ABSTRACT
Objectives
To compare using deep neuromuscular blockade during low abdominal insufflation pressure (DNMB/LAIP; n = 67) to conventional blockade and pressure (CNMB/CAIP; n = 68) for laparoscopic cholecystectomy and to evaluate the speed and efficacy of NMB recovery using sugammadex (SGX) as assessed by the Postoperative Quality Recovery Scale.
Patients & Methods
Rocuronium initiation and maintenance doses were 0.6 and 0.15 mg/Kg, respectively, and neostigmine or SGX was used as reverse agent for CNMB and DNMB, respectively. Abdominal insufflation was terminated at 15 and 8-mmHg, for CAIP and LAIP, respectively. The study outcome is the surgical feasibility under DNMB/LAIP, as judged by the frequency of shift-to-CAIP, surgical field visibility and operative time.
Results
The frequency of shift-to-CAIP was 2.9% due to surgeons’ inconvenience of LAIP. DNMB allowed significant control of intraoperative (IO) hemodynamic response to surgical manipulations. SGX allowed 3.2 times faster NMB-reversal with significantly higher percentages of patients returned to baseline physiologic statuses. The percentage of patients free of pain and nausea was significantly higher after DNMB/LAIP. At hospital discharge and day-7 PO, 86.6% and 98.5% of patients regained normalcy of their overall perspectives after DNMB/LAIP with a significant difference than after CNMB/CIAP. At 2-week PO, the frequency of shoulder-tip pain (STP) was significantly lower and surgeons’ satisfaction rate was significantly with DNMB/LAIP.
Conclusion
Laparoscopic cholecystectomy under DNMB/LAIP procedure is feasible and safe with lower incidence and severity of STP and high surgeons’ satisfaction. Sugammadex hastened the recovery of DNMB 3.2 times that of neostigmine-induced recovery of CNMB. Registration NO: RC.3.9.2023
1. Introduction
Laparoscopic surgery has gained popularity in clinical practice, and laparoscopic cholecystectomy is one of the most common laparoscopic procedures [Citation1]. Creation of pneumoperitoneum (PNP) is a key element in laparoscopic surgery; however, abdominal insufflation has multiple physiological impacts especially the ventilation and hemodynamic effects due to limited diaphragmatic mobility, CO2 absorption through the peritoneal surfaces, the pressure exerted on intra-abdominal vessels that could impede the venous return and cardiac filling capacity [Citation2–4]. Postoperative (PO) shoulder-tip pain (STP) is another problem related to PNP and is mostly related to phrenic nerve irritation [Citation5].
These PNP-induced complications are mostly related to the exerted abdominal insufflation pressure (AIP) to achieve the desired field visibility, so manipulations such as gasless laparoscopic surgery were suggested to lessen the effect of high AIP especially the cardiopulmonary side effects [Citation6]. Comparative studies assured the feasibility of low AIP (LAIP) with consequent decreases in CO2 absorption, significant improvement in PO-STP and less consumption of analgesia [Citation5,Citation7]. Moreover, extreme LAIP might be feasible without increasing operative and PO complications [Citation8].
Neuromuscular blockade (NMB) is used during laparoscopic surgery to expand the surgical field, and the quality of surgical conditions was found to be proportionate with the depth of NMB [Citation9]. Deep NMB (DNMB) for laparoscopic surgery would allow for the use of lower AIP while optimizing surgical space and enhancing patient safety [Citation10]. However, the risk of PO residual curarization is an additional risk for respiratory complications and increases the length of hospital stay and related costs [Citation11].
1.1. Objectives
Comparison of the outcomes of laparoscopic cholecystectomy using DNMB/LAIP versus using conventional AIP and conventional NMB (CNMB/CAIP) and to assess the speed and efficacy of DNMB-reversal using sugammadex (SGX) are the study objectives.
1.2. Design
Prospective multicenter comparative study
1.3. Setting
Departments of Anesthesia, Pain and ICU, Faculty of Medicine, Cairo and Benha Universities and multiple private surgical centers
1.4. Ethical considerations
The study protocol was approved by the Anesthesia Departmental Committee in June 2022 to permit the start of the application of the study protocol and after complete case collection, the study protocol and outcomes were approved by the Ethical Committee at the Faculty of Medicine, Benha University (Registration No.: RC.2.9.23).
1.5. Sample size
In 2021, one study detected insignificant differences between sugammadex and traditional reverse agents when the sample size was 50 patients per group [Citation12], while another study reported a highly significant difference when the number of patients was 75 patients per group [Citation13]. The null hypothesis was the detection of significant difference between groups and considering the effect size of 0.20, using the F-test model, the required sample size was calculated using the G*Power (Version 3.1.9.2) for sample size calculation [Citation14] and with the use of α error factor of 5% and a power of 80%, sample size of more than 67 patients per group would assure the reliability of the null hypothesis.
