ABSTRACT
Background
The current study compared the effect of ultrasound-guided quadratus lumborum block (QLB) to transversus abdominis plane block (TAPB) on post-operative pain in children undergoing lower abdominal laparoscopy.
Methods
Ninety male and female patients (ASA I to II), ages (1–7), performing elective laparoscopic lower abdomen surgery randomly allocated into three equal groups of 30 patients each. Group (C) received conventional analgesics. In addition to conventional analgesics, 0.5 ml/kg of bupivacaine 0.25% was injected under US-guidance on both abdominal sides, into transversal plane at subcostal level in group (TAP) or into the facial plane between the PM and QL muscles in group (QL). Our primary outcome was the measuring FLACC scale immediately following surgery, every 30 minutes in the PACU, and then at 4, 6, 8, 10, 12, 18, and 24 hours after surgery. Our secondary outcomes were the first analgesic request, the dosage of analgesics, the postoperative complications, and parents’ satisfaction during the first 24 hours.
Results
When comparing the FLACC pain scores, the QL group showed a significant reduction in pain for the whole postoperative period in comparison to C group (p < 0.001) and up to 12 h in TAP group (p < 0.001). Patients in QL group got the longest time to the first analgesic requirement (p < 0.001). The C group required more analgesics overall than the other groups.
Conclusions
Ultrasound-guided QLB after induction of general anesthesia in comparison to TAP block provides better postoperative pain, prolonged analgesia, and less postoperative analgesic consumption after lower abdominal laparoscopic surgery in pediatrics.
1. Introduction
The severity of children’s pain following abdominal procedures varies during the perioperative period; therefore, effective, and long-lasting analgesia is necessary to ensure satisfied parents and happy children. After abdominal procedures, systemic opioid analgesia techniques are frequently employed to treat pain; nevertheless, opioid use is commonly linked to issues like respiratory depression, nausea, and vomiting [Citation1]. For pain management, a central neuraxial block is highly recommended technique [Citation2], however, in some circumstances, it may be contraindicated (e.g., congenital spinal abnormalities, bacteremia, spine surgeries, and coagulopathy) [Citation3]. The novel Ultrasound-guided (US-guided) technology provides better understanding of abdominal wall anatomy and enhancing different interfascial abdominal plane blocks. The TAPB and QLB were developed as localized anesthetic treatments to relieve pain following abdominal surgery [Citation4,Citation5]. These blocks are commonly utilized for postoperative analgesia in abdominal surgery due to their efficacious nature as components of multimode analgesia. There are several meta-analyses available [Citation6–9].
Rafi presented the method for the first time in 2001, and Mc. Donnell expanded on it [Citation10,Citation11]. By administering local anesthetics to anesthetize the nerves supplying the anterior abdominal wall (T6 to L1) [Citation12], TAPB can inhibit the nerve signal and reduce pain during abdominal procedures [Citation11,Citation13]. So, several pediatric studies used TAPB, in order to lower the postoperative pain severity and the need for opioids following major abdominal procedures [Citation3,Citation14,Citation15]. Different studies estimate that pediatric patients’ postoperative analgesia with TAPB lasts for 15 to 24 hours. The risks of TAPB complications are low, particularly when the procedure is carried out under direct ultrasound imaging, and they don’t need to be followed up on with further treatments [Citation16,Citation17].
The QLB is a posterior abdominal trunk block that occupies the thoracic paravertebral area and thoracolumbar fascia with a local anesthetic to generate analgesic effects. There are three QLB techniques: anterior, posterior, and anterolateral, depending on the injection position and method. It has been proposed that the QL block, a localized version of the TAP block, is a more dependable method for treating pain following abdominal surgery than TAP blocks. Compared to TAP blocks, QL blocks cause more widespread sensory blockages [Citation18,Citation19].
The current study compared the effect of US-guided quadratus lumborum block (QLB) to transversus abdominis plane block (TAPB) on post-operative pain in children undergoing laparoscopic lower abdominal surgeries.
2. Patients and methods
Following permission from El-Minia University Hospital’s Ethics Committee (Protocol ID: 271:7/2019) and ClinicalTrials.gov registration (ID: NCT04552548). Written informed consent was taken from the parents of each patient after explanation of surgical procedure and potential risk and benefit of general anesthesia with regional anesthetic procedure.
