute the SMDD [Citation7]. ()
Figure 1. Photo I is the sternomental displacement measurement: A at extension and B at neutral position. Photo II is the thyromental height test measurement using a digital depth gauge. Our team captured the photo after the patient’s consent.
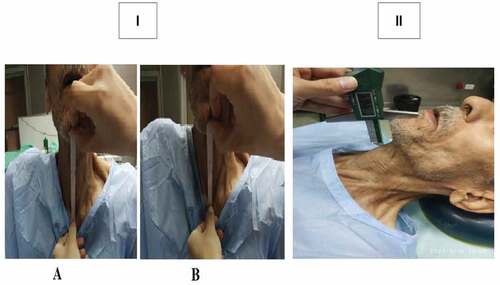
The patient was evaluated while lying supine and undergoing TMHT. A cushion was placed under the head to maintain a neutral position for the head and neck. The TMH was calculated as the vertical distance between the anterior border of the thyroid cartilage, which is placed directly on the thyroid notch, and the anterior border of the mentum using a digital depth gauge (standard type, insize, india) [Citation6]. ()
The patient was seated in a neutral position, with the mouth open wide, the tongue protruding, and no phonation throughout the modified mallampati test (MMT). The oropharyngeal features that were seen led to the right categorization being recorded [Citation9].
An intravenous line was in place in the operating room, and ringer acetate was commenced. Electrocardiograms, pulse oximeters, and non-invasive blood pressure monitors were all linked to the patients. For three minutes, patients received pre-oxygenation with 100% oxygen. Then, intravenous fentanyl 2 μg/kg, propofol 1–1.5 mg/kg, and succinylcholine 1 mg/kg lean body weight were used to induce anaesthesia. Mask breathing was kept up until a peripheral nerve stimulator showed that the muscles had completely relaxed.
The optimal laryngeal view was identified using the cormack-lehane (cl) [Citation10] grading system from i–iv utilising a macintosh laryngoscope by an anaesthesiologist with at least ten years of experience and who was blind to the outcomes of the preoperative examinations. Grade i: complete view of the glottis; grade ii: partially exposed glottis with no visible anterior commissure; grade iii: only the epiglottis visible; grade iv: no epiglottis visible. CL grades iii and iv were considered DL. External neck manipulation was performed when necessary to get the best laryngoscopic view. ETTintubation was accomplished.
Records were made of the quantity and length of intubation attempts. If it requires more than two trials or more than ten minutes to properly insert the ETTusing a standard laryngoscope, it is considered difficult tracheal intubation (DI). Failed ETTwas indicated after more than two unsuccessful intubation attempts, after 10 minutes passed, and by using an alternative airway technique to secure the airway. No other dose of succinylcholine was administered after recovery.
The primary outcome was the accuracy of the SMDD as a predictor of DL (AUROC curve). The secondary outcomes were the AUROC curve for the SMDD as a predictor of di and the AUROC curve for the TMHT as a predictor of DL and DI.
3. Sample size calculation
Using the Med-Calc programme, the sample size was computed to get an AUROC curve for SMDD of 0.70 with such a null hypothesis AUROC of 0.5.for a research power of 90% and an alpha error of 0.05, we determined a minimum of 134 patients (including at least 16 DL instances) based on the assumption that the rate of DL in elderly surgical patients is 12% [Citation8].150 patients were added to account for potential dropouts.
4. Statistical analysis
For data collection and analysis, IBM SPSS software version edition 23 was employed (Chicago, IL, USA). The Shapiro-Wilk test was used to determine if the data distribution was normal. While qualitative categorical data was reported as a number and percentage, continuous quantitative data was represented as means and standard deviations (SD) or median and range, as applicable. The student’s t-test was used to evaluate normally distributed data, and the Mann-Whitney test or the Kruskal-Wallis test, if applicable, was used to analyse non-normally distributed data. Statistical significance was defined as a p-value of less than 0.05
The validity of the SMDD, TMHT, and combined scores for DL and di were evaluated using the AUROC [Citation11], which was built using the Med-Calc programme. Both measurements indicate difficult laryngoscopy/intubation according to the combined scores, which are (SMDD and TMHT), or (SMDD or TMHT), which implies that any of the two measurements indicates difficult laryngoscopy/intubation. Easy versus difficult laryngoscopy and easy versus difficult intubation were defined as binary variables. The Youden index was employed to determine the optimal cut-off point for each of the evaluated variables using the AUROC curve. Additionally, the PPV and NPV, as well as the specificity, sensitivity, and accuracy were determined. Statistical significance was defined as a p-value of less than 0.05.
