ABSTRACT
Objective
Acute, severe pain following breast surgery affects about 40% of individuals. It has proven possible to lessen postoperative pain related to modified radical mastectomy (MRM) by developing several thoracic wall blocks. This study evaluated the analgesic benefit of pectoral nerve block type 2 (PECS II) in conjunction with ultrasonography-guided serratus anterior plane block (SAPB) as opposed to SAPB alone in patients undergoing MRM.
Methods
In this randomized double-blind trial, female patients undergoing MRM under general anesthesia were randomly assigned to the SAPB Group (n = 30) or the Combined Group (n = 30). Along with block-related problems, the total amount of fentanyl consumed during the procedure and the amount of morphine consumed over in the first 24 hours after surgery were noted. During rest and movement, pain was measured using the Numeric Rating Scale (NRS).
Results
The total intraoperative fentanyl consumption was reduced to 130.7 ± 44.4 µg in the combined group compared to 160.0 ± 53.2 µg in the SAPB group (p = 0.024). Also, postoperative morphine consumption was 1.5 mg (0–6) and 6 mg (3–9) in the two groups, respectively (p = 0.005). The Combined group showed significantly lower scores of NRS at rest and during movement than the SABP group throughout the postoperative period.
Conclusion
Ultrasound-guided SAPB plus PECS II block provides safer and more efficient analgesia in MRM than SABP alone, as evidenced by decreased postoperative morphine consumption, pain scores, and intraoperative fentanyl consumption.
1. Introduction
Globally, breast cancer (BC) has become the number one malignant tumor [Citation1]. Surgery remains the primary option in its treatment, with modified radical mastectomy (MRM) being the first alternative [Citation2], accounting for 31% of all breast surgical procedures [Citation3]. MRM is a major procedure involving the removal of the entire breast, including the areola, nipple, and the majority of axillary lymph nodes [Citation4].
In 40% of women undergoing MRM, extensive tissue dissection and seroma development lead to severe acute postoperative pain. Besides, between 25% and 60% experience persistent pain following mastectomy [Citation5]. Pain results from both neuropathic origin, brought on by interference with the second to sixth intercostal nerves, and inflammation generated by tissue damage. Prolonged hospital stays and substantial discomfort are the results of this [Citation6].
In breast surgery, postoperative pain management is a primary objective of anesthesia. Appropriate treatment of acute postoperative pain is critical for optimizing patient outcomes and enhancing satisfaction. A wide range of anesthetic agents, devices, and strategies are available. Intravenous opioid analgesia has long been the predominant method of postoperative pain management. However, new anesthetic techniques characterized by enhanced safety, reduced pain, and fewer complications have been advocated [Citation7].
Currently, multimodal analgesia is advised by international guidelines [Citation8]. As an element of multimodal analgesia, regional anesthesia techniques have demonstrated efficacy in managing postoperative pain. These comprise ultrasound-guided interfascial plane blocks, thoracic epidural anesthesia, and paravertebral blocks [Citation9].
As an interfascial plane block, the serratus anterior plane block (SAPB) can target the neural network supplying the breast and chest wall. SAPB provides analgesia to the chest wall by blocking the T2–9 intercostal nerves, which pass through the serratus anterior and intercostal muscles, as well as the long thoracic and dorsal thoracic nerves [Citation10]. The pectoral nerve (PECS) block is another interfascial plane block that affects the long thoracic nerves, intercostal nerves 3–to 6, and medial and lateral pectoral nerves [Citation11]. The local anesthetic (LA) is injected into two fascial planes in the PECS II block: the one between the serratus anterior and pectoralis minor muscles, and the other between the pectoralis major and minor muscles [Citation12].
By blocking the medial and lateral pectoral nerves that cause myofascial pain, which are spared in SAPB alone, adding a modified PECS block might improve pain management. Thus, in patients undergoing MRM, this study was performed to compare the analgesic efficacy and safety of ultrasound-guided SAPB plus PECS II block versus SAPB alone.