1.6. Patients
All adult patients presenting to the surgery outpatient clinic with the clinical picture of chronic calcular cholecystitis were evaluated clinically and by abdominal ultrasonography. Patients suspected to have complicated cholecystitis underwent abdominal MRI. Then, demographic and clinical data were determined
1.7. Exclusion criteria
Patients who had myopathies or neuromuscular disorders, ASA grade III or IV, obesity of >35 kg/m2, complicated cholecystitis, associated pancreatitis, peptic ulcer disease, uncontrolled diabetes mellitus, renal or liver diseases, and previous open abdominal surgeries were excluded from the study.
1.8. Inclusion criteria
Patients who had chronic calcular cholecystitis and were free of exclusion criteria were included in the study.
1.9. Randomization and grouping
Patients’ randomization was conveyed by an assistant who was blinded about the study protocol by computer sequencing system with 1:1 sequence and even-numbers dropping to provide the sequence of cases for each group. Patients’ sequence was transformed to group title; Conventional NMB (Group-C) and Deep NMB (Group-D) and patients were asked to choose an envelope that contained a card carrying the group title. Surgeons were blinded about the depth of the used neuromuscular block and about the reverse agent
1.10. Groups
All patients received an initial dose of rocuronium of 0.6 mg/Kg and the maintenance dose (0.15 mg/Kg) was adjusted according to the desired depth of anesthesia as previously described by Barrio et al. [Citation15]:
Conventional NMB (Group C): rocuronium was provided as a maintenance dose when two responses appeared in the Train of Four stimulation (TOF) and at the end of surgery neostigmine (70 μg/kg) was given as an NMB-reversing drug.
Deep NMB (Group D): the maintenance dose was given when two post-tetanic contractions (PTCs) appeared. NMB was reversed using sugammadex 4 mg/kg at the end of surgery.
1.11. Anesthetic technique
At the pre-anesthetic room, baseline preoperative hemodynamic variate; heart rate (HR) and mean arterial pressure (MAP) were non-invasively recorded. Midazolam premedication was provided in an intravenous dose of 0.05 mg/kg up to 2.5 mg. Pre-oxygenation was provided for all patients, anesthesia was induced using propofol 1.5–2.5 mg/kg and IV rocuronium bromide 0.6 mg/Kg, and after 3-min the trachea was intubated. Anesthesia was maintained with 50% air in oxygen, and an end-tidal concentration of 2–3% sevoflurane and a maintenance dose of rocuronium was provided as 0.15 mg/kg. Ventilation was controlled and minute ventilation was adjusted to maintain end-tidal CO2 at 35 ± 5 mmHg. Then, intraoperative fentanyl was given as 1–2 µg/kg/min to maintain non-invasive HR within a range of ± 20% of the basal values, and MAP measures are in the range of 65–100 mmHg. At the end of the surgery, NMB was reversed in Group-C using intravenous neostigmine (70 μg/kg) and atropine sulfate 15–20 µg/kg, while in Group-D using sugammadex 4 mg/kg and the trachea was extubated after reversal of NMB and patients were maintained on supplemental O2 until awake in the recovery room
1.12. Pneumoperitoneum and surgical procedure
The Verres needle was inserted through a snip umbilical, the patient was adjusted in 30° Trendelenburg position and an electronic variable-flow insufflator was connected for intra-peritoneal insufflation of CO2 that was terminated when the AIP reached 15 and 8 mmHg, for groups C and D, respectively. After the insertion of the video laparoscope through the cannula, exploratory laparoscopy was performed, and the patient’s position was changed to a steep reverse Trendelenburg position (RTP) with a lateral tilt to facilitate retraction of the gall bladder fundus. At the end of the surgery, abdominal desufflation was performed, and the patient’s position was corrected to the flat supine position [Citation16].
2. Monitoring
Operative monitoring:
The frequency of shifts to CAIP due to bad surgical field was recorded.
Heart rate (HR) and mean arterial pressure (MAP) were continuously monitored and the measures obtained before and after induction of anesthesia, 5-min before and after insufflation, and 5-min after tilting in RTP, after CO2 insufflation, and extubation were recorded.
Surgical field visibility was scaled using a 5-point Likert scale for quality with a high score (=5) indicating very good quality and a low score (= 1) indicating very poor quality of field visibility. The surgical field visibility scoring was presented as patients’ distribution and as a median value of the total score. Operative time was also recorded and presented as a mean value.
Recovery of NMB & PACU care
The time from the start of sugammadex/neostigmine administration to the recovery of the train-of-four ratio (TOFR) to 0.9 was determined.
