ABSTRACT
Background
Preventive analgesia is designed to ensure perioperative pain control. The erector spinae plane (ESP) block may abolish the neuroendocrine stress response and augments controlled hypotensive anesthesia. But to what extent does it interfere with spinal cord function.
Methods
The patient’s population is divided into Group N (control) and Group E (ESP Group). A baseline for the amplitude and/or latency of either somatosensory evoked potentials (SSEPs) or motor evoked potentials (MEPs) were collected (30 min after induction of anesthesia and after full reverse of muscle relaxant before performing ESP block) in group E, the change from the baseline was recorded as a percent decrease. The total dose of anesthetics, the adjuvant analgesics and the postoperative complications were recorded.
Results
The change in the latency and the amplitude of SSEPs and MEPs among the two groups showed a non-significant change from the baseline. The intra-operative fentanyl consumption was significantly lower in group E than in C. The mean was 21.5 ± 25 vs 178.2 ± 46 mg respectively. The total doses of propofol and dexmedetomidine were lower in group E than in C. 18% of the patients in group E requested a rescue analgesic at a median of 70 (65) min postoperatively vs 55% of those in group C that requested analgesics earlier at a median 16(6) min.
Conclusion
The ESP block can be safely used without interfering with the monitoring of the somatosensory and MEPs during complex spinal surgery.
1. Background
Preventive analgesia is designed to ensure appropriate level of perioperative pain control and to prevent acute as well as chronic pain [Citation1]. The type of surgery plays a crucial role in tailoring the analgesic regimen, those patients who are scheduled for spinal fusion surgery, usually need a complex multimodal analgesic protocol. Whenever possible, regional block should be a part of this regimen [Citation2], as directly blocking the activity of pain receptors by local anesthetics will eliminate or even reduce the need for long-term use of opioids [Citation3]. An issue which represents a cornerstone in enhanced recovery after surgery [Citation2].
Patient-related factors also play a role in the choice of the appropriate analgesic plan. Patients with scoliosis usually suffer from a restrictive pulmonary disease and will benefit from decreasing the opioid requirements [Citation2].
Ultrasound guided erector spinae plane (ESP) block involves local anesthetic injection between the erector spinae muscle group and the underlying transverse process [Citation4]. The mechanism of action of the ESP block is controversial as some suggest that the local anesthetic spreads- to soil the spinal dorsal rami through the paravertebral space or the epidural space, while others have suggested only facial spread [Citation5–7].
The ESP block is not only a mere analgesic, but also it aborts the neuroendocrine stress response and ensures a hypotensive and stable hemodynamic state without interfering with the spinal cord function as expected with neuraxial blocks [Citation7,Citation8].
Neurophysiological monitoring has largely been used with different types of surgery, replacing intraoperative wake-up testing. Somatosensory evoked potentials (SEPs) and motor evoked potentials (MEPs) are commonly used during spinal fusion surgery to improve the decision and possibly reduce the anticipated neurologic complications. The sites of stimulation and recording are the determinants of the morphology of the recorded waveform, while the amplitude and latency provide functional neurological assessment [Citation9–11].
Various anesthetic agents have different impacts on neurophysiological monitoring, the anesthetic agents may affect the interpretation of the electrophysiological monitoring which is usually needed to prevent radiculopathy [Citation12,Citation13]. In general, inhalational agents have a greater effect on all modes than do intravenous agents, MEPs are very sensitive, SSEPs are moderately affected [Citation9]. Some agents show controversy, while limited data are available on other agents like Dexmedetomidine and lidocaine [Citation14].
Accordingly, the goals of anesthesia for spine corrective surgery include maintaining hemodynamic stability with optimal pain control without interfering with the neuromonitoring [Citation7]. An issue has been raised by some authors whether ESP block would interfere with MEPs or SSEPs during spine surgery [Citation15–17], but results have not been yet validated.
1.1. Keywords
ESP block, neurophysiological monitoring, scoliosis repair.
1.2. Aim of the study
The aim is to study the possible effect of ESP block on neurophysiological monitoring in patients undergoing scoliosis repair.
2. Patients and methods
2.1. Study population
This study is a prospective randomized double blinded clinical trial (the patients and those involved in the data collection were blind). It was conducted at Ain Shams university hospitals’ general operating room, Cairo, Egypt over a period of 6 months from February till August 2023. After approval of the research ethical committee, all the patients or their guardians signed a written informed consent. Randomization was performed using a computer-generated random number sequence.