2. Subjects and methods
This randomized, double-blinded comparative study was conducted at the National Cancer Institute, Cairo University, and the Surgery Department of Kasr Alainy after approval of the scientific committee of Kasr Alainy, Cairo University (MS-201-2021). The study was registered at Clinicaltrials.gov (ID NCT05006612). The study included 60 adult female patients scheduled for modified radical mastectomy under general anesthesia. Informed consent to participate in the study was acquired.
Ages 18 to 65, ASA classes II and III, and body mass index (BMI) of 20 to 35 kg/m2 were the inclusion criteria. Excluded from the trial were patients with severe liver or renal diseases, pre-existing peripheral neuropathy, coagulopathy, respiratory or cardiac problems, history of psychological disorders or chronic pain, local sepsis, and sensitivity to or contraindication to the study’s drug(s).
Using computer-generated random numbers contained in opaque, closed envelopes, the patients were divided into two equal groups at random. Randomization was carried out by an independent statistician. The assignment was not disclosed until the patient was moved to the pre-anesthetic room. The researcher who assessed postoperative pain was blinded, as was the patient.
Patients in the SAPB Group (n = 30) underwent ultrasound-guided SAPB using 30 ml levobupivacaine 0.25% injection. Patients in the Combined Group (n = 30) underwent a PECS II block using 10 ml levobupivacaine 0.25% between the two pectoralis muscles, together with SAPB with an injection of 20 ml levobupivacaine 0.25%. After that, the probe was directed toward the axilla, and 10 ml of 0.25% levobupivacaine was injected above the serratus anterior muscle (SAM), located above the third and fourth ribs. Both blocks were performed after induction of general anesthesia, and surgery started 20 minutes after the block.
2.1. General anesthesia
Thirty minutes before surgery, all patients received intravenous midazolam (0.01–0.02 mg/kg) as a premedication. Throughout the surgical process, all patients were continually monitored with end-tidal CO2, peripheral O2 saturation, non-invasive blood pressure, and electrocardiography. A combination of 2 μg/kg fentanyl, 2–3 mg/kg propofol, and 1.5 mg/kg lidocaine was used to induce general anesthesia. A 0.5 mg/kg of rocuronium was used to ease endotracheal intubation. Sevoflurane 2–2.5% inhalation in oxygen-enriched air (FiO2 = 0.5) was used to maintain anesthesia. Every half an hour, maintenance doses of 0.1 mg/kg rocuronium were given. As part of multimodal analgesia, 1 gm of paracetamol and 30 mg of intravenous ketorolac were administered. If the heart rate (HR) or mean arterial blood pressure (MAP) increased above 20% of baseline, rescue analgesia (fentanyl 1 μg/kg) was administered. To restore fluid deficit and losses, and for maintenance of fluids balance, Ringer acetate was infused. The patients also had mechanical ventilation with suitable settings to maintain end-tidal CO2 at 30–35 mmHg.
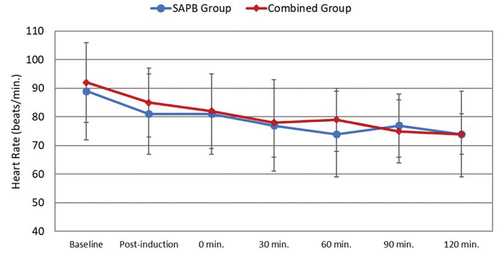
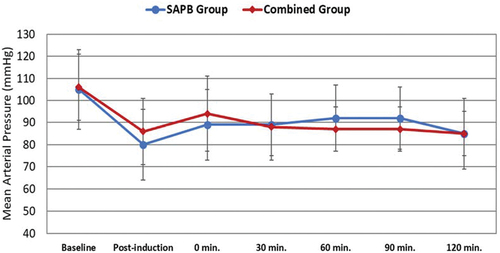
A baseline reading of MAP and HR was obtained before inducing general anesthesia. A second reading was obtained before the surgical incision (T0), and at 30-minute intervals thereafter. Hypotension, i.e., reduction >20% of baseline reading, was treated with incremental doses of 0.9% normal saline or 5 mg ephedrine to keep MAP >70 mmHg. The remaining neuromuscular blockade was reversed with 0.05 mg/kg neostigmine and 0.02 mg/kg atropine. After the airway reflexes were recovered completely, the patient was extubated.