In this prospective randomized double-blind trial, 90 children, ASA I and II, of both genders, aged 1 to 7, who underwent elective lower abdominal laparoscopic surgery under general anesthesia (between 1 October 2019, and 1 December 2020) were allocated.
Exclusion criteria: Hepatic disease, bleeding issues, infection at site of the regional anesthetic block, signs of peritonitis, history of significant cardiac disease, uncontrolled seizures, and their parents refusing the regional block.
After obtaining a medical history from the parents regarding any medical issues that had arisen for their siblings, all children underwent laboratory investigations those included: liver function tests, prothrombin time and concentration, bleeding time, clotting time, and complete blood count.
Prior to the study, the sample size was calculated. Based on data from the pilot study, a power calculation was used to determine the number of patients needed in each group. In the present study, the mean of the FLACC scale after 24 hours in the TAP group was 6.4 ± 1.07, in the QL group it was 6.5 ± 0.53, and, in the C group it was 7 ± 0.85. A sample size of 30 patients in each group was determined to provide 80% power for the One-Way ANOVA test at the level of 0.05 significance using G Power 3.1 9.2 software.
Using computer-generated table numbers, the patients were randomly divided into three groups, 30 patients each; control group (C group); QLB group (QL group) and TABB group (TAP group). The parents were not informed of the patients’ group assignment. Postoperative evaluations were performed by a separate anesthesiologist who was not informed of group assignment.
All the patients received conventional analgesics (1 μg/kg fentanyl with induction and 15 mg/kg paracetamol with 0.5 mg/kg ketorolac as iv infusion before extubation). The TAP group was given a bilateral TAPB using 0.5 ml/kg of 0.25% bupivacaine while bilateral QLB with 0.5 ml/kg bupivacaine 0.25% was administered to the QL group.
Standard peri-operative monitoring was attached to each patient those included continuous electrocardiogram and arterial blood pressure monitoring (non-invasive), end-tidal carbon dioxide, and oxygen saturation (SpO2). After sevoflurane inhalation induces anesthesia, an intravenous line is inserted. All the children received premedication with atropine (0.01–0.02 mg/kg), followed by atracurium (0.5 mg/kg) to aid in the process of endotracheal intubation. Anesthetic maintenance was achieved with isoflurane and atracurium at a dose of 0.1 mg/kg. Heart rate (HR) and mean arterial pressure (MAP) recorded before and immediately after induction of anesthesia and at 5, 10, 15, 20, 30, and then every 15 minutes up to 120 minutes postoperatively.
Using an ultrasound device, (SONOSITE NANOMAX; the linear 25N multi-frequency 13–6 MHz transducer served as the scanning probe), an US-guided TAPB or QLB was carried out after induction of general anesthesia and prior to surgical incision.
2.1. TAP block procedure
The block was performed in a supine position behind the midaxillary line laterally, between the iliac crest and the most inferior part of the ribs. The TAPB was executed under ultrasound guidance using a 25-G, 90-mm spinal needle. After disinfecting the skin and visualizing the entire needle using an “in-plane” approach, the tip of the needle was inserted into the space between the transversus abdominis muscle and the internal oblique abdominal muscle. Following negative aspiration, bupivacaine 0.5 ml/kg bupivacaine 0.25% was injected. When an echolucent lens shape developed in the space between the two muscles, the injection was deemed successful, and the other side was likewise injected in the same manner [Citation20] ().
2.2. QL block procedure
Using ultrasound guidance, a bilateral transmuscular quadratus lumborum (TQL) block was performed in a lateral position, with the side to be blocked kept up throughout the procedure. The transverse plane was used to put the probe in the midaxillary line, a little above the iliac crest. It then slid dorsally until the Shamrock sign was observed. In the “Shamrock sign,” the psoas major (PM) muscle forms the anterior leaf, the erector spinae muscles form the posterior leaf, and the QL muscle appears as the superior leaf of the Shamrock at the apex of the L4 transverse process. The transverse process symbolizes the stem that joins the three leaves. The spinal needle was introduced via the QL muscle into the facial plane between the PM and QL muscles, starting from the posterior end of the probe. The medicine was injected after the needle’s proper placement was verified. Similar injections were likewise made to the other side [Citation21] ().