5. Results
A total of 150 patients (83 males and 67 females) who matched our criteria for inclusion were recruited for this observational cohort study and completed it. Their mean age was 67.96 ± 4.12 years, with an ASA classification of ii/iii of 121/29. The DL cases were 21 of 150 (14%), while the di cases were 7 of 150 (4.7%).
The number of patients was separated into two groups based on the CL grades: easy laryngoscopy (n = 129) and DL (n = 21). The patients were subsequently split into two groups: easy intubation (n = 143) and di (n = 7), based on the circumstances that made intubation difficult. Then, each pair of groups’ demographic data and test scores were compared. In comparison to the easy laryngoscopy and easy intubation groups, SMDD and TMHT were considerably lower in the difficult laryngoscopy and difficult intubation groups, respectively. ()
Table 1. The demographic data and the studied tests; TMHT, SMDD, and MMT among the difficult and easy laryngoscopy and intubation groups.
To evaluate their propensity to predict instances with DL and DI, two roc curves were generated using the TMHT, SMDD, TMHT or SMDD, and combined TMHT & SMDD ().
Figure 2. Roc curves of SMDD, TMHT, SMDD TMHT and SMDD or TMHT for predicting difficult laryngoscopy. (SMDD and TMHT) refers to that both measurements indicated difficult laryngoscopy. (SMDD or TMHT) refers to that either of the two measurements indicated difficult laryngoscopy. TMHT: thyromental height test, SMDD: sternomental displacement distance, roc: receiver operating characteristic curve.
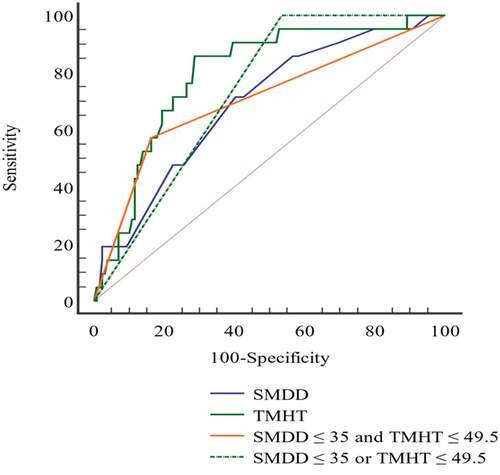
Figure 3. Roc curves of SMDD, TMHT, SMDD TMHT and SMDD or TMHT for predicting difficult intubation. (SMDD and TMHT) refer to that both measurements indicated difficult intubation. (SMDD or TMHT) refers that either of the two measurements indicated difficult intubation. TMHT: thyromental height test, SMDD: sternomental displacement distance, roc: receiver operating characteristic curve.
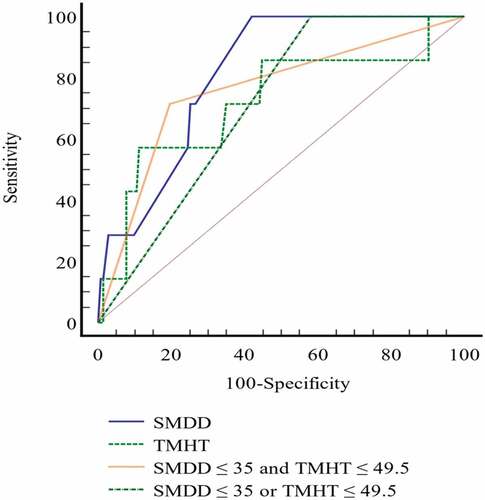
In , for DL and DI, respectively, are displayed the AUROC curve, sensitivity, specificity, PPV, NPV, and the cut-off value of the investigated parameters. TMHT and SMDD provided good predictive ability for both DL and DI, with the privilege of TMHT for predicting DL and SMDD for predicting DI. The combined TMHT and SMDT scores did not increase the predictive ability for DL or DI. However, the combined scores increased the test specificity.
Table 2. validity of SMDD, TMTH, TMHT or SMDD, and combined TMHT and SMDD for predicting difficult laryngoscopy (DL).
Table 3. Validity of SMDD, TMTH, TMHT or SMDD, and combined TMHT and SMDD for predicting difficult intubation (DI).
