ABSTRACT
Background
Hysteroscopy is a procedure for management of intrauterine pathology. Glycine 1.5% (200 mOsm/L) is one of the most commonly used distension media in hysteroscopy; but it carries risk of hypervolemia and dilutional hyponatremia.
Objectives
Studying effects of systemic absorption of irrigating fluids on hemodynamic parameters, detect fluid deficit impact on clinical outcome included biochemical, hematological parameters, conscious level, pulmonary congestion and/or edema postoperative bleeding and hospital stay.
Methods
Sixty patients ASA classes I & II aged between 20 and 40 years underwent elective operative hysteroscopy randomly assigned into two groups. The Study group (30 patients): where consequent saline 0.9% and glycine 1.5% were used as irrigating distension media. Control group (30 patients): where glycine 1.5% alone was used as a distension medium.
Results
Comparing study and control group regarding (MBP) and heart rate, they were significantly higher at recovery and 6 hours postoperatively in the control group. (CVP) readings, showed significantly higher reading in the control group at times (15 m, 30 m, 45 m after induction, six hours and after recovery). Thoracic electrical bioimpedance parameters showed that COP, Cardiac index, Stroke volume and Stroke index were significantly higher in the control group than study group at 6 hours postoperatively. Regarding serum sodium, it was significantly lower in the control group than study group at times (15 min, 30 min and 45 min intra operatively) compared to pre-induction value. Serum osmolality was lower at 6 hours in the control group. Hemoglobin, hematocrit and platelet count was lower at 6 hours among control group.
Conclusion
The sequential use of saline 0.9% and glycine 1.5% decreased the amount of absorbed glycine 1.5% and hence the related side effects and complications.
Trial registration
Clinical Trials.gov. (NCT03166228)
1. Introduction
Hysteroscopy is a procedure for management of intrauterine pathology.
A uterine distending medium is used for visualization of endometrial cavity. Glycine 1.5% (200 mOsm/L) is one of the most commonly used distension media in hysteroscopy; as it is electrolyte free, so helping to remove the pathology without any effect on the normal surrounding tissues [Citation1], but it causes hypervolemia and consequent dilutional hyponatremia, while the use of isotonic fluid is considered safer and not causes hyponatremia or hypervolemia [Citation2], so it can be used for early entrance of uterus, proper visualization and wash tissue debris after resection, but it is an electrolyte-containing fluid, so this can damage the tissues.
2. Patients and methods
This randomized single blinded comparative study was carried out at the Woman’s Health Hospital, Assuit University, in the duration from April 2018 to October 2019.
2.1. Ethical considerations
This study was approved by the Medical Ethics Committee, Faculty of Medicine, Assiut University (reference number IRB17200030). Before the first patient was enrolled, the trial was registered on Clinical Trials.gov. (NCT03166228), and written informed consent was obtained from all patients participating in the study.
2.2. Patients
Sixty female patients aged 20–40 years scheduled for operative hysteroscopy and had an American Society of Anesthesiologists (ASA) class I & II. Any patient with cardiac problem, renal problem, CNS problem, pulmonary problem, hepatic problems, coagulation abnormalities and post-menopausal bleeding were excluded from the study.
2.3. Randomization and blindness
The patients were randomized by using sealed envelope method to assign the patients in a 1:1 ratio. Only the patients in each group were blinded in our study.