In the control group, the surgical operation was initiated immediately, or 15 minutes after the nerve block in the other groups. Using CO2 insufflation, the pneumoperitoneum was kept at a pressure of 8–12 mm Hg and a flow rate of 0.5 L/min. When there was substantial movement or a change in heart rate and/or blood pressure of more than 20% of the basal values and the symptoms persisted for more than a minute following the skin incision, the block was deemed unsuccessful and the patient was excluded from the study.
At the end of the surgery, all children received 15 mg/kg of paracetamol by infusion and an intravenous infusion of ketorolac at a dosage of 0.5 mg/kg. Then, isoflurane was discontinued, and reversal of muscle relaxant was done using atropine (0.01 mg/kg) and neostigmine in a dose of 0.05 mg/kg, gentle suctioning, and when the patient fulfilled the criteria of extubation, an endotracheal tube was removed. Patients were then taken to the post-anesthesia care unit (PACU), where observation was carried out for a minimum period of 120 minutes.
Our primary outcome was the postoperative pain intensity which was evaluated using the face, leg, activity, cry, and consolability scale (FLACC scale) [Citation22]. It was measured immediately following surgery, every 30 minutes in the PACU, and then at 4, 6, 8, 10, 12, 18, and 24 hours after surgery. The total score of 0–10 is obtained by assigning a 0–2 scale for the five categories, where 0 indicates feeling at comfort and happiness, 1–3 denotes mild discomfort, 4–6 denotes pain that is moderate, and 7–10 signifies extreme pain, discomfort, or both [Citation22].
From the moment of surgery to the FLACC score of >4, we tracked our secondary outcomes, such as the length of time until the first analgesic requirement. Rescue analgesia was involved 15 mg/kg IV paracetamol (perfalgan), with a record of the entire paracetamol dosage. A 0.5 mg/kg intravenous infusion of ketorolac was given to individuals whose score was still ≥4, and a record of how many patients needed ketorolac during the first 24 hours would be kept. We also noted that the frequency of complications was noted. These included damage to the underlying structures, hematoma formation, postoperative nausea, and vomiting (PONV), and hemodynamic instability, which is defined as a drop in MAP or HR of more than 20% of the baseline value. A 5-point rating system [Citation23], with 1 denoting total dissatisfaction, 2 dissatisfaction, 3 neither satisfaction nor dissatisfaction, 4 satisfied, and 5 complete satisfaction, was used to evaluate parents’ level of satisfaction.
After the data was extracted and modified, with the IBM SPSS 20.0 statistical software, a statistical analysis was carried out. The data were expressed as mean ± SD, minimum and maximum range for quantitative parametric measures, or median and interquartile range (IQR) for quantitative non-parametric measures, data were further given as numbers and percentages for those that were categorized. The Kruskal–Walli test and the Mann–Whitney test were used to compare non-parametric quantitative data; the Chi-square test or Fisher’s exact test was used to compare categorical variables; and the analysis of variance. (ANOVA) was used to compare parametric data between independent groups. The intergroup differences were assessed using the LSD post hoc test. Within each group, the paired sample t-test was applied to quantitative parametric data, while for non-parametric quantitative data; the Wilcoxon signed rank test was applied. The P-values below 0.05 were considered statistically significant.
3. Results
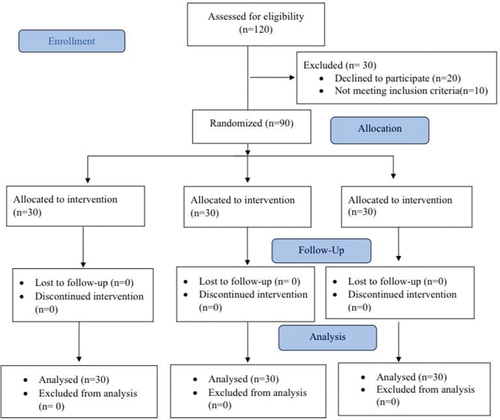
The patient’s enrollment is in ().
indicates that the patient characteristics of the analyzed groups were comparable. These variables included age, sex, weight, ASA classification, and length of operation.
Table 1. Patient’s data.
Regarding the face, legs, activity, cry, and consolability (FLACC scale), the QL Group had significantly lower FLACC scale (p < 0.001) at most of the time points postoperatively when compared to the C group. Whereas, when comparing the FLACC scale in TAP group with C group we found that it was significantly reduced in TAP up to 6 h postoperatively (p < 0.001), and also after 8 h (p = 0.003), while after 18 h it was p < 0.001. Also, when comparing the QL group with the TAP group, the QL group had a significantly lower FLACC scale p < 0.001 until 12 h postoperatively ().