6. Discussion
In our study, 14% of our patients presented DL, while 4.7% showed DI. The main finding of this study is that both TMHT and SMDD provided good predictive ability for both DL and di at cutoff values ≤ 35 and ≤ 49.5 mm, respectively, with the privilege of TMHT for predicting DL and SMDD for predicting DI. The combined TMHT and SMDD scores did not increase the predictive ability for either DL or di but increased the test specificity.
In the geriatric population, many structural abnormalities in the upper airway have been documented, such as tooth decay, an edentulous mandible, considerable decreases in neck range of motion, the existence of redundant tissue in the pharynx, and restricted mobility of the epiglottis. These modifications make di since it is difficult to see the vocal cords and/or position the endotracheal tube [Citation12,Citation13]. Furthermore, some age-related illnesses, such as rheumatoid arthritis, myelopathy, and the development of thyroid masses, may decrease neck mobility and exacerbate joint stiffness [Citation5].
Airway assessment in the elderly is essential because it enables the anaesthetist to be equipped for unforeseen circumstances by using the appropriate tools and personnel and selecting a senior anaesthetist, reducing the time and number of intubations attempts and, as a result, the risk of hemodynamic and respiratory complications [Citation14].
TMHT is an objective, convenient, easily applicable measurement representing the distance between the anterior surfaces of the mentum and thyroid cartilage. TMHT was first provided by Etezadi F et al. [Citation6], who demonstrated that TMHT ≤ 50 mm can be a single anatomical measure to predict the risk of DL with a sensitivity of 82.6%, specificity of 99.35%, PPV of 90.45%, and NPV of 98.6%. The more caudal and anterior larynx is associated with a lower thyromental height (TMH), making laryngoscopy more challenging. The TMHT is not dependent on active head extension, making it more convenient. To compensate, the anesthesiologist can apply backwards, upward, and rightward pressure to enhance the laryngoscopic vision and raise the TMH [Citation6].
The predictive ability of TMHT for di was demonstrated by rao kvn et al. [Citation13] on 316 patients, who revealed 84.62% sensitivity and 98.97% specificity, 88% PPV and 98.63% NPV with a cut-off value of <50 mm. In an Indian study [Citation15] conducted on 345 patients aged 35 to 80 years with coronary artery disease undergoing cabg surgery, the TMHT showed 97% specificity, 75% sensitivity, 73% PPV, and 97% NPV with a cut-off of <52.17 mm. The difference in cut-off value compared to our study could be related to the ethnic difference in the population, apart from including a wide range of ages in the Indian study.
On the other hand, Selvi o. Et al. [Citation16] showed a high sensitivity (91.89%) and NPV (98.63%) with decreased specificity and PPV values (52.2% and 14.7%, respectively) at the 50 mm cutoff point, and when TMHT was evaluated at the 43.5 mm cutoff point, the sensitivity and specificity decreased (64.86% and 78.02%, respectively). The use of different equipment by a technician may have caused a change in the results since the accuracy of the airway prediction tests could differ depending on the measurement techniques [Citation17].
A study conducted in our institution [Citation8] included 120 patients aged ≥ 65 years; the TMHT showed AUROC 0.85 (95% ci: 78–0.91), 73.3% sensitivity, 81.9% specificity, 36.7% PPV and 95.6 NPV% at a cutoff point ≤ 57 mm for predicting DL. For DI, TMHT showed the highest accuracy with an AUROC of 0.9 (95% ci: 0.83–0.95) at a cutoff value of 59 mm. This difference in our study’s cutoff values may be attribuTable to the different methodologies. As the experienced anesthesiologist who carried out the initial intubation attempts in our study had at least ten years of experience, this explains why there were no unsuccessful intubations and the lower incidence of di in our study (4.7%) compared to theirs (20%). We also presume that our results are more precise since, unlike the previous study, we employed a digital depth gauge to measure the TMHT in millimeters rather than two perpendicular rulers.
With just a modest contribution from the sub-axial cervical segments, the Occipito-Atlanto-axial joint movement that causes the cervical spine extension during the sniffing position for intubation increases the visibility of the glottic view. As demonstrated in cases of rheumatoid arthritis and ankylosing spondylitis, however, the limitation of this movement makes it difficult to intubate a patient who has restricted neck extension. With the patient in a neck-extended position, the classic SMD is modified by the unique airway measure designated as the SMDD. The difference between the SMDD when the head is in a neutral posture and when it is extended along the neck is what is evaluated by SMDD. The ideal posture for laryngoscopy and intubation is indicated by the SMDD, which measures cervical spine mobilisation [Citation18].