2.2. Ethical approval and clinical trial registration
The study was approved by the ethical committee of the faculty of medicine, Ain Shams University with approval number FAMSU R 193/2022. Clinical trial registration NCT05632016.
2.3. Sample size and study groups
The sample size was calculated by using power analysis and sample size software [PASS 11] (version 11.0.08) for sample size calculation, to reach power of 99%, at alpha error of 5%, after reviewing the previous study results by Siam et al., 2020 [Citation18]. They showed a response state entropy mean after ESP at the end of anesthesia which is lower than before induction (70.67 ± 10.36 vs 89.67 ± 2.74 respectively); based on a sample size of 40 patients undergoing scoliosis repair under TIVA divided into two groups (20 patients in each group). Accordingly, 44 patients were included in this study for possible drop out and were allocated into two groups: Group C (control) N = 22: where the patients received only intravenous analgesia without any regional block. Group E (ESP block) N = 22: where the patients in addition received ESP block immediately after induction of anesthesia and before the skin incision.
2.4. Inclusion criteria
Patients between 12 and 25 years old with an American society of anesthesiologists (ASA) status up to III, undergoing posterior spinal fixation for scoliosis repair.
2.5. Exclusion criteria
Patients with an ASA status above III, patient or guardian refusal to participate, patients with multiple congenital anomalies, hypersensitivity, or contraindication to the study drugs and those with a body weight less than 40 kg.
2.6. Study outcomes
The primary outcome was to test the effect of ESP block on neurophysiological monitoring. Secondary outcome was to study the contribution of ESP block in decreasing the total dose of anesthetics used as well as achieving tight intra and postoperative pain control, and the impact on the early ambulation as one of the components of the enhanced recovery after surgery.
2.7. Study procedures
All the patients were assessed by detailed medical history, general examination. Complete blood count, serum creatinine, coagulation profile, random blood sugar, chest radiograph, pulmonary function tests, echocardiography were all done. The patients were monitored using 5-leads ECG, invasive blood pressure monitoring, capnography, bispectral index (BSI) and plethysmography. Anesthesia was induced using 1 µg/kg of fentanyl, propofol 2 mg/kg and 0.5 mg/kg of atracurium. Endotracheal intubation was done using wire reinforced endotracheal tube and positive pressure ventilation was adjusted to maintain an end-tidal carbon dioxide partial pressure between 30 and 35 mmHg. Anesthesia was maintained using propofol infusion at a rate of 80–150 μg/kg/min and dexmedetomidine 0.3–0.7 μg/kg/hr. Doses were adjusted to maintain bispectral index (BSI) around 50.
In group (C), patients were given 0.1 mg/kg morphine sulphate up to a total of 10 mg and 2–4 mg to be given after 4 hrs as needed.
In group (E), the Level above the kyphosis angle at T8- T10 and that below the angle of kyphosis at L3 were identified, ESP block was performed on both sides using a curvilinear probe placed in a parasagittal plane 3 cm lateral to the spinous process above and below the selected level. A 12-cm 22-gauge echogenic needle was directed using in plane technique targeting the plane below the erector spinae muscles. Injection of 10 mL of bupivacaine 0.25% at each of the four selected point was done.
If systolic blood pressure or heart rate increased > 20 above baseline, a bolus of 1 μg/kg fentanyl was given. At the end of surgery, total intravenous anesthesia (TIVA) was discontinued before surgical field closure. The patients were extubated after regaining consciousness, breathing spontaneously, and responding to verbal commands.
If there was a major change in the hemodynamics, body temperature or failure of extubation, the patient was excluded from the study and replaced by another.
Postoperative analgesic regimen was intravenous paracetamol 1 gm/8hr, intravenous ketorolac 30 mg/6hr, for those with a body weight less than 50 kg, 15 mg/6hr. while in the age group of 12–16 years were 0.5 mg/kg/6 hr with a total daily dose less than 60 mg. Morphine was given as a rescue analgesic in the case of moderate to severe pain with numerical analogue score (NAS) exceeding 7 with a dose of 0.1 mg/kg.
Those patients with NAS 0–3 were classified as having mild pain, while those with a pain score in the range of 4–6 were classified as having a moderate pain and those with a pain score more than 7 were classified as having severe pain.
2.8. Measurements
Hemodynamic parameters including heart rate and mean arterial blood pressure were continuously monitored and recorded before and after the induction of anesthesia, then at 30 min intervals throughout the surgery. The total dose of propofol, dexmedetomidine and the need for intraoperative fentanyl were also recorded.