Recovery of NMB was assessed using the Postoperative Quality Recovery Scale (PQRS) which consists of six domains including physiologic, nociceptive, emotive, activities of daily living, cognitive, and overall patient perspective as shown in [Citation17]. Recovery was defined as the percentage of patients who returned to baseline values (or better) of each domain at the defined time points [Citation18].
Table 1. Domains of the post-operative quality recovery scale for recovery from NMB [Citation17].
Patients were evaluated for PACU discharge using the modified Aldrete score that ranges between zero and 12 and the patient was discharged at a score of ≥9 [Citation19].
Postoperative care
All patients received routine PO analgesia as ketorolac tromethamine (15 mg/ml) diluted to 20 ml with normal saline 0.9% to yield 1.5 mg/ml and was injected intravenously in a dose of 7.5 mg as 5-ml shots.
Wound pain was assessed using an 11-point (0–10) numeric pain scale (NRS) score with zero indicating no pain and 10 indicating the worst intolerable pain [Citation20]. When the NRS score was ≥4 despite receiving ketorolac injection, morphine 5 mg was diluted to 10 using normal saline 0.9% and injected IV as 2-ml dose till pain resolution. The frequency of patients who required PO morphine injection and the received dose was recorded.
PO duration till 1st ambulation and 1st oral intake were determined
PO nausea and vomiting (PONV) was scored on 0-3 points for nausea; no, mild, moderate, and severe nausea, while vomiting was scored on 0-2 points; no, one and more than one mouthful of vomitus [Citation21]; antiemetic therapy was provided as ondansetron (Zofran), which was previously documented as effective in a dose of 4 mg [Citation22] and was repeated according to PONV severity.
Surgeons’ satisfaction with operative circumstances and surgical field visibility was evaluated using a 5-point Likert satisfaction scale ranging between very dissatisfactory (=1) and very satisfactory (=5).
Hospital discharge and follow-up
Patients were discharged from the hospital after taking their 1st oral intake and can ambulate unaided; the duration of PO hospital stay was defined.
PO treatment was prescribed as broad-spectrum antibiotics and oral analgesia.
Patients were asked to check for STP which was defined as pain at the tip of the shoulder occurring during the 1st 2-wk after surgery [Citation23]. STP was presented as the frequency of patients who developed STP and its severity as judged by NRS score.
2.1. Study outcomes
The primary outcome is the evaluation of the feasibility of laparoscopic surgery using DNMB/LAIP procedure using the frequency of shift-to-CAIP, the surgical field visibility, operative time and surgeons’ satisfaction rate as judge for feasibility
The secondary outcome is the time elapsed since injection of the reversal agent till neuromuscular recovery and quality of recovery as judged by assessment of PQRS domains.
2.2. Statistical analysis
The results were analyzed using the ANOVA test for intergroup variance and the Chi-square test and Mann–Whitney test for non-parametric data by the SPSS Software Program (IBM, USA). The significance of the intergroup difference was determined at the cutoff point of P < 0.05.
3. Results
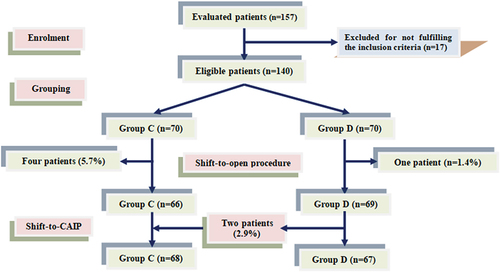
Seventeen patients were excluded; 3 pregnant women, 5 women were obese with body mass index (BMI) of >35 kg/m2, 4 patients had previous abdominal surgery, 3 patients had associated stone common bile duct and two patients were ASA III, while 140 patients were randomly allocated into the study groups. Five patients (3.57%) were shifted to open procedures for surgical indications and were also excluded from the study. Two of the Group-D patients (2.9%) were shifted to conventional AIP up on surgeons’ request for the inconvenience of low AIP and were considered as failure for low AIP (). The enrolment data of patients of both groups were comparable as shown in .
Table 2. Patients’ characteristic and demographic data in both groups.