2.4. Study protocol
2.4.1. Anesthetic technique
On patients’ arrival to the operating room, insertion of 20 gauge IV catheter and ECG, automated blood pressure cuff and pulse oximeter were attached to the patients (CARESCAPE B650 monitor, Finland), thoracic electrical bioimpedance apparatus was attached before induction of anesthesia to the patients (TEB) (BoMed7179, USA) and radial arterial catheter was inserted in the right radial artery after Allen’s test was done under local anesthesia for arterial sample for blood gas analysis. CVP was inserted under ultrasonographic guidance after induction of anesthesia. All patients were anesthetized by the same technique; they were premedicated with midazolam 0.1–0.2 mg (iv) 15 min before induction of anesthesia, 10 ml/kg normal saline were given to all patients of studied groups 20 min before induction of anesthesia to replace fasting period. Induction of anesthesia with fentanyl 1 µg/kg and propofol 2 mg/kg and endotracheal intubation was facilitated by cisatracurium 0.15 mg/kg; patients were mechanically ventilated at a rate of 12 breaths per minute and tidal volume of 8 ml/kg (GE Medical systems SCS 78530, France). Anesthesiawas maintained with supplemental isoflurane 1.0% in mixed oxygen-air and maintenance of muscle relaxation by additional dose of cisatracurium 0.1 mg/kg using train of four testing (TOF). No intravenous fluids were given to the patients during the procedure unless the patient is in need for intravenous fluid (in cases of hypotension) (guided by CVP readings).
After the patient was put in lithotomy position, the surgeon started to distend the uterus with glycine 1.5% only in the control group and saline 0.9% in the study group as long as diathermy is not in use and then we shifted on glycine 1.5% on firing of diathermy. At the end of surgery, reversal of curarization was accomplished by the slow intravenous injection of 0.04 mg/kg prostigmine with atropine 0.01–0.02 mg/kg until full tidal volume was resumed and extubation was done. The patients then shifted to (ICU) postoperatively for postoperative monitoring.
2.4.2. Data collection
Non-invasive blood pressure, heart rate, arterial oxygen saturation (Spo2). Non-invasive continuous cardiac output monitoring using thoracic Electrical Bio-impedance apparatus (TEB) (BoMed7179) was done which gives the following data: Cardiac output (CO), cardiac index (CI), stroke volume (SV), stroke index (SI), end diastolic volume (EDV), end diastolic index (EDI), ejection fraction (EF), and systemic vascular resistance (SVR). Arterial blood gases (PaO2 and PaCO2) in mmHg, serum sodium and serum potassium concentration, blood glucose level, Blood urea, serum creatinine (mg/dl), and blood osmolality [Blood osmolality = serum Na (mmol/L) x 2 + blood glucose+ blood urea (mmol)]. All these data were collected pre-induction and every 15 min intra-operatively and at 6 hrs. and 24hrs. postoperatively. Complete blood picture [hemoglobin concentration (Hb) gm/dl, hematocrit value (Hct)% and platelet count (PLT) (x103/mm3)], and coagulation parameters [prothrombin concentration (PC)%, prothrombin time (PT) in seconds and partial thromboplastin time (PTT) in seconds] were collected at 6 hrs. and 24 hrs. postoperatively. Fluid deficit was measured every 15 minutes intraoperatively, and the total was measured at the end of procedure.
Fluid outflow was collected and the absorbed volume was calculated as:
[Absorbed fluid volume (ml) = total used fluid volume – retrieved fluid volume
2.4.3. Assessment parameters
2.4.3.1. Primary outcome
The effects of systemic absorption of irrigating fluids on hemodynamic parameters (cardiac output, blood pressure, central venous pressure, heart rate).
2.4.3.2. Secondary outcome
Effect of fluid deficit on conscious level, pulmonary congestion and edema and postoperative bleeding, hospital stay, and also hematological parameters including (hemoglobin level, hematocrit, platelet count, INR, prothrombin time, prothrombin concentration and partial thromboplastin time (PTT) in seconds) and biochemical parameters (serum sodium and potassium, osmolality, serum urea and creatinine).