A baseline for the amplitude and latency of either SSEPs or MEPs were collected before ESP block (30 min after induction of anesthesia and after full reversal of muscle relaxant, before performing ESP), a change of the baseline at any time throughout the whole operative time was then recorded. Whenever there was a failure of neurophysiological monitoring a wake-up test was done and recorded (the anesthesia is markedly lightened or even discontinued directly following instrumentation of the spine, and the patient is asked to move his feet while still intubated and the surgical site still open. After test is completed anesthesia is resumed with the same regimen).
Emergence time was recorded, it was defined as the time from end of anesthesia delivery till full recovery state. Postoperative analgesia using NAS at time intervals 2, 4, 8 hr postoperatively was recorded. Time to first rescue analgesic and the total dose of morphine given were all recorded. Any postoperative complication including respiratory depression, post-operative nausea and vomiting (PONV) or constipation was recorded.
2.9. Statistical analysis
Data were analyzed using Microsoft 365 software package version. Qualitative data were described using number and percent. The normal distribution of the data was tested by using Shapiro Wilk test. Mean and standard deviation, median and interquartile range were used to describe quantitative data. The correlation of the categorical data was done by using Chi-square test and Fisher’s Exact or Monte Carlo correction if more than 20% of the cells show data count less than 5. For the normally distributed quantitative data, Student t-test was used while Mann–Whitney test for abnormally distributed quantitative data. P-value less than 0.05 is statistically significant.
3. Results
There were no significant differences in the demographic data among the two groups as shown in .
Table 1. Descriptive statistics for the patients in the two groups.
No significant statistical difference in the preoperative hemodynamic data among the two groups as shown in . The average values of intraoperative systolic and diastolic blood pressures were significantly higher in group C compared to group E in , but the average for the heart rate was comparable among the two groups.
Table 2. Average preoperative hemodynamic data.
Table 3. Average intraoperative hemodynamics data.
The percent decrease in the SSEPs and MEPs from the baseline regarding the latency and the amplitude among the two groups showed a non-significant change as shown in .
Table 4. Percent of the Change from the baseline among the Somatosensory evoked potential andmotor evoked potential among the two groups.
The total dose of intra-operative fentanyl consumption was significantly lower in group E compared to group C.
Eighteen percent of the patients in group E requested a rescue analgesic at a median of 70 (65) min postoperatively vs 55% of those in group C requested analgesic earlier at a median 16 (6) min. In group E, postoperative pain in 14 patients was controlled by a combination of NSAIDs and paracetamol, where only 8 patients were controlled by opioids. While in Group C, 86% of the patients needed opioids to control the pain as shown in .
Table 5. Comparing the need for intraoperative and postoperative analgesics in both groups.
The assessment of severity of pain at 2, 4, and 8 hr by using NAS showed better control of pain among the patients in group E, as shown in .
Table 6. Severity of pain among the two groups at different times postoperatively.
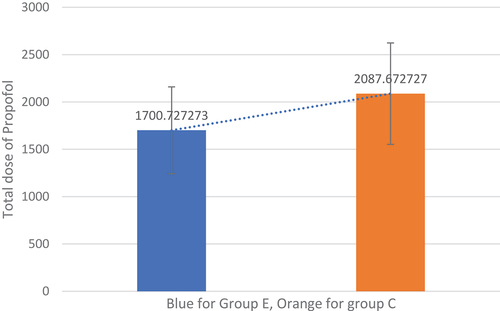
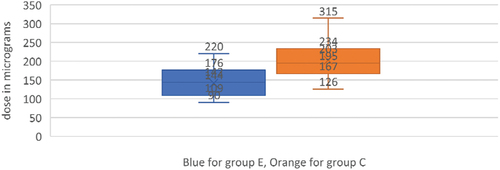
The total doses of propofol and dexmedetomidine were significantly lower in group E than in group C as shown in .
4. Discussion
It is well known that using large doses of opioids in the intra and postoperative settings of posterior spinal fusion (PSF) surgery leads to hazardous drawbacks, including respiratory depression, sedation, pruritus, nausea, vomiting, constipation, and ileus [Citation19]. Yet, pain is not tightly controlled in most of cases despite receiving mega doses of opioids thus increasing the risk for cardiac and respiratory complications, prolonging hospital stay by delaying mobilization and raising the incidence of developing chronic pain syndrome [Citation20]. Regional anesthesia techniques have not been applied routinely in spine surgery for fear of interference with postoperative neurological examination of the functions of the spinal cord, rendering neuraxial analgesia including spinal and epidural blocks as non-preferable techniques [Citation7].