Table 2. Pain score (FLAAC scale).
Throughout the study period, all three groups maintained a condition of hemodynamic stability, despite occasional statistically significant changes within or between the groups that had no effect on clinical stability and didn’t require intervention ().
Table 3. Heart rate (beat/min) in the three studied groups.
Table 4. Mean arterial pressure (mmHg) in the three studied groups.
There was a significant difference in the duration between the study groups before the need for analgesic medication; the QL group had a longer time, with a mean value of 19 ± 2.9 hours. The TAP group had a lower time, with a mean value of 14.5 ± 2.2 hours, as compared to the QL group. With a mean value of (4.8 ± 0.7 hours), the C group displayed the lowest of all ().
Table 5. Postoperative analgesic requirements.
The total paracetamol dosages (mg/kg) for the three groups varied considerably from one another. The QL group used less paracetamol than the TAP group (p = 0.013) and control group (p < 0.001), while the TAP group used less paracetamol than the control group (p < 0.001).
The frequencies of postoperative paracetamol administration in the first 24 were (3 ± 0), (1.9 ± 0.6), and (1.1 ± 0.5) in the C group, TAP group, and, QL group, respectively, with p < 0.001 indicating a significant difference between the three groups. The number of patients requiring ketorolac was significantly higher in the C group compared to the TAP and QL groups (p < 0.001 and p < 0.0001, respectively) ().
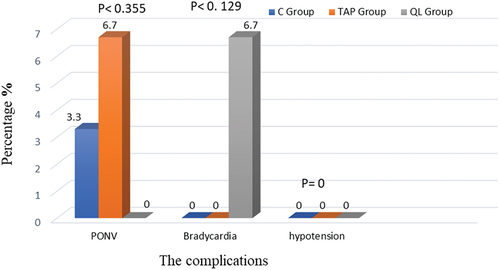
Regarding postoperative complications like nausea and vomiting, no statistically significant difference was found between the three research groups (p = 0.355); however, two patients in the TAP group and one patient in the C group reported having these symptoms. Furthermore, the TAP group did not have any patients complaining of hypotension or other issues, and only two patients were discovered to have bradycardia, which was addressed without the need for additional intervention (p = 0.129) ().
Figure 4. The complications.
As shown in , the QL and TAP groups had higher parent satisfaction than the control group, but there was no statistically significant difference between the two groups.
Table 6. Parent satisfaction with post-operative analgesia.
4. Discussion
This prospective, observer and parent blinded, randomized controlled trial included children undergoing lower abdomen laparoscopic procedures under general anaesthesia in order to compare QLB with TAPB for prophylactic analgesia.
Previous studies have demonstrated the safety and effectiveness of TAP and QL blocks in the treatment of postoperative pain after abdominal surgery [Citation24–27]. The use of QLB in this trial resulted in a statistically significant reduction in pain scores. At most postoperative time periods, it was significantly lower in the QL and TAP groups compared to the C group. When compared to the TAP group, the pain scores was likewise lower in the QL group for the first 12 hours after, but it was the same at all other intervals. Compared to the TAP group, the QL group exhibited a longer time for the first analgesic needed, and the control group showed the least amount of time. After surgery, the QL group used fewer analgesics than the TAP group and the control group.
The groups’ complications did not significantly differ from one another. In comparison to the control group, the parents in the QL and TAP groups expressed more satisfaction, indicating a substantial difference in parent satisfaction.
Because TAPB effectively relieves pain during abdominal surgical operations, it has established itself as a crucial part of multimodal analgesia approaches. The TAP block inhibits nerve conduction from the anterior abdominal wall originating from the subcostal, intercostal, and first lumbar (T6-L1) nerves, hence producing analgesia, and only somatic discomfort is alleviated [Citation3]. Even after surgery, there will still be diffuse visceral pain (from spasms or inflammation). However, it may not adequately cover the visceral pain, especially after large, significant abdominal procedures [Citation28]. So, TAP block is still not commonly utilized in modern therapy, and the outcomes for pediatric groups are still variable [Citation29].