2.2. Serratus anterior plane block technique
The block was performed in completely aseptic conditions with the patient in the lateral decubitus position with arm abduction. A linear transducer (6–13 MHz) tuned for small pieces and a depth of 1–4 cm was used. The ultrasonography probe was placed at the level of the fifth rib in the transverse plane, midaxillary line, with the indicator facing the left of the operator. Once the rib, pleural line, SAM, and latissimus dorsi muscle were visible, a 38-mm, 22-gauge regional block needle was inserted in-plane at an approximate 45-degree angle towards the fifth rib (). After aspiration, 30 ml of levobupivacaine 0.25% was injected anterior to the ribs and deep to the SAM.
2.3. Combined serratus anterior plane and modified pectoral nerve blocks technique
A Fujifilm Sonosite M-Turbo ultrasound system was used. SAPB with 20 ml levobupivacaine 0.25% was done as shown before. The patient underwent a PECS II block in the supine position, with the ipsilateral upper limb abducted 90 degrees below the lateral third of the clavicle. The ultrasound probe was turned inferolaterally after identifying the axillary vessels to locate the SAM and pectoralis muscles in the same plane. Ten milliliters of levobupivacaine 0.25% was injected into the space between the two pectoralis muscles (). Subsequently, the probe was angled in the direction of the axilla, and 10 milliliters of 0.25% levobupivacaine were injected above the SAM.
To exclude accidental pneumothorax, a lung ultrasonography was done after blocks. A Numeric Rating Scale (NRS) was used to rate the intensity of pain, and the patients were taught how to report pain (0 being “no pain” and 10 being “worst possible pain”).
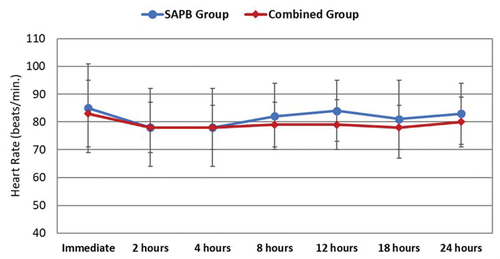
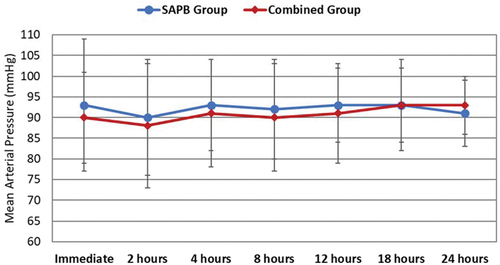
After being moved to the post-anesthesia care unit (PACU), the patients’ NRS score, MAP, and HR were recorded as soon as they arrived and then every two hours until they were moved to the ward. If the NRS scored 4 or higher, rescue analgesia in the form of IV morphine 3 mg boluses was given. The total dosage of morphine administered in 24 hours was calculated. A maximum of 0.5 mg/kg/24 hours was permitted. IV paracetamol 1 gm/6 hours and IV ketorolac 30 mg/8 hours were given as a part of multimodal analgesia. Side effects including respiratory depression (respiratory rate < 10/minute), nausea, vomiting, drowsiness, hallucinations, or nightmares were recorded. Sedation was evaluated using Ramsay scores. A score of 1 indicates inadequate sedation, a score of 2–4 indicates adequate sedation that requires surveillance, and a score of 5–6 indicates excessive sedation level.
The total amount of morphine taken in the 24 hours following surgery served as the primary outcome measure. The total amount of intraoperative fentanyl used, changes in the HR and MAP during and after the procedure, postoperative pain scores, side effects, and problems linked to the block were the secondary endpoints. Postoperative nausea and vomiting (PONV) was defined as mild if it does not request pharmacological rescue, and moderate if it does.