The current study reveals that the ESP block didn’t influence the neurophysiological monitoring as there was no significant change from the baseline regarding both amplitudes and latencies of evoked potentials among the patients in the two groups.
While many studies have reported the impact of ESP block on the intraoperative pain control as being reflected on the hemodynamic stability and lower consumption of anesthetic drugs as well as on the postoperative analgesic requirements as reflected on the lower pain scores, limited studies highlighted the impact of ESP block on intraoperative neuromonitoring.
Ueshima et al. [Citation21], in their retrospective study reported how ESP block could effectively kill the pain after lumbar spinal surgeries up to 24 hr Almeida et al. [Citation22], reported in their study that the block at the level of T8, will target the dorsal rami of the spinal nerves, which could explain the intense analgesia offered by the block postoperatively even in case of ongoing pathologies like spinal hematoma or infection.
Chin et al. [Citation23], reported ESP block for corrective spine surgeries as a simple and effective way in the regards of opioid-sparing in extensive multi-level correction by inducing adequate level of preemptive analgesia. Moreover Diwan et al. [Citation15], described it as a safe technique even with anatomical malformations, as they recorded neither a complication nor interference with the evoked potentials after scoliosis surgery in their case series.
The results in the aforementioned study were matching with the results in the study done by Zhang et al., and Siam et al. [Citation18,Citation24], where 13.3% of the patients studied by Siam et al., consumed a rescue fentanyl with a mean dose of 10.0 ± 28.03 µg with ESP block vs 53.3% patients used a higher dose of rescue fentanyl with a mean of 46.67 ± 48.06 µg during lumbar spine surgery with conventional general anesthesia. In addition, they concluded that ESP block could maintain an appropriate level of anesthesia through their watching for the hemodynamic data.
The mean difference for NAS for postoperative pain in a study done by Liu et al. [Citation25], between two groups of patients, one group received ESP block and the other is a control group was −1.89 at 2hr, −1.09 at 12 hr, and −0.68 at 12 hr. These results show a significant reduction in the postoperative use of opioid narcotics.
5. Conclusion
In our study, we concluded that ESP block can be safely used as a part of multimodal analgesia with total intravenous anesthesia to achieve an appropriate level of intra and post-operative analgesia without interfering with the monitoring of the somatosensory and MEPs during complex spinal surgery. The use of ESP block in this type of surgery could help in the adoption of enhanced recovery strategies in terms of avoiding or minimizing the use of opioids, maintaining a steady hemodynamic state and allowing for an early ambulation.
Disclosure statement
No potential conflict of interest was reported by the author(s).
References
- Ong CK, Lirk P, Seymour RA, et al. The efficacy of preemptive analgesia for acute postoperative pain management: a meta-analysis. Anesth Analg. 2005;100(3):757–773. doi: 10.1213/01.ANE.0000144428.98767.0E
- Mariano ER. Management of acute perioperative pain in adults. Uptodate. 2022;1:98.
- Leung CC, Chan YM, Ngai SW. Effect of pre-incision skin infiltration on post-hysterectomy pain—a double-blind randomized controlled trial. Anaesth Intensive Care. 2000;28(5):510. doi: 10.1177/0310057X0002800504
- Forero M, Adhikary SD, Lopez H, et al. The erector spinae plane block: a novel analgesic technique in thoracic neuropathic pain. Reg Anesth Pain Med. 2016;41(5):621–627. doi: 10.1097/AAP.0000000000000451
- Chin KJ, El-Boghdadly K. Mécanismes d’action du bloc du plan des muscles érecteurs du rachis (erector spinae, ESP) : un compte rendu narratif. Can J Anesth/J Can Anesth. 2021;68(3):387–408. doi: 10.1007/s12630-020-01875-2
- Chin KJ, Malhas L, Perlas A. The erector spinae plane block provides visceral abdominal analgesia in bariatric surgery: a report of 3 cases. Reg Anesth Pain Med. 2017;42(3):372–376. doi: 10.1097/AAP.0000000000000581
- Renee JC, van den Broek RJ, van de Geer R, et al. Evaluation of adding the erector spinae plane block to standard anesthetic care in patients undergoing posterior lumbar interbody fusion surgery. Sci Rep. 2021;11(1):7631. doi: 10.1038/s41598-021-87374-w
- Wang AZ, Fan K. Ultrasound-guided posterior ramus of spinal nerve block for anesthesia and analgesia in lumbar spinal surgery. J Clin Anesth. 2019;1(52):48–49. doi: 10.1016/j.jclinane.2018.08.032
- Koht A, Sloan TB, Hemmer LB, et al. Neuromonitoring in surgery and anesthesia. Uptodate. 2022:1–44.