Both children [Citation30] and adults [Citation31] who have had abdominal surgery can benefit from quadratus lumborum block for postoperative pain because it could cover the visceral pain. The actual mechanism underlying QLB’s visceral analgesic effects is yet unresolved. Some of the analgesia was reported to be caused by the local anesthetics that spread into the paravertebral space along the thoracolumbar fascia and the endothoracic fascia [Citation32–34]. On the other hand, another article in cadavers demonstrates that visceral analgesia in QLB arises from anesthetics spreading to the sympathetic trunk or celiac ganglia through splanchnic nerves [Citation35].
Our results align with those of Oksuz et al. [Citation9], who scheduled 50 children to undergo unilateral lower abdominal surgeries. They conducted all the blocks in their study under general anesthesia prior to surgery. They discovered that children with QLB scored lower on pain scales than those with TAPB (p < 0.05), and the QLB group’s parent satisfaction ratings were greater.
Our results agree with those of Baidya et al. [Citation30], who observed that the transmuscular QL block in pediatrics undergoing pyeloplasty was believed to be associated with effective postoperative analgesia. A 7-year-old girl child undergoing a laparoscopic appendicectomy was given a bilateral QL intramuscular block by Murouchi [Citation31], who found that the postoperative analgesia suited the patient and her mother with no apparent anesthetic-related complications. Also, other studies that evaluated and compared the effects of both methods of block in adults after cesarean sections [Citation36,Citation37] or after abdominal hysterectomy [Citation38] detected that, compared to TAPB, QLB resulted in much lower pain scores, a longer duration of analgesia, fewer opioid consumptions, and a wider distribution of analgesia.
Moreover, there were two meta-analyses, one on eight studies [Citation19] and the other on twenty-two studies [Citation39] with adult patients, to determine the effects of TAPB vs. QLB on postoperative analgesia. They found that the QL group’s postoperative pain scores were considerably lower than those of the TAP group. Also, in comparison to the TAP group, the QL group used less morphine after surgery, and they experienced postoperative analgesia for a longer period than the TAP group. Furthermore, there were no variations in postoperative complications related to the two methods [Citation19].
The Sato study [Citation40] and Alansary study [Citation41], respectively, they compared in their studies, the effect of caudal block vs. QLB in postoperative analgesia, and they reported comparable outcomes; as the QLB was superior to caudal in lowering the requirement for opioid-based rescue analgesia in the first 24 hours of the procedure, compared to the caudal group, the QLB group had a significantly greater mean time to first analgesic requirement. In a 2018 study, Kumar et al. [Citation42] assessed the length of analgesia following lower abdominal procedures utilizing the QL block and the TAP block using 0.25% ropivacaine. They found that, compared to the TAP block, the analgesia caused by the QL block remained noticeably longer. Even though we utilized 0.25% bupivacaine, this result was consistent with our study.
However, Blanco et al. [Citation43] found that, compared to the TAP block, the analgesia caused by the QL block remained noticeably longer. Zhu et al. [Citation44] showed that after 4 and 8 hours after total abdominal hysterectomy surgery, the pain scores of patients receiving QL blocks and TAP blocks did not differ from one another. Also, İpek et al. [Citation45] found that the perioperative analgesic treatments (QLB, caudal analgesia, and ultrasound-guided TAP block) used on pediatric patients undergoing open lower abdomen surgery had variable outcomes. The QLB was associated in their study with lower postoperative pain scores and shorter hospital stays, even though there was no statistically significant difference between the groups in terms of the number of patients requiring analgesia within the first 24 hours after surgery or the time to the first analgesic requirement. The difference in QLB technique (lateral approach) compared to transmuscular in our study and the fact that we conducted our research on laparoscopic rather than open surgery could be the reason for the divergence between our results and those of these studies.
There aren’t many publications in the literature on QLB-related side effects, such as organ damage, retroperitoneal hematoma, and local anesthetic toxicity. Hemodynamics, however, needs to be closely watched since local anesthetics can migrate to the paravertebral space and lower blood pressure and heart rate [Citation46]. According to one case report, quadriceps weakness brought on by femoral block vanished after 18 hours [Citation47]. There were no documented block administration-related issues in the current study, noteworthy alterations in hemodynamics and no patients in the QLB group showed signs of quadriceps muscle weakness. Few individuals in the C group and TAP group were found to have mild PONV, and just two patients in the TAP group were found to have bradycardia, which was managed without the need for additional treatment. The study’s small sample size could be the cause of these results, and a larger sample size and a more thorough investigation are required.