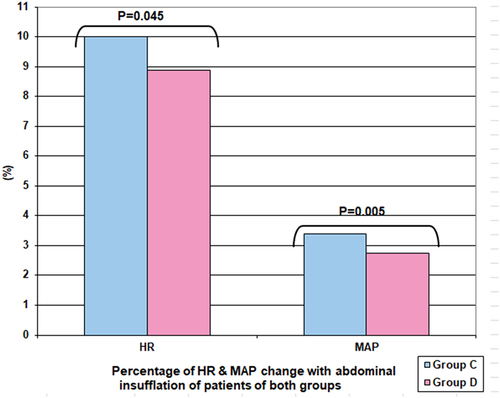
Deep NMB allowed proper control of intraoperative hemodynamic response to surgical manipulations as manifested by the reported significantly lower HR measures before (P = 0.039) and after (P < 0.001) abdominal insufflation and after table-tilting to RTP (P < 0.001) with significantly lower MAP measures after abdominal insufflation (P = 0.023) and insufflation (P = 0.003) in comparison to measures of patients of Group-C. Moreover, the extent of increase in HR and MAP measures of Group-D patients in response to abdominal insufflation was significantly (P = 0.045 & 0.005, respectively) lower compared to that recorded in Group-C patients (). Operative field visibility as scorings and mean score and operative time were comparable between both groups ().
Table 3. Patients’ intraoperative data.
Sugammadex allowed 3.2 times faster NMB-reversal than neostigmine within a significantly (P < 0.001) shorter duration than that of neostigmine. Regarding the domains of PQRS, the percentages of patients returned to baseline physiologic statuses after NMB-reversal and at the time of PACU discharge were significantly (P = 0.033 & 0.043, respectively) higher in Group-D than Group-C. The percentages of Group-D patients who had no pain at 4-h after PACU discharge and at hospital discharge were significantly (P = 0.038 & 0.028, respectively) higher than that of Group-C patients. Similarly, at 4-h after PACU discharge, the percentage of patients free of nausea sensation was significantly (P = 0.036) higher among Group-D patients. At time of hospital discharge and D-7 PO, 86.6% and 98.5% of Group-D patients regained normalcy of their overall perspectives with significant difference (P = 0.038 & 0.017, respectively) in comparison to the percentages of Group-C patients; 72.1% and 88.2% (). The frequency of patients reached Aldrete score of ≥9 was significantly (P = 0.027) higher with significantly (P = 0.0015) higher mean score among Group-D than Group-C patients ().
Figure 3. Patient’s distribution according to the percentages of patients returned to normally of PQRS domains at time of hospital discharge.
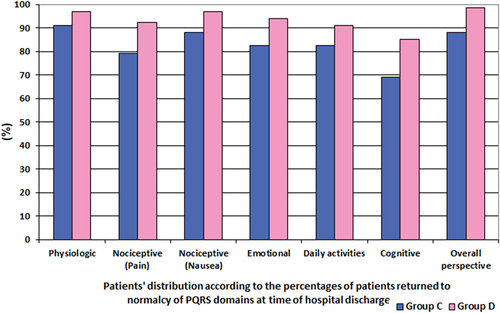
Table 4. Time till recovery of NMB and PQRS scale data.
During the hospital stay, no patient required morphine rescue analgesia. The reported pain scores were significantly higher at 2-h (P < 0.001) and 3-h (P = 0.032) PO, while were significantly (P = 0.0084) lower at 12-h PO in Group-D than Group-C patients, but other measures showed non-significant differences between both groups. Duration till 1st ambulation and oral intake were significantly (P = 0.006 & 0.025, respectively) shorter, while the duration of PO hospital stay was non-significantly (P = 0.157) shorter for patients of Group-D than patients of Group-C. No PO vomiting attacks were recorded, while 21 patients (15.6%) developed PO nausea with significantly lower incidence (P = 0.035) and score (P = 0.033) among Group-D than Group-C patients. At 2-w PO, 32 patients complained of STP, but the frequency of patients who complained of STP was significantly (P = 0.017) lower with significantly lower pain scores among Group-D than Group-C.
Regarding surgeons’ satisfaction, 101 surgeons (74.8%) were satisfied to very satisfied and 27 surgeons found either procedure was good, while only 6 surgeons (4.4) were dissatisfied with both procedures. The frequency of surgeons who were satisfied-to-very satisfied surgeons by the DNMB/LAIP procedure was significantly (P = 0.047) higher than those who were satisfied-to-very satisfied by the CNMB/CAIP, while the mean satisfaction score was non-significantly (P = 0.154) higher in Group-D than in Group-C (, ).
Figure 4. Surgeon’s distributionn according to their satisfaction by the applied procedure NMB & AIP.
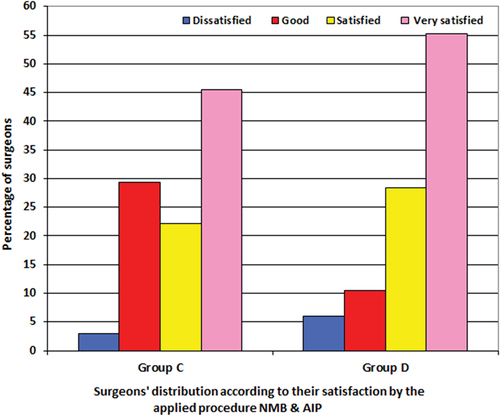
Table 5. Patients’ postoperative data.