2.5. Statistical methods
2.5.1. Power calculation
Based on the data from a previous study Darwish et al. [2010, Citation3] that compared saline (0.9%) and glycine (1.5%) in a study and control group with a 30 patients each comparing the To assess safety, efficacy of the use of 0.9% saline with monopolar resectoscope as long as diathermy is not in use (for early entrance of uterus, proper visualization and wash tissue debris after resection) and glycine 1.5% on firing of diathermy, and compared it with the usage of glycine 1.5% alone as a distension medium as a primary outcome. A power analysis was done to find a sufficient sample size in determining a significant difference between the two groups by using an alpha value of 0.05 and a power of 80%. This established that a sample size of 30 patients was adequate per group (30 patients in each group).
2.5.2. Statistical tests
Data were collected and analyzed using SPSS (Statistical Package for the Social Science, version 20, IBM, and Armonk, New York). Continuous data was expressed in the form of mean ± SD while nominal data was expressed in the form of frequency (percentage).
Chi2-test was used to compare the nominal data of the studied groups. Continuous variables of both groups were compared by Student t test. Level of confidence was kept at 95%, and hence, P value was significant if <0.05.
3. Results
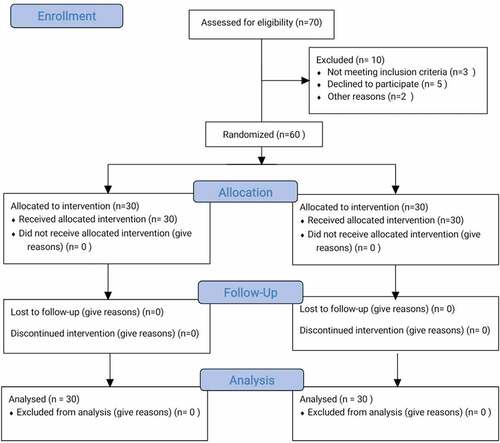
Seventy patients were eligible for this study. Sixty patients were enrolled into the two study groups (30 patients each) () (flow chart).
There was no significant differences between the studied groups regarding the demographic data and operative details except that the proper visualization of the lesion was significantly better in the study group than control group. The number of satisfied surgeons was higher in the stud
y group than the control group ().
Table 1. Demographic and operative data.
Comparison between study and control groups regarding MBP was significantly higher in the control group than the study group (p > 0.05) at times of recovery and 6 hours postoperatively compared to pre-induction value. CVP result among studied groups showed that it was significantly higher in the control group than in the study group at times (15 m, 30 m, 45 m after induction, six hours and after recovery) (p < 0.05) when compared to pre-induction value.
The cardiac output among studied groups showed that it was higher in the control group than study group at 6 hours which (p < 0.05). Cardiac index showed significant differences at 6 hours which was significantly higher in the control group (p < 0.05). Stroke volume and Stroke index were significantly higher in the control group than study group at 6 hours postoperatively ().
Table 2. Hemodynamic parameters.
Comparison of the amount of fluid absorption (glycine 1.5%) between study and control showed it was significantly lower in the study than control group. (P < 0.05). Serum osmolality showed it was lower in the control group than study group. Sodium level was significantly lower in the control group than the study group at times (15 minutes, 30 minutes and 45 minutes after induction) (P < 0.05). Regarding arterial blood gases data (ABG) (HCO3) we found no significant differences between the study and control groups except that HCO3 at 45 minutes after induction among the study group was significantly lower and these changes are still within the normal range and of no clinical importance. Comparison of (hemoglobin, hematocrit and platelet count) at different times showed that they were significantly lower in the control group than the study group at 6 hours postoperatively (P< 0.05) ().
Table 3. Fluid absorption, Osmolality, Biochemical and Hematological parameters.
4. Discussion
In this study, the comparison between the sequential use of saline 0.9% and glycine 1.5% (study group) and glycine 1.5% (control group) as a distension media showed that MBP significantly increased at times of recovery and six hours postoperatively as a part of hypervolemia that occurs with the use of glycine 1.5% but not with the study group. Heart rate showed a significant changes at times of recovery and 6 hours postoperatively. Still, these changes were within average values and of no clinical importance. CVP among studied groups showed that it was significantly higher in the glycine 1.5% group than in the study group. COP and CI readings between study and control groups showed that they were significantly higher at 6 hours in the control group.