However, there are certain limitations with this study. First, because the current study focused on administering blocks to pediatric patients after general anesthesia, we were unable to look for dermatomal levels in either group. Second, the fact that this study’s QL block only used one approach made it difficult to determine whether other QL block approaches could produce comparable outcomes. Finally, one potential weakness of the current study is that the pain score evaluations were not standardized for rest or movement. In future investigations, we suggest a more advanced monitoring of chronic pain following surgery with a longer follow-up period and large sample size to assess the impact of managing postoperative pain.
We concluded that the ultra-sound guided Quadratus lumborum block provided longer and more effective postoperative analgesia compared with the transversus abdominis plane block after laparoscopic lower abdominal surgery in pediatrics, as it provided a reduced pain score, a delayed analgesic request, and a lower analgesic requirement.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Johns N, O’neill S, Ventham N, et al. Clinical effectiveness of transversus abdominis plane (TAP) block in abdominal surgery: a systematic review and meta‐analysis. Colorectal Dis. 2012;14(10):e635–e42. doi: 10.1111/j.1463-1318.2012.03104.x
- Somri M, Tome R, Yanovski B, et al. Combined spinal–epidural anesthesia in major abdominal surgery in high‐risk neonates and infants. Pediatr Anesthesia. 2007;17(11):1059–1065. doi: 10.1111/j.1460-9592.2007.02278.x
- Suresh S, Chan VW. Ultrasound guided transversus abdominis plane block in infants, children and adolescents: a simple procedural guidance for their performance. Pediatr Anesthesia. 2009;19(4):296–299. doi: 10.1111/j.1460-9592.2009.02958.x
- De Oliveira GS Jr, Castro-Alves LJ, Nader A, et al. Transversus abdominis plane block to ameliorate postoperative pain outcomes after laparoscopic surgery: a meta-analysis of randomized controlled trials. Anesthesia & Analgesia. 2014;118(2):454–463. doi: 10.1213/ANE.0000000000000066
- Gözen Ö, Mahmut A, Aykut U, et al. Comparison of quadratus lumborum block and caudal block for postoperative analgesia in pediatric patients undergoing inguinal hernia repair and orchiopexy surgeries: a randomized controlled trial. Region Anesthes Pain Med. 2020:rapm-2019–101027.
- Liu L, Xie Y-H, Zhang W, et al. Effect of transversus abdominis plane block on postoperative pain after colorectal surgery: a meta-analysis of randomized controlled trials. Med Princ Pract. 2018;27(2):158–165. doi: 10.1159/000487323
- Hain E, Maggiori L, Prost à la Denise J, et al. Transversus abdominis plane (TAP) block in laparoscopic colorectal surgery improves postoperative pain management: a meta-analysis. Colorectal Dis. 2018;20(4):279–287. doi: 10.1111/codi.14037
- Viderman D, Aubakirova M, Abdildin YG. Transversus abdominis plane block in colorectal surgery: a meta-analysis. Front Med. 2022;8:8. doi: 10.3389/fmed.2021.802039
- Öksüz G, Bilal B, Gürkan Y, et al. Quadratus lumborum block versus transversus abdominis plane block in children undergoing low abdominal surgery: a randomized controlled trial. Reg Anesth Pain Med. 2017 5;42(5):674–679. doi: 10.1097/AAP.0000000000000645
- McDonnell JG, O’Donnell BD, Farrell T, et al. Transversus abdominis plane block: a cadaveric and radiological evaluation. Reg Anesth Pain Med. 2007;32(5):399–404. doi: 10.1016/j.rapm.2007.03.011
- Rafi A. Abdominal field block: a new approach via the lumbar triangle. Anaesthes. 2001;56(10):1024–1026. doi: 10.1111/j.1365-2044.2001.2279-40.x
- Petersen PL, Mathiesen O, Torup H, et al. The transversus abdominis plane block: a valuable option for postoperative analgesia? A topical review. Acta Anaesthesiol Scand. 2010;54(5):529–535. doi: 10.1111/j.1399-6576.2010.02215.x
- Hebbard P, Fujiwara Y, Shibata Y, et al. Ultrasound-guided transversus abdominis plane (TAP) block. Anaesth Intensive Care. 2007;35(4):616–617.