4. Discussion
The use of DNMB allowed the successful conduction of laparoscopic cholecystectomy under LAIP as manifested by the reported minimal rate of shift-to-conventional pressure (2.9%) and dissatisfied surgeons (6%). Moreover, the reported operative field visibility rate score, and operative time were comparable to surgery under CNMB/CAIP. In support of the efficacy of the DNMB/LAIP procedure for laparoscopic surgery, Krijtenburg et al. [Citation24] using MRI estimated the skin-sacral promontory distance and detected increased distance by about 15% with moderate NMB than no NMB, but DNMB did not provide further increase, while increased the mean pneumoperitoneum volume.
The applied DNMB/LAIP policy was advantageous concerning the impact of increased AIP on HR and MAP which showed a significantly lower percentage of increase secondary to abdominal insufflation in comparison to patients who received CNMB/CAIP. In line with these findings, Oh et al. [Citation25] detected better operating conditions and higher overall satisfaction in lumbar spinal surgery under general anesthesia using deep versus no NMB. Thereafter, Kathopoulis et al. [Citation26] reported comparable mean surgical field scores during laparoscopic gynecological surgeries under moderate versus deep NMB and Zheng et al. [Citation27], in a meta-analysis for studies comparing deep versus no-deep NMB, found DNMB provided the higher frequency of clinically acceptable surgical conditions and lower incidence of intraoperative complications with the comparable incidence of PO complications.
Laparoscopic surgery provided patients with a satisfactory PO course, where no patient required morphine for PO pain and the use of DNMB/LAIP significantly improved PO wound pain scores than patients who received CNMB/CIAP. These results go in hand with Oh et al. [Citation25] who recorded significantly reduced pain scores, and PO rescue fentanyl consumption both in PACU and ward after lumber spinal surgery under general anesthesia with deep versus no NMB. Similarly, Seo et al. [Citation28] detected decreased PO pain scores and opioid consumption during laparoscopic urologic surgeries and recorded no correlation between PO pain and the amount of CO2 gas used, operative method or operative time and attributed this to performing surgery under anesthesia with DNMB. Also, Albers et al. [Citation29] reported lower acute pain scores with LAIP during laparoscopic colorectal surgery and Kathopoulis et al. [Citation26] found patients who received moderate NMB consumed more extra opioid analgesia than patients who received DNMB.
The DNMB/LAIP procedure significantly reduced the incidence and scorings of STP, at 2-w PO, in comparison to CNMB/CAIP. Similarly, Zhang et al. [Citation30] using the DNMB/LAIP reported decreased scores of STP without hindering the surgical vision or increasing adverse respiratory events and found this policy can shorten the hospital stay duration and treatment. Furthermore, Tang et al. [Citation31] detected significantly lower PO pain scores and opioid consumption after spinal surgery under general anesthesia with DNMB than moderate NMB and found pain scores were still significantly reduced till 3-month PO with a significant reduction of the incidence of chronic post-surgical pain with DNMB.
The obtained results and the literature suggest the anti-nociceptive effect of NMB for both acute and chronic pain and these effects are positively related to the depth of NMB, but no study provided an explanation for this effect and there is insufficient evidence to recommend DNMB to reduce PO pain [Citation32]. However, the reported anti-nociceptive effect for acute pain might be attributed to blunting of expression and release of nociceptive proinflammatory cytokines as tumor necrosis factor-α and interleukins, but this suggestion needs to be evaluated in further studies and the effect of DNMB on chronic pain has to be elucidated.
The residual curarization, which is the major side effect of DNMB, was significantly alleviated with the use of sugammadex (SGX) as an NMB-reversing agent. SGX allowed 3.2 times more rapid reversal of DNMB than neostigmine (NEO) for CNMB with a significantly shorter time lag between reversal-agent injection and recovery of TOFR to 0.9. These findings were coincident with Chang et al. [Citation33] who documented that SGX showed better hemodynamic stability and lower incidence of PONV and PO urinary retention than NEO and with Tang et al. [Citation34] who detected 4.9 times faster recovery after SGX than NEO injection after simultaneous pancreas-kidney transplantation. Also, Cui et al. [Citation35] found SGX-reversal of muscle relaxation in patients undergoing intracranial aneurysm intervention surgery can optimize the quality of anesthesia recovery and reduce the incidence of PO complications. Furthermore, Tsai et al. [Citation36] suggested the use of SGX as a better option for NMB reversal during interventional neuroradiological procedures than NEO because SGX provides shorter extubation time and more stable hemodynamics during the emergence of anesthesia.