The researchers [Citation7] revealed that the SMDD is an objective tool for identifying individuals at risk of DL at a cut-off value of 5.25 cm by analysing the SMDD in 610 surgical Indian patients. The discrepancy in cut-off value between their study and ours may be attributed to the anthropometric variations in distinct ethnic population groups, as they found a positive correlation between patient height and SMDD.
Two hundred twenty-one surgical patients were included in the study by Kopanaki e. et al. [Citation19]. The SMD ratio, which compares SMD in extension to SMD in neutral neck postures, was determined by the authors. The authors identified a link between a lower SMD ratio and DL, noting that there was a negative association between the SMD ratio and the CL grade. The cut-off point of 1.7 (AUROC of 0.815; 95% ci: 0.743–0.887) had the highest sensitivity and specificity (63% and 86%, respectively).
To prevent the broad range of cut-off values for predicting difficult airways using SMD in previous research as 12.5 cm, 13.5 cm, and 15 cm owing to the anthropometric disparities among the population, the use of the SMDD and SMD ratio is often more accurate than using absolute values of the SMD [Citation20-22]. The performance of SMDD as a predictor of DL and di in a geriatric population is being evaluated for the first time in our study.
Theoretically, combining tests for airway assessment can be more informative than when a single airway test is used. A meta-analysis by Shiga t. et al. [Citation23] found poor to moderate discriminative power when performing a single test for airway assessment. Also, Prakash s et al. [Citation7] reported that combined tests or risk factors add incremental diagnostic value compared to the value of each test alone. The authors denoted an AUROC to predict DL from the multivariate regression model was 0.82, including multiple risk factors such as age, male gender, SMD, SMDD, inter‑incisor distance, range of neck movement <80°, short neck, and history of snoring. The combined TMHT and SMDT scores did not improve predictive ability for either DL or di in our study; however, they may provide more solid results about difficult airways than a single measurement.
Our study had certain limitations since we only looked at individuals who were scheduled for elective surgery and we didn’t take body height or gender into account. The fact that our study only investigated Egyptians is another drawback. Future multicentric research is recommended, with multi-ethnic groups included.
7. Conclusion
Our study demonstrated that TMHT and SMDD are simple, easy to perform, and objective measurements that provided a good predictive ability for DL and di at cutoff values ≤ 35 and ≤ 49.5 mm, respectively. The combined TMHT and SMDD scores did not increase the predictive ability for either DL or di but increased the test specificity.
Availability of data and material
Data are available from the authors upon reasonable request after cairo university’s permission.
Consent for publication
The authors accept the responsibility for releasing this material. This transfer of publication rights covers the non-exclusive right to reproduce and distribute the article, including reprints, translations, photographic reproductions, microform, electronic form (offline, online) or any other reproductions of similar nature.
Ethics approval and consent to participate
Approval was obtained before patatints inclusion from the research ethics committee of faculty of medicine, cairo university (email: [email protected]; id: ms-623-2021). Written informed consents were obtained from all participants before inclusion.
Clinical trial registration id
The study was registered prospectively on clinicaltrials.gov (id: nct05414214).
Clinical trial registration
The study was registered prospectively on clinicaltrials.gov (id: nct05414214).
Disclosure statement
No potential conflict of interest was reported by the author(s).
Additional information
Funding
References
- Cook Tm, Scott S, Mihai R. Litigation following airway and respiratory-related anaesthetic morbidity and mortality: an analysis of claims against the nhs in england 1995–2007. Anaesthesia. 2010;65(6):556–563.
- Cook Tm, Woodall N, Frerk C. Major complications of airway management in the uk: results of the 4th National audit project of the royal college of anaesthetists and the difficult airway society. Part 1 Anaesthesia. Br J Anaesth. 2011;106(5):617–631.
- Practice guidelines for management of the difficult airway an updated report by the american society of anesthesiologists Anesthesiology 2013; 118: 251–270.
- Lee SY, Shih Sc, Leu Ys, et al. Implications of age-related changes in anatomy for geriatric-focused difficult airways. Int J Gerontol. 2017);;11(3):130–133.
- Johnson kn, botros db, groban l, et al. Anatomic and physiopathologic changes affecting the airway of the elderly patient: implications for geriatric-focused airway management. Clin Interv Aging. 2015 dec 4;10: 1925–1934.
- Etezadi F, Ahangari A, Shokri H, et al. Thyromental height: a new clinical test for prediction of difficult laryngoscopy. Anesth Analg. 2013 Dec;117(6):1347–1351.