- Carney J, Finnerty O, Rauf J, et al. Ipsilateral transversus abdominis plane block provides effective analgesia after appendectomy in children: a randomized controlled trial. Anesthesia & Analgesia. 2010;111(4):998–1003. doi: 10.1213/ANE.0b013e3181ee7bba
- Mai CL, Young MJ, Quraishi SA. Clinical implications of the transversus abdominis plane block in pediatric anesthesia. Pediatr Anesthesia. 2012;22(9):831–840. doi: 10.1111/j.1460-9592.2012.03916.x
- Long JB, Birmingham PK, De Oliveira GS Jr, et al. Transversus abdominis plane block in children: a multicenter safety analysis of 1994 cases from the PRAN (pediatric regional anesthesia network) database. Anesthesia & Analgesia. 2014;119(2):395–399. doi: 10.1213/ANE.0000000000000284
- Long JB, Birmingham PK, De Oliveira GS Jr, et al. Transversus abdominis plane block in children: a multicenter safety analysis of 1994 cases from the PRAN (pediatric regional anesthesia network) database. Survey Anesthesiol. 2015;59(3):139–140. doi: 10.1097/01.sa.0000464134.30246.6c
- Urits I, Ostling PS, Novitch MB, et al. Truncal regional nerve blocks in clinical anesthesia practice. Best Pract Res Clin Anaesth. 2019;33(4):559–571. doi: 10.1016/j.bpa.2019.07.013
- Liu X, Song T, Chen X, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in patients undergoing abdominal surgeries: a systematic review and meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20(1):53. doi: 10.1186/s12871-020-00967-2
- Baeriswyl M, Kirkham KR, Kern C, et al. The analgesic efficacy of ultrasound-guided transversus abdominis plane block in adult patients: a meta-analysis. Anesthes Analges. 2015;121(6):1640–1654. doi: 10.1213/ANE.0000000000000967
- Børglum J, Moriggl B, Jensen K, et al. Ultrasound-guided transmuscular quadratus lumborum blockade. Br J Anaesth. 2013;111(eLetters Supplement). doi: 10.1093/bja/el_9919
- Merkel SI, Voepel-Lewis T, Shayevitz JR. The FLACC: a behavioral scale for scoring postoperative pain in young children. Pediatr Nurs. 1997;23(3):293–297.
- Al-Sadek WM, Rizk SN, Selim MA. Ultrasound guided transversus abdominis plane block in pediatric patients undergoing laparoscopic surgery. Egypt J Anaesth. 2014;30(3):273–278. doi: 10.1016/j.egja.2014.01.011
- Makhni R, Attri JP, Kaur H, et al. Comparison of ultrasound-guided transversus abdominis plane (TAP) block and quadratus lumborum (QL) block in inguinal hernia surgery. Indian J Anaesth. 2022;66(Suppl 14):S122–S5. doi: 10.4103/ija.ija_97_22
- Anbu G, Selvaraj V. Comparison study of quadratus lumborum block versus transversus abdominis plane block for postoperative analgesia in children undergoing infra-umbilical surgeries under general anesthesia: a prospective randomised study. J Anesthes/Anestezi Dergisi (JARSS). 2024;32(1):46–52. doi: 10.54875/jarss.2024.56933
- Ipek CB, Kara D, Yilmaz S, et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. 2019;49(5):1395–1402. doi: 10.3906/sag-1812-59
- Kumar GD, Gnanasekar N, Kurhekar P, et al. Comparative evaluation of ropivacaine and ropivacaine with dexamethasone in transverse abdominis plane block for lower abdominal surgeries: a prospective, randomized, double-blinded study. Anesth Essays Res. 2018;12(4):919–923. doi: 10.4103/aer.AER_162_18
- Zhu Q, Li L, Yang Z, et al. Ultrasound guided continuous quadratus lumborum block hastened recovery in patients undergoing open liver resection: a randomized controlled, open-label trial. BMC Anesthesiol. 2019;19(1):1–9. doi: 10.1186/s12871-019-0692-z
- Abdallah FW, Chan VW, Brull R. Transversus abdominis plane block: a systematic review. Reg Anesth Pain Med. 2012;37(2):193–209. doi: 10.1097/AAP.0b013e3182429531
- Baidya DK, Maitra S, Arora MK, et al. Quadratus lumborum block: an effective method of perioperative analgesia in children undergoing pyeloplasty. J Clin Anesth. 2015;27(8):694–696. doi: 10.1016/j.jclinane.2015.05.006
- Murouchi T, Iwasaki S, Yamakage M. Quadratus lumborum block: analgesic effects and chronological ropivacaine concentrations after laparoscopic surgery. Reg Anesth Pain Med. 2016;41(2):146–150. doi: 10.1097/AAP.0000000000000349
- Carney J, Finnerty O, Rauf J, et al. Studies on the spread of local anaesthetic solution in transversus abdominis plane blocks. Anaesthes. 2011;66(11):1023–1030. doi: 10.1111/j.1365-2044.2011.06855.x
- Tamura T, Shuichi Y, Ito S, eds. A crossover healthy volunteers study of quadratus lumborum block to detect the paravertebral space dissemination. Boston: ASA Annual Meeting; 2017.