2.4. Statistical analysis
SPSS version 23.0 was used in data management and data analysis. Numerical variables were tested for normality in both study groups, and if so, a t-test was used to compare the means of independent groups. If the variable distribution was not normal, the Mann-Whitney test was used. Categorical outcomes were compared by Chi-square or Fisher exact. A two-tailed p-value was considered significant at 0.05 level.
3. Results
Eleven patients did not match the inclusion criteria, and five patients declined to participate in the trial out of the 76 individuals evaluated for eligibility. The remaining 60 patients were randomly assigned to the study groups, and all were statistically analyzed (). Age, weight, and ASA class were similar across the two groups ().
Table 1. Baseline characteristics of the two studied groups.
demonstrates that the Combined group’s intraoperative fentanyl use was significantly lower than the SAPB group’s (p = 0.024). The duration of analgesia did not differ significantly between the two groups (p = 0.454). In comparison to the SAPB group, the Combined group’s total postoperative morphine use during the first 24 hours was significantly lower (p = 0.005). Throughout the postoperative period, patients who received both PECS and SAPB demonstrated significantly lower NRS values during movement and at rest as compared to the SABP group (). show the intra- and postoperative changes of HR and MAP in the two groups. All readings were within the clinically acceptable ranges.
Table 2. Analgesic profile of the two studied groups.
Table 3. Postoperative numerical rating scale score at rest in the two groups.
Table 4. Postoperative numerical rating scale score during movement in the two groups.
Mild to moderate PONV was observed in the two groups, with no statistically significant difference. There were no significant opioid-related complications in both groups; however, five patients in the SABP group developed intramuscular hematoma as observed intraoperatively ().
Table 5. Adverse events between both groups.
4. Discussion
The axillary lymph nodes, which involve a broad area, the pectoralis minor muscle, and the entire breast are removed in MRM. Therefore, a large number of nerves require blocking for effective regional analgesia. These comprise the intercostobrachial and long thoracic nerves that innervate the axillary region, the medial and lateral thoracic and supraclavicular nerves, and the anterior and lateral cutaneous branches of the intercostal nerves [Citation13]. To lower the risk of residual disease, excision of the pectoralis fascia (PF) has long been a part of the standard management of MRM [Citation14].
SAPB primarily impacts the lateral cutaneous branches of the intercostal nerves, as well as the long thoracic, intercostobrachial, thoracic intercostal, and thoracodorsal nerves. As a result, it can offer pain relief to the front and sides of the thoracic wall, i.e., the dermatomes T2 to T9 [Citation15]. The anteromedial chest wall is innervated by the anterior branches of the intercostal nerves, hence it is unlikely that SAPB would adequately cover this area [Citation16]. Achieving regional analgesia alone with SAPB is appropriate for most anterolateral breast surgeries. In the event that medial breast surgery is necessary, the analgesic regimen may include an anterior cutaneous branch of the intercostal nerve to enhance medial pain alleviation [Citation17].
Patients with breast cancer undergoing MRM may benefit from deep SAPB. However, if the pectoral muscles are involved in the surgery, a combination of a pectoral nerve block and SAPB can provide sufficient regional analgesia. This was the main idea of the present trial. The injection of the LA into three fascial planes – between the pectoralis major and minor, between the pectoralis minor and SAM, and deep to the latter – is ensured by the combination of deep SAPB and PECS II block. It is possible to think of it as a hybrid of the deep and superficial forms of SAPB.
In comparison to SAPB alone, the current investigation showed that the combined deep SAPB and PECS II block had a superior analgesic profile. The combined group’s intraoperative fentanyl usage and postoperative morphine consumption were both significantly less than those of the SAPB group. Additionally, compared to the SAPB group, the combined group’s pain levels were much lower both at rest and during movement. The duration of analgesia, however, was similar for both. Blocking the complicated innervation of the breast appears to be responsible for the combined technique’s superiority. Apart from the intercostal nerves that come from the thoracic area, the brachial plexus is the source of the pectoral and long thoracic nerves. The intercostobrachial nerve innervates the lateral portion of the axillar [Citation18]. Furthermore, the long thoracic nerve, which is superficial to the SAM, is guaranteed to be blocked by LA injection, both superficially and deeply to the SAM in the recommended combination method. You can’t do this with just deep SAPB.