The current study reported significantly lower incidence and severity of PONV after SGX reversal of DNMB than after NEO reversal for CNMB, similarly, Chang et al. [Citation33] and Hsieh et al. [Citation37] detected lower risk of PONV after SGX than with NEO especially for patients received volatile anesthetics, irrespective of using prophylactic antiemetics. Also, Ding et al. [Citation38] found SGX can decrease the incidence and severity of PONV, increase PO water intake and shorten the time to first flatus after bariatric surgery in comparison to NEO.
The applied procedure of DNMB/LAIP with SGX as a reversal agent allowed better immediate PO course in the form of significantly shorter time till 1st ambulation and oral intake with non-significantly shorter PO hospital stay than the procedure applied for Group-C patients. In line with these findings, Deljou et al. [Citation39] detected improved bowel function and a higher proportion of patients had bowel movement during the first 24 and 48 h after SGX than NEO reversal of NMB during craniotomy. Moreover, Azimaraghi et al. [Citation40] found SGX reversal of NMB was associated with a small decrease in PO length of hospital stay in the ambulatory care unit and attributed this to the reduced PONV. Also, Tan et al. [Citation41] reported that SGX-reversal of NMB after abdominal surgery showed excellent recovery profile with significantly shorter PACU stay, time to PO ambulation and reduced time-to-first-defecation when compared to the spontaneously recovered group
The reported improved surgical circumstances, recovery items and PO outcomes after the use of DNMB/LAIP with SGX-reversal coincided with the recently published recommendations of the European Society of Anesthesiology and Intensive Care that recommended deepening NMB if surgical conditions need to be improved and using SGX to antagonize deep, moderate and shallow NMB by aminosteroidal agents (32).
5. Conclusion
Laparoscopic cholecystectomy under DNMB and using LAIP is feasible and safe with a minimal failure rate and high surgeons’ satisfaction. The applied DNMB/LAIP improved surgical outcomes with a reduction of the incidence and severity of STP. Sugammadex hastened the recovery of DNMB 3.2 times that of neostigmine-induced recovery of CNMB and is advocated as a reversal agent for this procedure.
6. Limitations
Type of surgical procedure; laparoscopic cholecystectomy with its inherent short operative time and minimal tissue trauma is a limitation for the establishment of the obtained results with special regard to PO pain.
7. Recommendations
Further studies are mandatory to explore the underlying mechanisms for the reported decreased pain scores with DNMB than CNMB. Also, the same procedures were to be evaluated for laparoscopic procedures requiring long operative time or causing extensive tissue damage to settle the obtained results as an opioid-free procedure for laparoscopic surgeries
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Jolly S, Kundu N, Rathnayake S. A case of mistaken identity: bile duct masquerading as gallbladder. J Surg Case Rep. 2023;2023(1):rjad001. doi: 10.1093/jscr/rjad001
- Paek C, Yi J, Lee B, et al. No supplemental muscle relaxants are required during propofol and remifentanil total intravenous anesthesia for laparoscopic pelvic surgery. J Laparoendosc Adv Surg Tech A. 2009;19(1):33–37. doi: 10.1089/lap.2008.0051
- Eva I, Rosario V, Guglielmo R, et al. Laparoscopic surgery: a randomised controlled trial comparing intraoperative hemodynamic parameters and arterial-blood gas changes at two different pneumoperitoneal pressure values. Ann Med Surg. 2022;81:104562. doi: 10.1016/j.amsu.2022.104562
- Smith RB, Biller E, Hu C, et al. Impact of pneumoperitoneum pressure during laparoscopic hysterectomy: a randomized controlled trial.Eur. J Obstet Gynecol Reprod Biol. 2023;280:73–77. doi: 10.1016/j.ejogrb.2022.11.011