- Dam M, Moriggl B, Hansen CK, et al. The pathway of injectate spread with the transmuscular quadratus lumborum block: a cadaver study. Anesthes Analges. 2017;125(1):303–312. doi: 10.1213/ANE.0000000000001922
- Kumar A, Sadeghi N, Wahal C, et al. Quadratus lumborum spares paravertebral space in fresh cadaver injection. Anesthes Analges. 2017;125(2):708–709. doi: 10.1213/ANE.0000000000002245
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762. doi: 10.1097/AAP.0000000000000495
- Verma K, Malawat A, Jethava D, et al. Comparison of transversus abdominis plane block and quadratus lumborum block for post-caesarean section analgesia: A randomised clinical trial. Indian J Anaesth. 2019;63(10):820–826. doi: 10.4103/ija.IJA_61_19
- Yousef NK. Quadratus lumborum block versus transversus abdominis plane block in patients undergoing total abdominal hysterectomy: a randomized prospective controlled trial. Anesth Essays And Res. 2018;12(3):742–747. doi: 10.4103/aer.AER_108_18
- Wang Y, Wang X, Zhang K. Effects of transversus abdominis plane block versus quadratus lumborum block on postoperative analgesia: a meta-analysis of randomized controlled trials. BMC Anesthesiol. 2020;20(1):103. doi: 10.1186/s12871-020-01000-2
- Sato M, Bosenberg A. Ultrasound-guided quadratus lumborum block compared to caudal ropivacaine/morphine in children undergoing surgery for vesicoureteric reflex. Pediatr Anesthesia. 2019;29(7):738–743. doi: 10.1111/pan.13650
- Alansary AM, Badawy A, Elbeialy MAK. Ultrasound-guided trans-incisional quadratus lumborum block versus ultrasound-guided caudal analgesia in pediatric open renal surgery: a randomized trial. Korean J Anesth. 2023;76(5):471–480. doi: 10.4097/kja.22774
- Kumar GD, Gnanasekar N, Kurhekar P, et al. A comparative study of transversus abdominis plane block versus quadratus lumborum block for postoperative analgesia following lower abdominal surgeries: a prospective double-blinded study. Anesth Essays Res. 2018;12(4):919. doi: 10.4103/aer.AER_162_18
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block versus transversus abdominis plane block for postoperative pain after cesarean delivery: a randomized controlled trial. Reg Anesth Pain Med. 2016;41(6):757–762. doi: 10.1097/AAP.0000000000000495
- Zhu M, Tang Y, Xu Q, et al. Quadratys lumborum block versus transversus abdominis plane block for analgesia after total abdominal hysterectomy. Int J Anesthesiol Resuscitat. 2018;39(8):741–745.
- İpek CB, Kara D, Yılmaz S, et al. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. 2019;49(5):1395–1402. doi: 10.3906/sag-1812-59
- Spence NZ, Olszynski P, Lehan A, et al. Quadratus lumborum catheters for breast reconstruction requiring transverse rectus abdominis myocutaneous flaps. J Anesth. 2016;30(3):506–509. doi: 10.1007/s00540-016-2160-y
- Wikner M. Unexpected motor weakness following quadratus lumborum block for gynaecological laparoscopy. Anaesthes. 2017;72(2):230–232. doi: 10.1111/anae.13754