Guidelines from the British Society of Gynecological Endoscopy (BSGE) and the European Society of Gynecological Endoscopy (ESGE) consider a threshold of 750 ml can be absorbed without significant serious effect while using hypotonic non-electrolyte solutions, while a volume of 2,500 mls of isotonic electrolyte solution as used with bipolar electrosurgical units can be absorbed without significant sequelae in healthy women [Citation4].
A study by Yousef et al. [2010, Citation5] showed that the mean blood pressure significantly increased after using the glycine 1.5% group but not in saline groups. Also, in intragroup comparison within the group using glycine 1.5%, there were significant changes within the glycine 1.5% group as a part of hypervolemia that occurs early in the systemic circulation but not with the usage of saline 0.9% as distension medium as saline 0.9% in nature is isotonic and not affecting the systemic circulation except very late.
Also Mukherjee and Santra [2021, Citation6] and Umranikar et al. [2016, Citation1] found that the mean blood pressure gradually increased when using glycine 1.5% in patients planned for TURP or operative hysteroscopy. They attributed this change to the hypervolemia which occurred by glycine 1.5% in the systemic circulation over time.
A study was conducted by Darwish et al. [2010, Citation3]. A myomectomy utilizing 0.9% saline in group A and a myomectomy using glycine 1.5% in group B showed a significant increase in EDV and EDI, whereas in our study there was no significant difference or increase in EDV OR EDI, but in agreement with our study that SV, SI, CO, CI increased for 45 min, then decreased in the following 30 min and postoperatively. Unlike our research results, Darwish et al. [2010, Citation3] also found no significant changes between these groups as hypervolemia occurred in both groups as the amount of used saline 0.9% was high, although it is isotonic and also glycine 1.5% caused hypervolemia as known because it is a hypotonic distension medium, and also unlike our results they found no significant changes in intragroup comparison within the group using glycine 1.5% as a distension medium but not occurred within the group using saline 0.9% .
In our study comparison between study and control groups according to biochemical data including (serum sodium, serum potassium urea, creatinine and serum osmolality) showed that serum sodium levels were significantly lower in the control group than study group at times (15, 30, and 45 minutes after induction) and serum osmolality was significantly lower in the control group (glycine 1.5%) at 6 hours postoperatively, but not when using sequential saline 0.9% and glycine 1.5% (study group) as a part of hypervolemia caused by glycine 1.5%. The main factor affecting the serum level of osmolality is sodium.
In agreement with our results, Mukherjee and Santra [2021, Citation6] found that serum sodium had a gradual fall in glycine 1.5% and saline groups throughout the procedure, but the drop in the sodium level was more in the glycine 1.5% group than in the saline group, which was statistically significant .
Also there were multiple studies that agreed with our result. Bhatta et al. [2022, Citation7], Atieh et al. [2021, Citation8], Darwish et al. [2010, Citation3] and Yousef et al. [2010, Citation5] found that serum sodium concentration decreased considerably with glycine 1.5% as a distension medium in hysteroscopy as a part of hypervolemia, causing dilutional hyponatremia.
Shalal et al. [2020, Citation9] reported an incidence of fluid overload that led to hypervolemia, increased mean arterial pressure, and hyponatremia within the first 10 min of operation because about 2 liters of glycine 1.5% were absorbed due to high intrauterine pressure .
In the aspect of serum level of osmolality, in contrast to our study result, Atieh et al. [2021, Citation8] reported that the serum osmolality was not changed with the usage of glycine 1.5% due to the presence of osmotically active particles of glycine 1.5% in the extracellular space.
Regarding arterial blood gases data (ABG, HCO3) we found no significant differences between the study and control groups except that HCO3 at 45 minutes after induction among the study group was significantly lower and these changes are still within the normal range and of no clinical importance. Bhatta et al. [2022, Citation7] reported that excessive glycine 1.5% usage was associated with metabolic acidosis.