- Ortenzi M, MontorFi G, Sartori A, et al. Low-pressure versus standard-pressure pneumoperitoneum in laparoscopic cholecystectomy: a systematic review and meta-analysis of randomized controlled trials. Surg Endosc. 2022;36(10):7092–7113. doi: 10.1007/s00464-022-09201-1
- Jiang M, Zhao G, Huang A, et al. Comparison of a new gasless method and the conventional CO2 pneumoperitoneum method in laparoendoscopic single-site cholecystectomy: a prospective randomized clinical trial. Updates Surg. 2021;73(6):2231–2238. doi: 10.1007/s13304-021-01154-9
- Saway JP, McCaul M, Mulekar M, et al. Review of outcomes of low verses standard pressure pneumoperitoneum in laparoscopic surgery. Am Surg. 2022;88(8):1832–1837. doi: 10.1177/00031348221084956
- Park SE, Hong TH. The effectiveness of extremely low-pressure pneumoperitoneum on pain reduction after robot-assisted cholecystectomy. Asian J Surg. 2023;46(1):539–544. doi: 10.1016/j.asjsur.2022.06.077
- Kirmeier E, Eriksson LI, Lewald H, et al. Post-anaesthesia pulmonary complications after use of muscle relaxants (POPULAR): a multicenter, prospective observational study. Lancet Respir Med. 2019;7(2):129–140. doi: 10.1016/S2213-2600(18)30294-7
- Lowen D, Hodgson R, Tacey M, et al. Does deep neuromuscular blockade provide improved outcomes in low pressure laparoscopic colorectal surgery? A single blinded randomized pilot study. ANZ J Surg. 2022;92(6):1447–1453. doi: 10.1111/ans.17458
- Cappellini I, Picciafuochi F, Ostento D, et al. Recovery of muscle function after deep neuromuscular block by means of diaphragm ultrasonography and adductor of pollicis acceleromyography with comparison of neostigmine vs. sugammadex as reversal drugs: study protocol for a randomized controlled trial. Trials. 2018;19(1):135. doi: 10.1186/s13063-018-2525-7
- Ozbilgin S, Kuvaki B, Şimşek H, et al. Comparison of airway management without neuromuscular blockers in laparoscopic gynecological surgery. Medicine (Baltimore). 2021;100(7):e24676. doi: 10.1097/MD.0000000000024676
- Valencia Morales DJ, Stewart B, Heller S, et al. Urinary retention following Inguinal Herniorrhaphy: role of neuromuscular blockade reversal. Surg Laparosc Endosc Percutan Tech. 2021;31(5):613–617. doi: 10.1097/SLE.0000000000000962
- Faul F, Erdfelder E, Lang AG, et al. G*power 3: a flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav Res Methods. 2007;39(2):175–191. doi: 10.3758/BF03193146
- Barrio J, Errando C, Miguel G, et al. Effect of depth of neuromuscular blockade on the abdominal space during pneumoperitoneum establishment in laparoscopic surgery. J Clin Anesth. 2016;34:197–203. doi: 10.1016/j.jclinane.2016.04.017
- Dubois F, Icard P, Berthelot G, et al. Coelioscopic cholecystectomy preliminary report of 36 cases. Ann Surg. 1995;211(1):60–62. doi: 10.1097/00000658-199001000-00010
- Royse CF, Newman S, Chung F, et al. Development and feasibility of a scale to assess postoperative recovery: the post-operative quality recovery scale. Anesthesiology. 2010;113(4):892–905. doi: 10.1097/ALN.0b013e3181d960a9
- Amorim P, Lagarto F, Gomes B, et al. Neostigmine vs. sugammadex: observational cohort study comparing the quality of recovery using the postoperative quality recovery scale. Acta Anaesthesiol Scand. 2014;58(9):1101–1110. doi: 10.1111/aas.12389
- Aldrete JA. The post-anesthesia recovery score revisited. J Clin Anesth. 1995;7(1):89–91. doi: 10.1016/0952-8180(94)00001-k
- Williamson A, Hoggart B. Pain: a review of three commonly used pain rating scales. J Clin Nurs. 2005;14(7):798–804. doi: 10.1111/j.1365-2702.2005.01121.x
- Watcha MF. White PF: postoperative nausea and vomiting. Its etiology, treatment, and prevention. Anesthiology. 1992;77(1):162–184. doi: 10.1097/00000542-199207000-00023
- Garbe C, Drechsler S, Fiedler H, et al. Dose comparison of tropisetron (navoban) 5 mg and 10 mg orally in the prophylaxis of dacarbazine-induced nausea and emesis. Semin Oncol. 1994 21(5 Suppl 9):12–16.