- Jameson LC, Sloan TB. Monitoring of the brain and spinal cord. Anesthesiol Clin. 2006;24(4):777–791. doi: 10.1016/j.atc.2006.08.002
- Chui J, Manninen P, Valiante T, et al. The anesthetic considerations of intraoperative electrocorticography during epilepsy surgery. Anesth Analg. 2013;117(2):479. doi: 10.1213/ANE.0b013e318297390c
- Holland NR. Intraoperative electromyography. J Clin Neurophysiol. 2002;19(5):444. doi: 10.1097/00004691-200210000-00007
- Hamilton DK, Smith JS, Sansur CA, et al. Rates of new neurological deficit associated with spine surgery based on 108,419 procedures: a report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976). 2011;36(15):1218–1228. doi: 10.1097/BRS.0b013e3181ec5fd9
- Bala E, Sessler DI, Nair DR. Motor and somatosensory evoked potentials are well maintained in patients given dexmedetomidine during spine surgery. Anesthesiology. 2008;109(3):417. doi: 10.1097/ALN.0b013e318182a467
- Diwan SM, Yamak Altinpulluk E, Khurjekar K, et al. Bloqueo bilateral en el plano del músculo erector de la columna para cirugía de escoliosis: serie de casos. Rev Esp Anestesiol Reanim. 2020;67(3):153–158. doi: 10.1016/j.redar.2019.11.012
- Melvin JP, Schrot RJ, Chu GM, et al. Bloc du plan des muscles érecteurs du rachis thoracique bas pour analgésie périopératoire dans la chirurgie du rachis lombosacré : une série de cas. Can J Anaesth. 2018;65(9):1057–1065. doi: 10.1007/s12630-018-1145-8
- Tsui BCH, Esfahanian M, Lin C, et al. Moving toward patients being pain and spasm-free after pediatric scoliosis surgery by using bilateral surgically placed erector spinae plane catheters. Can J Anaesth. 2020;67(5):621–622. doi: 10.1007/s12630-019-01543-0
- Siam EM, Abo Aliaa DM, Elmedany S, et al. Erector spinae plane block combined with general anaesthesia versus conventional general anaesthesia in lumbar spine surgery. Egypt J Anaesth. 2020;36(1):201–226. doi: 10.1080/11101849.2020.1821501
- Cozowicz C, Olson A, Poeran J. Opioid prescription levels and postoperative outcomes in orthopedic surgery. Pain. 2017;158(12):2422–2430. doi: 10.1097/j.pain.0000000000001047
- Tepsoparn M, Sereeyotin J, Pannangpetch P. Efects of combined lower thoracic epidural/general anesthesia on pain control in patients undergoing elective lumbar spine surgery: a randomized controlled trial. Spine. 2018;43(20):1381–1385. doi: 10.1097/BRS.0000000000002662
- Ueshima H, Inagaki M, Toyone T, et al. Efficacy of the erector spinae plane block for lumbar spinal surgery: a retrospective study. Asian Spine J. 2019;13(2):254–257. doi: 10.31616/asj.2018.0114
- Almeida CR, Oliveira AR, Cunha P. Continuous bilateral erector spinae plane block at T8 for extensive lumbar spine fusion surgery: case report. Pain Pract. 2019;19(5):536–540. doi: 10.1111/papr.12774
- Chin KJ, Dinsmore MJ, Lewis S, et al. Opioid-sparing multimodal analgesia with bilateral bi-level erector spinae plane blocks in scoliosis surgery: a case report of two patients. Eur Spine J. 2020;29(Suppl 2):138–144. doi: 10.1007/s00586-019-06133-8
- Zhang TJ, Zhang JJ, Qu ZY. Bilateral Erector Spinae Plane Blocks for Open Posterior Lumbar Surgery. J Pain Res 2020; Volume 13:13:709–717. doi: 10.2147/JPR.S248171
- Liu MJ, Zhou XY, Yao YB, et al. Postoperative analgesic efficacy of erector spinae plane block in patients undergoing lumbar spinal surgery: a systematic review and meta-analysis. Pain Ther. 2021;10(1):333–347. doi: 10.1007/s40122-021-00256-x