To the authors’ knowledge, it is the first time that these two interfascial plane blocks have been combined. As a matter of fact, the two blocks are closely related, with the SAPB being a development of Blanco’s PECS block concept. The SAPB is a variant of PECS II blockade through injecting the LA into the plane deep to the pectoralis minor and superficial to the SAM [Citation19]. This was further modified depending on the injection site, whether superficial or deep to the SAM. The literature included studies comparing the two procedures with other analgesic strategies for breast surgery, despite the lack of trials combining them.
Two different meta-analyses of randomized controlled trials (RCTs) comparing the PECS II block with either systemic analgesia alone or thoracic paravertebral blockade (TPVB) in breast surgery came to similar conclusions [Citation20,Citation21]. A comparable decrease in pain ratings and 24-hour opioid usage was observed with PECS II and TPVB. PECS II block dramatically reduced pain scores and postoperative opioid use compared to systemic analgesia. To investigate the relevance of PECS block in relation to mastectomy patients, three more meta-analyses have been carried out. Systemic analgesia was compared with PECS I or PECS II blocks in two investigations. With only slight reductions in postoperative pain scores, the data showed that PECS blocks significantly decreased postoperative opioid usage [Citation22,Citation23]. The third study reported comparable analgesic effects with a PECS II block or SAPB compared to TPVB [Citation24].
A recent meta-analysis reviewed 19 RCTs that compared SAPB with TPVB in breast and thoracic surgery [Citation25]. Pain scores were substantially reduced when a SAPB was implemented. Superficial versus deep blocks revealed comparable magnitudes of effect. Furthermore, SAPB was correlated with reduced opioid consumption and a longer analgesic duration.
5. Conclusion
According to the findings of this double-blind, randomized trial, ultrasound-guided PECS II block in conjunction with SAPB offers more efficient analgesia in MRM than SAPB alone. Adopting the combination strategy resulted in reduced postoperative pain intensity, less intraoperative fentanyl consumption, and less postoperative morphine consumption. The SAPB and PECS II block combination was hemodynamically safe with few trivial adverse effects.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–249. doi: 10.3322/caac.21660
- Qiu H, Xu WH, Kong J, et al. Effect of breast-conserving surgery and modified radical mastectomy on operation index, symptom checklist-90 score and prognosis in patients with early breast cancer. Med. 2020;99(11):e19279. doi: 10.1097/MD.0000000000019279
- Gupta K, Srikanth K, Girdhar KK, et al. Analgesic efficacy of ultrasound-guided paravertebral block versus serratus plane block for modified radical mastectomy: a randomised, controlled trial. Indian J Anaesth. 2017;61(5):381–386. doi: 10.4103/ija.IJA_62_17
- Plesca M, Bordea C, El Houcheimi B, et al. Evolution of radical mastectomy for breast cancer. J Med Life. 2016;9(2):183–186.
- Shamim Seth U, Perveen S, Ahmed T, Kamal MT, Soomro JA, Murtaza Khomusi M, et al. Postoperative analgesia in modified radical mastectomy patients after instillation of bupivacaine through surgical drains. Cureus. 2024;14:e24125.