In our study hemoglobin, hematocrit and platelet count were significantly lower at 6 hours among the control group. These changes may be dilutional and attributed to hypervolemia which occurred in the control group.
In agreement with our results, Darwish et al. [2010, Citation3], and Bhatta et al. [2022, Citation7] found that hemoglobin level, hematocrit level, prothrombin time and prothrombin concentration decreased when using glycine 1.5% as a distension medium.
In another study by Mukherjee and Santra [2021, Citation6] hematological parameters showed significantly decreased levels of hemoglobin and hematocrit in the glycine 1.5% group than the saline group, attributed to the hypervolemia caused by using glycine 1.5% and the resultant dilutional anemia.
5. Limitations
The present study has some limitations. Firstly: small sample size.
Secondly: the study did not use the advanced invasive modalities used in the monitoring of fluid overload as transesophageal echo and arterial blood pressure wave analysis. Another limitation is that this study was not a double blinded study.
6. Conclusion
The sequential use of saline 0.9% and glycine 1.5% decreased the amount of absorbed glycine 1.5% and hence the related side effects and complications. This method provides hemodynamic stability (cardiac output variables, blood pressure, and HR), so it decreases the functional load on the heart and consequent heart failure. This sequential use of saline 0.9% and glycine 1.5% kept blood electrolytes (sodium and potassium) within the normal range. Hence plasma osmolality does not disturb. Disturbed conscious level and pulmonary edema did not occur with this method. Lastly, this method helped in maintaining the average level of hemoglobin and normal coagulation profile. Surgeon satisfaction is good with this method.
Acknowledgments
Authors are grateful to the colleagues and staff of ICU for their co-operation in data collection.
Disclosure statement
No potential conflict of interest was reported by the authors
References
- S. Umranikar S, Clark TJ, Saridogan E, et al. BSGE/ESGE guideline on management of fluid distension media in operative hysteroscopy. Gynecol Surg. 2016;13(4):289–303.
- Mehta SJ, Roche Recinos A, Saggi SJ. A hypothesis for mechanism for brain oedema due to glycine. Med Hypotheses. 2017;103:58–61.
- Darwish AM, Hassan ZZ, Attia AM, et al. Biological effects of distension media in bipolar versus monopolar resectoscopic myomectomy: a randomized trial. J Obstetrics Gynaecol Res. 2010;36(4):810–817.
- Munro MG, Storz K, Abbott JA, et al.; AAGL Advancing Minimally Invasive Gynecology Worldwide. AAGL practice report: practical guidelines for the management of hysteroscopic distending media. J Minim Invasive Gynecol. 2013;20:137–148.
- Yousef AA, Suliman GA, Elashry OM, et al. A randomized comparison between three types of irrigating fluids during transurethral resection in benign prostatic hyperplasia. BMC Anesthesiol. 2010;10(1):1–7.
- Mukherjee P, Santra S. A Comparison of Hemodynamic and Biochemical Changes Between Normal Saline Irrigation and Glycine Irrigation in Transurethral Resection of Prostate. Int J Health Clin Res. 2021;4(22):279–285.
- Bhatta PN, Yadav UK, Raya A, et al. Comparison of Glycine versus Sterile Water Use in Transurethral Resection of the Prostate (TURP): a Cross Sectional Study. J Nat Med Colle. 2022;6(2):64–67.
- Atieh AS, Abu Shamma OK, Abdelhafez MO, et al. Acute Severe Hyponatremia following Hysteroscopic Procedure in a Young Patient: a Case Report and Review of the Literature. Case Rep Nephrol. 2021;2021:1–9.
- Shalal H, Aburawi A, Wright G. Phillip H. Is 1.5% Glycine a Comfortable Assistant in the Performance of Operative. Hysteroscopy Gynecol Surg. 2020;9(2):87–89.