- Madsen MV, Istre O, Staehr-Rye A, et al. Postoperative shoulder pain after laparoscopic hysterectomy with deep neuromuscular blockade and low-pressure pneumoperitoneum: a randomised controlled trial. Eur J Anaesthesiol. 2016;33(5):341–347. doi: 10.1097/EJA.0000000000000360
- Krijtenburg P, Bruintjes M, Fütterer J, et al. MRI measurement of the effects of moderate and deep neuromuscular blockade on the abdominal working space during laparoscopic surgery, a clinical study. BMC Anesthesiol. 2023;23(1):238. doi: 10.1186/s12871-023-02201-1
- Oh S, Kwon W, Park S, et al. Comparison of operating conditions, postoperative pain and recovery, and overall satisfaction of surgeons with deep vs. No neuromuscular blockade for spinal surgery under general anesthesia: a prospective randomized controlled trial. J Clin Med. 2019;8(4):498. doi: 10.3390/jcm8040498
- Kathopoulis N, Protopapas A, Stamatakis E, et al. Deep versus Moderate Neuromuscular Blockade in Gynecologic Laparoscopic Operations: Randomized Controlled Trial. J Pers Med. 2022;12(4):561. doi: 10.3390/jpm12040561
- Zheng J, Du L, Zhang L, et al. Deep neuromuscular block for endolaryngeal surgery: a systematic review and meta-analysis. Laryngoscope. 2023;133(9):2055–2065. doi: 10.1002/lary.30561
- Seo IY, Oh T, Lee C. Is the amount of carbon dioxide gas used in urologic laparoscopic surgeries associated with postoperative pain? Investig Clin Urol. 2020;61(3):284–290. doi: 10.4111/icu.2020.61.3.284
- Albers K, Polat F, Helder L, et al. RECOVER study collaborators: quality of recovery and innate immune homeostasis in patients undergoing low-pressure versus standard-pressure pneumoperitoneum during laparoscopic colorectal surgery (RECOVER): a randomized controlled trial. Ann Surg. 2022;276(6):e664–e673. doi: 10.1097/SLA.0000000000005491
- Zhang Y, Li Y, Huang W, et al. Utilization of deep neuromuscular blockade combined with reduced abdominal pressure in laparoscopic radical gastrectomy for gastric cancer: an academic perspective. World J Gastrointest Surg. 2023;15(7):1405–1415. doi: 10.4240/wjgs.v15.i7.1405
- Tang X, Wu Y, Chen Q, et al. Deep neuromuscular block attenuates chronic postsurgical pain and enhances long-term postoperative recovery after spinal surgery: a randomized controlled trial. Pain Ther. 2023;12(4):1055–1064. doi: 10.1007/s40122-023-00528-8
- Chang HC, Liu SY, Lee MJ, et al. Sugammadex reversal of muscle relaxant blockade provided less post-anesthesia care unit adverse effects than neostigmine/glycopyrrolate. J Formos Med Assoc. 2022;121(12):2639–2643. doi: 10.1016/j.jfma.2022.04.017
- Tang J, He R, Zhang L, et al. Safety and efficacy of 4 mg·kg− 1 sugammadex for simultaneous pancreas-kidney transplantation recipients: a prospective randomized trial. Ann Transplant. 2023;28:e940211. doi: 10.12659/AOT.940211
- Fuchs-Buder T, Romero C, Lewald H, et al. Peri-operative management of neuromuscular blockade: a guideline from the European Society of Anaesthesiology and Intensive care. Eur J Anaesthesiol. 2023;40(2):82–94. doi: 10.1097/EJA.0000000000001769
- Cui J, Yao L, Wu J, et al. Effect of sugammadex on postoperative nausea and vomiting after surgery for intracranial aneurysm. Zhonghua Wai Ke Za Zhi. 2023;61(8):700–706. doi: 10.3760/cma.j.cn112139-20230111-00016
- Tsai Y, Chen C, Wong H, et al. Comparison of neostigmine and sugammadex for hemodynamic parameters in neurointerventional anesthesia. Front Neurol. 2023;14:1045847. doi: 10.3389/fneur.2023.1045847
- Hsieh Y, Lin C, Liu Y, et al. The effect of sugammadex versus neostigmine on postoperative nausea and vomiting: a meta-analysis of randomized controlled trials with trial sequential analysis. Minerva Anestesiol. 2023;89(5):434–444. doi: 10.23736/S0375-9393.22.16972-5
- Ding X, Zhu X, Zhao C, et al. Use of sugammadex is associated with reduced incidence and severity of postoperative nausea and vomiting in adult patients with obesity undergoing laparoscopic bariatric surgery: a post-hoc analysis. BMC Anesthesiol. 2023;23(1):163. doi: 10.1186/s12871-023-02123-y
- Deljou A, Soleimani J, Sprung J, et al. Effects of reversal technique for neuromuscular paralysis on time to recovery of bowel function after Craniotomy. Am Surg. 2023;89(5):1605–1609. doi: 10.1177/00031348211058631
- Azimaraghi O, Ahrens E, Wongtangman K, et al. Association of sugammadex reversal of neuromuscular block and postoperative length of stay in the ambulatory care facility: a multicentre hospital registry study. Br J Anaesth. 2023;130(3):296–304. doi: 10.1016/j.bja.2022.10.044
- Tan J, He J, Wang L, et al. Analysis of the association of sugammadex with the length of hospital stay in patients undergoing abdominal surgery: a retrospective study. BMC Anesthesiol. 2023;23(1):32. doi: 10.1186/s12871-023-01979-4