- Sansone P, Giaccari LG, Faenza M, et al. What is the role of locoregional anesthesia in breast surgery? A systematic literature review focused on pain intensity, opioid consumption, adverse events, and patient satisfaction. BMC Anesthesiol. 2020;20(1):290. doi: 10.1186/s12871-020-01206-4
- Rivedal DD, Nayar HS, Israel JS, et al. Paravertebral block associated with decreased opioid use and less nausea and vomiting after reduction mammaplasty. J Surg Res. 2018;228:307–313. doi: 10.1016/j.jss.2018.03.018
- Chou R, Gordon DB, de Leon-Casasola OA, et al. Management of postoperative pain: a clinical practice guideline from the American pain society, the American society of regional Anesthesia and pain medicine, and the American society of anesthesiologists’ committee on regional anesthesia, executive committee, and Administrative council. J Pain. 2016;17(2):131–157. doi: 10.1016/j.jpain.2015.12.008
- Wick EC, Grant MC, Wu CL. Postoperative multimodal analgesia pain management with nonopioid analgesics and techniques: a review. JAMA Surg. 2017;152(7):691–697. doi: 10.1001/jamasurg.2017.0898
- Zocca JA, Chen GH, Puttanniah VG, et al. Ultrasound-guided serratus plane block for treatment of postmastectomy pain syndromes in breast cancer patients: a case series. Pain Pract. 2017;17(1):141–146. doi: 10.1111/papr.12482
- Kuthiala G, Chaudhary G. Ropivacaine: a review of its pharmacology and clinical use. Indian J Anaesth. 2011;55(2):104–110. doi: 10.4103/0019-5049.79875
- Deng W, Fu D, He L. Evaluation of pectoral nerve block in modified radical mastectomy: comparison of three concentrations of ropivacaine. Clin Interv Aging. 2020;15:937–944. doi: 10.2147/CIA.S251613
- Loukas M, Tubbs RS, Mirzayan N, et al. The history of mastectomy. Am Surg. 2011;77(5):566–571. doi: 10.1177/000313481107700515
- Vallejo da Silva A, Rodriguez FR, Loures CM, et al. Mastectomy in the era of implant-based reconstruction: should we be removing the pectoralis fascia? Breast. 2012;21(6):779–780. doi: 10.1016/j.breast.2012.07.011
- de la Torre PA, García PD, Alvarez SL, et al. A novel ultrasound-guided block: a promising alternative for breast analgesia. Aesthet Surg J. 2014;34(1):198–200. doi: 10.1177/1090820X13515902
- Chin KJ. An anatomical basis for naming plane blocks of the anteromedial chest wall. Reg Anesth Pain Med. 2017;42(3):414–415. doi: 10.1097/AAP.0000000000000575
- Sherwin A, Buggy DJ. Anaesthesia for breast surgery. BJA Educ. 2018;18(11):342–348. doi: 10.1016/j.bjae.2018.08.002
- Sarhadi NS, Shaw Dunn J, Lee FD, et al. An anatomical study of the nerve supply of the breast, including the nipple and areola. Br J Plast Surg. 1996;49(3):156–164. doi: 10.1016/S0007-1226(96)90218-0
- Blanco R, Parras T, McDonnell JG, et al. Serratus plane block: a novel ultrasound-guided thoracic wall nerve block. Anaesthesia. 2013;68(11):1107–1113. doi: 10.1111/anae.12344
- Hussain N, Brull R, McCartney CJL, et al. Pectoralis-II myofascial block and analgesia in breast cancer surgery: a systematic review and meta-analysis. Anesthesiol. 2019;131(3):630–648. doi: 10.1097/ALN.0000000000002822
- Versyck B, van Geffen GJ, Chin KJ. Analgesic efficacy of the pecs II block: a systematic review and meta-analysis. Anaesthesia. 2019;74(5):663–673. doi: 10.1111/anae.14607
- Zhao J, Han F, Yang Y, et al. Pectoral nerve block in anesthesia for modified radical mastectomy: a meta-analysis based on randomized controlled trials. Medicine (Baltimore). 2019;98(18):e15423. doi: 10.1097/MD.0000000000015423
- Lovett-Carter D, Kendall MC, McCormick ZL, et al. Pectoral nerve blocks and postoperative pain outcomes after mastectomy: a meta-analysis of randomized controlled trials. Reg Anesth Pain Med. 2019;44(10):923–928. doi: 10.1136/rapm-2019-100658
- Grape S, El-Boghdadly K, Albrecht E. Analgesic efficacy of PECS vs paravertebral blocks after radical mastectomy: a systematic review, meta-analysis and trial sequential analysis. J Clin Anesth. 2020;63:109745. doi: 10.1016/j.jclinane.2020.109745
- Chong M, Berbenetz N, Kumar K, et al. The serratus plane block for postoperative analgesia in breast and thoracic surgery: a systematic review and meta-analysis. Reg Anesth Pain Med. 2019:rapm–100982. doi: 10.1136/rapm-2019-100982