- Prakash S, Mullick P, Bhandari S, et al. Sternomental distance and sternomental displacement as predictors of difficult laryngoscopy and intubation in adult patients. Saudi J Anaesth. 2017 Jul-Sep;11(3):273–278.
- Mostafa M, Saeed M, HASAnin A, et al. Accuracy of thyromental height test for predicting difficult intubation in elderly. J Anesth. 2020 Apr;34(2):217–223.
- Mallampati SR, Gatt SP, Gugino LD, et al. A clinical sign to predict difficult tracheal intubation: a prospective study. Can Anaesth Soc J. 1985;32(4):429–434. PMID: 4027773. doi:10.1007/BF03011357
- Cormack RS, Lehane J. Difficult tracheal intubation in obstetrics. Anaesthesia. 1984;39(11):1105–1111.
- Hajian-Tilaki K. Receiver operating characteristic (roc) curve analysis for medical diagnostic test evaluation. Caspian J Intern Med. 2013;4(2):627–635. Pmid: 24009950; pmcid: pmc3755824.
- Penna V, Stark G, Eisenhardt SU, et al. The aging lip: a comparative histological analysis of age-related changes in the upper lip complex. Plast Reconstr Surg. 2009 Aug;124(2):624–628.
- Sawatsubashi M, Umezaki T, Kusano K, et al. Age-related changes in the hyoepiglottic ligament: functional implications based on histopathologic study. Am J Otolaryngol. 2010Nov-Dec;31(6):448–452. epub 2009 oct 9.
- Rao KVN, Dhatchinamoorthi D, Nandhakumar A, et al. Validity of thyromental height test as a predictor of difficult laryngoscopy: a prospective evaluation comparing modified mallampati score, interincisor gap, thyromental distance, neck circumference, and neck extension. Indian J Anaesth. 2018 Aug;62(8):603–608.
- Jain N, Das S, Kanchi M. Thyromental height test for prediction of difficult laryngoscopy in patients undergoing coronary artery bypass graft surgical procedure. Ann Card Anaesth. 2017 Apr-Jun;20(2):207–211.
- Selvi O, Kahraman T, Senturk O, et al. Evaluation of the reliability of preoperative descriptive airway assessment tests in prediction of the cormack-lehane score: a prospective randomised clinical study. J Clin Anesth. 2017Feb;36:21–26.
- Karkouti K, Rose DK, Ferris LE, et al. Inter-observer reliability of ten tests used for predicting difficult tracheal intubation. Can J Anaesth. 1996 Jun;43(6):554–559.
- Takenaka I, Aoyama K, Iwagaki T, et al. The sniffing position provides greater Occipito-Atlanto-axial angulation than simple head extension: a radiological study. Can J Anaesth. 2007 Feb;54(2):129–133.
- Kopanaki E, Piagkou M, Demesticha T, et al. Sternomental distance ratio as a predictor of difficult laryngoscopy: a prospective, double-blind pilot study. Anesth Essays Res. 2020Jan-Mar;14(1):49–55. epub 2020 mar 11.
- Savva D. Prediction of difficult tracheal intubation. Br J Anaesth. 1994 Aug;73(2):149–153.
- Al Ramadhani S, Mohamed LA, Rocke DA, et al. Sternomental distance as the sole predictor of difficult laryngoscopy in obstetric anaesthesia. Br J Anaesth. 1996Sep;77(3):312–316. Erratum in: br j anaesth 1996 nov;77(5):701.ramadhani sa [corrected to al ramadhani s]. pmid: 8949801
- Liaskou C, Vouzounerakis E, Moirasgenti M, et al. Anatomic features of the neck as predictive markers of difficult direct laryngoscopy in men and women: a prospective study. Indian J anaesth. 2014mar;58(2):176–182. Erratum in: Indian j anaesth. 2015 jan;59(1):63.chara, liaskou [corrected to liaskou, chara]; eleftherios, vouzounerakis [corrected to vouzounerakis, eleftherios]; maria, moirasgenti [corrected to moirasgenti, maria]; anastasia, trikoupi [corrected to trikoupi, anastasia]; chryssoula, staikou [corrected. erratum in: Indian j anaesth. 2015 jan;59(1):63
- Shiga T, Wajima Z, Inoue T, et al. Predicting difficult intubation in apparently normal patients: a meta-analysis of bedside screening test performance. Anesthesiology. 2005 Aug;103(2):429–437.
